Abstract
Introduction Caries in the primary dentition affects around one-quarter of children in England. There is uncertainty and varying practice regarding the management of these children within NHS primary dental care. Silver diamine fluoride (SDF) is an approach that is not well-adopted nationally. This study aims to explore the factors affecting treatment choices for caries management in young children within primary dental care, including the use of SDF.
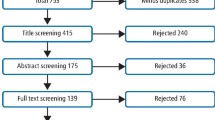
Methods Semi-structured interviews were carried out via video conferencing with general dental practitioners and therapists working in NHS primary care. The topic guide covered factors which influence the management of caries in primary teeth, with SDF-specific questions. These were transcribed verbatim and analysed using thematic analysis.
Results A total of 13 interviews were conducted with dental professionals working across Yorkshire and the East Midlands. Decision-making for caries management was dependent on inter-related factors, which also influenced SDF use. Treatment decisions were taken on a case-by-case basis, but were influenced by the child, their parents, the dental professional and service factors, along with the clinical technique.
Conclusion Many individual- and system-level factors influence treatment decisions for early childhood caries. However, issues relating to remuneration and governance appear to be specific barriers to adoption of SDF in primary dental care.
Key points
-
Challenges to managing children with caries in the primary dentition are multi-factorial.
-
Management options must be appropriately remunerated to support their implementation.
-
Clinical recommendations must be designed in such a way as to be amenable for use in this young population by the dental professionals carrying out the work.
Similar content being viewed by others
Introduction
Caries in the primary dentition affects a large proportion of young children nationally. The most recent national health survey suggests that around one-quarter of five-year-olds in England have obvious caries experience in the primary dentition.1 Despite evidence-based preventive regimes and treatment options, tens of thousands of children still undergo general anaesthesia (GA) for dental extractions each year.2,3 The majority of these extractions are as a consequence of dental caries.2
Uncertainty and disparity remains regarding the management of caries in primary care, with a variety of treatments being undertaken.4 This is despite the availability of evidence-based guidance.5 It is important to understand what factors influence practitioners' decision-making around the management of caries in the primary dentition and consider why this may be the case. Additionally, strategies to encourage successful management of caries in the primary dentition need to be considered. Silver diamine fluoride (SDF) is a topical treatment that has efficacy in arresting caries in the primary dentition (Fig. 1). Multiple systematic reviews have reported on its ability to arrest the progression of caries in primary teeth, with one performing a meta-analysis that demonstrated greater success rates than the atraumatic restorative technique or sodium fluoride varnish for this indication.6,7 Its use is routine in many countries around the world, but adoption is limited within the UK. It was licenced for use in the European Union through a CE mark in 2017. However, the specific use for caries arrest in children is off-label. There are limited data for the cost-effectiveness of SDF: the cost of the material itself is approximately ten times the cost of one application of sodium fluoride varnish. However, the greater effectiveness of SDF in caries arrest may offset the direct cost of the material.8 As such, it is important to consider how treatment alternatives to current options such as SDF could be used from the practitioners' perspective.
Dental appearance of a six-year-old child showing a range of treatment modalities previously provided for their carious primary teeth. SDF was used to arrest caries in their upper central primary incisors and performed metal crowns and extractions undertaken for the management of their carious primary molars
Aim
This study aimed to explore the factors affecting the management of caries for young children in primary dental care.
Objectives
-
1.
To use semi-structured interviews to explore the challenges of treating children with dental caries affecting their primary teeth in general dental practice
-
2.
To explore the attitudes of dental professionals towards the use of SDF.
Method
Ethical approval was received by the Central Bristol NHS Research Ethics Committee (approval reference: 21/SW/0018). All participants consented to take part in the research and have their data used for the purpose of this research.
The aim of the study was met through qualitative semi-structured interviews with dental professionals working in NHS general dental practice. The interviews were carried out in 2021. Interviews were undertaken virtually through video conferencing software. This decision was for pragmatic and feasibility reasons; however, it did support the ability to conduct the interviews in a place of the participant's own choosing (home or workplace). The researcher was in a private office. Only the audio was recorded using a digital voice recorder. Audio-recordings were then transcribed verbatim by LT, or professional dictation services.
Participants were dental professionals working in the NHS in South Yorkshire and the East Midlands. Purposive sampling was used to include those working under different contracts, across areas within the regions and within various practice sizes. The professionals had a range of levels of experience and included dental therapists and general dental practitioners (both associates and practice owners).
Participants were recruited through professional networks and contacts. The initial invitation was by email through contact lists of local dental committees, primary care research networks and tutors working in general practice associated with the University of Sheffield. It is not possible to ascertain the number of potentially eligible participants that were invited, owing to many professionals on the mailing lists not delivering NHS treatment. The consent form was sent electronically for participants to complete and return via email. Subsequently, a video call was arranged. Consent was taken or reaffirmed at the start of the interview.
Semi-structured interviews were conducted and followed a topic guide informed by the literature. This was piloted and explored experiences of treating children with caries in the primary dentition in primary dental care. Other topics discussed included participants' specific views on SDF treatment and what factors influenced their decision-making. Data analysis was through thematic analysis by LT.9 Interviews continued until data saturation.
Results
In total, 13 interviews were completed. The interviews lasted approximately 10-30 minutes. The practices were based across Yorkshire and the East Midlands and all had an NHS component. Both dentists and a dental therapist were interviewed (practice owner: n = 1; foundation dentist: n = 1; associates: n = 10).
Decision-making for caries management was dependent on inter-related factors, which also influenced the use of SDF in practice. Treatment decisions were taken on a case-by-case basis, but were influenced by the child, their parents, the dental professional and service provision/the practice environment, along with the clinical technique, as described below.
Patient factors
The patient factors were salient in terms of informing the dental professional's approach to caries management. The child's perceived ability to co-operate with their treatment was fundamental; practitioners reported this as being dependent on the child's age. For example, if the dental professional did not feel they would have the ability to carry out the technical aspects required for an option to be successful, they would not use this treatment. Examples cited were local anaesthesia (LA) for caries removal or moisture isolation for adhesive restorations. The dental professionals also considered the child's previous experience of treatment when evaluating management options:
-
'If they're a bit young and they're not co-operating that well, I think complete caries removal might need LA, but they're not going to cope with that' (P4, associate dentist).
The clinical presentation was also pertinent. This included the extent of caries in terms of whether the caries was an early or advanced lesion, if there was pain or infection, whether there were multiple teeth affected, and if the lesion was active. Furthermore, the child's caries risk status, following preventive interventions, was also an important element, as it determined the likelihood of success of different options:
-
'I will generally consider referring for GA if there's multiple carious teeth plus pain or sepsis […] if they've got one small lesion I'd be more tempted to manage it preventatively...' (P8, associate dentist).
The clinical presentation was also related to the position of the tooth and whether there were any aesthetic concerns. Another consideration was whether the tooth was close to exfoliation due to the patient's age.
Patient wishes were considered, as were the experiences of the patient's siblings. The child-dentist/therapist relationship was relevant to considering the child's views, ability to implement behaviour management techniques and effective information sharing with the child.
Parental influences
The parental influences included parental attitudes towards the need to manage the child's primary teeth and their attitude towards GA. Parents' attitudes towards LA and extractions were also relevant, as some thought their child would be anxious about these elements of treatment and therefore wished to avoid them. Some dental professionals felt that parental communication and anxiety influenced the cooperation of the child:
-
'...there's a number of parents that I see who won't […] don't want their children's teeth taken out. Probably the only way they would manage it is a GA, and they don't want that. So, for them, I think it [SDF] would be a really good treatment option' (P3, associate dentist).
Dental professionals perceived that parents can struggle to adopt prevention advice and bring their children to appointments and this influenced their treatment choices:
-
'Health literacy of the family […] are they going to be able to support what we're doing at home?' (P2, dental therapist)
-
'I will be honest, I know I probably should do more Hall crowns and things like that. A lot of parents are like "no we've got them out of school can you just sort it now" […] so you end up doing a GIC [glass ionomer cement]' (P9, associate dentist).
Parental understanding and information sharing about different treatment options was important, as was the communication between parents and dental professionals. Their relationship with the family was relevant. There was discussion of parental attitude towards aesthetics depending on the clinical situation and the proposed treatment option, such as preformed metal crowns and SDF. However, there were different reports of this, with some participants considering it a potential barrier and some not finding this as an issue in their experience:
-
'Touch wood we've not had any issues at the moment. I know that there's a discolouration issue [from SDF use], but the patients haven't complained and we've probably used it on 20 children and no, no real big issues with parents regarding it at the moment' (P12, practice owner).
Dental professional
There were multiple factors relating to the dental professional themselves that affected how they managed children with caries in the primary dentition.
The dental professionals' experience was a prominent factor - their experience generally and specifically with a certain technique. This affected their confidence with the technique and their willingness to use it. In some instances, it was recognised that there was a better approach in terms of efficacy, but they were not confident in using it so chose an alternative:
-
'Well, evidence wise, I'd prefer to do stainless steel crowns, but I'm not that comfortable with them […] direct restorations I do all the time […] so that's why I lean towards that, even though they don't work' (P1, associate dentist).
The participants' knowledge of different techniques was important, which was influenced by their training, both as an undergraduate and continuing professional development. A supportive environment with the opportunity to learn was pertinent, enabling the use of new techniques. National bodies such as Health Education England were seen as appropriate to provide training to qualified practitioners:
-
'I know that we tend to kind of use what we were taught at dental school to be honest […] what we're used to using when we first qualify' (P10, associate dentist).
Their personal philosophy to treatment planning was an overarching influence, which was also affected by the approach adopted within the practice. Additionally, dental care professionals' approaches to change and adoption of new ideas was a key factor; the first quote below discusses the adoption of SDF:
-
'I would also guess that professional scepticism, does that make sense? I don't know that many clinicians would sort of take to it straight off the bat in the same way that […] because we're so used to conventional restorations' (P8, associate dentist)
-
'We probably go along the biological management approach more…' (P12, practice owner).
Service provision
The practice environment and provision of service affected participants' treatment choices. The contract was particularly pertinent to this. The current contractual arrangement in England is to provide remuneration through units of dental activity (UDA). The UDA system was described as influential over treatment choice, that treatments need to be remunerated appropriately, and that they felt the UDA system was not congruent with this. The contract influenced the time available for appointments, which then determined the number of appointments available to carry out a treatment:
-
'You just don't have the time to keep bringing them back, bringing them back' (P2, dental therapist)
-
'That's so much time for just three UDAs, you shouldn't think like that, but that is sometimes how you have to think about it on the NHS' (P13, foundation dentist)
-
'I know this is awful, but it is financially a better option because it's [glass ionomer cement] quicker, it's less like […] you can obviously put a GIC in quickly in most situations. The crown, obviously […] more often than not you're gonna [sic] have to do the spacers and then get them back […] but I think realistically, and I know that is awful, erm, but financially, I don't think you're rewarded enough for Hall crowns' (P9, associate dentist)
-
'Probably UDAs wise, if you're doing it on one course of treatment I think you can get three UDAs, but that's whether you do, like, one filling as you know, or five crowns, two restorations, obviously fissure sealants which are only band one, so yeah, that's a bit of, you're not really rewarded for doing anything better, because obviously if you're doing stainless steel crowns then you'll need two appointments' (P1, associate dentist).
Specific practice pressures and the overall patient cohort were factors that affected treatment. Treatments that were of short duration and did not require multiple appointments were preferable due to the scant resource of appointment time. Participants considered the cost of treating some children meant there was reduced time to treat others:
-
'To put them on a three-month recall means that there are other children we are pushing on to a six-, seven-, eight-, nine-month recall. And it's trying to get a balance between seeing the kids we really, really need to see and doing the things we really need to be doing…' (P6, associate dentist).
The availability of products nationally and within the practice was a key barrier or facilitator. Relevant to this was the participant's job role within the practice and the practice attitude to new products and treatment philosophy. In particular, the attitude of the gatekeeper for ordering materials and their priorities were influential. Professionals had to justify the need for a treatment choice, with characteristics such as cost taken into consideration and compared to other materials. With respect to SDF specifically, clarity about licensing and cost implications were highlighted as issues:
-
'Money because we don't get paid to use it. So, it costs a lot of money and I don't get any form of remuneration from it at all [...] the shelf life on it was quite short as well, so if I manage to persuade my principal to buy it for me, and then the shelf life runs out, then it's just not going to work. I think for all these things […] it's the same as Hall crowns, you know, especially if there's an added cost to the practice, you know, people are more than happy to do them but it's not a charity and you need to be paid for it' (P6, associate dentist).
Clinical treatment
A number of factors, inherent to each different clinical modality, were cited as influencing treatment planning. Participants considered the patient experience to be a deciding factor. This was related to whether the technique needed LA, the side effects of treatment, such as discolouration or aesthetics, and if the use of a handpiece is required. Positive attributes that led to the choice of a particular option were if it was less invasive, there was less time for the patient in a chair, and if it was perceived to be less traumatic for the child:
-
'Yeah, I will be honest, majority is GIC because it's one visit and it's done, erm, and it's a bit easier to manage for the kids, but I know, that is probably not the most ideal' (P9, associate dentist).
The expected success of the treatment was important, both in terms of the known evidence base and through the experience of the practitioners themselves or their peers. The usefulness of the treatment for a wider patient group rather than for a sole individual was considered, as well as the availability of any patient information resources:
-
'I think that the videos that BSPD [British Society of Paediatric Dentistry] have done are really, really, really useful. And the [...] obviously having a leaflet to be able to give to patients at the same time that explains everything would be really helpful' (P5, associate dentist).
Reflexivity
One researcher (LT) designed and conducted the interviews and analysed the data. The final analysis was discussed and agreed upon by the research team. LT is a dentist working in paediatric specialist services with an interest on the topic. A reflexive stance was taken and the linking of the factors to the raw data was carried out to mitigate this. The topic guide was viewed by other research team members ahead of the interviews for additional perspectives. Some participants had previously reviewed some training resources on SDF, produced by LT, which had the potential to impact on how they discussed SDF in their interviews.
Discussion
This study demonstrates that there are a wide variety of factors that influence how dental professionals manage caries in young children in an NHS practice setting, in terms of both traditional techniques and newer modalities, such as SDF. Some of these factors, namely caries status and caries risk of the participant; training; practice environment; and colleague influence, have also been identified as influencing the choices made by dentists working in primary care settings in Germany, USA and New Zealand.10
Within this study, participants discussed using treatments which are not recognised as having the most successful outcomes. Delivery of treatment that does not follow best practice clinical guidelines has been previously demonstrated in the literature and remains a topic of debate in the dental arena.11 There are multiple reasons for this, as identified in this present study; notably, there are circumstances particularly with young children where recommended treatment options or those with the best evidence base may not be possible. This may be due to patient factors, such as ability to co-operate, lack of consent, or system factors. Participants described using GIC restorations despite knowing they are less successful than evidence-based alternatives. This finding is in keeping with clinical studies, carried out in primary dental care, that also highlighted the common adoption of this approach.4,12
There is acknowledgement in the literature that failure to follow clinical guidelines is not a UK-only phenomenon and that internationally, despite the evidence base for minimally invasive dentistry, many colleagues opt for more invasive caries management techniques.11 This highlights the importance of not only creating an evidence base, but considering how this evidence may translate into everyday clinical practice; the need for intervention implementation must be considered and explored.13 Furthermore, it was no surprise that the present research revealed how participants' clinical choices and activity were affected by the NHS contract and remuneration arrangements. This relationship appeared to be based on multiple factors, including time, number of visits and cost of materials weighed up against the remuneration provided. Although this is not a novel finding, as previous research has clearly demonstrated that contractual changes can affect clinical activity, it is one that warrants greater consideration.14,15,16
Relevant training and familiarity of technique are mentioned as relevant to treatment choice and given SDF has been only fairly recently introduced to the UK, this would contribute to its relatively poor adoption. Similarly, there is a paucity of health economic evaluations. As such, further investigation is required into how SDF is remunerated and its cost-effectiveness as a treatment in the NHS.
A strength of this study was that it involved participants from different practices and regions. The perspectives of both dentists and a dental therapist were gained. This led to insights particularly related to SDF from a primary care viewpoint. Notwithstanding this, the aim was to explore decision-making factors rather than provide generalisable results to all practitioners across the region.
Virtual interviews were used through video conferencing software, which was not without limitations. On some occasions, there were technical difficulties owing to poor internet connections. This limited the natural cadence of conversation and introduced some stilted discussion and overlap, which may have affected the data quality.
These findings have important relevance in the wider debate of how to implement the most effective interventions for managing childhood caries in primary care. Clinical recommendations must be designed in such a way as to be amenable for use in this young population by the practitioners carrying out the work within the setting required. Ultimately, the use of evidence-based and minimally invasive treatments for children must be supported by an appropriate remuneration system.
Conclusion
For treatment options for caries management to be implemented in primary dental care, including SDF, multiple factors must be considered, which range from individual- to system-level factors, including remuneration and governance level.
References
UK Government. National Dental Epidemiology Programme for England: oral health survey of 5-year-olds 2019. 2020. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/873492/NDEP_for_England_OH_Survey_5yr_2019_v1.0.pdf (accessed August 2023).
Levine R S. Childhood caries and hospital admissions in England: a reflection on preventive strategies. Br Dent J 2021; 230: 611-616.
NHS Digital. 3.7.ii: Tooth extractions due to decay for children admitted as inpatients to hospital, aged 10 years and under. 2020. Available at https://digital.nhs.uk/data-and-information/publications/statistical/nhs-outcomes-framework/february-2020/domain-3-helping-people-to-recover-from-episodes-of-ill-health-or-following-injury-nof/3-7-ii-tooth-extractions-due-to-decay-for-children-admitted-as-inpatients-to-hospital-aged-10-years-and-under (accessed August 2023).
Harford S, Sharpling J, Williams C, Northover R, Power R, Brown N. Guidelines relevant to paediatric dentistry - do foundation dentists and general dental practitioners follow them? Part 2: Treatment and recall. Br Dent J 2018; 224: 803-808.
Scottish Dental Clinical Effectiveness Programme. Prevention and Management of Dental Caries in Children. 2018. Available at https://www.sdcep.org.uk/media/2zbkrdkg/sdcep-prevention-and-management-of-dental-caries-in-children-2nd-edition.pdf (accessed August 2023).
Seifo N, Cassie H, Radford J R, Innes N P. Silver diamine fluoride for managing carious lesions: an umbrella review. BMC Oral Health 2019; 19: 145.
Chibinski A C, Wambier L M, Feltrin J, Loguercio A D, Wambier D S, Reis A. Silver Diamine Fluoride Has Efficacy in Controlling Caries Progression in Primary Teeth: A Systematic Review and Meta-Analysis. Caries Res 2017; 51: 527-541.
Timms L, Sumner O, Deery C, Rogers H J. Everyone else is using it, so why isn't the UK? Silver diamine fluoride for children and young people. Community Dent Health 2020; 37: 143-149.
Clarke V, Braun V, Hayfield N. Thematic analysis. In Smith J A (ed) Qualitative Psychology: A Practical Guide to Research Methods. pp 222-248. London: SAGE, 2015.
Schwendicke F, Foster Page L A, Smith A L, Fontana M, Thomson W M, Baker S R. To fill or not to fill: a qualitative cross-country study on dentists' decisions in managing non-cavitated proximal caries lesions. Implement Sci 2018; 13: 54.
Innes N P, Frencken J E, Schwendicke F. Don't Know, Can't Do, Won't Change: Barriers to Moving Knowledge to Action in Managing the Carious Lesion. J Dent Res 2016; 95: 485-486.
Maguire A, Clarkson J E, Douglas G V et al. Best-practice prevention alone or with conventional or biological caries management for 3- to 7-year-olds: the FiCTION three-arm RCT. Health Technol Assess 2020; 24: 1-174.
Schwendicke F, Doméjean S, Ricketts D, Peters M.Managing caries: the need to close the gap between the evidence base and current practice. Br Dent J 2015; 219: 433-438.
Hill H, Howarth E, Walsh T, Tickle M, Birch S, Brocklehurst P. The impact of changing provider remuneration on clinical activity and quality of care: Evaluation of a pilot NHS contract in Northern Ireland. Community Dent Oral Epidemiol 2020; 48: 395-401.
Tickle M, Macdonald R, Franklin J, Aggarwal V R, Milsom K, Reeves D. Paying for the wrong kind of performance? Financial incentives and behaviour changes in National Health Service dentistry 1992-2009. Community Dent Oral Epidemiol 2011; 39: 465-473.
Davies B J, Macfarlane F. Clinical decision making by dentists working in the NHS General Dental Services since April 2006. Br Dent J 2010; DOI: 10.1038/sj.bdj.2010.1080.
Acknowledgements
The authors wish to acknowledge all the participants for providing their time to take part in this research.
Author information
Authors and Affiliations
Contributions
Laura Timms: study design, collected and analysed data, drafted and revised the manuscript. Helen Rodd, Paul Brocklehurst and Chris Deery: study design, reviewed findings and revised and contributed to the manuscript. Zoe Marshman: study design, supervised the data analysis, reviewed findings and revised the manuscript.
Corresponding author
Ethics declarations
Laura Timms has received funding from the RCS England FDS, British Society of Paediatric Dentistry and the National Institute of Health and Care Research (Doctoral Fellowship; funding ID: NIHR301740) for separate projects involving research considering child and parent perspectives on SDF, and research into using SDF in primary care. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. Funding was not received for this study.
Ethical approval was received by the Central Bristol NHS Research Ethics Committee (approval reference: 21/SW/0018). All participants consented to take part in the research and have their data used for the purpose of this research.
Data availability: not applicable.
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0.© The Author(s) 2023
About this article
Cite this article
Timms, L., Rodd, H., Deery, C. et al. 'You just don't have the time to keep bringing them back, bringing them back': the experience of primary care dental professionals in England when treating young children with carious teeth. Br Dent J (2023). https://doi.org/10.1038/s41415-023-6229-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-023-6229-3