Abstract
Professional delay is an important delay in referral of patients with suspected mouth cancer. Missing the possibility of cancer might not only result in worse outcomes in respect to function and survival, but also have medicolegal implications. The aim of this article was to review a consecutive cohort of patients over a two-year period with mouth cancer diagnosis and identify those with professional delay and illustrate the main types of presentations using short case histories. The multi-disciplinary team records were used to identify case notes of a two-year (2019 and 2020) consecutive cohort of patients diagnosed with mouth cancer, including referrals from primary and secondary care. Professional delay was considered if red flag symptoms were not referred within two weeks or if there was initial misdiagnosis. In total, 246 patients with mouth cancer were discussed with the multi-disciplinary team: 35 had delay in referral or misdiagnosis of mouth cancer. Six common scenarios were identified: 1) sudden onset paraesthesia; 2) dental abscess; 3) temporomandibular joint dysfunction syndrome (TMJD) and abscess; 4) TMJD; 5) trauma/facial fracture; and 6) non-healing socket following dental extraction. To conclude, it can be difficult to accurately diagnose mouth cancer in primary dental and medical care and an index of suspicion is essential in order to minimise the possibility of professional delay.
Key points
-
Professional delay is an uncommon but important aspect of delay in referral of patients with suspected mouth cancer.
-
Professional delay can occur when the symptoms are misinterpreted as a common non-cancer condition, such as a dental abscess, temporomandibular joint dysfunction syndrome or a non-healing socket following dental extraction.
-
Greater awareness of red flag symptoms in both general dental and medical practitioners is needed to ensure prompt referral and early detection of mouth cancer.
Similar content being viewed by others
Introduction
The incidence of new head and neck cancer is increasing in the UK, with approximately 12,000 new cases diagnosed every year,1 with approaching 7,000 registrations of cancer in the oral cavity, lip and pharynx in 2017. Information requests made by the Oral Health Foundation2 found that in 2020, this number increased to almost 9,000 cases.3,4,5,6 General dental and medical practitioners have a vital role in referral of suspected mouth cancer to specialist centres and National Institute for Health and Care Excellence guidelines on suspected cancer referrals recommends referral to specialist cancer centres within two weeks.7 However, delays in head and neck cancer diagnosis are extensively reported, with many cases presenting at an advanced stage, worsening long-term prognosis.
Professional factors in diagnosis of malignancy encompasses clear referral pathways, access to primary and secondary care services and clinicians' knowledge of signs and symptoms aiding their decision to refer. Professional delay is defined in the literature as ‘the interval between the first professional consultation and definitive histological diagnosis of malignancy'.8 Patient delay is defined as ‘the time between onset of symptoms to seeking an appointment with a dental or medical professional'. Patient delay may be linked to the lack of initial notable symptoms, patient awareness, health seeking behaviours and access to primary care services.9 Mouth cancer referrals are unique in that they are made by both general practitioners (GPs) and general dental practitioners (GDPs). Many referrals from GDPs are picked up during screening in routine examinations in the absence of symptoms; however, many patients do not have access to routine dental care, particularly patients of low socioeconomic backgrounds, so may present to their GP. Recent studies have shown 70% of patients with mouth cancer symptoms are more likely to consult their GP rather than their GDP; however, no significant difference between GPs and GDPs in delay in referral has been reported.10,11 When discussing delays in diagnosis of mouth cancer the majority of cases are related to patient factors; however, professional factors in both primary and secondary care also play an important role.
Cancer Research UK reports late stage diagnosis (Stages 3 and 4) in 62% patients with mouth cancer1 and mortality rates are reported as <30% survival within five years in patients with advanced stage disease.12 Silverman et al. have stated an 80% increase in survival rates if oral cancer is diagnosed and treated earlier, so early referral is critical.13
Current guidelines advise urgent referral to specialist centres for an appointment within two weeks for the following criteria:7,14 persistent ulcer or mass for three weeks or more; unresolved mouth swelling for more than three weeks; unexplained neck lumps; red and white patches with bleeding and pain; unexplained unilateral pain to head and neck for more than four weeks with otalgia; unexplained tooth mobility persisting for more than three weeks; unexplained persistent trismus; sore throat and hoarseness; and any other unexplained signs or symptoms in the mouth that have not resolved. The 28-day faster diagnosis standard pathway has been developed to provide clear guidance on the stages from referral to cancer diagnosis.15
The aim was to review a consecutive cohort of patients over a two-year period with mouth cancer diagnosis; identify those with professional delay; and illustrate the main types of presentations using short case histories and what we can learn to improve this and outcomes for patients with mouth cancer. The cases illustrate potential scenarios where clinicians might misdiagnose the symptoms and signs as benign pathology, hence leading to a delay in diagnosis.
Methods
Inclusion criteria
The sample analysed included new mouth cancer patients with new primaries (both curative and palliative), referred to the Liverpool University Hospital Foundation Trust head and neck multi-disciplinary team (MDT) meeting, from 1 January 2019 to 31 December 2020. The patients were identified from MDT meeting lists provided by MDT coordinators. A sample size of 246 cases was analysed and included a time frame pre and post the COVID-19 pandemic. Information was collected from patient case notes, referral letters and clinical letters scanned onto an electronic document management system (sigma). Professional delay was established through analysing the patient's pathway from first presentation of signs and symptoms to cancer diagnosis, taking into account clinical histories taken from the patient's histories documented in their clinical notes and referral documentation. Delay was considered when red flag signs and symptoms were not referred on a two-week wait pathway and when cases were misdiagnosed initially. The vignettes discussed were selected to provide a broad spectrum of the differing reasons for delays.
Exclusion criteria
Non-mouth cancer referrals, for example, larynx and skin cancers. Patients were omitted from data collection if they had no clinical notes scanned.
Results
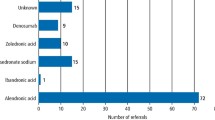
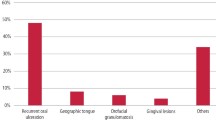
In total, 264 patients diagnosed were identified: 130 referred from GPs, 115 from GDPs and 1 from A&E. Overall, 14% of total referrals (n = 35) had delay in referral of oral cancer, with 48% (n = 17) and 46% (n = 16) from GPs and GDPs, respectively. One case referred had delay from both GP and GDP and another had delay from both their GDP and secondary care. Of the patients where delay was identified, 77% received treatment with curative intent, with 23% palliative. Six common scenarios were identified: 1) sudden onset paraesthesia; 2) dental abscess; 3) temporomandibular joint dysfunction syndrome (TMJD) and abscess; 4) TMJD; 5) trauma/facial fracture; and 6) non-healing socket following dental extraction (Table 1).
Cases
Case 1: sudden onset paraesthesia
An elderly patient was routinely referred by their GDP with ‘sudden onset of paraesthesia to the left lower lip and chin' in February 2020. Medically, they had hypercholesterolemia but were otherwise fit and well, had no allergies and they did not smoke or drink to excess. They lived alone. They were first seen in April 2020 following a visit to A&E with left sided facial swelling, trismus and ear pain. An orthopantomogram (OPG) (Fig. 1) showed an impacted lower left wisdom tooth, which was treated with antibiotics and incision and drainage arranged, with a view to surgically remove the tooth under general anaesthesia. Differential diagnosis was pericoronitis. Telephone consultations were carried out in line with the COVID-19 pandemic, in which the patient reported slight improvement in symptoms. They attended a face-to-face consultation in July 2020, reporting continued trismus, shooting pain to the left ear, dysphagia and weight loss, with no improvement in paraesthesia. Examination revealed swelling to the left cheek, mouth opening of 18 mm and an exophytic soft tissue mass in the left retromolar region. This region was irrigated, further antibiotics prescribed and a computerised tomography (CT) scan ordered (Fig. 2). The CT revealed a potential, advanced-stage mouth cancer affecting the left retromolar fossa, extending into the infratemporal fossa. The provisional staging was T4b N2b Mx. Face-to-face consultation in August revealed a necrotic tumour in the left retromolar area and fixed lymph node in the left submandibular triangle. Fine needle aspiration cytology and soft tissue biopsy confirmed squamous cell carcinoma (SCC). They were admitted to Aintree Hospital for pain management, speech and language therapy (SALT) and dietetic assessment due to increasing dysphagia, poor nutrition and severe pain. MDT discussion determined no surgical intervention and to consider palliative radiotherapy; however, the patient declined this. During their admission, they deteriorated, suffering bouts of delirium and confusion and were discharged to a hospice for end-of-life care. Unfortunately, they passed away in October 2020.
This case highlights professional delay in both primary and secondary care. Patients presenting with red flags, such as sudden onset paraesthesia and neuropathic pain, must be explored further and referred via the two-week wait pathway. Sudden onset paraesthesia should be considered malignant until proven otherwise. The COVID-19 pandemic may have complicated this case due to the lack of face-to-face consultations; however, red flags were missed on multiple occasions and the initial referral for pericoronitis may have introduced tunnel vision, with clinicians missing key red flag symptoms.
Case 2: dental abscess
A middle-aged patient presented to A&E in September 2020 with right-sided facial swelling and a tingling sensation on the right upper lip. They were fit and well, had given up smoking eight years previously (having smoked 15 cigarettes per day for 20 years) and did not consume alcohol. They had a history of toothache in the upper right quadrant for the past eight months, with progressive swelling present for four weeks and had previously seen their GDP where they had two teeth extracted from this quadrant. The swelling increased following this and their dentist prescribed antibiotics with no relief. They attended A&E one week later. An OPG (Fig. 3) revealed multiple carious teeth and initial diagnosis of dental abscess was treated with incision and drainage and antibiotics. Little pus was drained from the region so they were booked an urgent clinic review. On examination, the patient had an extraoral swelling to the right cheek. Intraorally, there was a 5 x 3 cm mass surrounding the upper right premolars. An urgent soft tissue biopsy and extraction of upper right first premolar was performed, which diagnosed a SCC. Magnetic resonance imaging (MRI) (Fig. 4) and CT imaging staged this right maxillary tumour as T4 N2b M0. Due to their age and lack of comorbidities, MDT discussion determined radical palliative surgery with post-operative chemoradiotherapy with curative intent was feasible. The patient underwent dental clearance, right maxillectomy, selective neck dissection, scapula free flap and tracheostomy. Due to the aggressive nature of this tumour, there is a high risk of recurrence.
This is an example of a rapidly progressing aggressive tumour that, if not diagnosed and referred early, surgery with curative intent may not have been possible. The signs and symptoms at initial presentation were similar to that of a dental abscess so was not referred to secondary care and only picked up when the patient self-presented to A&E. Suspicion should arise when facial swellings persist following removal of the presumed causative tooth.
Case 3: TMJD and dental abscess
A middle-aged patient presented to their GP with left-sided jaw and ear pain and difficulty eating, as they felt their jaw was locked, which had progressed over several months. They had multiple telephone consultations throughout August 2020 and a face-to-face review in September 2020. Initial impression was that of TMJD and they were prescribed pain relief and given conservative management advice and advised to contact their GDP. They saw their GDP early November 2020 who took an OPG (Fig. 5) and noted multiple carious teeth and left-sided facial swelling. They were treated with antibiotics and referred non-urgently to secondary care due to inability to access teeth due to trismus. The patient had hypertension, epilepsy (grand mal seizures), anxiety and depression. The patient then presented to A&E in December 2020 after being directly referred by their GDP for a queried maxillary dental abscess. On examination, there was swelling over the left masseter, absolute trismus and haemophysis (ongoing for three months). The patient mentioned a history of 1.5 stone weight loss over the last month. They smoked ten cigarettes a day for the last 30 years and had a history of alcohol excess. They were admitted for review from SALT, dietician, pain team, percutaneous endoscopic gastrostomy insertion and intraoral biopsy. MRI (Fig. 6) showed a locally advanced tumour of the left buccal mucosa/oropharynx, extending to base of tongue, epiglottis, soft palate and nasopharynx, left mandible and parapharynx. Soft tissue biopsy confirmed SCC. Due to the size and local extent of the disease, radical surgery was not possible and palliative radiotherapy was advised at the MDT discussion, with the aim of providing short-term control of their symptoms. Palliative care liaised in their care and they were transferred to a hospice for ongoing support.
There were multiple professional delays in primary care involved in this case, as their symptoms were thought to be related to TMJD and dental abscess. They were not referred on an urgent basis by either their GDP or GP, resulting in the tumour progressing over several months and prognosis very poor. Perhaps if referred sooner, their outcome may have been different, but this is speculative. Patients presenting with absolute trismus must be referred to secondary care urgently for suspected malignancy.
Case 4: TMJD (telephone consultation)
This patient was referred by their GP following a telephone consultation in September 2020, in which they described a history of right-sided jaw pain with right-sided temporal headaches and otalgia, which had gotten much more severe in recent months, with a painless lump in their right neck for two months. They had previously been seen by an ear, nose and throat specialist privately and this was presumed to have been temporomandibular joint in origin. Their GP subsequently routinely referred to the maxillofacial unit. On review in November 2020, an urgent MRI of the head and neck (Fig. 7) was requested to evaluate the swelling to the right neck, which showed a tumour of the right base of the tongue and significant right level II node swelling. Panendoscopy and biopsy of the right base of tongue were completed under general anaesthetic which confirmed SCC and with imaging, was staged as T4a N2b M0 base of tongue. This was not amenable to surgery and the patient is undergoing radical concurrent chemoradiotherapy.
Case 5: trauma with suspected facial fracture
A middle-aged patient had a mechanical fall in July 2018, hitting their face. They had no strong recollection of the incident due to alcohol intake, but reported no significant bruising, with some mild swelling at the time, for which they took nonsteroidal anti-inflammatory drugs. Six weeks later, they attended a walk-in centre, complaining of decreased sensation in their right cheek, which was diagnosed clinically as a fractured zygoma, due to the previous history of fall. There was no evidence of this on plain film imaging (Fig. 8). No referral was made at this point. They saw their GP in October 2018 with ongoing problems, mainly a residual lump on the right cheek and ongoing pain. A hard bony lump in the right infraorbital region was reported, thought to be a callous from healing of fracture. They were subsequently referred routinely to the maxillofacial department who saw the patient in November 2018. A CT (Fig. 9) was requested, as there was some suspicion of an underlying haematoma. Imaging (Fig. 10) revealed an extensive antral carcinoma extending to the right orbit and pathology completed in December 2018 confirmed a poorly differentiated SCC with staging T4a N0 M0. Although extensive, the tumour was amenable to surgery and they underwent radical resection/maxillectomy in January 2019, plus reconstruction with a fibula free flap and adjuvant radiotherapy. At review, there has been no evidence of local or regional recurrence. This is an example of both patient and professional delay.
Case 6: non-healing socket following dental extraction
This middle aged patient was first seen by the maxillofacial department after attending A&E (February 2020) following dental extractions. They had, four weeks previously (January 2020), seen their GDP, who extracted the lower right second and third molars due to increasing mobility, pain and swelling from this region. The pain and swelling worsened post-operatively over the next few weeks. Their GDP referred the patient to A&E as they were concerned of possible post-operative infection. On examination, there was buccal and lingual expansion and an extensive suspicious lesion on the gum in the lower right second and third molar region, evident on OPG imaging (Fig. 11). They had limited mouth opening due to tumour invasion and pain. They were otherwise fit and well, an ex-smoker and did not drink alcohol. An incisional biopsy was performed, which revealed the presence of moderately differentiated SCC of the right retromolar region. MRI (Fig. 12) showed involvement of buccal mucosa, mandible invasion and sublingual space. They underwent right radical neck dissection, mandibulectomy and reconstruction with a fibula free flap, with post-operative radiotherapy due to positive nodes. Surgery was initially delayed as the patient developed flu-like symptoms on their first admission and due to suspected COVID-19 infection, had to isolate for two weeks. Their final staging was T4aN3aM0. Review early 2021 showed extensive recurrence to the right infratemporal fossa with intracranial extension. They were referred to palliative care and sadly passed away not long after. The aetiology of swelling and mobility in teeth in patients of relatively young age should be investigated. Non-healing sockets should be referred urgently on the two-week wait pathway.
Discussion
A number of cases with professional delay were identified, highlighting the diverse presentation of mouth cancers, which may aid clinicians in identifying these signs and symptoms early to ensure prompt referral.
Patients presenting with pain and visible lesions are often referred promptly using the two-week wait pathway. It was those with symptoms such as trismus, jaw pain and altered sensation where most delays were identified. Delays to diagnosis were often due to treatment for other causes, with many cancers initially diagnosed as dental abscesses and temporomandibular joint dysfunction. Other causes of delays may be related to lack of knowledge of the healthcare provider. Longer professional delays are linked to poorer prognosis and worse survival,16 with many patients presenting with late-stage disease not suitable for treatment with curative intent. However, Guggenheimer et al.17 and McGurk et al.18 found that prognosis and staging of mouth cancers is not impacted by delays in diagnosis. There are often delays in patients seeking medical attention in the demographic of patients with head and neck cancer.
Although the timeframe for this study included pre and post COVID-19 pandemic, given the relatively small number of professional delays and lack of detail collected retrospectively, it is not possible to comment on the possible effect of the pandemic on professional delay, nor the impact of telephone/virtual consultations. Further evaluation would be useful to establish whether this impacted patient and professional delay and postal questionnaires could be used to gather this information.
Many patient consultations in both primary and secondary care were conducted over telephone during the COVID-19 pandemic. This may have played a role in delayed diagnosis; however, a number of delays were identified before March 2020. Telephone consultations have proved useful during the COVID-19 pandemic; however, it is difficult to gather all information without conducting a face-to-face examination.
Often, if risk factors such as smoking and alcohol excess are absent in patients considered low risk, symptoms that indicate malignancy may be overlooked. Surgical sieve should be used to establish a differential diagnosis, always including a suspicion of neoplastic causes. It would be prudent to always have a degree of suspicion for malignancy in your differential diagnosis. The importance of regular dental check-ups for mouth cancer screening needs to be emphasised to patients. Taking thorough histories of signs and symptoms at appointments are vital in identifying cancer where obvious lesions are not visible on clinical examination. The clinical presentation of oral malignancies are diverse and it is important not to avoid tunnel vision. That being said, mouth cancer diagnosis is difficult for even the most experienced clinicians; if there is any doubt, referral is always sensible.
Limitations
It was difficult to acquire full information on the reason for delay in those patients referred to the peripheral hospitals, as a number of referral letters and additional details were not scanned into the patients notes accessible to the regional centre.
Recommendations
Professional delay accounted for only 14% in patients referred with the diagnosis of mouth cancer. The common clinical presentations in those with delay were sudden onset paraesthesia, dental abscess, TMJD and dental abscess, TMJD (telephone consultation), trauma with suspected facial fracture, and non-healing socket following dental extraction. It is hoped that the cases illustrated in this article serve to highlight the types of case presentations most likely to lead to a diagnostic dilemma and potential clinician delay. Further education is needed for both GPs and GDPs on mouth cancer detection and swift diagnosis may be improved with a more collaborative working approach between healthcare providers and increasing practitioner and patient awareness.
References
Cancer Research UK. Head and neck cancer mortality statistics. 202. Available at https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/head-and-neck-cancers/mortality (accessed March 2022).
Oral Health Foundation. The State of Mouth Cancer UK Report 2022. Available at https://www.dentalhealth.org/thestateofmouthcancer (accessed March 2022).
Office for National Statistics. Cancer registration statistics, England: 2020. Information request made by Oral Health Foundation. Available at https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/cancerregistrationstatisticsengland/previousReleases (accessed November 2022).
Public Health Scotland. Cancer Statistics. 2020. Information request for cancer incidences for Scotland made by Oral Health Foundation. Available at https://www.isdscotland.org/Health-Topics/Cancer/Cancer-Statistics/ (accessed November 2022).
Public Health Wales. Cancer incidence in Wales 2002-2019. 2022. Information request for latest cancer incidences for Wales made by Oral Health Foundation. Available at https://phw.nhs.wales/services-and-teams/welsh-cancer-intelligence-and-surveillance-unit-wcisu/cancer-survival-in-wales-2002-2019/ (accessed November 2022).
Northern Ireland Cancer Registry. Official Statistics. 2022. Information request for latest cancer incidences for Northern Ireland made by Oral Health Foundation. Available athttps://www.qub.ac.uk/research-centres/nicr/CancerInformation/official-statistics/ (accessed November 2022).
National Institute for Health and Care Excellence. Suspected cancer: recognition and referral. 2015. Available at https://www.nice.org.uk/guidance/ng12 (accessed June 2021).
Yu T, Wood R E, Tenenbaum H C. Delays in diagnosis of head and neck cancers. J Can Dent Assoc 2008; 74: 61.
Rogers S N, Glen P, Robinson A, Lowe D, Grieveson B, Edwards D. A survey of general dental practitioners in Merseyside regarding urgent appointments and suspected cancer referrals. Prim Dent Care 2008; 15: 25-30.
Langton S, Cousin G C S, Plüddemann A, Bankhead C R. Comparison of primary care doctors and dentists in the referral of oral cancer: a systematic review. Br J Oral Maxillofac Surg 2020; 58: 898-917.
Rogers S N, Pabla R, McSorley A, Lowe D, Brown J S, Vaughan E D. An assessment of deprivation as a factor in the delay in presentation, diagnosis and treatment in patients with oral and oropharyngeal squamous cell carcinoma. Oral Oncol 2007; 43: 648-655.
Grafton-Clarke C, Chen K W, Wilcock J. Diagnosis and referral delays in primary care for oral squamous cell cancer: a systematic review. Br J Gen Pract 2019; DOI: 10.3399/bjgp18X700205.
Silverman S, Kerr A R, Epstein J B. Oral and pharyngeal cancer control and early detection. J Cancer Educ 2010; 25: 279-281.
Scottish Government. Scottish referral guidelines for suspected cancer. 2019. Available at https://www.gov.scot/publications/scottish-referral-guidelines-suspected-cancer-january-2019 (accessed March 2022).
NHS West Midlands Cancer Alliance. Implementing a Timed Head and Neck Diagnostic Pathway. 2022. Available at https://wmcanceralliance.nhs.uk/images/Documents/Best_practice_timed_pathway/Head_and_Neck_Faster_Diagnosis_Pathway_Guidance_v3.2_FINAL.pdf (accessed November 2022).
Kantola S, Jokinen K, Hyrynkangas K, Mäntyselkä P, Alho O P. Detection of tongue cancer in primary care. Br J Gen Pract 2001; 51: 106-111.
Guggenheimer J, Verbin R S, Johnson J T, Horkowitz C A, Myers E N. Factors delaying the diagnosis of oral and oropharyngeal carcinomas. Cancer 1989; 64: 932-935.
McGurk M, Chan C, Jones J, O'Regan E, Sherriff M. Delay in diagnosis and its effect on outcome in head and neck cancer. Br J Oral Maxillofacial Surg 2005; 43: 281-284.
Author information
Authors and Affiliations
Contributions
Marie Daniel conceived and designed analysis, collected data, performed data analysis and wrote the paper. Simon N Rogers contributed to design, data analysis and writing of the paper.
Corresponding author
Ethics declarations
There are no conflicts of interest to declare.
This study was approved by Liverpool University Hospital NHS Foundation Trust Audit Department (CAMS registration number 9052). Patient consent is not applicable as this is a retrospective review of anonymised data with removal of personal identifiers.
Rights and permissions
About this article
Cite this article
Daniel, M., Rogers, S. Professional delays in referral of patients with mouth cancer: six case histories. Br Dent J 233, 1003–1008 (2022). https://doi.org/10.1038/s41415-022-5304-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-022-5304-5
This article is cited by
-
Do we recognize oral cancer? Primary professional delay in diagnosis of oral squamous cell carcinoma
Clinical Oral Investigations (2024)