Abstract
Introduction There is currently reduced access to NHS dental services in the UK, particularly in England, with rural and coastal areas significantly affected. Recruitment and retention in dentistry has been highlighted as an issue contributing to the problem.
Objectives To explore what is known or unknown about recruitment and retention of the dental workforce in the UK, with a particular focus on rural and coastal areas. We were keen to gain information relating to factors affecting recruitment and retention, geographical distribution of the workforce, anticipated challenges, strategies or proposals to assist workforce planning and the extent of empirical research.
Methods Searches for peer-reviewed literature and reports were undertaken and included when they met the eligibility criteria. Data were extracted and the findings narratively synthesised.
Discussion The findings suggested wide ranging recruitment and retention issues of the dental workforce in the UK. Most issues were associated with NHS dentists, followed by dental nurses across both the NHS and private sectors. The worst affected parts of the country were rural and coastal areas.
Conclusion It appears from the evidence that there are many dental professionals discussing recruitment and retention issues, followed by stakeholders. However, there is limited research and data to initiate change.
Key points
-
Identifies factors affecting recruitment and retention in the dental workforce in the UK, including future challenges and potential strategies for assisting workforce planning.
-
Discusses the consequence of recruitment and retention issues leading to reduced patient access to dental care.
-
Highlights geographical dental workforce imbalances in the UK, with a particular interest in rural and coastal areas.
Similar content being viewed by others
Introduction
Access to NHS dental services in the UK is currently reduced, particularly in England, with demand massively outstripping capacity.1 Recruitment and retention (R&R) in NHS dentistry has been highlighted as an issue of concern2 and has been a chronic problem in certain areas for many years, exacerbated by the COVID-19 pandemic.3
It has been reported that staff morale dramatically declined during the pandemic,4 with high levels of stress and burnout.5 There is evidence that the impact has increased the number of dental professionals leaving the profession, through early retirement or a change in career.6 Workforce data revealed that more than 2,500 dentists across England and Wales ended their NHS roles in 2021.2
A report by the Association of Dental Groups has identified rural areas as a matter of concern, with Lincolnshire, Cumbria and the South West Peninsula experiencing specific challenges in NHS access.3 The Chief Medical Officer for England recently highlighted the health inequality which exists within rural and coastal (R&C) communities. Coastal communities are of particular concern because of the high burden of health inequalities and low levels of policy and research attention.7 Many factors affect access to NHS dentistry but the R&R of dentists is undoubtedly contributing to the problem.7 This is particularly challenging for R&C practices where recruitment is a longstanding issue.8
Most research into R&R in rural areas has been conducted in Australia, America and Canada. Remote areas of the UK are geographically less isolated and potentially face different challenges compared to those explored in the international literature international literature.
R&R in dentistry has been brought into focus within the UK recently due to severe problems of NHS access. General Dental Council (GDC) data regarding the number of dentist registrants are likely to be flawed,9 as they fail to reflect changes in working patterns, with increasing numbers of dentists working part-time.10
Immediate and long-term solutions are being widely discussed but there is currently a paucity of high-quality research. It is important to identify what evidence exists on R&R in UK dentistry to inform future workforce decisions.
Aim and objectives
The aim was to explore what is known or unknown about R&R in the dental workforce in the UK, with particular attention given to R&C areas. The objectives were constructed around five focused questions, used to guide the selection of results, the extraction of data and the presentation of the findings:
-
1.
What factors affect R&R in the dental workforce in the UK?
-
2.
What do we know about the current geographical distribution of the dental workforce across the UK?
-
3.
What are the anticipated challenges to R&R in the dental workforce in the UK?
-
4.
What strategies are there to assist workforce planning in the UK?
-
5.
What is the extent of empirical research in this field?
In order to reflect the current situation, this review was limited to evidence from the past five years, as it would include recent external events, such as the COVID-19 pandemic and Brexit.
Methods
To answer these questions, we undertook a scoping review, a method of evidence synthesis used to explore broad topics across wide varieties of literature and studies. Scoping reviews address wider questions than systematic reviews and incorporate a wider range of evidence, such as reports and opinion pieces. For this reason, scoping reviews typically do not include a critical appraisal of the included items.11 Scoping review methodology has developed over recent years,12 and we followed the guidance by Peters et al.13
Protocol and registration
The protocol was developed a priori in accordance with the Joanna Briggs Institute guidelines for scoping review protocols,13 accessed at: https://osf.io/ctb7v/.
Eligibility criteria
All types of evidence, including empirical studies, secondary research, reports, opinion pieces and webpages, were considered. All categories of dental care professionals in primary or secondary care, privately or in the NHS, were considered. Inclusion criteria are described in Table 1.
Website searches
A number of websites were searched (see Box 1).
Literature searches
Three bibliographic databases were searched: Scopus (Elsevier), Web of Science (Clarivate) and Dentistry and Oral Sciences Source (EBSCOhost). The search strategy comprised terms for dental care professionals, recruitment and retention, and the UK. Searches were undertaken by an information specialist. Results were deduplicated in EndNote and transferred to Rayyan for screening.14
Selection of sources of evidence
All results were single screened against the eligibility criteria by the lead author (DE).
Data items
The following data items were extracted: author; year; type of evidence; factors affecting recruitment or retention; geographical distribution of dental professionals; future challenges to the workforce; and strategies, recommended or implemented.
Critical appraisal of individual sources of evidence
No critical appraisal was undertaken. Critical appraisal is an essential component of systematic reviewing, especially for clinical research into efficacy of interventions. This has less merit in scoping reviews, where the aim is to explore broad conceptual questions across a range of evidence types.15
Synthesis of results
The findings are synthesised narratively and presented to address each question in turn.
Results
What factors affect recruitment and retention in the dental workforce in the UK?
Factors affecting R&R in the dental workforce were widely discussed in the literature:
-
1.
The NHS Units of Dental Activity contract was deemed the most common factor in England,5,16,17 including its associated workload.18The literature pointed to a relationship between stress-related R&R issues and the NHS working environment,19 reporting that stress and burnout commonly affects dentists across the UK.20 This was widely corroborated, with sources stating that dentists are 'deeply discontent with the NHS primary care systems' in England17 and are 'fed up with a system that is fundamentally flawed'.21 Ultimately, it was found that, in England, the contract is 'driving people out of the profession'5
-
2.
Limited opportunities for career progression impacts retention, particularly NHS dentists and dental nurses across both NHS and private sectors.10 One study found that many dentists working for NHS dental services were keen to upskill,17 but are discouraged by the lack of financial incentives under the NHS contract22
-
3.
Financial factors include the increase in the cost of expenses and indemnity23 and the long-term reduction in income.24 Remuneration was also identified as an important factor in attracting and retaining dental hygienists and therapists.25 Dental nurses report feeling 'underpaid and undervalued'24 and the feeling of being undervalued was commonly noted across the dental workforce.2 Many also expressed worries about costly and stressful litigation.21Financial factors were also found at the systems level.26 In England, government funding has reduced in real terms by 29% since 201027 and dentistry is the only part of the NHS now operating on a lower budget than previously28
-
4.
Brexit and the pandemic were widely discussed, with issues including legislative uncertainty, the need for work permits and financial aspects.29 The number of European Union applicants entering the UK dental register fell from 1,249 in 2016-2017 to 686 in 2017-2018,29 the same year Article 50 was formally triggered.30 The decline continuing with only 357 applicants added to the register in 2020.31The situation deteriorated markedly in 2020 due to suspension of the Overseas Registration Examination (ORE) due to COVID restrictions.4 The ORE process was already under pressure and criticised for its effectiveness, capacity and laborious processes recognising overseas dentists2,32,33
-
5.
Specific geographical challenges for rural and coastal areas have historically been more prevalent2 but some additional factors impact these locations:34
-
Poor transport links35
-
Urban prominence of dental schools, teaching hospitals and training opportunities23
-
The tendency for dentists to work within urban areas, where they have family ties36and personal connections23
-
Dentists often settle where they complete foundation training,35 coupled with a lack of R&C placements.37
-
What is the geographic distribution of the dental workforce across the UK?
An uneven geographical distribution of the dental workforceis highlighted within the literature and this maldistribution is not a new phenomenon.32,38 The National Audit Office reported that the UK has the fewest dentists per capita in Europe, with England having the fewest NHS primary care dentists per person.1 From 2020-2021, a fall in NHS dentist numbers was found in all regions in England,16 taking the headcount to its lowest level since 2013-2014.7 Further data suggest there are NHS dentist shortages across Wales.38 In Scotland, practice owners were unconfident staffing levels could be maintained and in Northern Ireland there is evidence dentists are leaving NHS dentistry.39
Workforce data and evidence submitted to the Health and Social Care Committee supports these findings, where nine in ten NHS practices across England were facing difficulties recruiting.2
Urban working preferences were noted and in 2018, an 'oversaturation of dentists in urban areas' was reported,18 particularly in London.40 A proposed explanation was that 22-23% of dental school applicants are from London41 and that students tend to return to their hometowns after graduating.42 Furthermore, 46% of speciality registrars chose London as their preferred location.
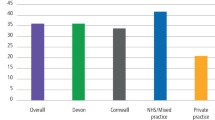
Locations with severe recruitment issues were Lincolnshire,21 Cornwall,43 Somerset,44 Scarborough, Hull and the Isle of Wight.45 Overall, the worst affected parts of the country were R&C areas.45 A practice in Barrow had permanent, unfilled vacancies for five years46 and a recruitment agency in Cumbria was unable to fill any vacancy in a 12-month period.47 There were many sources describing difficulties attracting the dental workforce to rural areas,2,24,38 and now major cities.7
A severe maldistribution of dentists across the UK was reported, especially affecting deprived and less populated communities.48
What are the anticipated challenges to recruitment and retention in the dental workforce in the UK?
Anticipated challengesto the future dental workforce include:
-
1.
GDC data showed the number of registered dentists fell by 961 from 2021-2022.19 This impact is difficult to understand as the GDC does not collect information regarding how registrants work, for example, part-time, percentage NHS/private, or those on the register not currently practising clinically.49 This lack of workforce data was also discussed by Health Education England (HEE)50 and the British Dental Association (BDA)2
-
2.
The pandemic has had a large influence on the challenges to R&R, by exacerbating existing problems and raising new issues:
-
The recruitment of dentists from outside Europe is a challenge, as they may not be able to complete their ORE in time.51 This is reportedly due to inflexible legislation and the pandemic backlog.4 It is believed that due to its limited capacity,32 the ORE will be unable to process the 2,000 waiting dentists4 before the strict legal time limit runs out51
-
During the pandemic, many dental professionals felt dentistry was less secure. A number of hygienists, therapists and technicians believed they would not be in their current roles in the next 12 months and younger professionals were considering career changes.6 In 2020, it was suggested that the worst effects of the pandemic on the mental health of the dental workforce was yet to materialise.52 A more recent source reinforced this, stating dentists were 'exhausted and demoralised'53
-
Exacerbation of limited NHS capacity,54 along with financial and workload pressures,55 contribute to the perception that NHS dentistry is an unattractive and stressful working environment,2 particularly if there is a requirement to work longer hours.52 These factors act as a driver to reduce NHS commitments and to work in private practice instead,22 where it was reported dentists feel there is less pressure.56
-
-
3.
Change to working patterns with dentists not working clinically five days a week57
-
4.
R&C issues, including young dentists' concerns regarding stress and wishing to work in urban areas with a perceived better quality of life,42 and that those wishing to undertake further training and hospital jobs locate near to teaching hospitals,35 mainly in urban areas.23
What strategies are there to assist workforce planning in the UK?
Strategies to assist workforce planningwere reviewed. There were many suggestions; however, few had been implemented:
-
1.
In England, the Advancing dental care review by HEE aims to support retention by restructuring education to fit trainees' preferences, via flexible training.50 The development of 'integrated centres for dental development' was promoted, with hubs providing additional training opportunities in areas remote from dental schools,50 as well as apprenticeships to promote a local dental workforce58
-
2.
Train more dental professionals, particularly in areas with poor access,32 commonly R&C.50 A number of sources also highlighted the need for more dental foundation trainers23 and a change in the competitive dental foundation training application process, to address uneven workforce distribution50
-
3.
It was recognised that work engagement could reduce dental nurses' intentions to leave,59 by creating avenues for career progression60
-
4.
National strategieswere proposed by the BDA, who 'urged the government to factor dentistry into its NHS plan',28 and The College of General Dentistry, to 'support workforce retention through its career pathways programme'.61It was also noted that the NHS recruited 'thousands of reservists';62 however, no evidence shows these resources in dentistry
-
5.
Contract reform was the most frequently mentioned factor in England for improving conditions across the dental team5 and addressing recruitment problems.61 Workforce retention is considered 'intimately related' to the NHS contract63 and if there are no 'significant changes' introduced, the drift to private dentistry will continue22
-
6.
After Brexit, commentators called for an easier system for assisting overseas dental professionals to practise in the UK. This would involve extending the recognition of qualifications32 and reforming the ORE.51 This has been partially addressed by the Professional Qualifications Act 2022,64 allowing countries to mutually recognise qualifications
-
7.
Local level strategies have been implemented across several regions, such as the South West, including recruitment campaigns35 and funding for post-graduate courses.35 Joint initiatives with various local dental networks and authorities65 were also identified.
What is the extent of empirical research in this field?
Of the 73 included sources, most were editorial and opinion pieces (n = 37), often in dental publications. The audience were assumed to be mainly dentists working across the NHS and private sectors. The second largest proportion came from official reports and documents (n = 21). There was a limited amount of empirical research (n = 15): 13 quantitative and 2 qualitative.
The quantity and type of evidence identified provides some indication of the level of interest around R&R, but, unfortunately, with limited empirical research and inadequate statistical evidence and workforce data to support these discussions.
Many sources highlighted most R&R issues were associated with primary care NHS dentists, followed by dental nurses working across both the NHS and private sectors.
A summary of the evidencesources based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) process is in Figure 1.66
PRISMA flow diagram showing the sources of evidence included in the review66
Discussion
In 2019, it was stated that 'dentistry faces existential crisis'. Three years later, it is reported that only 'urgent change can save NHS dentistry'.60 This scoping review has focused on identifying current workforce R&R challenges facing UK dentistry, with a particular focus on R&C areas. The R&R of dental staff is critical in maintaining a viable dental service and failure to act quickly and decisively will cause irreversible damage to NHS dentistry.27
Escalating problems could be envisaged if more dentists move into private practice, with the impact felt by NHS patients and practices. NHS access for patients will be further compromised, and practices will have increased vacancies or may close completely.36 Issues such as Brexit, the pandemic and financial pressures, affect both NHS and private practices, but the latter has greater control in adapting. This is likely to lead to greater opportunities within the private sector, thereby accelerating the transition of dentists from the NHS.
This could further negatively impact how new graduates view the NHS,2 meaning they may migrate earlier in their careers to the private sector.56 Increased demand on private practices, due to the lack of NHS patient access, will then place additional pressures. The challenges of R&R may not be isolated to NHS practice and problems of recruitment within the private sector in rural areas has already been reported.1,45
Priority for rural and coastal areas will aid deprived communities with access to dental care and address inequalities.48,50 It was reported in Australia that to develop a stable healthcare system, the factors that influence R&R of dental practitioners in rural areas must be better understood.67 Although rural Australia is geographically more isolated than the UK, strategies there could still be explored in the UK,28 including: increased financial remuneration; the development of social bonds and an enjoyment of the rural lifestyle, achieved by integration via the rural placement of dental schools; placement programmes; and increasing career opportunities.67 The proposed 'integrated centres for dental development' by HEE,50 located in areas remote from dental schools, could provide training opportunities within R&C areas.50 This would obviate the need for dentists to locate themselves in urban areas23 and could increase the number of dental professionals in R&C and deprived communities.48,50
Government actions will be key to initiating and assisting the strategies found to improve R&R of the dental workforce in the UK.
Firstly, increasing overall funding within dentistry, as well as towards new and established dental schools, could prevent the falling projected numbers of the future workforce and 'increase reach and training in underserved areas'.19
Furthermore, altering the legislation to enable more overseas dentists to complete the ORE4,32 and simplifying the recognition process33 would ease this barrier to recruitment.
Undoubtedly, the most common factor affecting R&R of the dental workforce is the NHS working environment,19 in particular, the NHS contract in England.5,16,17 Contract reform would directly address many recruitment problems61 and aid retention of the existing workforce.63
The reform would also be an opportunity to improve professional fulfilment and retention. Dental therapists63 and nurses with additional qualifications are not recognised as 'performers' under the current contract. This is a barrier to NHS access, undermines team-working and compromises the provision of preventative oral health care.
Future research is necessary to inform long-term strategic decisions, but this must be supplemented by urgent action. Research should include an exploration of the influences on graduates' decisions, in particular, location choices, to better understand the barriers, drivers and facilitators informing career choices. This is particularly relevant in R&C areas to address geographic inequalities.67
Secondly, there is a 'need for reliable contemporaneous workforce data', to allow full understanding of the problem50 and help predict the future workforce numbers needed.
Addressing these knowledge gaps, gaining more qualitative data and performing longitudinal studies would ensure that future R&R interventions can be more effective and target areas with the greatest needs. Ensuring collaboration across multiple stakeholders and joint working would produce both short- and long-term strategies that are paramount in improving the R&R of the dental workforce in the UK.
Limitations
Inevitably, reviews are constrained by the extent and nature of the literature. In this instance, there was a limited amount of empirical research, with most documents being from grey literature sources and with a lot being commentaries or similar. In addition, while the five-year timeframe we chose for the review ensured a focus on current workforce issues, it may have limited our access to longer-term concerns. It was also found that many evidence sources discussed R&R issues affecting dentists only and not the rest of the dental team, as well as a number of evidence sources discussing issues within England and not the rest of the UK. Finally, the review focused on workforce issues across the whole UK and it is acknowledged that there may be specific issues or initiatives at local levels that merit further attention.
Conclusions
This review has identified the key current challenges for the R&R of the dental workforce in the UK. Within the literature, the perilous state of NHS dentistry is widely acknowledged; although there appears to have been little progress in addressing the underlying issues. Further delays will undoubtedly impact on patient care, leading to a deterioration in oral health and unnecessary suffering for many. This will predominantly affect the most vulnerable in society, resulting in greater oral health inequality.
Our review also found that the situation appears to be particularly acute within R&C areas, but data needs to be collected and analysed to provide a better understanding. Well-informed, evidence-based decisions are essential in mapping out the future of dentistry in the UK, but this must not delay immediate action at a local, regional and national level.
References
National Audit Office. Dentistry in England: A National Audit Office memorandum to support a Health and Social Care Committee inquiry. 2020. Available at https://www.nao.org.uk/wp-content/uploads/2020/03/Dentistry-in-England.pdf (accessed April 2022).
British Dental Association. Written evidence submitted by The British Dental Association (RTR0101). 2022. Available at https://committees.parliament.uk/writtenevidence/42795/pdf/ (accessed April 2022).
Healthwatch England. What people have told us about NHS dentistry. 2021. Available at https://www.healthwatch.co.uk/sites/healthwatch.co.uk/files/20210524%20Dentistry%20during%20COVID-19%20Insight%20Briefing.pdf (accessed May 2022).
Westgarth D. The dental workforce: An assessment of the recruitment market. BDJ In Pract 2022; 35: 14-18.
Witton R, Plessas A, Wheat H et al. The future of dentistry post-COVID-19: perspectives from Urgent Dental Care centre staff in England. Br Dent J 2021; DOI: 10.1038/s41415-021-3405-1.
General Dental Council. Responding to the changing strategic context. 2020. Available at https://www.gdc-uk.org/docs/default-source/corporate-strategy/responding-to-the-changing-strategic-context.pdf?sfvrsn=fe91126e_12 (accessed April 2022).
King T. Problems recruiting associates are now endemic. Br Dent J 2022; 232: 7.
Jo O, Kruger E, Tennant M. Dental specialist workforce and distribution in the United Kingdom: a specialist map. Br Dent J 2021; DOI: 10.1038/s41415-021-3167-9.
General Dental Council. Registration report - January 2022. 2022. Available at https://www.gdc-uk.org/docs/default-source/registration-reports/registration-report_january-2022.pdf?sfvrsn=bd140c06_5 (accessed May 2022).
Holmes R D, Burford B, Vance G. Development and retention of the dental workforce: findings from a regional workforce survey and symposium in England. BMC Health Serv Res 2020; 20: 255.
Tricco A C, Lillie E, Zarin W et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol 2016; 16: 15.
Peters M D J, Marnie C, Tricco A C et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth 2020; 18: 2119-2126.
Peters M D J, Godfrey C, McInerney P, Munn Z, Tricco A C, Khalil H. Chapter 11: Scoping Reviews (2020 version). In Aromataris E, Munn Z (eds) JBI Manual for Evidence Synthesis. Adelaide:JBI, 2020.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan - a web and mobile app for systematic reviews. Syst Rev 2016; 5: 210.
Munn Z, Peters M D J, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 2018; 18: 143.
Association of Dental Groups. New figures show workforce crisis as number of NHS dentists fall across the whole of England. 2021. Available at https://www.theadg.co.uk/new-figures-show-workforce-crisis-as-number-of-nhs-dentists-fall-across-the-whole-of-england/ (accessed April 2022).
Gallagher J E, Colonio-Salazar F B, White S. Supporting dentists' health and wellbeing - workforce assets under stress: a qualitative study in England. Br Dent J 2021; DOI: 10.1038/s41415-021-3130-9.
Puryer J, Sidhu G, Sritharan R. The career intentions, work-life balance and retirement plans of UK dental undergraduates. Br Dent J 2018; 224: 536-540.
Dental Schools Council. Written evidence submitted by the Dental Schools Council (RTR0030). 2022. Available at https://committees.parliament.uk/writtenevidence/42610/pdf/ (accessed April 2022).
Stagnell S, Patel N, Shah S. Is less-than-full-time training in dentistry swimming against the tide? Br Dent J 2019; 227: 347-351.
Payne D. PERSPECTIVES: The dental recruitment crisis. Br Dent J 2018; 224: 472-475.
Anonymous. NHS dentistry: I don't want to leave, but I feel there is no choice. 2022. Available at https://bda.org/news-centre/blog/Pages/NHS-dentistry-I-don%E2%80%99t-want-to-leave-but-I-feel-there-is-no-choice.aspx (accessed April 2022).
Bupa Global & UK. Written evidence submitted by Bupa Global & UK (RTR0130). 2022. Available at https://committees.parliament.uk/writtenevidence/42978/pdf/ (accessed April 2022).
Sellars S. Workforce. Br Dent J 2021; 231: 321.
Association of Dental Hospitals. Written evidence submitted by Association of Dental Hospitals (RTR0068). 2022. Available at https://committees.parliament.uk/writtenevidence/42723/pdf/ (accessed April 2022).
Hanks S, Cotton D, Spowart L. Leadership in Dental Practice: a Three Stage Systematic Review and Narrative Synthesis. J Dent 2020; 102: 103480.
Cann R. The recruitment crisis in NHS dentistry needs to be addressed. 2019. Available at https://bda.org/news-centre/blog/Pages/The-recruitment-crisis-in-NHS-dentistry-needs-to-be-addressed.aspx (accessed April 2022).
British Dental Association. Dentists urge government to act as NHS access hotspots go Blue in election. 2019. Available at https://bda.org/news-centre/press-releases/Pages/Dentists-urge-government-to-act-as-NHS-access-hotspots-go-Blue-in-election.aspx (accessed April 2022).
O'Dowd A. Brexit delay is hurting dentistry recruitment. Br Dent J 2019; 227: 179-182.
UK Parliament. Brexit timeline: events leading to the UK's exit from the European Union. 2021. Available at https://commonslibrary.parliament.uk/research-briefings/cbp-7960/ (accessed May 2022).
General Dental Council. Registration Statistical Report 2020. 2020. Available at https://www.gdc-uk.org/docs/default-source/registration-reports/gdc-registration-statistical-report-2020---final311fef86-9e9f-44bb-81d8-68b3a44cae39.pdf?sfvrsn=918f77ec_5 (accessed May 2022).
Association of Dental Groups. 30 years of hurt: The urgent need to rebuild our dentistry workforce. 2020. Available at https://www.theadg.co.uk/wp-content/uploads/2020/12/30-Years-of-Hurt-Report.FINAL_.Dec20.pdf (accessed April 2022).
British Dental Journal. UK dental practices are struggling to fill roles. Br Dent J 2018; 224: 60.
Hussain I, Thomson A, Norfolk T. Recruitment and retention. Br Dent J 2020; 228: 59.
NHS England and NHS Improvement. Dental Access for Adults and Children in Devon. 2021. Available at https://democracyindevon.moderngov.co.uk/documents/s34891/2021%2003%2008%20Dev (accessed April 2022).
Lewis J. Rural recruitment issues: A Cumbrian perspective. BDJ In Pract 2021; 34: 12-13.
NHS England and NHS Improvement. Dental Transformation SPRINT Workshop 1: Output. 2021. Available at https://www.england.nhs.uk/south/wp-content/uploads/sites/6/2021/08/dental-sprint-1-output-report.pdf (accessed April 2022).
Jo O, Kruger E, Tennant M. Geospatial analysis of the urban and rural/remote distribution of dental services in Scotland, Wales and Northern Ireland. Int Dent J 2020; 70: 444-454.
Review Body on Doctors' and Dentists' Remuneration. Review Body on Doctors' and Dentists' Remuneration Forty-Ninth Report 2021. 2021. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1005003/DDRB_2021_Web_Accessible_v2.pdf (accessed April 2022).
British Dental Journal. Dentists willing to sacrifice higher wages to work in richer areas, study shows. Br Dent J 2018; 225: 797.
Gallagher J E, Calvert A, Niven V, Cabot L. Do high tuition fees make a difference? Characteristics of applicants to UK medical and dental schools before and after the introduction of high tuition fees in 2012. Br Dent J 2017; 222: 181-190.
Thomson F, Macey R, O'Malley L, Tickle M. Factors influencing dental trainees' choice of training programme and working patterns: a mixed-methods study. Br Dent J 2021; 230: 363-368.
King T. NHS recruitment crisis. Br Dent J 2019; 227: 759.
UK Government. Chief Medical Officer's annual report 2021: health in coastal communities. 2021. Available at https://www.gov.uk/government/publications/chief-medical-officers-annual-report-2021-health-in-coastal-communities (accessed April 2022).
Association of Dental Groups. Oral health in our coastal communities. 2021. Available at https://www.theadg.co.uk/oral-health-in-our-coastal-communities/ (accessed April 2022).
British Dental Journal. Three quarters of NHS dental practices failing to fill vacancies. Br Dent J 2019; 226: 480.
Rural Services Network. If oral health matters, how can we prevent rural residents pulling their teeth out? 2021. Available at https://rsnonline.org.uk/if-oral-health-matters-how-can-we-prevent-rural-residents-pulling-their-teeth-out (accessed April 2022).
Jo O, Kruger E, Tennant M. Disparities in the geographic distribution of NHS general dental care services in England. Br Dent J 2021; DOI: 10.1038/s41415-021-3005-0.
General Dental Council. Total number of registered UK dentists remains stable following renewal. 2022. Available at https://www.gdc-uk.org/news-blogs/news/detail/2022/01/17/total-number-of-registered-uk-dentists-remains-stable-following-renewal (accessed April 2022).
Health Education England. Advancing Dental Care Review: Final Report. 2021. Available at https://www.hee.nhs.uk/our-work/advancing-dental-care (accessed April 2022).
Czerniawski S. The ORE: a flawed system made worse by the pandemic with further challenges ahead. 2021. Available at https://www.gdc-uk.org/news-blogs/blog/detail/blogs/2021/12/17/the-ore-a-flawed-system-made-worse-by-the-pandemic-with-further-challenges-ahead (accessed April 2022).
Westgarth D. What does the future hold for the workforce of tomorrow? BDJ In Pract 2020; 33: 12-17.
McColl D. Scotland: Preventing the collapse of NHS dentistry. 2022. Available at https://bda.org/news-centre/blog/Pages/Scotland-preventing-the-collapse-of-NHS-dentistry.aspx (accessed April 2022).
British Dental Association. Written evidence submitted by the British Dental Association (CBP0034). 2021. Available at https://committees.parliament.uk/writtenevidence/38571/pdf/ (accessed April 2022).
Scales R. Financial and workforce impacts on dentistry will continue to be felt for some time. 2021. Available at https://www.gdc-uk.org/news-blogs/blog/detail/blogs/2021/03/11/financial-and-workforce-impacts-on-dentistry-will-continue-to-be-felt-for-some-time (accessed April 2022).
Patel K. Young dentists: breaking the silence. Br Dent J 2018; 224: 767-768.
Eaton K A. Oral healthcare workforce planning in post-Brexit Britain. Br Dent J 2020; 228: 750-752.
Health Education England. New plans for dental training reform in England to tackle inequalities in patient oral health. 2021. Available at https://www.hee.nhs.uk/news-blogs-events/news/new-plans-dental-training-reform-england-tackle-inequalities-patient-oral-health-0 (accessed August 2022).
Awojobi O, Movahedi S, Jones E, Gallagher J E. The evaluation of an innovative dental nurse training pilot scheme. Br Dent J 2018; 224: 875-880.
Anonymous. Calling it quits: only urgent change can save NHS dentistry. 2022. Available at https://bda.org/news-centre/blog/Pages/Calling-it-quits-only-urgent-change-can-save-nhs-dentistry.aspx (accessed April 2022).
College of General Dentistry. College response to NHS England announcement of additional dentistry funding. 2022. Available at https://cgdent.uk/2022/01/25/college-response-to-nhs-england-announcement-of-additional-dentistry-funding/ (accessed April 2022).
NHS England. Major drive launched to recruit NHS reservists. 2022. Available at https://www.england.nhs.uk/2022/03/major-drive-launched-to-recruit-nhs-reservists/ (accessed April 2022).
Association of Dental Groups. Written evidence submitted by the Association of Dental Groups (RTR0010). 2022. Available at https://committees.parliament.uk/writtenevidence/42289/pdf/ (accessed April 2022).
UK Parliament. Professional Qualifications Act 2022. 2022. Available at https://bills.parliament.uk/bills/2865 (accessed April 2022).
NHS England and NHS Improvement. Oral Health Needs Assessment South West of England. Appendix 3: Somerset STP Analysis. 2021. Available at https://www.england.nhs.uk/south/wp-content/uploads/sites/6/2021/02/SW-OHNA-Appendix-3-Somerset-STP.pdf (accessed April 2022).
Page M J, McKenzie J E, Bossuyt P M et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; DOI: 10.1136/bmj.n71.
Godwin D M, Hoang H, Crocombe L A, Bell E. Dental practitioner rural work movements: a systematic review. Rural Remote Health 2014; 14: 2825.
Funding
This review was funded by the Faculty of Health Strategic Investment Fund, University of Plymouth.
Author information
Authors and Affiliations
Contributions
Deborah Evans: screening, data extraction, analysis, writing manuscript, writing abstract, referencing, and revising and proofreading the manuscript. Lorna Burns: developing themes, methodology expert, principal investigator, conducting search, quality analysis, quality appraisal, writing methods, language editor, and revising and proofreading the manuscript. Ian Mills: developing themes, writing introduction, quality analysis, language editor, and revising and proofreading the manuscript. Marie Bryce: developing themes, methodology expert, quality analysis, language editor, and revising and proofreading the manuscript. Sally Hanks: developing themes, quality analysis, language editor, and revising and proofreading the manuscript.
Corresponding author
Ethics declarations
The authors confirm there are no conflicts of interest in this project.
This study was deemed not to require ethical review by the University of Plymouth Faculty of Health Research Ethics and Integrity Committee on the grounds that it involved only the synthesis of data obtained from/about human subjects already in the public domain through previous publication.
Rights and permissions
About this article
Cite this article
Evans, D., Burns, L., Mills, I. et al. Recruitment and retention in dentistry in the UK: a scoping review to explore the challenges across the UK, with a particular interest in rural and coastal areas. Br Dent J (2023). https://doi.org/10.1038/s41415-022-5406-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-022-5406-0
This article is cited by
-
Inappropriate behaviours in a dental training environment: pilot of a UK-wide questionnaire
British Dental Journal (2023)
-
What can the GDC's monthly registrant reports offer strategic dental nurse workforce planning?
British Dental Journal (2023)
-
Dental nurse retention in the UK
BDJ Team (2023)
-
Dental practice workforce challenges in rural England: survey into recruitment and retention in Devon and Cornwall
British Dental Journal (2023)
-
Does the NHS Dental Workforce Plan in England align with the UN Sustainable Development Goals?
British Dental Journal (2023)