Abstract
Background
In ovarian carcinomas, the likelihood of disease cure following first-line medical-surgical treatment has been poorly addressed. The objective was to: (a) assess the likelihood of long-term disease-free (LDF) > 5 years; and (b) evaluate the impact of the tumour primary chemosensitivity (assessed with the modelled CA-125 KELIM) with respect to disease stage, and completeness of debulking surgery.
Methods
Three Phase III trial datasets (AGO-OVAR 9; AGO-OVAR 7; ICON-7) were retrospectively investigated in an “adjuvant dataset”, whilst the Netherlands Cancer Registry was used in a “neoadjuvant dataset”. The prognostic values of KELIM, disease stage and surgery outcomes regarding the likelihood of LDF were assessed using univariate/multivariate analyses.
Results
Of 2029 patients in the “adjuvant dataset”, 82 (4.0%) experienced LDF (Stage I–II: 25.9%; III: 2.1%; IV: 0.5%). Multivariate analyses identified disease stage and KELIM (OR = 4.24) as independent prognostic factors. Among the 1452 patients from the “neoadjuvant dataset”, 36 (2.4%) had LDF (Stage II–III: 3.3%; IV: 1.3%). Using multivariate tests, high-risk diseases (OR = 0.18) and KELIM (OR = 2.96) were significant.
Conclusion
The probability of LDF > 5 years after first-line treatment in 3486 patients (<4%) was lower than thought. These data could represent a reference for future studies meant to assess progress related to PARP inhibitors.
Similar content being viewed by others
Introduction
The majority of patients (~75%) with high-grade carcinomas are diagnosed at advanced Stages III–IV [1]. The standard treatment in the first-line setting has historically relied on the combination of debulking surgery and systemic medical therapy. In addition, maintenance treatment with poly(ADP-ribose) polymerase inhibitors (PARPi) and/or bevacizumab as maintenance treatment was recently introduced [2,3,4].
The strong prognostic value of the completeness of debulking surgery has largely been reported and structured in the disease management guidelines. More recently, potential indicators of the tumour primary platinum sensitivity were described, including the ELIMination rate constant K (KELIM), based on the longitudinal kinetics of CA-125 during the first 100 days of first-line platinum-based chemotherapy [5]. KELIM, calculated with the mathematical equation driving the CA-125 longitudinal kinetics (≥3 values) during the first three to four cycles of neoadjuvant or adjuvant chemotherapy, has been developed to obtain an accurate characterisation of the CA-125 dynamics. The reliability of KELIM as an independent indicator of tumour platinum-based chemosensitivity has been reproducibly shown in many studies with more than 12,000 patients [6,7,8,9,10,11,12]. These studies have confirmed the capacity of KELIM to reproducibly predict: (1) the likelihood of complete resection at IDS in the neoadjuvant setting, (2) the probability of subsequent platinum-resistant relapse, (3) the patient PFS and OS.
The main purpose of medical-surgical treatment is to maximise the likelihood of obtaining a disease cure. It is considered that ~70% of patients with epithelial ovarian cancers will experience disease relapse, with numbers varying according to disease stages (from 10% at Stage I to 90% at Stage IV) (https://www.cancer.org/cancer/ovarian-cancer/detection-diagnosis-staging/survival-rates.html). However, the probability of cure has actually been poorly addressed.
The objective was to assess the likelihood of disease cure, explored with the rate of long-term disease-free (LDF) ≥ 5 years after first-line treatment, and evaluate the respective parts of (1) the tumour primary chemosensitivity, (2) disease stage and (3) the completeness of debulking surgery, relative to the success of the medical-surgical treatment, before the emergence of PARPi.
Methods
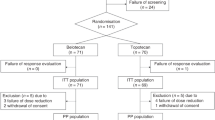
Three large randomised Phase III datasets encompassing 2868 patients treated with the standard first-line carboplatin-paclitaxel (CP) regimen with/without a third agent (AGO-OVAR 9, CP ± gemcitabine; AGO-OVAR 7, CP ± topotecan; and ICON-7 trials, CP ± bevacizumab), previously analysed for KELIM investigation [6], were used to build an “adjuvant dataset” of 2029 assessable patients (70.7%) with Stage I–IV diseases, treated with primary debulking surgery and adjuvant chemotherapy. LDF was defined as the absence of disease progression or death within the first 5 years. Patients were assessable if they had experienced disease progression or death, or if they were free-of-progression or death with a minimum 5-year follow-up. The Netherlands Cancer Registry (NCR) composed of 1582 patients with Stage II–IV diseases treated with neoadjuvant chemotherapy potentially followed by interval debulking surgery (IDS) was used to build a “neoadjuvant dataset” with 1452 assessable patients (91.8%) [10].
The calculation of individual KELIM values in these datasets was previously reported [6, 10].
Descriptive statistics, along with univariate and multivariate logistic regressions were performed to assess the prognostic values of pathological subtypes; treatment arms; disease stage combined to the completeness of IDS in order to separate high-risk diseases (Stage IV, or incompletely resected Stage III diseases) and low-risk diseases in the NCR; and individual standardised (std) KELIM (considered as a continuous covariate; or categorised as a score: unfavourable if <1, or favourable if ≥1). BRCA mutational status was available for a small percentage of patients enrolled in the NCR. To explore the prognostic value of KELIM with respect to BRCA mutational status, univariate and multivariate analyses were performed in the subgroup of patients with known BRCA mutational status.
To account for the limited number of patients with LDF and potential biases related to the exclusion of patients without progression events within the first 5 years, censored quantile regressions were performed in order to assess the effects of these parameters on the distributions of progression-free survival (PFS) events [13].
All assessed studies (AGO-OVAR 7, AGO-OVAR 9, ICON-7 and NCR) were conducted in accordance with the Declaration of Helsinki ethical guidelines. All patients recruited in the study signed an informed written consent.
Results
The characteristics of assessable patients are presented in Table 1. Out of 2029 patients in the “adjuvant dataset” (median PFS, 13.8 months, 95% CI 13.3–14.2; median overall survival, 37.9 months, 95% CI 36.8–39.8), 82 patients (4.0%) experienced LDF (45-month median follow-up). As expected, the probability of LDF decreased in higher disease stages, from 25.9% in Stage I–II, to 2.1% in Stage III, and 0.5% in Stage IV. The median std KELIM was significantly higher among patients who experienced LDF (1.14 versus 0.81 days−1, P < 0.01). Among 641 patients with favourable std KELIM (31.5%), 7.9% experienced LDF, ranging from 34.9% in Stage I–II to 4.5% in Stage IV. Using logistic regression models, two significant independent prognostic factors were associated with the likelihood of LDF: disease stage (Stage I–II, reference; Stage III, odds ratio (OR) = 0.07, 95% confidence interval (CI) 0.04–0.12; Stage IV, OR = 0.02, 95% CI 0.00–0.07); and std KELIM (OR = 4.24, 95% CI 2.36–7.69) (Fig. 1a). Censored quantile regression of PFS distribution showed that the highest evaluable decile (6th decile) of the failure-time of patients with favourable was higher by 23.0 months (95% CI 13.4–29.9) compared to those with unfavourable KELIM.
Multivariate logistic regression model of the probability of long-term disease-free (LDF) > 5 years according to: a disease stage and standardised KELIM in the “adjuvant dataset”; b to disease-risk group (based the disease stage and the completeness of interval debulking surgery) and to standardised KELIM in the “neoadjuvant dataset” (Netherlands Cancer Registry). For example, for a patient with a Stage III disease, the probability of LDF is estimated at 7.0% in the case of complete IDS & favourable std KELIM at 1.5 days−1; 3.0% in the case of complete IDS & unfavourable std KELIM at 0.5 days−1; 2.0% in the case of incomplete IDS & favourable std KELIM at 1.5 days−1; and 1.0% in the case of incomplete IDS & favourable std KELIM at 0.5 days−1. Dashed black line: cut-off for unfavourable KELIM < 1; or favourable KELIM ≥ 1. LCR Long complete remission.
Among the 1452 patients in the “neoadjuvant dataset” (median PFS, 12.1 months, 95% CI 11.6–12.4; median overall survival, 23.1 months, 95% CI 21.8–24.2), 36 patients (2.4%) experienced LDF (95-month median follow-up) (Table 1). Similarly, to the “adjuvant dataset”, the percentages of patients experiencing LDF were higher among patients with favourable KELIM, regardless of disease stage (Table 1). Using logistic regression models, two independent prognostic factors were significantly associated with the likelihood of LDF: disease-risk group (high-risk versus low-risk, OR = 0.18, 95% CI 0.07–0.38); and std KELIM (OR = 2.96, 95% CI 1.46–5.90) (Fig. 1B). Censored quantile regressions of PFS distribution showed that the highest evaluable decile (8th decile) of the failure-time of patients with favourable was higher by 12.0 months compared to unfavourable KELIM (95% CI 8.2–17.7), and lower by −25.1 months (95% CI −39.7 to −17.6) for those with high-risk versus low-risk diseases.
The germline BRCA mutational status was available in 449 patients of the NCR (30.9%) (Table 1). BRCA1 mutation did not exhibit any prognostic value in univariate analysis (yes versus no, OR = 1.0, 95% CI 0.15–3.79). Among patients with a BRCA2 mutation (n = 30 patients), LDF were observed in a higher percentage of patients (16.7%), regardless of KELIM. In the multivariate analysis, standardised KELIM was not significantly associated with survival when tested together with high-risk disease (yes versus no, OR = 0.28, 95% CI 0.08–0.95) and BRCA2 mutation (yes versus no, OR = 1.78, 95% CI 1.46–21.03), suggesting that BRCA2 mutation integrates the information about the tumour’s intrinsic chemosensitivity.
Discussion
The actual risk of disease relapse after first-line treatment is a subject of controversies. Indeed very few studies addressed this question, and inconsistent numbers were reported in the literature, ranging from 17 to 80% [14, 15].
This study composed of two large independent datasets, provides new data about the determinants of the first-line treatment success before the PARPi era. The present study showed that the probability of disease cure after first-line treatment was much lower than thought within the scientific community. In patients with Stage III and IV, representing ~75% of cases at diagnosis, the rates of LDF were only ~3%, and ~1%, respectively. As expected, the overall prognosis of patients treated with neoadjuvant chemotherapy and interval debulking surgery was worse than those treated with primary debulking surgery, in terms of PFS, and OS especially. Nevertheless, the probability of long-term disease-free was not very different between the two datasets, thereby meaning both endpoints are not necessarily related.
Interestingly, our data show that these probabilities are 3.5 times higher in patients with favourable KELIM compared to those with unfavourable KELIM, suggesting a major role of tumour primary chemosensitivity. The multivariate logistic regression models confirmed that the tumour primary chemosensitivity exhibited an independent prognostic value, together with the disease stage and the completeness of IDS.
These results should be analysed with caution due to significant limitations. Among them, the selection of the LDF as a potential indicator of disease cure is highly debatable. Approximately 22% of patients were not assessable regarding this endpoint (29% for the “adjuvant dataset” and 8% for the “neoadjuvant dataset”). To account for the potential biases related to the exclusion of these patients, the censored quantile regressions of all patient PFS distributions confirmed the impact of KELIM on the highest PFS deciles. Moreover, the present study is limited by the heterogeneity of patient characteristics and medical-surgical treatments, the low numbers of patients with Stage I–II diseases, along with the lack of data about the completeness of surgery and BRCA mutational status in the “adjuvant dataset”. The BRCA mutational status was available for only 31% of patients of IKNL registry (449 patients), meaning that the data about links between KELIM and BRCA1 or BRCA2 mutations are still very exploratory. Recent data on patients enrolled in the SOLO-1, PAOLA-1 and PRIMA trials suggest that the probability of LDF will improve with PARPi in the future [16]. It is likely that the patients with BRCA2 mutations will derive the highest benefit from these therapeutics [17,18,19]. A part of this effect may be related to the higher tumour primary chemosensitivity related to BRCA2 mutation, as suggested here with KELIM.
The present data could be used as a reference for future studies meant to assess the progress related to the introduction of PARPi in the first-line setting.
References
Torre LA, Trabert B, DeSantis CE, Miller KD, Samimi G, Runowicz CD, et al. Ovarian cancer statistics, 2018. CA Cancer J Clin. 2018;68:284–96.
Colombo N, Sessa C, Bois AD, Ledermann J, McCluggage WG, McNeish I, et al. ESMO-ESGO consensus conference recommendations on ovarian cancer: pathology and molecular biology, early and advanced stages, borderline tumours and recurrent disease. Int J Gynecol Cancer. 2019;30:672–705.
Karam A, Ledermann JA, Kim JW, Sehouli J, Lu K, Gourley C, et al. Fifth Ovarian Cancer Consensus Conference of the Gynecologic Cancer InterGroup: first-line interventions. Ann Oncol. 2017;28:711–7.
Tew WP, Lacchetti C, Ellis A, Maxian K, Banerjee S, Bookman M, et al. PARP inhibitors in the management of ovarian cancer: ASCO guideline. J Clin Oncol. 2020;38:3468–93.
You B, Freyer G, Gonzalez-Martin A, Lheureux S, McNeish I, Penson RT, et al. The role of the tumor primary chemosensitivity relative to the success of the medical-surgical management in patients with advanced ovarian carcinomas. Cancer Treat Rev. 2021;100:102294.
Colomban O, Tod M, Leary A, Ray-Coquard I, Lortholary A, Hardy-Bessard AC, et al. Early modeled longitudinal CA-125 kinetics and survival of ovarian cancer patients: a GINECO AGO MRC CTU Study. Clin Cancer Res. 2019;25:5342–50.
Colomban O, Tod M, Peron J, Perren TJ, Leary A, Cook AD, et al. Bevacizumab for newly diagnosed ovarian cancers: best candidates among high-risk disease patients (ICON-7). JNCI Cancer Spectr. 2020;4:pkaa026. https://doi.org/10.1093/jncics/pkaa026.
You B, Robelin P, Tod M, Louvet C, Lotz JP, Abadie-Lacourtoisie S, et al. CA-125 Elimination rate constant K (KELIM) is a marker of chemosensitivity in patients with ovarian cancer: results from the phase II CHIVA trial. Clin Cancer Res. 2020;26:4625–32.
Corbaux P, You B, Glasspool R, et al. Survival prognostic and surrogate values of the early modeled CA-125 KELIM in newly diagnosed advanced ovarian cancer: data from the GCIG meta-analysis group. Ann Oncol. 2021;32:S744.
Van Wagensveld L, Colomban O, Van der AA M, Sonke GS, Kruitwagen R, You B. 847P The prognostic value of chemosensitivity, estimated by the modeled CA-125 KELIM, in ovarian cancer patients treated with neo-adjuvant chemotherapy in the Netherlands. 2020;31:S633. https://doi.org/10.1016/j.annonc.2020.08.986.
You B, Clamp A, Cook A, McNeish I, Colomban O. Differential benefit from fractionated dose-dense first-line chemotherapy for epithelial ovarian cancer (EOC) according to KELIM-evaluated tumor primary chemosensitivity: exploratory analyses of ICON-8 trial. J Clin Oncol. 2021;39:5530–5530.
You B, Sehgal V, Hosmane B, Chen B, Huang X, Sullivan D M. et al. Prognostic value and association with veliparib benefit of modeled CA-125 elimination kinetics (KELIM) in patients with newly diagnosed ovarian cancer: analysis from the VELIA/GOG-3005 Study. Int. J. Gynecol. Cancer. 2020;30:A24–A25.
Qiu Z, Ma H, Chen J, Dinse GE. Quantile regression models for survival data with missing censoring indicators. Stat Methods Med Res. 2021;30:1320–31.
Pignata S, S CC, Du Bois A, Harter P, Heitz F. Treatment of recurrent ovarian cancer. Ann Oncol. 2017;28:viii51–viii6.
du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d’Investigateurs Nationaux Pour les Etudes des Cancers de l’Ovaire (GINECO). Cancer. 2009;115:1234–44.
Mirza MR, Coleman RL, Gonzalez-Martin A, Moore KN, Colombo N, Ray-Coquard I, et al. The forefront of ovarian cancer therapy: update on PARP inhibitors. Ann Oncol. 2020;31:1148–59.
DiSilvestro P, Colombo N, Scambia G, Kim BG, Oaknin A, Friedlander M, et al. Efficacy of maintenance olaparib for patients with newly diagnosed advanced ovarian cancer with a BRCA mutation: subgroup analysis findings from the SOLO1 trial. J Clin Oncol. 2020;38:3528–37.
Monk BJ, Gonzalez Martin A. Efficacy of niraparib therapy in patients with newly diagnosed advanced ovarian cancer by BRCA and homologous recombination status: PRIMA/ENGOT-OV26/GOG-3012 study. Proceedings of SGO 2020 Virtual Meeting. 2020. https://sgo.confex.com/sgo/2020/meetingapp.cgi/Paper/15986.
Coleman RL, Oza AM, Lorusso D, Aghajanian C, Oaknin A, Dean A, et al. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;390:1949–61.
Acknowledgements
This work was supported by the Dutch Cancer Society [IKNL2014–6838]. OC is an employee of Lyon University. Previous Presentation: This work was presented as a « mini-oral presentation » at ESMO 2020 congress (Abs 815 MO).
Funding
None.
Author information
Authors and Affiliations
Contributions
Study design, analyses of the data, methodology, discussion, manuscript writing and approval: BY, LLVW, MT and OC. Ressources, study design, manuscript writing and approval: GS, HH, RK and MVA. Ressources, analyses of the data, manuscript writing, approval: AdB, FS, TP, JP, FJ, AC, MCK, KW, AL, OT, AL and GF.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All assessed studies (AGO-OVAR 7, AGO-OVAR 9, ICON-7 and NCR) were conducted in accordance with the Declaration of Helsinki ethical guidelines. All patients recruited in the study signed an informed written consent.
Consent to publish
Not applicable.
Competing interests
AdB: Honoraria/Institutional Grants for Advisory Boards and/or educational activities (last 3 years): Roche; AstraZeneca/MSD; GSK/Tesaro; Clovis; Pfizer; Biocad; Genmab/Seattle Genetics; AMGEN; Zodiac; Founder/Chairman/Executive Board AGO Study Group; Co-Founder, Strategic Board and past president ENGOT; Past Chairman, Scientific Committee, and faculty of consensus conferences GCIG and ESGO/ESMO; Past/Present member national guideline committees Breast- and Ovarian Cancer, and multiple further; Committees, working groups, and editorial boards (eg. J Clin Oncol, Gynecol Oncol, Int J Gynecol Cancer); GSS: GSS reports institutional research support from AstraZeneca, Biovica, Merck, Novartis, Roche and Seagen. BY: consulting for MSD, AstraZeneca, GSK-TESARO, BAYER, Roche-Genentech, ECS Progastrine, Novartis, LEK, Amgen, Clovis Oncology, Merck Serono, BMS, SEAGEN, Myriad. The other authors declare no competing interests that might have impacted the results of this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
You, B., Van Wagensveld, L., Tod, M. et al. Low probability of disease cure in advanced ovarian carcinomas before the PARP inhibitor era. Br J Cancer 127, 79–83 (2022). https://doi.org/10.1038/s41416-022-01732-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-01732-7