Abstract
Aim Dentistry is routinely associated with aerosol generating procedures. It has been suggested that aerosol generating procedures may place the dental professionals at increased risk of infection from respiratory pathogens. In the absence of widespread testing of the dental workforce to ascertain the incidence of COVID-19, a web-based self-reporting survey captured self-isolation patterns in dental professionals.
Method A web-based closed questionnaire via the Survey Monkey platform captured reported COVID-19 self-isolation patterns in the dental team.
Results A total of 3,309 responses were collected: 2,888 (87.3%) responses contained valid data and 26.8% of respondents reported self-isolating. Of these, 31.2% did so because they were suffering from COVID-like symptoms, 21.3% did so in order to protect a vulnerable member of their household, 25.7% did because a member of their household was suffering from COVID-like symptoms, and 21.8% self-isolated to protect themselves.
Conclusion Despite the inherent limitations of self-reporting surveys, a web-based self-reporting questionnaire rapidly captured self-isolating patterns in DCPs. The initial findings from this survey would suggest that between February and April 2020, dental professionals did not experience disproportionately higher levels of COVID-like symptoms than the general population.
Key points
-
Demonstrates the use of an online survey tool to collect real-time data to assess the symptom distribution of a new disease within the dental care professional (DCP) workforce.
-
The data do not support the assumption that DCPs were at greater risk of developing COVID-19 symptoms during a period of rapid community disease spread.
-
Primary care practitioners should feel empowered to design and conduct their own research projects outside of an institutional framework.
Similar content being viewed by others
Introduction
The UK experienced unparalleled disruption to dental activity in Spring 2020. On 25 March 2020, in response to the escalating COVID-19 pandemic, the Office of the Chief Dental Officer (OCDO) issued its third regular update to general practitioners and community dentists.1 The update directed that dental teams cease 'all routine, non-urgent dental care until advised otherwise'. Patients with urgent needs were to be managed remotely via telephone triage and 'whenever possible, [treated] with advice, analgesia, [and] antimicrobial means where appropriate.' Dental conditions which could not be managed through these means were to be referred to urgent dental care hubs.
In the week preceding the OCDO update, chief dental officers from the other home nations had made similar recommendations. Dental teams were advised wherever possible to reduce the number of routine examinations and aerosol generating procedures. These March 2020 recommendations contrasted the first NHS England Standard Operating Procedure (SOP).2 The 27 February SOP determined 'most patients presenting in primary dental care settings are unlikely to have COVID-19' and that a 'possible case of COVID-19 needs both clinical symptoms and travel history or contact with a confirmed case'.
The basis for policy change was likely a combination of factors: 1) the announcement the UK was moving from contain phase and into delay;3 2) the Public Health England recommendation that people identified as 'clinically extremely vulnerable' strictly observe shielding measures;4 3) that dental teams may be at increased risk of infection;5 and 4) dental care itself may be a route for transmission of SARS-CoV-2 within the community.6
In the absence of widespread testing of SARS-CoV-2 infection in the dental workforce, it was believed a simple self-reporting survey could capture self-isolation patterns in dental care professionals (DCPs). It was hoped that such a survey could provide useful epidemiological data to policymakers when considering the risks of COVID-19 transmission within dental settings. Electronic surveys are straightforward for respondents, mitigate the risk of data loss and facilitate data transfer and analysis.7,8 Web-based platforms have been used previously to capture data from healthcare professionals.9,10,11,12
Method
A web-based closed questionnaire via the Survey Monkey platform (SurveyMonkey Inc, San Mateo, California, USA, www.surveymonkey.com) captured reported COVID-19 self-isolation patterns in the dental team between 10-17 April 2020. The survey was openly distributed through messaging apps and dental social media channels (see the online Supplementary Information).
The original data were stored on the survey platform in accordance with their privacy and security policies (https://www.surveymonkey.co.uk/mp/legal/security/) (https://help.surveymonkey.com/en/policy/surveymonkey-data/). Access was password-restricted to one of the authors (AH), who validated the data before removing potential identifiers (General Dental Council [GDC] numbers and IP addresses). It was not possible to identify participants from the working data set.
A list of COVID-like symptoms was developed by combining the information available at that time13,14 (Box 1).
A total of 3,309 responses were collected. All incomplete responses were discarded. Only responses from UK dental professionals were evaluated. The GDC number was screened and rejected where the format did not match the registrant type (however, GDC numbers were not individually validated). Responses were discarded where GDC numbers were duplicated, or where the date for self-isolation predated the first confirmed UK COVID-19 case.15
The 2,888 (87.3%) valid responses remaining for evaluation represents 2.55% of dental professionals registered as of 31 December 2019 (113,439).16
Results were analysed in GNU PSPP (GNU PSPP for GNU/Linux, version 1.2.0-g0fb4db, Boston, MA, Free Software Foundation, www.gnu.org/software/pspp/). The data from the survey are presented through descriptive statistics.
Prior to data collection, an assessment was made of the need for ethical review. The survey was found to be exempt from UK ethical approval.
The Health Research Authority's (HRA's) Does my project require review by a research ethics committee?17 document was consulted in conjunction with the HRA online decision tool.18 The proposed survey was identified as research. At stage two, assessment for each country within the UK was made using the online decision tool 'Do I need NHS REC review?'19 The online tool established that the survey did not meet the necessary requirements for ethical approval. The UK HRA document Standard operating procedures for research ethics committees was additionally consulted.20 The proposed survey did not meet the necessary requirements for ethical review: the research only involved staff of healthcare services (by virtue of their professional role).20 Further reference to Governance arrangements for research ethics committees confirmed the proposed survey did not meet the necessary criteria for ethical review.21
The study participants had to enter their GDC number on the landing page as part of the confirmation that they were willing to take part in the survey and to ensure that duplicate entries were not received. Consent to participate was implied by completion of the survey. IP addresses were used on a temporary basis to ensure the integrity of the data, but these were not stored. A statement explaining that each participant's survey data would be anonymised was made.
Results
Of the 2,888 valid responses, 0.6% (18) were clinical dental technicians (CDTs), 22.9% (661) dental hygienists, 10.8% (313) dental nurses, 1.3% (38) dental technicians, 18.2% (526) dental therapists, 45.7% (1,321) dentists including specialists, 0.3% (8) oral and maxillofacial surgeons and 0.1% (3) orthodontic therapists.
The mean number of days dental professionals reported treating patients before the current pandemic was 4.03 (standard deviation [SD] = 1.07). On a typical pre-pandemic day, 2.1% (61) of dental professionals reported that they did not normally see any patients, 1.7% (50) typically saw between 1-5 patients, 11.7% (339) saw 5-10 patients, 59.7% (1,725) between 10-20 patients, and 24.7% (713) saw more than 20 patients each day.
Self-isolation patterns
In total, 26.8% (775) of respondents reported that they self-isolated due to COVID-19. Of these, 31.2% (242) reported they did so because they were suffering from the symptoms associated with COVID-19 (COVID-like symptoms), 21.3% (165) did so in order to protect or shield a vulnerable member of their household, 25.7% (199) did because a member of their household was suffering from COVID-like symptoms, and 21.8% (169) self-isolated in order to protect or shield themselves (Table 1).
Of those who self-isolated in this survey, 15.5% (120) did so for between 1-7 days, 41.9% (325) 8-14 days, and 42.6% (330) for 15 or more days.
The proportion of each registrant type who identified themselves as shielded or vulnerable was: CDTs = 16.7% (3); dental hygienists = 6.2% (41); dental nurses = 6.4% (20); dental technicians = 7.9% (3); dental therapists = 7.6% (40); dentists = 4.7% (62); and 0.0% of oral/maxillofacial surgeons and orthodontic therapists.
Further information relating to household size was gathered from those who reported they self-isolated. For respondents who reported self-isolation for any reason, mean household size was 3.15 (SD = 1.24; n = 775). For those who reported COVID-like symptoms, mean household size was 3.02 (SD = 1.28; n = 242). Where the dental professional reported a household member having COVID-like symptoms, mean household size was 3.52 (SD = 1.06; n = 199). For those who self-isolated to protect a vulnerable member of their household, mean household size was 3.4 (SD = 1.4; n = 165). For dental professionals who self-isolated because they identified as vulnerable, mean household size was 2.64 (SD = 1.03; n = 169). Figure 1 displays the 95% confidence intervals (CIs) for each of these groups.
Where the dental professional self-isolated, supplementary information was gathered regarding the total number of household members who currently were, or had been suffering from, COVID-19 symptoms. For all groups who self-isolated, mean number of household members reporting COVID-like symptoms was 1.05 (SD = 1.17; n = 775). For dental professionals with COVID-like symptoms, the mean number of household members with COVID-like symptoms was 1.81 (SD = 1.11; n = 242). Where the dental professional reported a household member having COVID-like symptoms, mean household members with symptoms was 1.63 (SD = 1.03; n = 199). For those who self-isolated to protect a vulnerable member of their household, the mean symptomatic household members was 0.19 (SD = 0.53; n = 165). For dental professionals who self-isolated because they identified as vulnerable, the mean symptomatic members of the household was 0.11 (SD = 0.44; n = 169). Figure 2 displays the 95% CIs for each of the groups.
Moreover, 89.5% (299) of households which did not report any household members with COVID-like symptoms at the time of self-isolation remained free of occupants with COVID-like symptoms; 10.5% (35) of households did not.
Description of the symptoms
The proportion of each registrant type who reported they self-isolated due to COVID-like symptoms were: CDTs = 5.6% (1); dental hygienists = 6.5% (43); dental nurses = 6.7% (21); dental technicians = 5.3% (2); dental therapists = 9.9% (52); dentists = 9.1% (120); oral or maxillofacial surgeons = 37.5% (3); and orthodontic therapists 0.0% (0). The symptoms reported by these dental professionals and their household members can be found in Table 2.
In the current survey, only 2.9% (7) of dental professionals who reported they self-isolated because they were suffering from COVID-like symptoms also reported they had been tested for the disease. Of these, 42.9% (3) tested positive. Furthermore, 8.5% (17) of dental professionals who self-isolated due to a household member suffering from COVID-like symptoms also reported that their household member had been tested for the disease. Of those household members tested, 52.9% (9) tested positive.
Dental aerosol
Of the respondents who self-isolated because they were suffering from COVID-like symptoms, 96.7% (234) considered themselves routinely exposed to dental aerosol. Of those who did not self-isolate or self-isolated for other reasons, 96.5% (2,553) considered themselves routinely exposed to dental aerosol.
Date of self-isolation
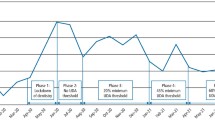
Frequency polygons displaying the incidence of self-isolation over time can be found in Figure 3, Figure 4, Figure 5 and Figure 6. The first dental professional self-isolating in relation to COVID-19 in this survey did so on 10 February 2020. The frequency of self-isolation increases in all groups from 10 March 2020 and decreases following the national lockdown on 23 March 2020.
Discussion
In this survey of UK-registered dental professional self-isolation patterns during the early phase of the COVID-19 pandemic, 8.4% of dental professionals self-isolated due to COVID-like symptoms and 6.9% did so because a member of their household had symptoms. Table 3 provides a comparison of the current study with others conducted during the early stages of the COVID-19 pandemic.
Similar to other studies conducted during the early phase of the pandemic, this study found that levels of dental professionals reporting COVID-like symptoms were comparable with the estimated community infection rate. For the UK, based on serological sampling, the Office for National Statistics estimated that, on 24 May 2020, 6.78% (95% CI: 5.21; 8.64) of the population had COVID-19 antibodies.22The current study, based on self-reported COVID-like symptoms, estimates that 8.4% (95% CI: 6.6; 10.2%) of UK dental professionals experienced COVID-like symptoms before 17 April 2020.
The pattern of self-isolation in those who reported COVID-like symptoms are less erratic than those in other groups. This most likely is due to the fact that the dental professional is fully conversant with their own symptoms. dental professionals who reported they self-isolated due to COVID-like symptoms did so earlier than the other groups. Peak frequency for those who reported they self-isolated due to COVID-like symptoms was on 16 March (n = 22). For those who self-isolated for other reasons, the peak frequency for self-isolation occurs seven days later, at the point of the national lockdown.
The mean household size for dental professionals who self-isolated due a member of their household displaying COVID-like symptoms, or self-isolated to protect a member of their household, was generally larger than the mean household size of those who self-isolated due to individually suffering from COVID-19 symptoms, or individually identified as vulnerable (Fig. 1). This may simply reflect that due to their increased size, larger households could be expected to contain at least one household member who identifies as vulnerable. Similarly, by virtue of their size, larger households may suffer from double jeopardy: they are more likely to have at least one member who is infected, and additionally contain more potential vectors and opportunities for the disease to enter the household. Smaller households are customarily associated with younger and older adults.23 The latter are associated with greater prevalence of multi-morbidity; accordingly, they could be expected to more readily identify as vulnerable.24
Aside from at a nation level, this survey neglected to record respondents' geographical location. Accordingly, it was unable to map self-isolation patterns to recognised zones showing elevated rates of infection. Future surveys may be able to improve upon this by recording location information.
As a proportion of those registered, the number of respondents for the following registration types was below 1%: dental nurses, dental technicians and orthodontic therapists. Future surveys need to find ways of engaging these vital members of the dental workforce.
Conclusion
According to this survey, 8.4%, (95% CI: 6.6; 10.2) of UK registered dental professionals self-isolated before 14 April 2020 due to COVID-like symptoms. It is likely that a number these symptomatic dental professionals did not have COVID-19. Equally, it is probable that infected dental professionals did not self-isolate due to lack of COVID-like symptoms and were not identified by this survey.
This survey is limited by virtue of its self-reporting nature. Ordinarily, survey questionnaires should be corroborated by alternative research methods to ensure the information they capture authentically represents the data which they purport to evaluate. Additionally, self-reporting questionnaires require verification to confirm they generate reliable results over time. However, the circumstances in Spring 2020 did not allow sufficient time for the normal processes of acceptance to occur.
The data were uploaded onto a pre-print server on 29 April 2020. Despite the lack of other available data during the earliest phase of the pandemic, it is not known if the national, strategic policymakers considered the data from this survey to inform decision-making. If future policymakers are to make well-informed decisions about risk, it is critical that wide-scale systems are already in place to collect data during the earliest phases of a pandemic in order to rapidly understand the risks to DCPs. It is difficult to understand why there was no organised national effort to achieve this. It cannot be assumed that testing regimens for new pathogens will be available from day-zero.
References
NHS England. Third of a series of regular updates to general dental practices and community dental services regarding the emerging COVID-19 situation.2020. Available at https://wokingham.moderngov.co.uk/documents/s43592/Issue%25203%2520Preparedness%2520letter%2520for%2520primary%2520dental%2520care%2520-%252025%2520March%25202020.pdf (accessed March 2023).
NHS England. Novel coronavirus (COVID-19) standard operating procedure. Primary dental care settings (including community dental services). 2020. Available at https://www.evidenceaid.org/wp-content/uploads/2020/02/NHS-England-covid-19-primary-care-sop-dental-care-settings-v1.pdf (accessed March 2023).
UK Government. COVID-19: government announces moving out of contain phase and into delay. 2020. Available at https://www.gov.uk/government/news/covid-19-government-announces-moving-out-of-contain-phase-and-into-delay (accessed February 2022).
UK Government. COVID-19: guidance for people whose immune system means they are at higher risk. 2021. Available at https://web.archive.org/web/20200322215848/https://www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19 (accessed February 2022).
Meng L, Hua F, Bian Z. Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J Dent Res 2020; 99: 481-487.
Ather A, Patel B, Ruparel N B, Diogenes A, Hargreaves K M. Coronavirus Disease 19 (COVID-19): Implications for Clinical Dental Care. J Endod 2020; 46: 584-595.
Carbonaro M, Bainbridge J. Design and Development of a Process for Web-Based Survey Research. Alberta J Educ Res 2000; 46: 392-394.
Regmi P R, Waithaka E, Paudyal A, Simkhada P, van Teijlingen E. Guide to the design and application of online questionnaire surveys. Nepal J Epidemiol 2016; 6: 640-644.
Peng J, Rushton M, Johnson C et al. An international survey of healthcare providers' knowledge of cardiac complications of cancer treatments. Cardiooncology 2019; 5: 12.
Milkiewicz P, Krawczyk M, Wunsch E, Ponsioen C, Hirschfield G M, Hubscher S G. Primary Sclerosing Cholangitis With Features of Autoimmune Hepatitis: Exploring the Global Variation in Management. Hepatol Commun 2020; 4: 399-408.
Kessler R A, Shrivastava R K, Chen S L et al. Snapshot: Socioeconomic Competence in US Neurosurgery Residents. World Neurosurg 2019; DOI: 10.1016/j.wneu.2019.07.030.
Jenkins S M, Bissell V, Dawson L J, Murphy R. What did they do next? A survey of dentists who have passed the Overseas Registration Examination of the General Dental Council. Br Dent J 2019; 226: 342-348.
ZOE Health Study. New research on loss of smell or taste. 2020. Available at https://health-study.joinzoe.com/us-post/loss-of-smell-or-taste-is-a-key-symptom-of-covid-19 (accessed March 2022).
NHS UK. Coronavirus (COVID-19) symptoms in adults. 2022. Available at https://www.nhs.uk/conditions/coronavirus-covid-19/symptoms-and-what-to-do/ (accessed March 2022).
World Health Organisation. Novel Coronavirus (2019-nCoV) Situation Report.2020. Available at https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200201-sitrep-12-ncov.pdf?sfvrsn=273c5d35_2 (accessed March 2023).
General Dental Council. Registration statistical report. 2019. Available at https://www.gdc-uk.org/docs/default-source/registration-reports/gdc-registration-statistical-report-2019---final-30-09-2020.pdf (accessed March 2023).
Health Research Authority. Does my project require review by a Research Ethics Committee? Available at https://www.hra-decisiontools.org.uk/ethics/docs/Algorithm%20-%20Does%20my%20project%20require%20REC%20review%20v2.0%2020200304.pdf (accessed June 2022).
Health Research Authority. Is my study research? Available at https://www.hra-decisiontools.org.uk/research/ (accessed June 2022).
Health Research Authority. Do I need NHS REC review? Available at www.hra-decisiontools.org.uk/ethics/ (accessed June 2022).
Health Research Authority. Research Ethics Committee - Standard Operating Procedures. 2022. Available at https://s3.eu-west-2.amazonaws.com/www.hra.nhs.uk/media/documents/RES_Standard_Operating_Procedures_Version_7.4_June_2019.pdf (accessed March 2022).
Health Research Authority.Governance arrangements for Research Ethics Committees.2021. Available at https://www.hra.nhs.uk/planning-and-improving-research/policies-standards-legislation/governance-arrangement-research-ethics-committees/ (accessed March 2023).
Office for National Statistics. Coronavirus (COVID-19) Infection Survey pilot: 29 May 2020. 2020. Available at https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/ bulletins/coronaviruscovid19infectionsurveypilot/ 28may2020 (accessed February 2020).
Office for National Statistics: Average household size by single year of age of Household Reference Person, England, 2015. 2016. Available at https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/families/adhocs/005813 averagehouseholdsizebyageofhouseholdreference personengland2015 (accessed April 2020).
Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L. Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med 2005; 3: 223-228.
Cagetti M G, Cairoli J L, Senna A, Campus G. COVID-19 Outbreak in North Italy: An Overview on Dentistry. A Questionnaire Survey. Int J Environ Res Public Health 2020; 17: 3835.
Negri E, Scarpino V, La Vecchia C. Prevalence of COVID-19-like symptoms in Italy and Lombardy, March-April 2020, and their implications on cancer prevention, diagnosis and management. Eur J Cancer Prev 2021; 30: 123-512.
Jungo S, Moreau N, Mazevet M E et al. Prevalence and risk indicators of first-wave COVID-19 among oral health-care workers: A French epidemiological survey. PloS One 2021; DOI: 10.1371/journal.pone.0246586.
Estrich C G, Mikkelsen M, Morrissey R et al. Estimating COVID-19 prevalence and infection control practices among US dentists. J Am Dent Assoc 2020; 151: 815-824.
Author information
Authors and Affiliations
Contributions
Ronuk Vasant had the original idea, helped in the development of the survey questions and contributed to the writing and editing of the manuscript. Andre Haigh created the survey, wrote much of the manuscript, and collated and formatted the data. Dominic O'Hooley helped to disseminate the survey and edit the manuscript.
Corresponding author
Ethics declarations
The authors have no interests to declare.
The data were uploaded onto a pre-print server on 29 April 2020.
Prior to data collection, an assessment was made of the need for ethical review. The survey was found to be exempt from UK ethical approval. The HRA's 'Does my project require review by a research ethics committee?' document was consulted in conjunction with the HRA online decision tool. The proposed survey was identified as research. At stage two, assessment for each country within the UK was made using the online decision tool 'Do I need NHS REC review?' The online tool established that the survey did not meet the necessary requirements for ethical approval. The UK HRA document 'Standard operating procedures for research ethics committees' was additionally consulted. The proposed survey did not meet the necessary requirements for ethical review: the research only involved staff of healthcare services (by virtue of their professional role). Further reference to 'Governance arrangements for research ethics committees' confirmed the proposed survey did not meet the necessary criteria for ethical review.
The study participants had to enter their GDC number on the landing page as part of the confirmation that they were willing to take part in the survey and to ensure that duplicate entries were not received. Consent to participate was implied by completion of the survey. IP addresses were used on a temporary basis to ensure the integrity of the data, but these were not stored. A statement explaining that each participant's survey data would be anonymised was made.
The BDJ Editor-in-Chief is satisfied that an appropriate ethical pathway was followed in this study given the unique prevailing circumstances.
Supplementary Information
Rights and permissions
About this article
Cite this article
Vasant, R., Haigh, A. & O´Hooley, D. COVID-19 self-isolation patterns in UK dental care professionals from February to April 2020. Br Dent J 234, 519–525 (2023). https://doi.org/10.1038/s41415-023-5694-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-023-5694-z
This article is cited by
-
An irretrievably biased sample
British Dental Journal (2023)