Abstract
Malnutrition is prevalent in patients with head and neck cancer (HNC) at diagnosis but can occur at any stage of the treatment pathway. The impact of disease burden and treatment side effects can lead to altered anatomy, compromised quality and quantity of saliva and impaired swallowing function, which can result in deleterious effects on nutritional status. Optimising nutrition status is critical, as malnutrition is adversely associated with treatment tolerance and outcomes, wound healing, morbidity, mortality, quality of life and survival. Dietitians are integral members of the HNC multidisciplinary team and are uniquely qualified in the assessment, management and optimisation of nutritional status across the care pathway. This includes providing informational counselling to patients and carers on the short- and long-term nutritional impact of planned treatments alongside multidisciplinary members. Dietitians lead on the recommendation, provision and monitoring of nutrition support, which can be via the oral, enteral or parenteral route. Oral nutrition support includes dietary counselling, nourishing dietary, food fortification advice and high energy/protein oral nutritional supplements. Enteral nutrition support, or tube feeding, can be required on a short- and/or long-term basis and dietitians support appropriate decision-making for the type of tube and timing of placement across the care pathway.
Key points
-
Head and neck cancer (HNC) is a multifaceted disease requiring multi-disciplinary intervention. The impact of tumour burden and treatment side effects can lead to altered anatomy, impaired swallowing function and deleterious effects on nutritional status. Many patients are at risk of malnutrition which can occur at any stage of the care pathway.
-
Dietitians are core members of the HNC multi-disciplinary team and lead on the nutritional management of patients at any stage of the treatment pathway, from diagnosis until death, palliation and/or survivorship.
-
Nutrition support is vital in the prevention and treatment of malnutrition. This includes dietary counselling, nourishing dietary advice and the provision of high energy/protein oral nutritional supplements, as well as enteral tube feeding on a short- and/or long-term basis when indicated. Dietitians work alongside restorative dentists to balance nutritional needs with prevention of dental caries.
Similar content being viewed by others
Introduction
Head and neck cancer (HNC) is multifaceted in nature. The aetiology of the disease and consequences of treatment have a profound impact on nutritional status and risk of malnutrition. This includes impact on functional swallowing status and the ability to take adequate nutrition orally and/or via alternative nutrition support. Nutritional intervention is integral in preventing disease- and treatment-related malnutrition and/or weight loss. Dietitians are healthcare professionals that are uniquely qualified to translate scientific information about food and nutrition into practical dietary advice. Within HNC, specialist dietitians are integral members of the multidisciplinary team (MDT) and lead on assessing patients' nutritional status and needs, alongside providing individualised nutritional advice. This often includes the provision of nutritional support throughout the patient's journey, from diagnosis to survivorship, palliation and/or death.1
Malnutrition and survival
Patients with HNC are at a high risk of malnutrition which takes place when a negative energy balance occurs due to reduced intake or uptake of nutrients, resulting in unintentional weight loss.2 This can occur at any stage of the patient pathway and has been reported in 60% of HNC patients before commencing treatment,3 increasing to up to 86% at the end of chemoradiotherapy.4 Malnutrition is common due to the impact of the disease site, tumour burden and side effects of treatment modalities (see Table 1).5,6
Recent studies have reported that patients who are overweight/obese at presentation can be at a higher risk of becoming malnourished during treatment.7 Malnutrition is adversely associated with treatment tolerance, wound healing, surgical complications, morbidity, mortality, quality of life (QofL) and survival.6 Furthermore, weight loss is a predictor for poor survival and treatment tolerance.8 All MDT members can support screening for malnutrition and refer to the dietitian for assessment and intervention at the earliest opportunity to prevent further decline.9
Cachexia in cancer is a complex disease characterised by unintentional weight loss, loss of appetite and muscle wasting. Cachexia differs from conventional starvation where lean muscle is preserved and adipose tissue is mainly affected. It is associated with metabolic abnormalities leading to an overall catabolic state and systemic inflammation. Prevalence in HNC can range from 6.1% at diagnosis to 41% post treatment.10 It is challenging to manage, as aggressive nutritional intervention is insufficient to reverse and/or prevent further loss, leading to functional impairment.11
Beyond weight and body mass index, dietitians can also undertake an assessment of body composition to analyse the nature of overall weight loss and differentiate between loss of adipose tissue and loss of skeletal muscle. Commonly used methods include measurement of hand-grip strength, bioelectrical impedance analysis and skinfold thickness. When accessible, dual-energy x-ray absorptiometry and computer tomography can be used for in-depth body composition assessment.12 Sarcopenia is a condition characterised as the loss of muscle mass and strength and is associated with reduced survival. Prevalence in HNC has been reported to range from 6.6-64.6% before commencing radiotherapy with curative intent ± other treatment modalities increasing to 12.4-65.8% post-treatment.13
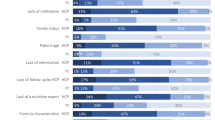
Impact of the dietitian and nutritional counselling
Specialist dietitians are integral members of the HNC MDT and provide individualised nutritional advice throughout the patient's continuum of care. UK standards state that all HNC units should have a specialist dietitian with at least 50% of their clinical time dedicated to HNC.1 Nutritional counselling has an important role to play in the management of HNC, with positive effects reported on nutritional intake, nutritional status, clinical outcomes and QofL.3 Individualised nutritional counselling given by a dietitian has been reported as more efficacious compared to generalised advice given by nursing staff or no counselling.3,14,15,16 Furthermore, behaviour change training is a key skill of clinicians working with patients with complex needs. Dietitians are often supported with undertaking advanced communication skills courses. The effectiveness of incorporating psychological intervention to nutritional care is gaining momentum. In Australia, the Eating As Treatment trial investigated the use of a dietitian delivered behaviour change intervention, with the goal of reducing malnutrition in HNC patients undergoing radiotherapy. Patients receiving the intervention had shorter and fewer unplanned hospital admissions alongside statistically significantly better nutritional status scores.17
Dietitians can also extend their scope of practice in the HNC MDT and train to become advanced clinical practitioners.18,19 This may include training to place enteral feeding tubes, prehabilitation programmes and undertaking post-graduate courses to become a non-medical supplementary prescriber (NMP).19 Dietitians are well-placed to become NMPs in the radiotherapy setting, owing to regularly reviewing patients and identifying barriers to taking adequate nutrition early. This means that dietitians can prescribe medications such as analgesia and anti-emetics to optimise tolerance of nutritional interventions.19
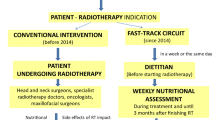
The role of the dietitian at each point of the care pathway
The dietitian can be referred to at any point of the care pathway (Fig. 1). The frequency of contact depends on individualised needs.1,9
Screening and referral
Patients usually present initially to HNC units, where any issues with ability to meet nutritional needs are screened and identified by core MDT members. Following this, any patient identified at risk of malnutrition should be referred promptly to the dietitian for a baseline nutritional assessment and advice to prevent deterioration. This may include the provision of nutritional support to treat malnutrition via the appropriate feeding route and advice on diagnosing and treating refeeding syndrome (adverse metabolic changes that can occur when nutrition is re-introduced in those that are malnourished or in a starved state)2 where appropriate. It has been reported that early intervention from dietetics has been associated with improved clinical outcomes.20
MDT discussion
After initial referral to the HNC unit, cases are discussed in the HNC MDT meeting. Specialist dietitians can provide input to support treatment decision-making, especially when proposed treatment plans are likely to impact on functional swallowing and nutritional status, with anticipated requirements for enteral tube feeding.
Pre-treatment
Following the MDT meeting and decision outcomes for treatment have been made, a key role of the dietitian is to prepare the patient for the proposed treatment. All patients that are planned for treatment that will affect nutritional status should be seen in a pre-treatment appointment.1 The purpose of this appointment is to: provide informational counselling on the likely impact of proposed treatment on eating, drinking and nutritional status; conduct a baseline nutritional assessment (if not prior conducted); and, when applicable, provide nutritional advice and intervention to prevent decline.9
For patients undergoing major surgery and that are severely malnourished, this may include recommending pre-operative nutritional support with or without an admission to hospital to optimise nutritional status, as inadequate oral intake for >14 days is associated with higher mortality.21,22,23
For patients undergoing radiotherapy, chemoradiotherapy, or any treatment leading to enteral feeding requirements, the dietitian should discuss enteral tube feeding options. This may include prophylactic gastrostomy placement when indicated and in conjunction with locally agreed criteria and service provisions in individual units.24
On-treatment
Surgery in HNC often involve resections that impact on the anatomy and physiology required for safe swallow function. Therefore, many patients require enteral feeding postoperatively on a short- or long-term basis. All patients requiring nutritional support should be reviewed by the dietitian at regular intervals during their inpatient stay. Enteral feeding, when indicated, should be initiated without delay and within 24 hours postoperatively25,26 as part of enhanced recovery after surgery protocols, which aim to accelerate recovery after surgery by facilitating early return to function and reduced stress through implementing multimodal care pathways.21 Dietitians attend ward rounds, meetings and collaborate with MDT members. For example, if/when patients can resume oral intake, dietitians liaise with the surgeons and speech and language therapists (SLTs) on the type and timing of diet that can be resumed.
Oncological treatments for HNC include radiotherapy/proton beam therapy which can be used in conjunction with surgery (adjuvant) and or chemotherapy (neoadjuvant/concurrent) or as a single-modality treatment. The side effects of radiotherapy take a cumulative effect and are detailed in Table 1.27 The extent of side effects impacting on the ability to take adequate oral nutrition depends on the treatment site, dose and fields. Maintaining weight stability is crucial during radiotherapy treatment due to the precise nature of mask fitting and accuracy of the treatment plan based on body measurements. Significant weight loss during treatment can result in ill-fitting masks and therefore risks treatment being stopped and/or re-planned.28 Therefore, any deficit should be identified early and patients should be reviewed by the dietitian at least once a week, ideally twice-weekly during treatment.9 Dietitians also support the MDT in encouraging adherence to treatments, such as analgesia, to alleviate side effects and in turn, optimise tolerance to nutrition support.
Post treatment
Dietitians continue to review patients either in the acute setting or may refer to the community dietitian for patients requiring home enteral feeding. Some patients require long-term enteral feeding due to extensive treatment. Dietitians can signpost these patients to support groups and ensure feeding regimens are optimised for QofL.
The goal of dietetic intervention following treatment is to rehabilitate patients back to their baseline diet where feasible.9 This may include reducing the provision of enteral feeding while increasing oral intake as feasible/safe with guidance from SLTs. Side effects can be experienced on a short- and long-term basis and ongoing nutritional support may be required. Late side effects can also present, such as osteoradionecrosis, stenosis and dysphagia, which can lead to ongoing poor nutritional intake.27
Palliation
Recurrence is common in HNC and patients may be referred for palliative care and/or further treatments.29 Nutritional status can deteriorate with disease progression and the benefits of nutrition support should account for prognosis. Dietitians work with patients, carers and MDT members to discuss, consider and balance the risks, benefits and appropriateness of initiating nutritional support, especially invasive forms, with the goal to uphold QofL and comfort.9,30
Survivorship
Where patients are no longer at risk of malnutrition and as part of survivorship, dietitians can provide healthy eating and physical activity advice on an individualised basis.9,30
Nutrition support
A major role of the dietitian in HNC is initiating, monitoring and reviewing nutritional support requirements. There are three main forms of nutrition support and Figure 2 outlines how decision-making is made:2,9,24
-
1.
Oral (by assessing current intake and optimising this by offering nourishing dietary advice with or without the use of oral nutritional supplements [ONS])
-
2.
Enteral (by delivery of nutrition via a tube that enters the gastrointestinal tract when oral intake is either contraindicated or insufficient to meet nutritional requirements)
-
3.
Parenteral (by delivery of nutrition via an intravenous route when the gastrointestinal tract is inaccessible or compromised/contraindicated).
Oral nutrition support (ON) is first line practice to prevent further nutritional decline and/or meet existing deficiencies if the oral route is not contraindicated (for example, nil by mouth post surgery or dysphagia). Interventions include providing food fortification, nourishing dietary advice and use of ONS. ONS are high protein/energy formulas, available as liquid, ready-to-drink bottles or powdered to make up with milk or water.2 The benefits include the energy-dense formula (as high as 4 kcal/ml), of which most are fortified with vitamins and minerals, making them 'nutritionally complete' in specified volumes, alongside their convenience and wide product range available on prescription. Due to the nature of disease location and side effects of treatment, meeting nutritional requirements via a food-first approach only is often unfeasible. During these periods, energy-dense ONS taken alongside are an effective means to supplement energy/protein deficits.9
A randomised controlled trial investigated the impact of use of ONS in HNC patients undergoing radiotherapy or radiotherapy plus systemic treatment and receiving nutritional counselling. It was reported that the use of ONS resulted in a statistically significant smaller loss of body weight, higher protein-calorie intake, improved treatment tolerance and improved QofL compared to nutritional counselling alone.31
The disadvantages of ONS include that the majority of products available are sweet flavour options (with limited savoury options available), thus can be high in sucrose and highly cariogenic.32 The volume and frequency of supplements therefore needs to be monitored alongside appropriate preventative measures, including oral hygiene, dental care professional support and fluoride regimes, and also on patients with poorly-controlled diabetes (Table 2). Nutritional needs are met with frequent consumption of ONS products which are carbohydrate-rich, with some patients drinking these over a protracted period of time: five to seven times daily. This creates an oral environment which encourages plaque build-up, which in turn causes demineralisation of tooth structure and dental caries. In patients with short-term or long-term xerostomia, caries can progress rather fast as these patients also have reduced oral clearance and reduced buffering capacity.33 The priority is to ensure optimum nutrition but it is also essential to ensure that the risk of dental caries is reduced by supportive strategies given by the restorative dentist and dental care professionals. On patients receiving high doses of radiotherapy, dental extractions should be avoided, so preventing a deterioration of the dentition is paramount. Additionally, it can be challenging to provide dental restorations for patients with trismus as a side effect of treatment for HNC, so prevention of dental disease is in the patient's best interest.33
Ready-to-drink ONS have been reported to range between 6.6-27.2 g of sugar/serving; powder mixed with 200 ml full-fat milk ranged between 16.4-35 g sugar/serving; and ONS 'shots' ranged between 0-4 g of sugar/serving.34 ONS 'shots' can therefore be a good option alongside oral diet/ready-to-drink ONS/powder, as they are lower in sugar. However, they are not generally recommended in volumes aiming to meet a significant proportion of estimated nutritional requirements (≥50%) as they are not nutritionally complete, are often considered less palatable by patients affecting compliance and can have adverse gastrointestinal effects. Malnutrition and dental caries have both been reported to have negative impacts on QofL.35 Dietitians can work closely with restorative dentistry (as per Table 2), diabetes clinical nurse specialists and other MDT members to optimise diet and the safe use of ONS alongside dental health and blood glucose control. Evidence for HNC is limited but follows first principles with regards to dental hygiene:36
-
Caries is caused by the interaction of fermentable carbohydrates and plaque biofilm on a susceptible tooth surface37
-
Fermentable carbohydrates include sucrose, glucose, lactose and fructose. Sucrose is especially cariogenic due to its effect on plaque biofilm development, as well as being fermentable38
-
Caries is preventable
-
Good oral hygiene is key for caries prevention
-
Tailored fluoride regimes are essential on patients with HNC
-
Regular reviews with restorative dentists and dental care professionals are essential to intervene at early stages of dental disease
-
Treatments for HNC can cause xerostomia. While xerostomia does not cause dental caries per se, reduced quality and quantity of saliva reduces the remineralisation potential of early caries lesions.
Enteral nutrition support is often required in HNC. This may be as early as initial presentation due to the impact of disease location affecting swallowing function and/or the ability to take adequate nutrition orally. Some patients may be advised to be nil by mouth (NBM) due to aspiration risk by SLT and thus will need immediate placement of an enteral feeding tube. Enteral feeding may be used as the sole source of nutrition (for example, when NBM status) or on a partial basis to supplement oral intake (for example, when able to tolerate some oral diet/fluids but inadequate to meet full nutritional requirements).9,24
Enteral feeding tube options include those for the short-term (generally considered <4 weeks but not limited to this time frame) and long-term (≥4 weeks).2 Short-term options include naso-enteral tubes such as naso-gastric, naso-jejunal, oesophageal-fistulae and orogastric. Long-term options include gastrostomy tube feeding, such as percutaneous endoscopic gastrostomy (PEG) (see Figure 3), radiologically inserted gastrostomy (RIG) (see Figure 4) or surgical gastrostomy/jejunostomy. Decision-making for the type of tube placed should account for the anticipated length of enteral feeding (with consideration to tumour type, size, location and treatment plan), patient choice and local resources/policy.24 In some centres, gastrostomies may be placed before commencing HNC treatment if it is anticipated that treatment may result in requiring enteral feeding for a long-term period. Controversy exists for placement of prophylactic gastrostomy before radiotherapy/chemoradiotherapy and the evidence base remains inconclusive.39,40 Guidelines have been developed to support appropriate decision-making, which often include tumour stage, site, age, nutritional status, pre-existing dysphagia, performance status and impact of planned treatment.7,24,41,42 Dietitians are key stakeholders for supporting appropriate decision-making within the MDT, which has led to the development of dietetic-led gastrostomy services in some centres. This enables dietitians to lead on screening, assessing and counselling patients to support appropriate decision-making for gastrostomy insertion and removal, working alongside gastroenterology and radiology departments and HNC MDT members.43
Clinical photographs of a PEG tube. a) Depicts a patient's abdominal site with a 15 French Freka PEG tube (Fresenius Kabi) in situ which was placed endoscopically. b) Depicts a patient administering feed through his 15 French Freka PEG tube (Fresenius Kabi) by the 'bolus method'. A syringe is used to draw enteral feed/oral nutritional supplements and then screwed onto the end of the PEG. The PEG tube is unclamped and feed is delivered. c, d) Depicts a demonstration model of a 15 French Freka PEG tube (Fresenius Kabi). The end of the tube has a cap and a clamp is placed on the tube lumen to prevent leakage. An external triangular fixator plate is clamped close to the skin to keep the PEG in position. The tube is retained by an internal bumper/disc. The patient is advised to advance and rotate the tube weekly after the stoma tract has developed (10-14 days post insertion) to prevent 'buried bumper syndrome' (when the internal bumper becomes buried within the wall of the abdomen)
Clinical photograph of a RIG tube. a) Depicts a patient's abdominal site with a 14 French MIC* gastrostomy feeding tube (Avanos) in situ which was placed radiologically. b) Depicts a patient administering feed through his 14 French MIC* gastrostomy feeding tube (Avanos) by the 'bolus method'. A syringe is used to draw enteral feed/oral nutritional supplements and then screwed onto the end of the RIG to deliver the feed. c, d) Depicts a demonstration model of a 12 French MIC* gastrostomy feeding tube (Avanos). The end of the tube has a feeding port and a luer lock balloon inflation valve. The feeding port is capped to prevent leakage. An external retention ring is kept close to the skin to keep the RIG in position. The tube is retained by an internal silicone balloon. The balloon is filled with water to keep the tube in situ. Once the tract is developed two weeks post RIG insertion, the patient is then advised to change the water weekly thereafter
Parenteral nutrition is seldom used in HNC as most patients have an accessible gastrointestinal tract and can tolerate enteral nutrition. However, it should be considered when clinically appropriate and in consultation with specialist gastroenterology nutrition teams in hospital settings.
Consideration of dental care alongside nutritional intervention across the pathway
Dental condition is a risk factor for weight loss in HNC at the outset.44 Dietitians work alongside restorative dentists and the wider MDT to ensure nutritional needs are met while balancing the importance of oral hygiene and prevention of dental caries.33 This is further explained by the risks outlined in Table 2 and strategies to mitigate these.36,45
Conclusion
The aetiology of HNC itself, and treatments, can lead to altered anatomy and impaired swallowing function which can compromise nutritional status. Many patients are at risk of malnutrition and require nutritional support. Dietitians have a key role in assessing and treating malnutrition with the provision of nutrition support. Due to the limitations on texture and tolerance of oral diet, use of ONS, nourishing dietary advice and enteral feeding are often required. Dietitians can work with restorative dentists to promote safe consumption of ONS and other high-cariogenic food/drink and in addition, can help with rehabilitation back to a baseline diet alongside SLT when feasible, to reduce reliance on ONS.
References
Schache A, Kerawala C, Ahmed O et al. British Association of Head and Neck Oncologists (BAHNO) standards 2020. J Oral Pathol Med 2021; 50: 262-273.
National Institute for Health and Care Excellence. Nutrition support for adults: oral nutrition support, enteral tube feeding and parenteral nutrition. 2006. Available at https://www.nice.org.uk/guidance/cg32 (accessed October 2022).
Ravasco P, Monteiro-Grillo I, Marques Vidal P, Camilo M E. Impact of nutrition on outcome: a prospective randomized controlled trial in patients with head and neck cancer undergoing radiotherapy. Head Neck 2005; 27: 659-668.
Orell H, Schwab U, Saarilahti K, Österlund P, Ravasco P, Mäkitie A. Nutritional Counseling for Head and Neck Cancer Patients Undergoing (Chemo) Radiotherapy - A Prospective Randomized Trial. Front Nutr 2019; 6: 22.
Bossi P, Delrio P, Mascheroni A, Zanetti M. The Spectrum of Malnutrition/Cachexia/Sarcopenia in Oncology According to Different Cancer Types and Settings: A Narrative Review. Nutrients 2021; 13: 1980.
Van Bokhorst-de van der Schueren M A, van Leeuwen P A, Sauerwein H P, Kuik D J, Snow G B, Quak J J. Assessment of malnutrition parameters in head and neck cancer and their relation to postoperative complications. Head Neck 1997; 19: 419-425.
Brown T, Ross L, Jones L, Hughes B, Banks M. Nutrition outcomes following implementation of validated swallowing and nutrition guidelines for patients with head and neck cancer. Support Care Cancer 2014; 22: 2381-2391.
Langius J A E, Bakker S, Rietveld D H F et al. Critical weight loss is a major prognostic indicator for disease-specific survival in patients with head and neck cancer receiving radiotherapy. Br J Cancer 2013; 109: 1093-1099.
Talwar B, Donnelly R, Skelly R, Donaldson M. Nutritional management in head and neck cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 2016; DOI: 10.1017/S0022215116000402.
Kwon M, Kim R B, Roh J-L et al. Prevalence and clinical significance of cancer cachexia based on time from treatment in advanced-stage head and neck squamous cell carcinoma. Head Neck 2017; 39: 716-723.
Peixoto da Silva S, Santos J M O, Costa E Silva M P, Gil da Costa R M, Medeiros R. Cancer cachexia and its pathophysiology: links with sarcopenia, anorexia and asthenia. J Cachexia Sarcopenia Muscle 2020; 11: 619-635.
Ferrão B, Neves P M, Santos T, Capelas M L, Mäkitie A, Ravasco P. Body composition changes in patients with head and neck cancer under active treatment: a scoping review. Support Care Cancer 2020; 28: 4613-4625.
Findlay M, White K, Stapleton N, Bauer J. Is sarcopenia a predictor of prognosis for patients undergoing radiotherapy for head and neck cancer? A meta-analysis. Clin Nutr 2021; 40: 1711-1718.
Isenring E A, Capra S, Bauer J D. Nutrition intervention is beneficial in oncology outpatients receiving radiotherapy to the gastrointestinal or head and neck area. Br J Cancer 2004; 91: 447-452.
Isenring E A, Bauer J D, Capra S. Nutrition support using the American Dietetic Association medical nutrition therapy protocol for radiation oncology patients improves dietary intake compared with standard practice. J Am Diet Assoc 2007; 107: 404-412.
Van den Berg M G A, Rasmussen-Conrad E L, Wei K H, Lintz-Luidens H, Kaanders J H A M, Merkx M A W. Comparison of the effect of individual dietary counselling and of standard nutritional care on weight loss in patients with head and neck cancer undergoing radiotherapy. Br J Nutr 2010; 104: 872-877.
Britton B, Baker A L, Wolfenden L et al. Eating As Treatment (EAT): A Stepped-Wedge, Randomized Controlled Trial of a Health Behaviour Change Intervention Provided by Dietitians to Improve Nutrition in Patients With Head and Neck Cancer Undergoing Radiation Therapy (TROG 12.03). Int J Radiat Oncol Biol Phys 2019; 103: 353-362.
Simmance N, Cortinovis T, Green C et al. Introducing novel advanced practice roles into the health workforce: Dietitians leading in gastrostomy management. Nutr Diet 2019; 76: 14-20.
NHS England. Supplementary prescribing by Dietitians. Available at https://www.england.nhs.uk/ahp/med-project/dietitians/ (accessed October 2022).
Wei J, Wu J, Meng L et al. Effects of early nutritional intervention on oral mucositis in patients with radiotherapy for head and neck cancer. QJM 2020; 113: 37-42.
Weimann A, Braga M, Carli F et al. ESPEN practical guideline: Clinical nutrition in surgery. Clin Nutr 2021; 40: 4745-4761.
Sandström R, Drott C, Hyltander A et al. The effect of postoperative intravenous feeding (TPN) on outcome following major surgery evaluated in a randomized study. Ann Surg 1993; 217: 185-195.
Von Meyenfeldt M F, Meijerink W J, Rouflart M M, Builmaassen M T, Soeters P B. Perioperative nutritional support: a randomised clinical trial. Clin Nutr 1992; 11: 180-186.
National Institute for Health and Care Excellence. Cancer of the upper aerodigestive tract: assessment and management in people aged 16 and over. 2016. Available at https://www.nice.org.uk/guidance/ng36 (accessed May 2021).
Kompan L, Kremžvar B, Gadžvijev E, Prošek M. Effects of early enteral nutrition on intestinal permeability and the development of multiple organ failure after multiple injury. Intensive Care Med 1999; 25: 157-161.
Perel P, Yanagawa T, Bunn F, Roberts I, Wentz R, Pierro A. Nutritional support for head-injured patients. Cochrane Database Syst Rev 2006; DOI: 10.1002/14651858.CD001530.pub2.
Sroussi H Y, Epstein J B, Bensadoun R-J et al. Common oral complications of head and neck cancer radiation therapy: mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med 2017; 6: 2918-2931.
Stauch Z, Zoller W, Tedrick K et al. An evaluation of adaptive planning by assessing the dosimetric impact of weight loss throughout the course of radiotherapy in bilateral treatment of head and neck cancer patients. Med Dosim 2020; 45: 52-59.
Cocks H, Ah-See K, Capel M, Taylor P. Palliative and supportive care in head and neck cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 2016; DOI: 10.1017/S0022215116000633.
Muscaritoli M, Arends J, Bachmann P et al. ESPEN practical guideline: Clinical Nutrition in cancer. Clin Nutr 2021; 40: 2898-2913.
Cereda E, Cappello S, Colombo S et al. Nutritional counseling with or without systematic use of oral nutritional supplements in head and neck cancer patients undergoing radiotherapy. Radiother Oncol 2018; 126: 81-88.
Stillhart A, Wegehaupt F J, Nitschke I, Attin T, Srinivasan M. Cariogenic potential of oral nutritional supplements measured by intraoral plaque pH telemetry. Clin Nutr 2021; 40: 3448-3453.
Samim F, Epstein J B, Zumsteg Z S, Ho A S, Barasch A. Oral and dental health in head and neck cancer survivors. Cancers Head Neck 2016; 1: 14.
Coffey N, O' Leary F, Burke F et al. "Oral Nutritional Supplements: Sugar Content and Potential Dental Implications". Gerodontology 2021; DOI: 10.1111/ger.12592.
De Pauli Paglioni M, Palmier N R, Prado-Ribeiro A C et al. The impact of radiation caries in the quality of life of head and neck cancer patients. Support Care Cancer 2020; 28: 2977-2984.
Butterworth C, McCaul L, Barclay C. Restorative dentistry and oral rehabilitation: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 2016; DOI: 10.1017/S0022215116000414.
Sheiham A, James W P T. A reappraisal of the quantitative relationship between sugar intake and dental caries: the need for new criteria for developing goals for sugar intake. BMC Public Health 2014; 14: 863.
Du Q, Fu M, Zhou Y et al. Sucrose promotes caries progression by disrupting the microecological balance in oral biofilms: an in vitro study. Sci Rep 2020; 10: 2961.
Nugent B, Lewis S, O'Sullivan J M. Enteral feeding methods for nutritional management in patients with head and neck cancers being treated with radiotherapy and/or chemotherapy. Cochrane Database Syst Rev 2013; DOI: 10.1002/14651858.CD007904.pub3.
Paleri V, Patterson J, Rousseau N et al. Gastrostomy versus nasogastric tube feeding for chemoradiation patients with head and neck cancer: the TUBE pilot RCT. Health Technol Assess 2018; 22: 1-144.
Brown T E, Getliffe V, Banks M D et al. Validation of an updated evidence-based protocol for proactive gastrostomy tube insertion in patients with head and neck cancer. Eur J Clin Nutr 2016; 70: 574-581.
Talwar B, Findlay M. When is the optimal time for placing a gastrostomy in patients undergoing treatment for head and neck cancer? Curr Opin Support Palliat Care 2012; 6: 41-53.
Talwar B P, Hewitt R. Nutrition and dietetic-led gastrostomy pathway of care for insertion and removal contributes to outcomes. Proc Nutr Soc 2009; DOI: 10.1017/S0029665109002067.
Devoize L, Dumas C, Lambert C et al. Poor dental condition is a factor of imbalance of the nutritional status at the outset of management of head and neck cancer. Clin Oral Investig 2022; 26: 1251-1259.
Wu L-L, Gao Q-P, Fu Q-Y, Geng K. Analysis of the risk factors of radiation-induced caries in patients with head and neck cancer. Hua Xi Kou Qiang Yi Xue Za Zhi 2019; 37: 87-91.
Marx R E. Osteoradionecrosis: A new concept of its pathophysiology. J Oral Maxillofac Surg 1983; 41: 283-288.
Zick S M, Snyder D, Abrams D I. Pros and Cons of Dietary Strategies Popular Among Cancer Patients. Oncology (Wiliston Park) 2018; 32: 542-527.
Nadelman P, Magno M B, Masterson D, da Cruz A G, Maia L C. Are dairy products containing probiotics beneficial for oral health? A systematic review and meta-analysis. Clin Oral Investig 2018; 22: 2763-2785.
Restorative Dentistry UK. Predicting and Managing Oral and Dental Complications of Surgical and Non-Surgical Treatment for Head and Neck Cancer: A Clinical Guideline. 2016. Available at https://www.restdent.org.uk/uploads/RD-UK%20H%20and%20N%20guideline.pdf (accessed October 2022).
Kovarik J P, Voborna I, Barclay S et al. Osteoradionecrosis after treatment of head and neck cancer: a comprehensive analysis of risk factors with a particular focus on role of dental extractions. Br J Oral Maxillofac Surg 2022; 60: 168-173.
The Royal College of Surgeons of England. The Oral Management of Oncology Patients Requiring Radiotherapy, Chemotherapy and/or Bone Marrow Transplantation: Clinical Guidelines. 2018. Available at https://www.rcseng.ac.uk/dental-faculties/fds/publications-guidelines/clinical-guidelines/ (accessed July 2022).
Parahoo R S, Semple C J, Killough S, McCaughan E. The experience among patients with multiple dental loss as a consequence of treatment for head and neck cancer: A qualitative study. J Dent 2019; 82: 30-37.
Acknowledgements
We are grateful to Dharmesh Patel for his support with developing the infographics in this article. We thank the UCLH Head and Neck dietitians for reviewing the draft manuscript. We are deeply grateful to the patients who contributed to this article by agreeing to have clinical photographs of their feeding tubes included. We are grateful to Restorative Dentistry UK for the invitation to support this themed Head and Neck Cancer edition of the British Dental Journal.
The authors declare no conflicts of interest.
Funding
This project did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Florence Cook: conceptualisation and design of the article, acquisition, analysis and interpretation, drafting, and critically revising and approving the final manuscript for submission. Jose M. Rodriguez: review of the dental aspects of the article and critically revising and approving the final manuscript for submission. Lorna K. McCaul: conceptualisation with Florence Cook, review of the dental aspects of this article and critically revising and approving the final manuscript for submission.
Corresponding author
Ethics declarations
Written consent was obtained from the patients for publication of the clinical photographs taken in Figure 3 and 4.
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0.© The Author(s) 2022
About this article
Cite this article
Cook, F., Rodriguez, J. & McCaul, L. Malnutrition, nutrition support and dietary intervention: the role of the dietitian supporting patients with head and neck cancer. Br Dent J 233, 757–764 (2022). https://doi.org/10.1038/s41415-022-5107-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-022-5107-8