Abstract
Aims and objectives The aim of this Plan-Do-Study-Act cycle was to establish if undergraduate students believe they have a role to play in suicide risk assessment, and to discuss the implementation of suicide risk prevention into the undergraduate dental curriculum. Data gathered informed development of a subsequent suicide risk assessment educational workshop.
Methodology An online questionnaire was disseminated to undergraduate students as part of a quality improvement service evaluation within a UK dental hospital and school. This sought to gain information on attitudes to suicide prevention, previous suicide awareness training, and the appetite and potential barriers to future training.
Results A response rate of 23% (n = 30) was achieved. In total, 87% of undergraduate students responding reported having no experience or training in the identification of suicidal patients, 97% of respondents expressed a desire for training, and 80% stated not knowing what to do if a patient disclosed suicidal thoughts during an appointment.
Conclusion The dental team have a role to play in suicide risk assessment and the signposting of at-risk patients to appropriate services. To embed this within daily practice, awareness and training must be introduced to undergraduate curricula.
Key points
-
Dental professionals have an increasingly important role to play in suicide awareness, risk assessment and signposting patients when needed to appropriate services.
-
Dental and dental therapist graduates have varying degrees of training surrounding suicide and mental health. Suicide education rarely appears to be embedded within undergraduate dental curricula.
-
Results in a UK dental school found further education and support in providing appropriate holistic care for dental patients would be welcomed by dental and dental therapist undergraduates.
Similar content being viewed by others
Introduction
In 2020 alone, 6,211 deaths by suicide were recorded in the UK1 and in 2021, 753 probable deaths by suicide were registered in Scotland.2 Increased suicide rates during the COVID-19 pandemic have been recognised among younger members of society and this has led to more mental health awareness and the need for appropriate educational training for dental undergraduates being highlighted.3 Recently, the Scottish Government published Creating hope together: Scotland's suicide prevention strategy 2022-2032. This proposes a societal approach to suicide risk assessment and awareness, along with highlighting the importance of undergraduate education to prepare graduates for their role in mental health awareness.4 This document follows the 2021 General Dental Council (GDC)-endorsed Mental health wellness in dentistry framework.5 This flags mental health as a key priority for the dental team and future dental professionals. It outlines the importance of rapid intervention and ensuring individuals receive support from the appropriate services. A key recommendation is the importance of undertaking risk assessment in dental settings and the improvement of mental wellbeing for all staff and patients. It is therefore important that dental graduates have had the appropriate training and skills to allow management (in the form of signposting and onward referral to support or specialist services) of mental health concerns of both colleagues and patients.
While traditionally, dental professionals may not come to mind when suicide risk assessment is considered, the dental team are in a unique position to screen for suicidal tendencies. Members of the public, who may not regularly attend other healthcare specialties, might attend regular dental visits. Clinicians working within dentistry are familiar with the need to screen for systemic health conditions which impact oral health. Such health screening ensures the delivery of safe dental care. Dental professionals also undertake routine screening for conditions such as oral cancer, non-accidental injuries and dental disease on a daily basis.
Studies suggest that 80-90% of people who die by suicide increase contact with healthcare professionals in primary care before their death.6 This suggests opportunities are there for identifying at-risk patients, providing support, and signposting to mental health services. Only 28% of all deaths by suicide in the UK are of people who had contact with mental health services in the 12 months beforehand.7 Other healthcare professionals within primary care, such as dentists, are therefore likely to be encountering at-risk individuals.
The government initiative Making every contact count was launched in May 2015. This aims to improve mental health for patients through routine interactions with health professionals, promoting behaviour change.8 Although NHS dental services reduced during the COVID-19 pandemic, 18.2 million NHS dental patients were seen in England over a two-year period until June 2021, highlighting the vast number of individuals attending dental appointments who could benefit from this approach.9
Patients with mental health issues may have a greater risk of oral disease because of side effects of medication, lack of self-care and higher treatment needs because of difficulties in accessing care.10 The dental team are therefore in an ideal position to recognise potential oral health-related signs of mental health concerns, such as suicidal ideation. Furthermore, head and neck cancer survivors are twice as likely to die by suicide than survivors of other cancers.11 It is important the dental team understand the effect such conditions have on patients' mental wellbeing, and the increased risk of such patient groups.
However, despite publications and recommendations as to the role dentistry might play in suicide awareness and signposting, research suggests dental practitioners have low confidence regarding managing patient mental health concerns.12 While the prevalence of mental health conditions rise, there appears a greater need to address this at an early stage in dental workforce training. This would create a trained and skilled dental team, able to recognise suicidal tendencies and mental health concerns and to signpost to appropriate mental health services.12,13 In considering where such training might be incorporated within dental curricula, literature promotes including education on psychiatry within dentistry.12
Indeed, the GDC's Preparing for practice guidance states that all dental graduates should be able to 'identify, explain and manage the impact of medical and psychological conditions';14 however, it is reported that formal education surrounding mental health is rarely implemented into dental undergraduate curriculums across the UK.15 Clarity is required as to how best provide this training. A recent study of Irish and British dental students identified low confidence levels when dealing with patient mental health concerns.12 Subsequent workshop teaching was piloted in five dental schools and was found to improve dental student confidence significantly, promoting the benefits of mental health awareness training within the dental undergraduate curricula.12
In designing twenty-first century dental curricula, educators must consider the population's evolving health needs and equip trainees with the skills to appropriately manage these.16 This need is not new, nor limited to the UK, being highlighted in the USA two decades previously by Alexander et al. (1999).17 This survey found dental students lacked preparedness when tasked with managing mental health concerns and suicidal tendencies in clinical environments. Only 30% of dental schools included in this study at that time offered suicide awareness training to dental students.17
Equipping the dental workforce with the skills to actively screen for mental health concerns may favourably impact self-care. Research surrounding dental student burnout has recently increased and high levels of emotional exhaustion, depersonalisation and low personal accomplishment scores recognised.18,19 Focusing and attuning the dental workforce to mental health may inculcate enhanced stress management and coping skills.17 The British Columbia Faculty of Dentistry (2014) report introducing teaching modules into the undergraduate curriculum to educate on stress management and suicide prevention.20 Brondani et al. propose that, through interactive suicide awareness and educational workshops, education and self-reflection, dental students will develop skills to recognise and manage mental health concerns with colleagues, patients and also individually.20 Literature highlights the benefits of interactive workshops and experience with suicide risk assessment tools.21
This article shares the findings of a quality improvement, cross-sectional service evaluation questionnaire, distributed to fourth and fifth year undergraduate dental students (penultimate and final year Bachelor of Dental Surgery [BDS]) and third year (final year) Bachelor of Science (BSc) (oral health sciences, dental therapists) students at a UK dental hospital and school. This project sought to gain insight on attitudes to suicide ideation, previous suicide awareness training, and the appetite and potential barriers to future training. This project was a standalone Plan-Do-Study-Act (PDSA) cycle used to garner information for developing suicide risk awareness training for dental staff and students in-house.
Materials and methods
This quality improvement project ultimately aims to introduce a local framework for the identification of patients at higher risk of suicide and the management of suicidal disclosures during dental outpatient appointments. The Model for Improvement and PDSA cycles were used to design each iterative cycle of this project.22 The service evaluation questionnaire formed one such PDSA cycle and the information gathered was used to develop targeted, relevant, educational workshops.
A questionnaire was designed to gain an insight into undergraduate:
-
Beliefs and attitudes regarding the role of the dental team in identifying:
-
Risk factors for suicide
-
Suicide prevention via signposting and referral to support services
-
-
Previous suicide awareness and prevention training undertaken
-
Confidence levels and barriers to suicide screening in dental care settings.
Within the questionnaire, information was gathered to highlight correlations between respondent demographics, previous training, beliefs, attitudes and barriers. Free-text boxes were included to gain further information. A five-point Likert scale with responses ranging from 'strongly agree' to 'strongly disagree' was chosen to record the range of participant responses.
A section of the questionnaire included a previously validated and published questionnaire by Herron et al.: 'Attitudes to suicide prevention scale'.23 Permission for use was kindly given by the authors. Including this previously published survey aimed to increase the reliability and validity of findings in this quality improvement project.24 Face validity testing was carried out before dissemination of the questionnaire by dental and clinical psychology colleagues working in primary and secondary care in the UK.25 Participant information resources were circulated with the anonymous, online questionnaire in February 2022, via electronic mailing lists. Participant information explained the survey purpose, data usage and support services available for participants. The questionnaire was circulated to all fourth and fifth year BDS students and third year BSc students at a dental hospital and responses collected February to March 2022. All participants received information resources providing details of the project, advising that completion of the service evaluation questionnaire was deemed as valid consent to take part in the project, and that anonymous findings may be included in future publications.
Confirmation that this service evaluation project did not require ethical approval was sought and granted from the local health board's ethics contact and thereafter, the local NHS Clinical Research Governance Group.
Results
The response rate for the questionnaire was 23% (n = 30) from undergraduate students.
Demographics
Figure 1 shows the female-to-male ratio of respondents. Most responses were from female students 67% (n = 20); there were nine male students (30%) and one respondent (3%) chose not to disclose their sex.
Experience of suicide awareness training
Only 10% of respondents had previously undertaken suicide awareness training as an undergraduate student within the last two years (n = 3); one respondent was unsure (3%) and 87% had no previous suicide awareness training (n = 26) (Fig. 2). Interestingly, only one respondent who had completed suicide awareness training stated it was undertaken in relation to their dental role and one had had the opportunity to use their training when seeing dental patients.
Moreover, 90% of undergraduate students responding stated they would like suicide awareness training (n = 27) (Fig. 3), the majority wishing for a combination of in-person and virtual training resources (73%; n = 22). Free-text responses revealed respondents felt education in this area would be useful and may be more engaging if there was a face-to face/in-person element to training.
Information gained on attitudes to suicide using the prevention scale
It was found that 97% of students responding (n = 29) disagreed or strongly disagreed with the statement that they were resentful about being asked to do more to prevent suicide. The majority also disagreed or strongly disagreed that suicide prevention was not their responsibility (97%; n = 29). However, 50% (n = 15) of students agreed or strongly agreed that they would feel uncomfortable assessing individuals for suicide risk. Additionally, 63% (n = 19) of participants felt a large number of deaths by suicide were preventable and 50% (n = 15) disagreed or strongly disagreed with the idea that there was no way of knowing who would die by suicide.
The role of the dental team
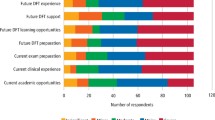
In total, 97% of students agreed the dental team have a role to play in identifying suicidal individuals (n = 29) and 93% agreed that they personally have a role to play in suicide prevention (n = 28) (Fig. 4).
Confidence in recognising mental health concerns
Here, 80% (n = 24) of students felt they did not know what to do if a patient disclosed suicidal thoughts during a dental appointment (Fig. 5). Also, 97% (n = 29) of students replying wished for further training in suicide prevention and risk assessment, and 100% agreed they would like further resources available for education and support.
Interestingly, despite reported reservations about screening and identifying patients with mental health conditions, 70% (n = 21) of undergraduate students felt that they would be able to recognise mental health concerns in staff or fellow students. Further information is needed to understand these contrasting views.
Discussion
The GDC's Preparing for practice guidance14 states that all dental graduates should be able to 'identify, explain and manage the impact of medical and psychological conditions'; however existing curricula may emphasise physical rather than psychological disorders. Indeed, publications suggest dental schools provide varying degrees of education in this area (often limited or none), despite increasing recommendations in this regard.26 The GDC-endorsed Mental health wellness in dentistry framework highlights mental health as a key priority for the dental team, future dental professionals, and the need for incorporation into dental curricula.5
Findings from the questionnaire correlate with published evidence: the majority of undergraduate dental students appear to have little or no experience of suicide awareness training.17 In this study, 87% of students responding to the survey had no previous suicide awareness and risk assessment training; however, 97% expressed a desire for such training, highlighting willingness to engage and embrace this as a role of the dental professional. This parallels findings from Elliot et al. (2021),12 who reported student feedback following educational workshops was overwhelmingly positive, with students reporting increased confidence subsequently. Elliot concluded that educational workshops were an effective way to improve student confidence surrounding patient mental health and should be considered for implementation into dental undergraduate curricula.12 Students responding to the service evaluation survey wished future educational training in the form of in-person workshops coupled with online virtual training.
The PDSA cycle in this quality improvement project achieved its aims, as insight was gained into student views and confidence on suicide awareness and prevention. Limitations are acknowledged, however, in the low number of questionnaire responses (23%; n = 30). Higher response rates are desirable; however, lower rates are often associated with questionnaires used in this manner.27 While it is unclear why some students did not respond, this may be attributable to clinical tasks, workload and time pressures. The questionnaire was disseminated online as this offered the most convenient way of contacting a large number of students and sharing participant information sheets. Although findings may not necessarily be generalisable to all dental schools, these results have proved a useful baseline measure, subsequently used to inform the design of a suicide awareness training workshop as a separate, iterative PDSA cycle. Educational workshops are required to improve knowledge, confidence and skills in the ability to carry out a basic suicide risk assessment, signpost to the appropriate services, and to ensure dental graduates are appropriately trained to manage the rising prevalence of mental health concerns experienced by dental patients. However, there is a need to also measure how this type of training might improve the quality of care patients receive.
Interestingly, 70% of undergraduates responding to the survey felt confident that they could identify mental health concerns with fellow students and staff. However, only 20% felt they would know what to do if a patient disclosed suicidal thoughts during an appointment. This highlights the need for further education to build the skills and knowledge required to actively manage patients, or indeed colleagues, who appear in need of appropriate support and services. It is important to acknowledge that dental professionals should be trained to signpost and/or refer to appropriate support services, and are not expected, nor adequately equipped through possession of a dental or dental therapy degree, to provide active suicide prevention management. While previous research has highlighted low predictability of suicide risk assessment tools, in part due to the rarity of the outcome, production of a suicide risk pathway in dental settings which signposts to support services and aims to support patients, dental staff and students, while ensuring awareness of mental health services, is available.28 This approach may need to suffice until data-driven models with predictive ability are developed and readily available in dental settings.28
Conclusion
This quality improvement service evaluation found that students who completed the questionnaire had an appetite for suicide awareness training, felt they had not had education/training to address this within their undergraduate curricula thus far, and lacked confidence in identifying and managing patients displaying suicidal ideation.
Current evidence and policies recommend the dental workforce be suitably trained and skilled to identify mental health concerns and those patients with greater suicide risk. To achieve this, suicide risk awareness and mental health training must be embedded into curricula for all members of the dental team. However, there is currently an unmet need for a suitable evidence-based educational framework and standards to support the design and implementation of such skills training for all dental team members.
References
Samaritans. Latest suicide data. 2021. Available at https://www.samaritans.org/about-samaritans/research-policy/suicide-facts-and-figures/latest-suicide-data/ (accessed March 2023).
Public Health Scotland. Suicide statistics for Scotland: Update of trends for the year 2021. 2022. Available at https://publichealthscotland.scot/publications/suicide-statistics-for-scotland/suicide-statistics-for-scotland-update-of-trends-for-the-year-2021/ (accessed March 2023).
O'Connor R C, Wetherall K, Cleare S et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry 2021;218: 326-333.
Scottish Government. Suicide prevention strategy and action plan drafts: consultation. 2022. Available at https://www.gov.scot/publications/consultation-new-suicide-prevention-strategy-action-plan-scotland/ (accessed March 2023).
Mental Health Wellness in Dentistry. Mental Health Wellness in Dentistry Framework 2021. Available at https://mhwd.org/download/mental-health-wellness-in-dentistry-framework/ (accessed March 2023).
Harmer B, Lee S, Duong T V H, Saadabadi A. Suicidal Ideation. Treasure Island: StatPearls Publishing, 2023.
University of Manchester. The National Confidential Inquiry into Suicide and Homicide by People with Mental Illness. Making Mental Health Care Safer: Annual Report and 20-year Review. 2016. Available at https://documents.manchester.ac.uk/display.aspx?DocID=37580 (accessed March 2023).
UK Government. Making Every Contact Count (MECC): Consensus Statement. 2016. Available at https://www.gov.uk/government/publications/making-every-contact-count-mecc-practical-resources (accessed March 2023).
NHS Digital. NHS Dental Statistics for England - 2020-21 Annual Report. 2021. Available at https://digital.nhs.uk/data-and-information/publications/statistical/nhs-dental-statistics/2020-21-annual-report (accessed March 2023).
Dental Nursing. Dental care for adults with mental health problems. 2012. Available at https://www.dental-nursing.co.uk/features/dental-care-for-adults-with-mental-health-problems (accessed March 2023).
Osazuwa-Peters N, Simpson M C, Zhao L et al. Suicide risk among cancer survivors: Head and neck versus other cancers. Cancer 2018; 124: 4072-4079.
Elliott E, Sharma S, Omar A et al. A multi-centre early evaluation of the effectiveness of workshop teaching to improve the confidence of UK and Irish dental students when addressing patient mental health. Br Dent J 2021; DOI: 10.1038/s41415-021-3613-8.
Mind. Mental Health in Primary Care: A briefing for Clinical Commissioning Groups June 2016. 2016. Available at https://www.mind.org.uk/media-a/4409/13296_primary-care-policy_web_op.pdf (accessed March 2023).
General Dental Council. Preparing for practice: Dental team learning outcomes for registration. 2015. Available at https://www.gdc-uk.org/docs/default-source/quality-assurance/preparing-for-practice-%28revised-2015%29.pdf (accessed March 2023).
Elliott E, Sharma S, Omar A, Hurst D. How confidently do students address patients with psychiatric conditions in the dental clinic? A service evaluation in a UK dental school. Br Dent J 2020; 228: 376-380.
McHarg J, Kay E J. Designing a dental curriculum for the twenty-first century. Br Dent J 2009; 207: 493-497.
Alexander R E. Stress-related suicide by dentists and other health care workers. Fact or folklore? J Am Dent Assoc 2001; 132: 786-794.
Galán F, Ríos-Santos J-V, Polo J, Rios-Carrasco B, Bullón P. Burnout, depression and suicidal ideation in dental students. Med Oral Patol Oral Cir Bucal 2014; 19: 206-211.
Takayama Y, Miura E, Miura K, Ono S, Ohkubo C. Condition of depressive symptoms among Japanese dental students. Odontology 2011; 99: 179-187.
Brondani M A, Ramanula D, Pattanaporn K. Tackling stress management, addiction, and suicide prevention in a predoctoral dental curriculum. J Dent Educ 2014: 78: 1286-1293.
Smith A R, Silva C, Covington D W, Joiner T J. An assessment of suicide-related knowledge and skills among health professionals. Health Psychol 2014; 33: 110-119.
NHS England and NHS Improvement. Plan, Do, Study, Act (PDSA) Cycles and the model for improvement. Available at https://www.england.nhs.uk/wp-content/uploads/2022/01/qsir-pdsa-cycles-model-for-improvement.pdf (accessed March 2023).
Herron J, Ticehurst H, Appleby L, Perry A, Cordingley L. Attitudes toward suicide prevention in front-line health staff. Suicide Life Threat Behav 2001; 31: 342-347.
Galliher J M, Bonham A J, Dickinson L M, Staton E W, Pace W D. Representativeness of PBRN physician practice patterns and related beliefs: the case of the AAFP National Research Network. Ann Fam Med 2009; 7: 547-554.
Holden R R. Face Validity. In Weiner I B, Craighead W E (eds) The Corsini Encyclopaedia of Psychology. New Jersey: John Wiley & Sons, 2010.
Freeman R, Knights J, Beaton L et al. Prediction of emotional exhaustion over the course of the COVID-19 pandemic in primary care dental staff: an intensive longitudinal study. BMJ Open 2021; DOI: 10.1136/bmjopen-2021-054827.
Booker Q, Austin J, Balasubramanian B. Survey strategies to increase participant response rates in primary care research studies. Fam Pract 2021; 38: 699-702.
Velupillai S, Hadlaczky G, Baca-Garcia E et al. Risk Assessment Tools and Data-Driven Approaches for Predicting and Preventing Suicidal Behaviour. Front Psychiatry 2019; 10: 36.
Acknowledgements
The authors wish to thank Dr Lindsay-Jo Sevier-Guy for gaining permission to use 'Attitudes to suicide prevention scale' and to thank Jane Herron, Louis Appleby and co-authors of the 'Attitudes to suicide prevention scale' (Herron et al., 2001) for the permission given. Thanks are also extended to the students who responded to the service evaluation.
Author information
Authors and Affiliations
Contributions
Niamh Kelly and Julie Kilgariff were responsible for drafting and revision of the manuscript, production of the questionnaire, and collection of results.
If you have been affected by the content of this piece, you can reach out to the following support lines: The Dentists' Health Support Trust via 020 7224 4671 and The Samaritans via 116 123.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
The Health Research Authority 2017 (hra-decisiontools.org.uk) define differences between research, service evaluation and audit. NHS ethical research committee review is not required for service evaluations or research which seeks to elicit the views, experiences, knowledge and contributions of healthcare professionals on a given subject area. Confirmation that this service evaluation project did not require ethical approval was sought and granted from the local Health Board's ethics contact and thereafter, the local NHS Clinical Research Governance Group.
All participants received information resources providing details of the project, advising that completion of the service evaluation questionnaire was deemed as valid consent to take part in the project, and that anonymous findings may be included in future publications.
Rights and permissions
About this article
Cite this article
Kelly, N., Kilgariff, J. Should suicide risk assessment be embedded in undergraduate dental curricula?. Br Dent J 234, 601–605 (2023). https://doi.org/10.1038/s41415-023-5736-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-023-5736-6