Abstract
Background
Acknowledging the role of inflammation in colorectal carcinogenesis, this study aimed to evaluate the associations between diet-associated inflammation, as measured by the energy-adjusted dietary inflammatory index (E-DIITM), and distinct stages of colorectal carcinogenesis.
Methods
The Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial enrolled participants without a colorectal cancer history, who were asked to complete baseline questionnaires and food frequency questionnaires. To estimate the associations between the E-DII and risks of newly incident colorectal adenoma, recurrent adenoma, and colorectal cancer, multivariable-adjusted Cox proportional hazards regression models were employed.
Results
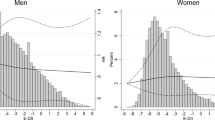
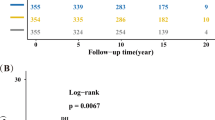
Among 101,680 participants, with an average age of 65 years, a total of 1177 incident colorectal adenoma cases, 895 recurrent adenoma cases and 1100 colorectal cancer cases were identified. Higher E-DII scores from food and supplement (HRQ5 vs Q1: 0.86 [0.69–1.06], Ptrend: 0.27) or from food only (HRQ5 vs Q1: 0.82 [0.64–1.05], Ptrend: 0.06) were not associated with higher risks of incident adenoma. However, the elevated risk of recurrent adenoma was found in the highest category of E-DII from food plus supplement (HRQ5 vs Q1: 1.63 [1.28–2.03], Ptrend: < 0.001) when compared with the lowest category. A significant association between colorectal cancer risk and E-DII from food plus supplement (HRQ5 vs Q1: 1.34 [1.09–1.65], Ptrend: 0.009) was found, where this association was only pronounced in distal colorectal cancer.
Conclusion
Higher E-DII scores from diet plus supplement but not from diet only were associated with a higher risk of recurrent adenoma and distal colorectal cancer. The role of nutrient supplements on cancer risk, especially when combined with diet, needs to be elucidated in future studies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Clinical and supplemental data that support the findings of this study have been deposited at https://biometry.nci.nih.gov/cdas/plco/. The PLCO trial has the following five registration numbers: NCT00002540 (Prostate), NCT01696968 (Lung), NCT01696981 (Colorectal), NCT01696994 (Ovarian) and NCT00339495 (EEMS) on ClinicalTrials.gov. This study had registered in Cancer Data Access System and had been approved.
References
GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–71.
Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer. 2010;46:765–81.
Strum WB. Colorectal adenomas. N. Engl J Med. 2016;374:1065–75.
Bedenne L, Faivre J, Boutron MC, Piard F, Cauvin JM, Hillon P. Adenoma−carcinoma sequence or “de novo” carcinogenesis? A study of adenomatous remnants in a population-based series of large bowel cancers. Cancer. 1992;69:883–8.
Brenner H, Kloor M, Pox CP. Colorectal cancer. Lancet. 2014;383:1490–502.
Kim SE, Paik HY, Yoon H, Lee JE, Kim N, Sung MK. Sex- and gender-specific disparities in colorectal cancer risk. World J Gastroenterol. 2015;21:5167–75.
Taylor DP, Burt RW, Williams MS, Haug PJ, Cannon-Albright LA. Population-based family history-specific risks for colorectal cancer: a constellation approach. Gastroenterology. 2010;138:877–85.
Lasry A, Zinger A, Ben-Neriah Y. Inflammatory networks underlying colorectal cancer. Nat Immunol. 2016;17:230–40.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–7.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883–99.
Santos S, Oliveira A, Lopes C. Systematic review of saturated fatty acids on inflammation and circulating levels of adipokines. Nutr Res. 2013;33:687–95.
Bordoni A, Danesi F, Dardevet D, Dupont D, Fernandez AS, Gille D, et al. Dairy products and inflammation: a review of the clinical evidence. Crit Rev food Sci Nutr. 2017;57:2497–525.
Barbaresko J, Koch M, Schulze MB, Nöthlings U. Dietary pattern analysis and biomarkers of low-grade inflammation: a systematic literature review. Nutr Rev. 2013;71:511–27.
Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444:860–7.
Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public health Nutr. 2014;17:1689–96.
Rafiee P, Shivappa N, Hébert JR, Nasab SJ, Bahrami A, Hekmatdoost A, et al. Dietary inflammatory index and odds of colorectal cancer and colorectal adenomatous polyps in a case-control study from Iran. Nutrients. 2019;11:1213.
Haslam A, Wagner Robb S, Hébert JR, Huang H, Wirth MD, Shivappa N, et al. The association between Dietary Inflammatory Index scores and the prevalence of colorectal adenoma. Public health Nutr. 2017;20:1609–16.
Sardo Molmenti CL, Steck SE, Thomson CA, Hibler EA, Yang J, Shivappa N, et al. Dietary inflammatory index and risk of colorectal adenoma recurrence: a pooled analysis. Nutr Cancer. 2017;69:238–47.
Shivappa N, Godos J, Hébert JR, Wirth MD, Piuri G, Speciani AF, et al. Dietary inflammatory index and colorectal cancer risk-a meta-analysis. Nutrients. 2017;9:1043.
Sánchez-Alcoholado L, Ramos-Molina B, Otero A, Laborda-Illanes A, Ordóñez R, Medina JA, et al. The role of the gut microbiome in colorectal cancer development and therapy response. Cancers. 2020;12:1406.
Vipperla K, O’Keefe SJ. Diet, microbiota, and dysbiosis: a ‘recipe’ for colorectal cancer. Food Funct. 2016;7:1731–40.
Zhang Y, Yu X, Yu E, Wang N, Cai Q, Shuai Q, et al. Changes in gut microbiota and plasma inflammatory factors across the stages of colorectal tumorigenesis: a case-control study. BMC Microbiol. 2018;18:92.
Prorok PC, Andriole GL, Bresalier RS, Buys SS, Chia D, Crawford ED, et al. Design of the prostate, lung, colorectal and ovarian (PLCO) cancer screening trial. Control Clin Trials. 2000;21:273s–309s.
Schoen RE, Pinsky PF, Weissfeld JL, Yokochi LA, Church T, Laiyemo AO, et al. Colorectal-cancer incidence and mortality with screening flexible sigmoidoscopy. N. Engl J Med. 2012;366:2345–57.
Kitahara CM, Berndt SI, de González AB, Coleman HG, Schoen RE, Hayes RB, et al. Prospective investigation of body mass index, colorectal adenoma, and colorectal cancer in the prostate, lung, colorectal, and ovarian cancer screening trial. J Clin Oncol. 2013;31:2450–9.
Subar AF, Thompson FE, Kipnis V, Midthune D, Hurwitz P, McNutt S, et al. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: the Eating at America’s Table Study. Am J Epidemiol. 2001;154:1089–99.
Subar AF, Ziegler RG, Thompson FE, Johnson CC, Weissfeld JL, Reding D, et al. Is shorter always better? Relative importance of questionnaire length and cognitive ease on response rates and data quality for two dietary questionnaires. Am J Epidemiol. 2001;153:404–9.
Rothman KJ, Greenland S, Lash TL. Introduction to stratified analysis. In: Modern epidemiology, introduction to stratifies analysis. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008. p. 261–3.
Tahir MR, Tran QX, Nikulin MS. Comparison of hypertabastic survival model with other unimodal hazard rate functions using a goodness-of-fit test. Stat Med. 2017;36:1936–45.
Yuan F, Deng L, Sun X, Chen Z, Shivappa N, Sheth AK, et al. Dietary inflammatory index and risk of colorectal adenoma: effect measure modification by race, nonsteroidal anti-inflammatory drugs, cigarette smoking and body mass index? Cancer Causes Control: CCC. 2021;32:837–47.
Obón-Santacana M, Romaguera D, Gracia-Lavedan E, Molinuevo A, Molina-Montes E, Shivappa N, et al. Dietary inflammatory index, dietary non-enzymatic antioxidant capacity, and colorectal and breast cancer risk (MCC-Spain Study). Nutrients. 2019;11:1406.
Wirth MD, Shivappa N, Steck SE, Hurley TG, Hébert JR. The dietary inflammatory index is associated with colorectal cancer in the National Institutes of Health-American Association of Retired Persons Diet and Health Study. Br J Nutr. 2015;113:1819–27.
Shivappa N, Zucchetto A, Montella M, Serraino D, Steck SE, La Vecchia C, et al. Inflammatory potential of diet and risk of colorectal cancer: a case-control study from Italy. Br J Nutr. 2015;114:152–8.
Sharma I, Zhu Y, Woodrow JR, Mulay S, Parfrey PS, McLaughlin JR, et al. Inflammatory diet and risk for colorectal cancer: a population-based case-control study in Newfoundland, Canada. Nutrition. 2017;42:69–74.
Harmon BE, Wirth MD, Boushey CJ, Wilkens LR, Draluck E, Shivappa N, et al. The dietary inflammatory index is associated with colorectal cancer risk in the multiethnic cohort. J Nutr. 2017;147:430–8.
Cho YA, Lee J, Oh JH, Shin A, Kim J. Dietary inflammatory index and risk of colorectal cancer: a case-control study in Korea. Nutrients. 2016;8:469.
Bailey RL, Gahche JJ, Miller PE, Thomas PR, Dwyer JT. Why US adults use dietary supplements. JAMA Intern Med. 2013;173:355–61.
Mulholland CA, Benford DJ. What is known about the safety of multivitamin-multimineral supplements for the generally healthy population? Theoretical basis for harm. Am J Clin Nutr. 2007;85:318s–322s.
Ronis MJJ, Pedersen KB, Watt J. Adverse effects of nutraceuticals and dietary supplements. Annu Rev Pharm Toxicol. 2018;58:583–601.
Ashmore JH, Lesko SM, Miller PE, Cross AJ, Muscat JE, Zhu J, et al. Association of dietary and supplemental iron and colorectal cancer in a population-based study. Eur J Cancer Prev. 2013;22:506–11.
Oliai Araghi S, Kiefte-de Jong JC, van Dijk SC, Swart KMA, van Laarhoven HW, van Schoor NM, et al. Folic acid and vitamin B12 supplementation and the risk of cancer: long-term follow-up of the B vitamins for the prevention of osteoporotic fractures (B-PROOF) trial. Cancer Epidemiol, Biomark Prev. 2019;28:275–82.
Bairati I, Meyer F, Gélinas M, Fortin A, Nabid A, Brochet F, et al. Randomized trial of antioxidant vitamins to prevent acute adverse effects of radiation therapy in head and neck cancer patients. J Clin Oncol. 2005;23:5805–13.
Omenn GS, Goodman GE, Thornquist MD, Balmes J, Cullen MR, Glass A, et al. Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N. Engl J Med. 1996;334:1150–5.
Alpha-Tocopherol, Beta Carotene Cancer Prevention Study Group. The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N. Engl J Med. 1994;330:1029–35.
Glebov OK, Rodriguez LM, Nakahara K, Jenkins J, Cliatt J, Humbyrd CJ, et al. Distinguishing right from left colon by the pattern of gene expression. Cancer Epidemiol, Biomark Prev. 2003;12:755–62.
Zamora-Ros R, Shivappa N, Steck SE, Canzian F, Landi S, Alonso MH, et al. Dietary inflammatory index and inflammatory gene interactions in relation to colorectal cancer risk in the Bellvitge colorectal cancer case-control study. Genes Nutr. 2015;10:447.
Tabung FK, Steck SE, Ma Y, Liese AD, Zhang J, Caan B, et al. The association between dietary inflammatory index and risk of colorectal cancer among postmenopausal women: results from the Women’s Health Initiative. Cancer Causes Control: CCC. 2015;26:399–408.
Gualco G, Reissenweber N, Cliché I, Bacchi CE. Flat elevated lesions of the colon and rectum: a spectrum of neoplastic and nonneoplastic entities. Ann diagnostic Pathol. 2006;10:333–8.
Nawa T, Kato J, Kawamoto H, Okada H, Yamamoto H, Kohno H, et al. Differences between right- and left-sided colon cancer in patient characteristics, cancer morphology and histology. J Gastroenterol Hepatol. 2008;23:418–23.
Haggar FA, Boushey RP. Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg. 2009;22:191–7.
Festa A, D’Agostino R Jr., Howard G, Mykkänen L, Tracy RP, Haffner SM. Chronic subclinical inflammation as part of the insulin resistance syndrome: the Insulin Resistance Atherosclerosis Study (IRAS). Circulation. 2000;102:42–47.
Bruce WR, Giacca A, Medline A. Possible mechanisms relating diet and risk of colon cancer. Cancer Epidemiol, Biomark Prev. 2000;9:1271–9.
Grosso G, Godos J, Lamuela-Raventos R, Ray S, Micek A, Pajak A, et al. A comprehensive meta-analysis on dietary flavonoid and lignan intake and cancer risk: Level of evidence and limitations. Mol Nutr Food Res. 2017;61:1600930.
Gilsing AM, Fransen F, de Kok TM, Goldbohm AR, Schouten LJ, de Bruïne AP, et al. Dietary heme iron and the risk of colorectal cancer with specific mutations in KRAS and APC. Carcinogenesis. 2013;34:2757–66.
Zhu Y, Wang PP, Zhao J, Green R, Sun Z, Roebothan B, et al. Dietary N-nitroso compounds and risk of colorectal cancer: a case-control study in Newfoundland and Labrador and Ontario, Canada. Br J Nutr. 2014;111:1109–17.
Diggs DL, Huderson AC, Harris KL, Myers JN, Banks LD, Rekhadevi PV, et al. Polycyclic aromatic hydrocarbons and digestive tract cancers: a perspective. J Environ Sci Health Part C, Environ Carcinogenesis Ecotoxicol Rev. 2011;29:324–57.
Dvorak HF. Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N. Engl J Med. 1986;315:1650–9.
Gao R, Davis A, McDonald TO, Sei E, Shi X, Wang Y, et al. Punctuated copy number evolution and clonal stasis in triple-negative breast cancer. Nat Genet. 2016;48:1119–30.
Cross W, Kovac M, Mustonen V, Temko D, Davis H, Baker AM, et al. The evolutionary landscape of colorectal tumorigenesis. Nat Ecol Evol. 2018;2:1661–72.
Shivappa N, Steck SE, Hurley TG, Hussey JR, Ma Y, Ockene IS, et al. A population-based dietary inflammatory index predicts levels of C-reactive protein in the Seasonal Variation of Blood Cholesterol Study (SEASONS). Public Health Nutr. 2014;17:1825–33.
Acknowledgements
Thanks to the National Cancer Institute for providing access to data collected by the Prostate, Lung, Colorectal, and Ovarian Cancer (PLCO) Cancer Screening Trial. The statements contained herein are solely those of the authors and do not represent or imply concurrence or endorsement by the National Cancer Institute.
Funding
No financial support was received.
Author information
Authors and Affiliations
Contributions
ZYL and XLJ conceived and designed the analysis. ZYL, HC and HL collected and processed the data. NS and JRH calculated E-DII scores. ZYL and KW performed the analysis. ZYL wrote the paper. ZYL, KW, JRH and XL.J revised the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. JRH owns controlling interest in Connecting Health Innovations LLC (CHI), a company that has licensed the right to his invention of the dietary inflammatory index (DII®) from the University of South Carolina in order to develop computer and smartphone applications for patient counselling and dietary intervention in clinical settings. Dr. NS is an employee of CHI. The subject matter of this paper will not have any direct bearing on that work, nor has that activity exerted any influence on this project. The remaining authors declare no competing interests.
Ethics approval and consent to participate
Institutional Review Board of the National Cancer Institute approved the study protocol of PLCO Cancer Screening Trial, and all participants provided a written informed consent.
Consent to publish
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Li, Z., Wang, K., Shivappa, N. et al. Inflammatory potential of diet and colorectal carcinogenesis: a prospective longitudinal cohort. Br J Cancer 126, 1735–1743 (2022). https://doi.org/10.1038/s41416-022-01731-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-01731-8