Abstract
Introduction National surveys of the oral health of adults are conducted decennially. For reasons of feasibility and cost, these only provide accurate information at large geographical areas. To address this, a survey of adults attending dental practices in England was undertaken.
Aim To describe and discuss the survey method and findings.
Method A clinical examination and questionnaire survey was conducted in a sample of English dental practices.
Results Questionnaires (n = 16,572) and clinical examinations (n = 14,270) were completed with patients from 1,173 dental practices. Poorer oral health disproportionately affected older adults and those from more socioeconomically deprived areas. Over one in three from more deprived areas had untreated caries compared with one in five in the less deprived (36.2% vs 19.9%) and impacts of oral problems were nearly three times higher in the more deprived areas (27.9% vs 11.0%). Of those receiving NHS care, 28.7% and 46.2% reported they would struggle/be unable to pay a Band 2 and Band 3 NHS patient charge, respectively.
Conclusion It is feasible to undertake a survey of adults in dental practices but care must be taken generalising the findings to the general population and comparing them with other surveys undertaken using different methods.
Key points
-
Describes and discusses the method and results of a survey of adults undertaken in dental practices in England.
-
Poorer oral health disproportionately affected older participants and those from more socioeconomically deprived areas. Those with the highest need were least able to afford care.
-
Surveys can be undertaken in dental practices, but the results should be interpreted with caution, especially when comparing them with those from surveys undertaken using different methods.
Similar content being viewed by others
Introduction
In the UK, there has been a national decennial programme to survey adult oral health since the 1960s.1,2,3,4,5,6 These surveys have provided information on the oral health of adults over time and identified changes such as the increased retention of the natural dentition and the emergence of root caries as a public health problem. This information has been used to inform oral health needs assessments and workforce planning. However, for reasons of cost and feasibility of accessing large numbers of adults in their own homes, these surveys have been restricted to samples representative of populations from large geographical levels, with at least ten years between surveys. Consequently, there is a paucity of information on the oral health of adults to inform service planning, particularly at local levels, and the information that exists can be up to ten years old.
There are two main challenges when collecting adult oral health data. First, it is difficult to access large representative samples. Secondly, if dental examinations are included, these are often required outside of normal working hours in participants' homes, which adds technical difficulty, costs, and time required for data collection. An earlier study7 used a questionnaire survey to capture self-assessed oral health of adults in part to address these difficulties. Although its findings were useful for primary care organisations in the region it covered, it was administratively and methodologically demanding and lacked the clinical data of the national surveys. Consequently, temporal and regional comparisons were not possible.
Another possible approach would be to undertake a survey in dental practices. Such an approach was used in Scotland to survey adults who were aged 45 and over.8 In England, in 2018/19, approximately 50.0% of the adult population had accessed NHS primary dental care over a two-year period.9 Many others attend private practices.10 Therefore, it should be possible to select a large, representative sample of participants of all ages of adults from dental practices and to undertake an examination for the survey during a routine dental visit. Although not standardised, this would provide better examination conditions compared with 'field' conditions, where lighting and the participant's position may be less optimal. It should also be more convenient for participants.
Given the need for contemporary local oral health data, adults attending dental practices were selected as the survey population for the 2018 National dental epidemiology programme in England as a pragmatic way to obtain information on local oral health needs. The aim of this report is to describe and discuss the methods and findings of the survey.
Methods
A summary of the methods used is provided here and were based on the methods used in other National dental epidemiology programme surveys.11,12 A more detailed description of the methods is available in a separate publication.13
Survey population and sampling
The survey population was patients aged 16 years or over who were attending an appointment within an NHS, mixed or private general dental practice in England.
A pragmatic approach to sampling dental practices was taken to ensure that a large number of patients could be included in the survey within a limited time frame, with lower-tier local authorities (LAs) of England as the primary sampling unit. Size of practice was used as a proxy for levels of activity and it was assumed that larger practices were most likely to have an unoccupied surgery for use by the survey team. Therefore, a list of NHS, mixed and private dental practices within each LA area was compiled and ordered by size; purely specialist practices were excluded. No stratification other than LA area was used. Practices were contacted in listed order within each LA by the examining team. The method required them to recruit a minimum of ten practices and examine a minimum of 16 adults at each, producing a minimum sample size of 160. The trained examining teams attended each participating practice for the equivalent of a day.
Data collection
Fieldwork teams who had previously trained and calibrated for epidemiological surveys were commissioned by LAs or by NHS England on their behalf. Survey training on standardised protocols was conducted by the same training team across multiple sites before data collection. All adults attending for examination or treatment on survey days were invited to participate in completing a questionnaire, taking around five minutes, and to have a brief clinical examination, taking around ten minutes. Written consent was sought. Data were collected for the equivalent of one day at each participating practice.
Questionnaire
The 'adults in practice' questionnaire was developed in consultation with LAs and commissioners. It drew upon previously validated questions used in the Adult dental health survey 20096 and included questions on the following: oral health behaviours; oral health impacts; dental attendance; past experiences; and the impacts of NHS patient charges.
Clinical examination
A visual-only examination technique was used to measure the prevalence of severe untreated dental caries and gingival condition (bleeding on probing)14 was assessed using a standard Community Periodontal Index of Treatment Needs/Basic Periodontal Examination probe. Need for treatment was assessed, collated and reported as fitting within one of three NHS dental treatment bands.15 A Band 1 course of treatment includes examination, preventive treatment and advice, scale and polish and radiographs. A Band 2 course of treatment includes fillings, extractions, root canal therapy and periodontal therapy. A Band 3 course of treatment includes crowns, bridges and dentures. The highest band was recorded for each participant based on an assessment of their treatment need. The degree of urgency of treatment needs was also assessed.
Data processing
Data were entered into a Microsoft Access database. Following data cleaning, they were shared securely with the then Public Health England. The data were collated, cleaned and analysed using Microsoft Excel and Access and linked to population statistics. These included the Index of Multiple Deprivation 201516 of the area of the participant's residence. The 'least deprived' and 'most deprived' quintiles comprised those areas falling among the least or most deprived 20% in England. Confidence intervals were calculated using the Wilson score method for prevalence and the statistical significance level was set to p <0.05.
Ethical approval for the study was provided by the NHS Research Authority (Ref. 17/LO/1594).
Results
Questionnaire and clinical examination data were collected from 16,572 (65% of those approached) and 14,270 (56% of those approached) patients, respectively. This involved 1,173 dental practices (nearly all NHS: 25%; fully private: 10%; and mixed practices: 65%) from 107 of the 152 upper-tier and 212 of the 326 lower-tier LAs across England. Response rates varied geographically, being highest in the East Midlands (66.8%) and lowest in the East of England (34.5%).
Despite the survey being restricted to dental attendees, participant demographics were similar to that of the general population of England17 in terms of sex, age, ethnicity and socioeconomic deprivation of area of residence (data not presented but available in the full report).18
Only 0.9% of participants had none of their own teeth, 15.0% wore dentures (partial or full) and 10.0% had bridges or implants replacing missing teeth. The majority (81.9%) had 'functional dentitions' (comprising 21 or more natural teeth); however, nearly all (90.2%) had at least one filling (mean 7.2 fillings), and approximately half (46.5%) had at least one crowned tooth. Most (70.5%) were assessed as having a current treatment need. The proportion of participants with a functional dentition varied by age, but less so by ethnicity and area of residence deprivation (Fig. 1).
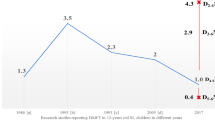
More than one-quarter (27.0%) had untreated dentinal caries, on average affecting 2.1 teeth. This varied by age and deprivation but not ethnicity. Those living in the most deprived areas were more likely to have untreated caries than those in the least (36.2% vs 19.9%) (Fig. 2).
Similar trends were seen in the proportion reporting oral pain (overall 18.3% reported currently being in pain) (Fig. 3), those who had experienced one or more impacts of poor oral health (overall 17.7% reported impacts 'fairly' or 'very often' in the previous year) (Fig. 4) and those who had identifiable pulpal, involvement, ulceration, fistula, and abscess (PUFA) conditions (overall 7.2%) (Fig. 5).
More than half (52.9%) had gingival bleeding on probing. Although this varied little by age and ethnicity, there was a socioeconomic gradient, and those who had last attended two or more years ago were more likely to have gingival bleeding than those that had attended more recently (60.9% vs 52.1%). Those with non-urgent and urgent treatment needs, also varied little by age and ethnicity, but there was also a socioeconomic gradient (data not presented but available in the full report).18
Most participants (83.6%) reported attending a dentist in the previous 12 months. For those who had not attended in the last two years (7.9%), the most common reasons were: 'no need to see the dentist/nothing wrong with my teeth/no natural teeth' (28.2%); 'afraid of the dentist/don't like seeing the dentist' (27.6%); and 'keep forgetting/haven't got round to it' (23.9%). Overall, 6.8% of participants reported a disability or long-term illness that limited their ability to attend. Unsurprisingly, the proportion reporting a disability increased by age and there was also a socioeconomic gradient (data not presented but available in the full report).18 The most common limitations to attendance were the inability to climb stairs (47.0%) and to sit in the dental chair (14.3%). A further 5.7% reported they were usually unable to leave their home.
Perceived barriers to dental care were explored by asking participants how difficult they thought it would be for their neighbours to access care. In total, 46% perceived they would have no problems accessing NHS care. Of those who perceived barriers (49.5%), the most commonly reported were: 'hardly any dentists accepting new NHS dentists' (52.9%); 'long waiting lists for care' (40.9%); and high costs of care (40.3%).
Overall, 52.2% of participants paid all NHS charges and 12.9% were fully exempt from charges (Table 1).
Of the 16.7% receiving solely private care, 34.7% had chosen to stay with their practice when it stopped providing NHS care, 25.9% perceived that private dental care was better and 14.9% indicated there were no dentists offering NHS care nearby.
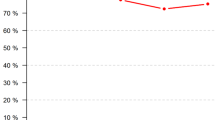
Participants receiving NHS care were asked if they could afford to pay Band 2 and 3 charges (£56 and £244, respectively, at the time of the survey). For Band 2 charges, 28.7% were unable or would struggle to pay. For Band 3 charges, 46.4% were unable or would struggle to pay. Unsurprisingly, the ability to pay followed a socioeconomic gradient (Fig. 6).
With regard to health behaviours and prevention, more than half (54.7%) reported they had never smoked and 14.0% were currently smoking. Most participants (71.2%) reported consuming alcohol on two days or fewer and 8.4% on five or more days of the preceding week. The majority had received preventive advice (89.5%) and this varied little by sex, ethnic group or area of deprivation (data not presented but available in the full report).18 Advice about oral hygiene was most frequently reported (80.2%) and advice about alcohol use the least (32.0%).
Discussion
This was the first large-scale dental health survey undertaken in dental practices in England which sampled all ages of adults. It identified a complex picture of oral health needs, with poorer oral health disproportionately affecting older adults and those from more socioeconomically deprived areas. Around two-thirds (67.8%) of participants aged 85 years and over did not have a functional dentition. One-in-three participants residing in more deprived areas had untreated dental caries compared with one in five in the less deprived (36.2% vs 19.9%), and reports of impacts from oral problems were nearly three times higher in those from more deprived areas (27.9% vs 11.0%). Of those attending NHS practices, over one-quarter (28.7%) and nearly one-half (46.2%) reported they would struggle or would be unable to pay a Band 2 and Band 3 charge, respectively. To compound this problem, there was a clear socioeconomic gradient, meaning that those likely to have higher needs were less likely to be able to afford some aspects of NHS treatment. Other common barriers to care included physical restrictions related to disabilities and the need for domiciliary care.
This survey has a number of strengths. Although the data are presented here in aggregate, given the large scale of the survey, more granular data (at the upper-tier LA level) are available for local analysis and for geographic comparison than has been previously available in UK adult oral health surveys. In addition, the dental examiners had been calibrated for recent earlier surveys and they received standardisation training for this. They were not re-calibrated for reasons of cost and feasibility of a central calibration exercise. Consistent with the findings of a Scottish survey of older adults undertaken in a similar way,9 the survey method and processes were feasible and acceptable to the majority of dental practices; a full evaluation has been undertaken to inform future surveys.19 As well as providing a snapshot of the oral health of adults attending dental practices, the data also provides a baseline for future surveys undertaken with the same method.
Yet, the limitations of the survey should be considered. For reasons of practicality and feasibility, neither the dental practices nor participants were randomly selected and clustering effects of sampling from whole dental practices were not accounted for in the analysis presented. Although the process was deemed acceptable by participating dental practices, some practices declined to host the survey and in others, patient participation was low. This may have also introduced bias and affected the ability to offer data at lower-tier LA levels. Nonetheless, the participation rates were 65.5% and 56.4% for the questionnaire and clinical examination, respectively, which compare favourably with other large-scale surveys.6,7 There is no agreed acceptable response rate. It is generally accepted that in large surveys, rates below 60% are suboptimal, but achieving higher rates while avoiding coercion can be challenging.20 However, the effect of any non-response bias should be considered. It is unknown whether those patients consenting to participate were systematically different from those who did not. Reasons for non-participation varied: reported barriers for dental practices included time and space and patients also cited time as a barrier.19
Although the sample was broadly representative of the general population, white people, women, those between 55-84 years, and those residing in the two least deprived areas were a little overrepresented. Furthermore, preferentially selecting larger practices may also have introduced sampling bias. Weighting of the data was not undertaken as there were too few data on dental practice populations to support this.18 In addition, with all other characteristics being equal, there may be differences between those who attend practices and those who do not, that impact the findings. For example, on average, participants could have had better oral health than the general population, as most were regular dental attenders. Conversely, participants were patients attending an appointment and so the prevalence of dental problems could be higher than in the population. There is a paucity of contemporary data on attendance patterns and their impact on oral health. However, the last decennial survey reported a tendency toward more people only seeking care when having dental problems and the oral health of regular, symptomatic and non-attenders was unpredictable.6 This survey may also underrepresent a proportion of the population for whom attending the dentist is unaffordable and/or perceived as unnecessary. For example, edentulous patients are likely to be underrepresented in the sample, as they tend to attend less frequently than the dentate,6 particularly those requiring social support.21
Notwithstanding these methodological concerns and their effects on generalisability, with few exceptions, the broad trends in the distribution of oral diseases and their impacts reflect those reported earlier6 and elsewhere in England,7 and smoking prevalence was similar to that reported in the GP patient survey undertaken at the same time (14.0% and 14.5%, respectively).22 However, detailed comparison of the findings, particularly temporally, would be inappropriate given important differences in the methods. As well as the survey population being different in this study, it was undertaken in a dental setting with more favourable, unstandardised lighting and participant positioning for the clinical examination compared with conditions in the field. This may have increased the likelihood of scoring for the disease elements in the clinical examination. Nonetheless, the caries data reported in this study will still underestimate the prevalence in the population, as the diagnostic threshold was set at the D3level (clinically obvious caries into dentine) and so earlier stages of the disease were not counted.
Conclusion
Overall, this survey of adult dental patients in England describes a population where nearly all have at least some natural teeth but where impacts and signs of dental disease are prevalent, even though the majority report attending a dentist annually. It highlights that the effects of poorer oral health disproportionately affect parts of this population, most notably, older patients and those living in the more deprived areas. This group also reports more difficulty affording some aspects of care. Finally, it demonstrates that surveys can be undertaken in dental practices, but care must be taken generalising the findings to the population and comparing the findings with other surveys undertaken differently.
References
Gray P G, Todd J E, Slack G L, Bulman J S. Adult Dental Health Survey in England and Wales in 1968. London: His Majesty's Stationery Office, 1970.
Todd J E, Walker A M. Adult Dental Health: England and Wales 1968-1978. Vol 1. London: His Majesty's Stationery Office, 1980.
Todd J E, Walker A M, Dodd P. Adult Dental Health: UK 1978. Vol 2. London: His Majesty's Stationery Office, 1982.
Todd J E, Walker A M, Dodd P. Adult Dental Health 1988: United Kingdom. London: His Majesty's Stationery Office, 1988.
Kelly M, Steele J, Nuttall N et al. Adult Dental Health Survey: Oral Health in the United Kingdom in 1998. London: The Stationary Office, 2000.
NHS Digital. Adult Dental Health Survey 2009. 2010. Available at https://digital.nhs.uk/data-and-information/publications/statistical/adult-dental-health-survey (accessed January 2022).
Marshman Z, Dyer T A, Wyborn C G, Beal J, Godson J H. The oral health of adults in Yorkshire and Humber 2008. Br Dent J 2010; DOI: 10.1038/sj.bdj.2010.819.
NHS National Services Scotland. Scottish Adult Oral Health Survey 2016-2018. 2019. Available at https://www.scottishdental.org/wp-content/uploads/2019/04/2019-04-30-SAOHS-Report.pdf (accessed January 2022).
NHS Digital. NHS Dental Statistics for England 2018-19, Annual Report. 2019. Available at https://digital.nhs.uk/data-and-information/publications/statistical/nhs-dental-statistics/2018-19-annual-report-pas# (accessed June 2022).
NHS England. GP Patient Survey Dental statistics. 2021. Available at https://www.england.nhs.uk/statistics/statistical-work-areas/gp-patient-survey/gpps-dental-statistics/ (accessed January 2022).
UK Government. Dental public health epidemiology programme: Oral health of five-year-olds children 2016-2017. 2016. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/774469/Oral_health_survey_protocol_5_year_olds_2016.pdf (accessed January 2022).
UK Government. Dental public health epidemiology programme: Oral health survey of older people, 2015-2016. 2015. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/773633/Older_people_oral_health_survey_protocol_2015.pdf (accessed January 2022).
UK Government. Dental public health epidemiology programme: Oral health survey of adults attending general dental practice 2017/18. 2017. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/773630/Oral_health_survey_protocol_adults_in_practice_2017.pdf (accessed January 2022).
Pitts N B, Evans D J, Pine C M. British Association for the Study of Community Dentistry (BASCD) diagnostic criteria for caries prevalence surveys - 1996/97. Community Dent Health 1997; 14: 6-9.
NHS UK. How much will I pay for dental treatment? 2021. Available at https://www.nhs.uk/nhs-services/dentists/dental-costs/how-much-will-i-pay-for-nhs-dental-treatment/ (accessed January 2022).
UK Government. English indices of deprivation 2015. 2015. Available at https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed January 2022).
Office for National Statistics. Population estimates. Available at https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates (accessed February 2022).
UK Government. National Dental Epidemiology Programme for England: Oral health survey of adults attending general dental practices 2018. 2020. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/891208/AiP_survey_for_England_2018.pdf (accessed January 2022).
UK Government. Oral health survey of adults attending general dental practices 2018: evaluation of methods. A report on a process evaluation of the methods used to deliver the oral health survey of adults attending general dental practices 2018. 2020. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/892453/Oral_health_survey_of_adults_attending_general_dental_practices_2018.pdf (accessed January 2022).
Bowling A. Research Methods in Health: Investigating Health and Health Services. 4th ed. New York: Open University Press, 2014.
UK Government. National Dental Epidemiology Programme for England: oral health survey of mildly dependent older people, 2016. A report on the oral health and dental service use of older people living in supported housing. 2018. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/773355/NDEP_For_England_oral_health_survey_of_mildly_dependent_older_people_2016_report.pdf (accessed January 2022).
NHS England. GP patient survey 2019. 2019. Available at https://www.england.nhs.uk/statistics/2019/07/11/gp-patient-survey-2019/ (accessed January 2022).
Acknowledgements
The authors would like to thank Zoe Marshman for her comments on drafts of this report and Sally Weston-Price for her contribution to the original survey work.
Author information
Authors and Affiliations
Contributions
Kate Jones, Gail V. A. Douglas, Janet Neville, David Wilcox and Gill Davies: conceived and designed the work that led to the submission, acquired data and played an important role in interpreting the results, revised the manuscript, and approved the final version. Tom A. Dyer: conceived and designed the work that led to the submission, played an important role in interpreting the results, drafted the manuscript and approved the final version.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
Ethical approval for the study was provided by the NHS Research Authority (Ref. 17/LO/1594).
Written consent to participate was obtained from those participating.
Requests for access to the data from the survey should be made to the Office for Health Improvement and Disparities at DentalPHIntelligence@dhsc.gov.uk.
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0.© The Author(s) 2023
About this article
Cite this article
Douglas, G., Jones, K., Dyer, T. et al. The oral health of adults attending dental practices in England in 2018: a report of a novel method and findings. Br Dent J (2023). https://doi.org/10.1038/s41415-023-6033-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-023-6033-0