Abstract
Aims COVID-19 has significantly impacted the safety guidelines for personal protective equipment (PPE) within dental services. We quantified and compared the environmental impact of different forms of PPE.
Methods The PPE items were divided into three categories: 1) the body protection category, which included disposable and reusable gowns; 2) the eye protection category, which included a visor with a disposable face shield and a reusable visor; and 3) the respiratory protection category, which included respirator FP2SLw, respirator FFP2 and surgical masks. The OpenLCA software was used for analysing and comparing the environmental impact of all PPE products in the three categories.
Results The life cycle assessment results of this study showed that damage to human health was more significant for the reusable gown than the disposable gown for the body-protection-category PPE. A visor with a disposable face shield had a higher environmental footprint than the reusable visor across all impact categories for the eye protection category. In addition, a visor with a disposable face shield released five times more carbon dioxide equivalent emissions and used four times more dissipated water and three times more fossil fuels than the reusable visor. A disposable gown used four times more dissipated water and three times more fossil fuels than reusable gowns. For respiratory PPE, the FP2SLw respirator had the highest burden in all 16 categories, followed by the FFP2 respirator and then the surgical mask.
Conclusion The environmental impact of PPE is notable and could be reduced through using less damaging domestic products and increased usage of reusables. In addition, the selection of PPE that are reusable and made of recyclable materials can help to minimise the environmental impact and reduce environmental resource depletion.
Key points
-
Understanding that PPE used in dental clinics has an impact on Earth's environmental health.
-
Impact may vary based on PPE materials, country of origin, method of transportation and disposal process.
-
The findings may help inform PPE procurement decisions of dental clinics in the future.
Similar content being viewed by others
Introduction
Planetary health has been influenced by the rapid growth of human civilisation and advancing industrialisation, which has increased the usage of natural resources, such as freshwater, minerals and metals and fossil fuels.1 The world population has rapidly increased from less than 1 billion in 1800 to 7.7 billion in 2019.2 The industrialisation era is responsible for increasing the carbon dioxide in the atmosphere by increasing the combustion of fossil fuels. In 2018, the greenhouse gas emissions level reached 400 ppm, a 42% increase over the 1980s level (280 ppm).3 The build-up of carbon dioxide equivalent emissions (CO2-eq) has been shown to trap heat and has increased the Earth's temperature by approximately 1 °C compared to pre-industrialisation levels.3 If the carbon emissions continue at this current rate, the increase in Earth temperature will be at least 1.5 °C but potentially 4 °C.3 The environmental impact will be on a global scale, for example, climate change and ozone depletion, but also on a local scale, for example, water or soil pollution.4
Standards and guidelines have been developed to provide comparable metric measurements of a product's environmental impact, such as ISO 14040 and ISO 14044.5,6 These International Organisation for Standardisation (ISO) standards provide guidance and a framework for a process called life cycle assessment (LCA). The LCA is 'a comprehensive and widely accepted method that captures the total life cycle emissions of a product or process from "cradle to grave" depending on its system boundaries'.7
The carbon footprint is one of the measurement factors used to estimate the environmental impact of a product or activity on climate change. The CO2-eq represent the total amount of direct and indirect greenhouse gas emissions caused by a product or event.8 The global healthcare sector is a notable contributor to greenhouse gas emissions and is responsible for 5% of total carbon dioxide emissions in developed countries.9 In Ireland, health services account for 9.7% of the national carbon footprint.10 In England, the NHS is responsible for 25% of the public sector carbon dioxide emissions.11 Between 2014-2015, more than 64% of the carbon dioxide emissions in NHS dental services came from patients and staff transportation, 19% was related to product and services procurement and more than 15% was related to electricity and gas usage.12
In 2019, a novel respiratory infectious disease caused by the coronavirus SARS-CoV-2 virus started to spread in December 2019 in China, and in March 2020, the World Health Organisation (WHO) labelled the disease as a pandemic and COVID-19.13 The pandemic led to a revision of the clinical guidelines regarding using personal protective equipment (PPE) in healthcare settings. The European Centre for Disease Prevention and Control published new guidelines in February 2020 with recommendations on PPE usage when treating suspected or confirmed COVID-19 patients.14 However, the guidelines do not recommend sterilising PPE unless used in a sterilised environment.
Due to the pandemic, there has been a significant increase in the use of PPE materials by health workers and others to decrease the possibilities of infections.15 To meet the increase in PPE international demand, the WHO called for an increase of PPE manufacturing by 40% in the early months of the COVID-19 pandemic in 2020.16 PPE typically includes masks, gowns, pants, shoe covers, gloves and goggles, usually consisting of more than 50% plastics, such as polypropylene, polycarbonate and polyvinyl chloride.17
The carbon footprint of PPE distributed to the health and social care system in England during the first six months of the COVID-19 pandemic resulted in 106,478 tonnes of CO2-eq, an estimated 239 disability-adjusted life years (DALYs) damage to human health and an estimated $12.7 million cost in resource depletion.18 Researchers modelled a scenario that excluded: international travel during supply; eliminating glove use; reusing gowns and face shields; and maximal recycling and estimated a reduction in the total carbon footprint by 75%, with an estimated 183 DALYS and $7.4 million saved due to resource depletion.18 The modelled scenario looks promising but it did not consider the increase in PPE prices that might result due to UK manufacturing and whether domestic producers would be able to compete with international competitors.
This study aimed to assess the environmental impact of different PPE before and after COVID-19 that were used at Dublin Dental University Hospital (DDUH). A free LCA software (OpenLCA) was used for the LCA.19
Methods
LCA is a method used to measure and understand the environmental impact of a product system or process. The product system's life cycle includes different steps that include raw material extraction and production and the manufacturing, transportation and disposal processes of the product system.5 OpenLCA is a software created and maintained by GreenDelta in which LCA can be modelled and environmental impacts calculated.19 The Ecoinvent 3.7.1 cut-off unit database was chosen, which offers well-documented data about thousands of products and which can be used to study the environmental impact of the products included in this research.20
The products included in this research were chosen based on PPE guidelines in the DDUH clinics comparing the differences in guidelines before COVID-19, such as using reusable gowns, or after COVID-19, using disposable gowns.14,21 The PPE products were collected from DDUH clinics which were used at the beginning of the academic year 2020/2021 (Table 1).
The PPE were divided into three groups with different functions for compression, as mentioned in Table 2. The LCA assessed all the processes that were involved in manufacturing, packaging, transportation and disposal for single-use products. Requirements for reuse, such as washing and disinfection processes, were added to the LCA where required. OpenLCA was used to conduct the analysis of the seven different reference flows, presented in Table 2. Appendix 1, 2 and 3 show the system boundaries diagram for each PPE category.
The reusable gowns were assumed to be used 60 times before disposal. For the visors, the reusable visor is reused 600 times and requires two disinfectant wipes/session. One wipe is used to disinfect the headband and one for the face shield. While the other visor, the headband, is reusable for 2,000 times and the face shield is single-use. It only requires one disinfecting wipe to disinfect the headband/session. All transportations were assumed to be taking the most direct and shortest route from manufacturers to DDUH and from DDUH to washing or disposable facilities. Google maps were used to estimate all land distances within Ireland and manufacturing countries (Google Maps, 2021), while Searates, an online freight marketplace website, was used to estimate sea distances to Dublin Port and the shortest route was chosen.22,23
Inventory
For the body protection PPE, the disposable gown weighed 71.02 g and was made of 50% polyethylene and 50% non-woven polypropylene. The packaging materials weight for one gown was calculated based on the number of items in one package. Therefore, 3.56 g of corrugated board and 0.79 g were used for one disposable gown in the packaging process.
For the reusable gown, the raw materials were calculated for one item of 392.9 g and made of 65% polyethylene and 35% non-woven polyester. The washing process included transportation to and from the washing facility (20 km) and new packaging materials.
In the eye protection PPE category, there were two visors. The first one had a disposable face shield and reusable headband, which means the face shield would be replaced with a new one after each session and the headband would be disinfected for the next session. The first visor was made of 21.13 g of polycarbonate for the face shield, 12.87 g of nylon 6 for the elastic band and 13.54 g of polyvinylidene chloride for the headband. To disinfect the headband between sessions, one wipe was used, made of 2.06 g of textile; non-woven polypropylene. The reusable visor was made of 164.1 g of polycarbonate for the reusable face shield and 25.51 g of polypropylene for the headband was assumed to be used 600 times. One wipe was used to disinfect the reusable face shield and another wipe for the headband.
The respiratory protection PPE category had two respirators and one surgical mask. They were all single-use which means one item was used to treat one patient during one dental visit. Firstly, the FP2SLw respiratory mask was made of 5.28 g of non-woven polypropylene and 1.69 g of non-woven polyester. In addition, 1.55 g of nylon 6 was used for the ear loops, 0.1 g of polyurethane for flexible foam around the headband and 0.92 g of aluminium for the adjustable nose bridge. The package raw material inputs for one product were 3.515 g of corrugated board and 0.268 g of packaging film; low-density polyethylene.
Secondly, the respiratory FFP2 mask was made of 4.11 g of non-woven polypropylene for the respiratory, 0.85 g of nylon 6 for the ear loops and 00.4 g of steel and 0.17 g of polyvinylchloride for the adjustable nose bridge. The packaging raw materials' weights were divided on 25 for the corrugated board as one box had 25 masks and each respiratory had its packaging film (low-density polyethylene). For one product, 2 g of corrugated board and 1.7 g of polyethylene were used for packaging materials.
Finally, the last PPE in this group was a surgical mask made in Germany. It was made of 1.68 g of non-woven polypropylene, 0.4 g of nylon 6 for ear loops and 0.28 g of steel wire, covered by 0.16 g of polyvinylidene chloride for the adjustable nose bridge. For one mask, 0.0606 g of corrugated board and 0.8588 g for plastic packaging film were used because in each package there were 50 masks.
Impact assessment
As recommended by the European Commission within the Product Environmental Footprint (PEF) guidance, the environmental impacts calculated include the harm caused by any process in the product life cycle to population health, plants, animals, soil, or water, or affecting the future availability of natural resources.24 The impacts could be on a global scale, such as climate change and ozone depletion, or on a local scale, such as water or soil pollution.4 Table 3 shows the impact categories included in this study with their descriptions according to the PEF guidance.24 The impact indicator data were normalised according to the PEF guidelines in-person equivalents.24
A harmonised LCA method called ReCiPe 2016 was used to measure the endpoint damage to human health, ecosystem and resource availability.25 ReCiPe 2016 provides a harmonised implementation of cause-effect pathways for calculating various environmental impacts, such as the impact of water use on human health, freshwater ecosystems and terrestrial ecosystems and the impact of climate change on freshwater ecosystems.25 The unit used for human health damage is DALYs, representing the years lost or that an individual is disabled because of an illness or accident.25
Results
Body protection PPE
The burden of the disposable gown was higher than the reusable gown across eight impact categories, including: photochemical ozone creation (102% higher); climate change total (101% higher); respiratory effects, inorganics (58% higher); freshwater and terrestrial acidification (57% higher); freshwater eutrophication (56% higher); ionising radiation (40% higher); and terrestrial eutrophication (25% higher). The results were normalised per person equivalents as recorded in Figure 1. They showed that the highest environmental burdens were found in the minerals and metals, fossil, climate change, freshwater eutrophication and dissipated water impact categories, with a normalised score superior to 1.12E-05 person equivalents. The reusable gown had higher impacts in two of the five highest categories, including minerals and metals and dissipated water (1.30E-04, 5.62E-05 person equivalents).
ReCiPe 2016 results showed that 99% of the damage to human health came from global warming and water consumption. Water consumption was the main contributor to human health damage for the reusable gowns, while global warming was the main contributor for the disposable gown, as shown in Figure 2.
Figure 1 shows that the reusable gown had higher environmental effects in five categories: minerals and metals, dissipated water, marine eutrophication, ozone layer depletion and land usage. For the disposable gown, the disposal process accounted for the largest share of the minerals and metals effects at 61% for 'hazardous waste', followed by 20% for 'market for fleece, polyethylene (Cutoff, U - GLO)' and 14% for 'market for textile, non-woven polypropylene (Cutoff, U - GLO)'. The highest contributors in greenhouse gases emissions for disposable gown were 41% for hazardous waste incineration, followed by the market for polyethylene and polypropylene (27.26% and 24.51%). For the fossil effect, the manufacturing process was the main contributor for a disposable gown at 85% and especially for the market for polyethylene and polypropylene (43% and 40%).
Dissipated water was five times higher in reusable gowns than disposable (1.3E-01 m3 water-eq; 6.4E-01 m3 water-eq, respectively). As part of the manufacturing process in the reusable gown, 'market for textile, woven cotton (Cutoff, U - GLO)' was alone responsible for 84.15% of dissipated water while 'market for textile, non-woven polyester (Cutoff, U - GLO)' was only responsible for 1.7%. Moreover, the market for cotton was responsible for 37.3% of the carcinogenic effects, which was higher than the market for polyester (10.97%). This difference could be explained in part by the material ratio of the reusable gown (65% cotton). While polyester accounted for 14.52% of fossil effects, cotton was at 9.4%. However, the main contributor to fossil effects for reusable gowns was the washing process, at 73%. Notably, the fossil fuel impact of reusing (washing) a reusable gown was still far lower than that of manufacturing a new disposable gown.
Eye protection PPE
The burdens of the visor with a disposable face shield were higher than the reusable visor across all impact categories. One functional unit of the reusable visor released 19.44% of greenhouse gases of what the other visor releases. The reusable visor needed 24.29% of dissipated water, 31.12% of fossil, 13.92% land use and 4.82% of metals resources used by the visor with the disposable face shield.
The normalised scores per person equivalents, as recorded in Figure 3, showed that the highest categories were minerals and metals, fossils, climate change and respiratory effects. The visor with a disposable face shield had the highest burdens in all environmental impact categories. In ReCiPe 2016, the results showed that the impact of the visor with a disposable face shield on human health was four times higher than the reusable visor in water consumption and five times more in climate change (Fig. 4).
For the fossil effect, the manufacturing process for the visor with disposable face shield was the main contributor with 66%, mainly for 'market for polycarbonate (Cutoff, U - GLO)'. Even though the environmental impact of transportation was as low as 0.23% for fossil use, transportation outside of Ireland was the main contributor (96%). However, the transportation of waste 'transport, freight, lorry 3.5-7.5 metric ton, EURO6 (Cutoff, U - RER)' was responsible for 19% of the fossil fuel usage.
Respiratory protection PPE
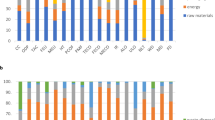
When comparing the normalised scores of the three respiratory protection PPE, it showed that the FP2SLw respirator had the highest-burden in all 13 categories, followed by the FFP2 respirator and then the surgical mask, as shown in Figure 5.
In ReCiPe 2016, the damage from global warming was the highest for the FP2SLw respirator at 7.92E-08 DALY, followed by the FFP2 respirator and then the surgical mask (5.43E-08, 1.80E-08 DALY, respectively). The impact of water consumption was also the highest for the FP2SLw respirator at 1.65E-08 DALY, followed by the FFP2 respirator and then the surgical mask (1.65E-08, 1.19E-08, 3.84E-09 DALY, respectively) (Fig. 6). As total damage to human health, the surgical mask could cause only 23% and 33% of the effects of the FP2SLw and the FFP2 respirator, respectively.
The highest respiratory protection PPE in the fossil impact category was the FP2SLw respirator at 1.17 MJ, followed by the FFP2 respirator at 8.58E-01 MJ and the surgical mask at 2.57E-01 MJ. While the carbon footprints of the highest PPE were estimated as follow: FP2SLw respirator 8.53E-02 CO2-eq; FFP2 respirator 5.86E-02 CO2-eq; and surgical mask 1.94E-02 CO2-eq.
The main contributor to the FP2SLw respirator manufacturing process in the minerals and metals effects category was the 'market for textile, non-woven polyester (Cutoff, U - GLO)' at around 64%, followed by 17% for market for polypropylene. The main contributors to the FFP2 respirator in the minerals and metals effects category were 39% for the market for polypropylene, 13% for packaging film and 11% for transportation as 'market for transport, freight, lorry 3.5-7.5 metric ton (EURO6 | Cutoff, U - RER)'. While for the surgical mask, the main contributors were 38% for market for polyethylene, 20% for 'hazardous waste, for incineration' and 15% for the ear loop materials' 'market for nylon 6 (Cutoff, U - RER)'.
The disposal process was the main contributor to human health-carcinogenic effects, non-carcinogenic effects and climate change in all three respiratory protection PPE. When comparing the packaging processes of respiratory PPE, the FFP2 respirator had the highest impact in all 16 categories, followed by the FP2SLw respirator and then the surgical mask.
Discussion
Body protection
The study findings were different in some categories compared to a previous study undertaken by Vozzola et al. 2020, which found that using reusable gowns had a lesser environmental impact than disposable gowns in all 16 impact categories.26 There are several plausible explanations for this. First, the disposable gown and the reusable gown used in DDUH was 12% and 63% higher, respectively, than the representative weights used in Vozzola's study. These weight differences play an important role in increasing the environmental impact of the reusable gown in some categories and especially in water consumption, since most of the impact comes from the manufacturing process. Second, DDUH's reusable gowns are made of 65% cotton fabrics and 35% polyester, while Vozzola's reusable gown are made of polyester.26
Cotton as a raw material has a higher environmental impact than acrylic or polyester, which could explain why the DDUH's reusable gown had a higher impact on some environmental categories, such as water consumption, marine eutrophication, dissipated water and land use.27 There is room to reduce the environmental impact of DDUH's gowns by simply replacing them with lighter fabrics which use lesser resources in manufacturing and disposal; however, this would need to be compatible with infection prevention and control guidance.
Eye protection
Face or eye protection equipment was second to body protection PPE in its planetary health impact, which was consistent with previous studies, such as Rizan et al. 2020. However, Rizan's study only included disposable face shields.18 Our findings showed that the reusable visor had a lesser effect on planetary health than the visor with a disposable face shield. The environmental impact of the visor with a disposable face shield was four times more than the reusable visor. The differences in the environmental impacts of the two visors could be influenced by the number of uses, total product mass weight and country of origin. For example, the weight of the visor with a disposable face shield was only 25% the weight of the reusable visor as products differed from 47.53-189.61 g. The accumulated weight of the visor with a disposable face shield was 66 times more than the reusable visor because of the difference in the estimated number of uses, especially for the disposable face shield. The effect of weight differences could be seen in all processes, especially in manufacturing and disposable.
Respiratory protection
Respiratory protection PPE had the least effect on planetary health compared with body and eye protection categories and our results were consistent with Rizan's findings.18 The surgical mask had the most negligible environmental impact among all three items in the respiratory protection category, while the FP2SLw respirator had the highest environmental impact in the respiratory protection category. The difference in effects among the three products could be because of the differences in their weights. The FP2SLw respirator was 72% higher in weight than FFP2 respirator, even though they both provide the same level of protection (minimum filter efficiency of 94%). This difference in weight was not necessary to increase the protection, so using the lighter weight respirator (FFP2) could reduce the environmental impact without compromising respiratory protection.
The package methods had also influenced the environmental impacts of the three products in the respiratory protection category. For example, individual packaging had increased the contribution of the packaging process in climate change to 0.01024 kg CO2-eq comparing with multiple items in one package for respirator FP2SLw and for the surgical mask (0.0048 kg CO2-eq and 0.00152 kg CO2-eq, respectively). The other reason was the country of origin, where Germany, Ireland and China produced surgical masks, FFP2 respirators and FP2SLw respirators, respectively. The difference in country of origin made differences in the required energy for transportation and source of electricity. For example, Germany used renewable energy, such as wind, solar and hydropower to produce 44.9% of its electricity in 2020, while China used renewable energy to produce 9.54% of its electricity in 2020 and Ireland had 33.3% of its electricity in 2018 generated by renewable energy.28,29,30
Incineration is not the best way for medical waste management; however, during the COVID-19 pandemic, many countries used incineration because of the increase in medical waste, especially PPE, plastics waste and preventing spreading COVID-19 through handling the recycling materials.31,32
Recommendations
The environmental impact should be one of the criteria to select PPE for dental services. The manufacturer's location also needs to be considered in the selection, as this might reduce the associated environmental impact. Many European countries, such as Germany and the UK, had introduced a scheme to support domestic PPE production. This would be an excellent chance to prioritise domestic or regional products in procurement.33
The efficiency in producing PPE is required by using the least number of raw materials and considering using recycled materials without compromising the PPE's protection features. It would also be beneficial for planetary health to reuse PPE when feasible. For example, the healthcare sector could require that PPE be made of recyclable material, such as recycled polyester, (rPET) to facilitate medical waste recycling, especially for large products such as reusable gowns where the gowns could be recycled to make new gowns.
Limitations of the study
This study may underestimate the planetary health impact of the dental services because our data were based on DDUH clinics. We also assumed that PPE was used by one clinician and did not include dental assistants or other staff as receptionists. In addition, the location of DDUH, which is very close to the Dublin port and incineration plant, may also underestimate the transportation effects since it does not reflect the average travel distances of PPE products to dental clinics across other countries.
The DDUH's waste management company does not incinerate all decontamination waste. Instead, the products are shredded and then used for other purposes, including construction materials, but they are incinerated for energy use if there is no market. For this paper to be applicable to most international settings, incineration was modelled. This modelling may worsen the impact of PPEs in this study; however, to avoid COVID-19 transmission, incineration was the most straightforward and safest choice for waste management worldwide.34
Conclusion
The environmental impact of PPE requires strong consideration to mitigate its effects on planetary health. The COVID-19 pandemic produced national procurement guidelines for PPE. Future versions of these could be used to improve PPE selection based on their environmental impact, materials and country of origin. Manufacturers need to optimise PPE production by using an efficient number of materials with the least environmental impact and by considering recycled materials in manufacturing PPE. Prioritising reusable PPE where possible and considering reprocessing some PPE without compromising safety would help in reducing dental services' effects on planetary health. Further studies may be needed to evaluate other PPE products within the market.

Appendix 1 System boundaries of reusable and disposable gowns

Appendix 2 System boundaries of visor with disposable face shield and reusable visor

Appendix 3 System boundaries of surgical mask, respiratory FP2SLw and surgical mask
References
Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services. Global Assessment Report on Biodiversity and Ecosystem Services: Summary for Policymakers. 2019. Available at https://ipbes.net/global-assessment (accessed July 2022).
Our World in Data. World Population Growth. 2013. Available at https://ourworldindata.org/world-population-growth#citation (accessed July 2022).
Intergovernmental Panel on Climate Change. Special Report: Global Warming of 1.5 C. Available at https://www.ipcc.ch/sr15/ (accessed July 2022).
Bare J C. Risk Assessment and Life-Cycle Impact Assessment (LCIA) for Human Health Cancerous and Noncancerous Emissions: Integrated and Complementary with Consistency within The USEPA. Human Eco Risk Assess 2006; 12: 493-509.
International Organisation for Standardisation. Environmental management - Life cycle assessment - Principles and Framework. 2006. Available at https://www.iso.org/standard/37456.html (accessed July 2022).
International Organisation for Standardisation. Environmental management - Life cycle assessment - Requirements and guidelines. 2006. Available at https://www.iso.org/standard/38498.html (accessed July 2022).
Duane B, Stancliffe R, Miller F, Sherman J, Pasdeki-Clewer E. Sustainability in Dentistry: A Multifaceted Approach Needed. J Dent Res 2020; 99: 998-1003.
Wiedmann T, Minx J. A Definition of 'Carbon Footprint'. In Pertsova C (ed) Ecological Economics Research Trends. pp 1-11. NY: Nova Science Publishers, 2008.
Pichler P-P, Jaccard I S, Weisz U, Weisz H. International comparison of health care carbon footprints. Environ Res Letters 2019; DOI: 10.1088/1748-9326/ab19e1.
Arup. Healthcare's climate footprint. 2019. Available at https://www.arup.com/perspectives/publications/research/section/healthcares-climate-footprint (accessed July 2022).
NHS England. Greener NHS. Delivering a 'Net Zero' National Health Service. 2020. Available at https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2020/10/delivering-a-net-zero-national-health-service.pdf (accessed July 2022).
Duane B, Lee M B, White S, Stancliffe R, Steinbach I. An estimated carbon footprint of NHS primary dental care within England. How can dentistry be more environmentally sustainable? Br Dent J 2017; 223: 589-593.
World Health Organisation. Coronavirus Disease 2019 (COVID-19). Available at https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed July 2022).
European Centre for Disease Prevention and Control. Guidance for wearing and removing personal protective equipment in healthcare settings for the care of patients with suspected or confirmed COVID-19. 2020. Available at https://www.ecdc.europa.eu/en/publications-data/guidance-wearing-and-removing-personal-protective-equipment-healthcare-settings (accessed July 2022).
Velavan T P, Meyer C G. The COVID-19 epidemic. Trop Med Int Health 2020; 25: 278-280.
World Health Organisation. Shortage of personal protective equipment endangering health workers worldwide. 2020. Available at https://www.who.int/news/item/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide (accessed July 2022).
Asian Development Bank. Global Shortage of Personal Protective Equipment Amid COVID-19: Supply Chains, Bottlenecks, and Policy Implications. 2020. Available at https://www.adb.org/publications/shortage-ppe-covid-19-supply-chains-bottlenecks-policy (accessed July 2022).
Rizan C, Reed M, Bhutta M F. Environmental impact of personal protective equipment distributed for use by health and social care services in England in the first six months of the COVID-19 pandemic. J R Soc Med 2021; 114: 250-263.
OpenLCA. GreenDelta. Available at https://www.openlca.org/greendelta/ (accessed May 2022).
Ecoinvent Association. Documentation of changes implemented in ecoinvent database v3. 7 & v3. 7.1. 2020. Available at https://ecoinvent.org/wp-content/uploads/2021/01/change-report_v3-7-1_20201217.pdf (accessed July 2022).
Dental Council of Ireland. Code of Practice Relating to Infection Control in Dentistry. Available at http://www.dentalcouncil.ie/files/Infection_Control.pdf (accessed July 2022).
Google. Google Maps. Available at https://www.google.com/maps (accessed January 2021).
SeaRates. Find the best freight quote. Available at https://www.searates.com/ (accessed January 2021).
European Commission. Product Environmental Footprint Category Rules Guidance. 2018. Available at https://ec.europa.eu/environment/eussd/smgp/pdf/PEFCR_guidance_v6.3.pdf (accessed July 2022).
Huijbregts M A J, Steinmann Z J N, Elshout P M F et al. ReCiPe2016: a harmonised life cycle impact assessment method at midpoint and endpoint level. Int J Life Cycle Assess 2016; 22: 138-147.
Vozzola E, Overcash M, Griffing E. An Environmental Analysis of Reusable and Disposable Surgical Gowns. AORN J 2020; 111: 315-325.
Van der Velden N M, Patel M K, Vogtländer J G. LCA benchmarking study on textiles made of cotton, polyester, nylon, acryl, or elastane. Int J Life Cycle Assess 2014; 19: 331-456.
German Federal Statistical Office. Gross electricity production in Germany. Available at https://www.destatis.de/EN/Themes/Economic-Sectors-Enterprises/Energy/Production/Tables/gross-electricity-production.html (accessed July 2022).
Wong S. China: power generation by source. 2020.
Sustainable Energy Authority of Ireland. Energy in Ireland 2018 Report. 2018. Available at https://www.seai.ie/publications/Energy-in-Ireland-2018.pdf (accessed July 2022).
Haque M S, Uddin S, Sayem S M, Mohib K M. Coronavirus disease 2019 (COVID-19) induced waste scenario: A short overview. J Environ Chem Eng 2021; DOI: 10.1016/j.jece.2020.104660.
Ilyas S, Srivastava R R, Kim H. Disinfection technology and strategies for COVID-19 hospital and bio-medical waste management. Sci Total Environ 2020; DOI: 10.1016/j.scitotenv.2020.141652.
National Audit Office. The supply of personal protective equipment (PPE) during the COVID-19 pandemic. 2020. Available at https://www.nao.org.uk/report/supplying-the-nhs-and-adult-social-care-sector-with-personal-protective-equipment-ppe/ (accessed July 2022).
Wang J, Shen J, Ye D et al. Disinfection technology of hospital wastes and wastewater: Suggestions for disinfection strategy during coronavirus Disease 2019 (COVID-19) pandemic in China. Environ Pollut 2020; DOI: 10.1016/j.envpol.2020.114665.
Author information
Authors and Affiliations
Contributions
Waleed Almutairi: methodology; software; and writing - original draft. Sophie Saget: software and writing - review and editing. Jarlath McDonnell: resources, review and editing. Agi Tarnowski: conceptualisation;,methodology; writing - review and editing. Mark Johnstone: conceptualisation, methodology, writing - review and editing. Brett Duane: supervision, writing - review and editing.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
Ethical approval was not required for this this study as it did not involve any patients or healthcare staff.
Rights and permissions
About this article
Cite this article
Almutairi, W., Saget, S., Mc Donnell, J. et al. The planetary health effects of COVID-19 in dental care: a life cycle assessment approach. Br Dent J 233, 309–316 (2022). https://doi.org/10.1038/s41415-022-4906-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-022-4906-2
This article is cited by
-
The environmental impact of community caries prevention - part 1: fluoride varnish application
British Dental Journal (2022)
-
A review of HTM 01-05 through an environmentally sustainable lens
British Dental Journal (2022)