Abstract
Patients deserve to be treated in a safe and clean environment with consistent standards of care every time they receive treatment. It is essential that the risk of person-to-person transmission of infections be minimised, yet it is also essential that planetary harm (and therefore public harm) is minimised with respect to resource consumption, air pollution, environmental degradation etc.
In 2013, the Department of Health introduced the Health Technical Memorandum (HTM) 01-05 providing dental practices with advice on patient safety when decontaminating reusable instruments in primary care. This paper provides a commentary on HTM 01-05 and similar decontamination guidance. We believe all decontamination documents needs to reflect the so-called 'triple bottom line' - the finance, social cost and impact on the planet.
The authors provide an environmental commentary on a number of items mentioned in decontamination documents, including autoclaves (including the use of helix tests), disposable paper towels, undertaking hand hygiene, using a log book, plastic bag use, the use of personal protective equipment, remote decontamination units, single use instruments, single use wipes, disinfection chemicals (for example, sodium hypochlorite) thermal disinfection and wrapping of instruments.
It is hoped, in the spirit of the ever-increasing numbers of papers published to highlight how healthcare (and dentistry) could become more sustainable, that these critiques will be taken in the spirit of providing a beginning of further discussion from an environmental perspective.
Key points
-
Decontamination documents, such as HTM 01-05, need a revision to include resource use.
-
Single-use instruments should only be used if they offer significant risk (patient safety/environmental resource use) benefit.
-
Clinicians should follow decontamination guidance but question where appropriate unnecessary resource use.
Similar content being viewed by others
Introduction
Patients deserve to be treated in a safe and clean environment with consistent standards of care every time they receive treatment. As part of this, it is essential that the risk of person-to-person transmission of infections be minimised as much as possible. In 2013, the Department of Health introduced the Health Technical Memorandum (HTM) 01-05.1 This gave dental practices advice on patient safety when decontaminating reusable instruments in primary care. The document highlights the duty of care for dentists to ensure they provide appropriate decontamination care.
Although the document provided consistent clear advice to the dental team, there has been significant critique of the document. One of the main criticisms is concerning the cost of implementation. Richardson demonstrated that waste management costs increased by 58% when HTM 01-05 was introduced.2 The problem is further compounded when considering what is essential practice and what is excessive. Excessive practice will lead to even greater waste, which we have seen during the COVID 19 pandemic.3
Measures to improve patient safety should ensure that that planetary harm (and therefore public harm) is minimised with respect to resource consumption, air pollution, environmental degradation etc. There has been a rapid increase in papers highlighting both the environmental harm associated with health systems overall,4,5 as well as the need for health care systems to be net zero (so their net carbon emissions are effectively zero).6There is an urgent need for this because we are not just facing a climate change crisis,7 but also crisis across biodiversity8 and water scarcity.9We know from a number of studies that a number of healthcare processes and products actively cause harm; the use of some products or procedures causes a loss of disability adjusted life years (DALY). Byrne's paper for example showed that using plastic disposable examination kit caused ten seconds of DALY loss, compared with three seconds for a reusable kit.10Within healthcare, Rizan has reported on the huge environmental cost of personal protective equipment (PPE) and this has been echoed in dentistry by Almutairi.11,12
There needs to be consideration therefore not only to the efficacy and safety of our decontamination processes but also to their sustainability.5 This paper provides a commentary on HTM 01-05. We believe all standards need to be updated to consider the so-called 'triple bottom line' - the finance, the social cost and the impact on the planet. While this paper will focus on HTM 01-05, we believe it is relevant to other decontamination documents including those in Canada,13 the Republic of Ireland,14 New Zealand,15Scotland,16 United Kingdom,1 United States of America17and Australia.18
Methodology
To understand how HTM 01-05 could be viewed from a sustainability perspective we followed the following steps:
-
1.
Critique of HTM 01-05 to identify potential areas of significant environmental impact and how these could be potentially mitigated
-
2.
Life cycle analysis of one decontamination method (laundry) as an exemplar to illustrate where the impacts on the environment come from and to allow us to hypothesise alternatives. We compared chemical disinfection (25 degrees), chemo-thermal disinfection (50 degrees) and thermal disinfection (71 degrees). The reference was washing 1 kilogram of laundry. The ecoinvent database v3.6.1 was used,19 with openLCA software 1.10.3 to calculate the environmental impact factors.20 (The results for this are shown in the section 'Thermal and/or disinfection cleaning; results from our LCA'.) The input output table used to construct this analysis can be found in the online Supplementary Information.
Results
There are several aspects of HTM 01-05 where an environmental comment would be useful. Themes identified are listed in Table 1.
Autoclave equipment/dishwasher equipment and manual washing
The use of the washer-disinfector and the vacuum autoclave are central processes in the disinfection cycle described in HTM 01-05. There is no discussion in HTM 01-05 of the environmental impact of either of these energy intensive processes. The bulk of the environmental impact from washer disinfectors arises from the energy consumed both in their use and to heat the water to the correct temperature. The volume of water used in a washer disinfector cycle also depends on the chamber size. Less water is typically used in washer disinfectors than would be used in handwashing but repeated use of washer disinfectors consumes considerable volumes of water. Many washer disinfectors consume additional energy to utilise water manufactured by reverse osmosis. The chemicals used in the washer disinfector can affect human health and can cause freshwater eutrophication.21
Strategies to reduce the environmental impact of washer disinfectors include using renewable energy sources to power washer disinfectors, using full chambers to decrease the number of cycles and running cycles close together to recycle heat from previous cycles. The volume of detergent used could be reduced by utilising selective settings based on the perceived soiling of the instruments.
The environmental impacts of vacuum autoclaves similarly originates from the water consumed and the energy required to produce reverse osmosis water and power cycles. Strategies to reduce the environmental impact of vacuum autoclaves include using renewable energy sources, using autoclaves with high energy efficiency and using full chambers to decrease the number of cycles. Autoclaves on standby mode consume significant energy and efforts should be made to confine their use to fixed times ie reduce standby mode. Where possible, thermal jackets to prevent heat loss should be fitted. Efficient procedure tray systems should be used so that only instruments required are autoclaved to reduce unnecessary cycles.
The environmental impact of the autoclave could potentially be reduced if policymakers determined that instruments were reprocessed according to use, rather than by class. In the hospitality industry, cutlery is re-used following rudimentary cleaning and is not described as a risk to public health. In healthcare, Spalding described categories of instruments that should undergo cleaning, disinfection or sterilisation.22 In medical practice, endoscopes that traverse the oral cavity are reprocessed by disinfection alone. By contrast, all dental instruments, regardless of the level of contamination, undergo cleaning, disinfection and sterilisation. Rutala estimated the risk of transmission from instruments decontaminated by disinfection but not sterilisation as 8 in 100 trillion for human immunodeficiency virus and 1 in 10 billion for hepatitis B.23 Reconsidering how we process items used in the oral cavity may be supported by reports of significant failures in the decontamination process in general practice in the UK that have not been accompanied by reports of transmission of infection between patients.24,25 Documented cases of transmission in the USA in oral surgery practice could not be linked to the decontamination process.26,27Public confidence in the decontamination process and possible demands to adhere to the current protocols may be offset by the low risk of transmission of disease by contaminated dental instruments and the need to reduce the environmental impact of autoclaves.
Both washer disinfectors and vacuum autoclaves should be properly commissioned, validated and serviced to ensure optimum efficiency in the decontamination cycle. Only devices with CE marks (in Europe) that that may be reliably initially commissioned should be purchased.
We recommend that devices such as autoclaves come with energy labels/kwhr use, with information on how to reduce resource use (energy, water) clearly shown in online instructions.
Disposable paper towels
HTM 01-05 recommends that hands should be dried to prevent decontamination with paper towels. From an environmental perspective, based on a life cycle assessment (LCA) from the Netherlands,28this practice is considerably worse from both an environmental perspective and a human health perspective than drying hands with a hot air dryer. The Dutch LCA, however, used an average electricity mix in the Netherlands (electricity was only 8.8% renewable in 2019).29 It would therefore be expected that drying your hands with a hot air dryer will become increasingly better from a human health perspective as the Netherlands increases its share of renewables.
The relationship between the use of hot air dryers and microbiological contamination is complex. A very recent review showed that in some studies air dryers provide better bacterial decontamination of hands than paper towels, but in other studies there was no data to support any human health claims (from a decontamination perspective) to support either model of hand drying. As an example, in a study by Pitts, the use of paper towels (PTs), air dryer and jet dryer, respectively decreased, increased and made no significant change to the number of microbial flora on hands. However, the air and jet dryer dispersed more microorganisms than PT.30 Similarly, in another recent study, there was fewer bacteria after jet drying compared with PTs.31 The authors concluded that there is inconclusive and conflicting results which make recommending a specific policy difficult.32More research is needed!
If a new edition of HTM 01-05 continues to recommend paper towels, it is our suggestion that they advocate for non-bleached paper to reduce the impact of chlorinated products being manufactured and disposed of. There is however some evidence to suggest that recycled towels contain more bacterial load than virgin products.33
Hand hygiene
Hand hygiene in the context of HTM 01-05 involves not just handwashing but also any other measures to disinfect hands, such as antibacterial-based hand-rubs/gels. Use of a mild soap is the standard; antimicrobial handrubs can be used in the absence of visible contamination. Bar soap is not permitted by the document. HTM 01-05 also mandates the use of wall-mounted liquid hand wash dispensers as refillable hand wash containers are thought to carry as risk of contamination.
Clearly hand hygiene is critical but there is some potential that the HTM 01-05 recommendations could be made more sustainable.
A recent review of hand washing versus hand sanitiser found that hand sanitiser was more environmentally sustainable than handwashing with soap. This was most likely because use of hand sanitiser reduces water use or hand drying was not required. A starting point for HTM 01-05 therefore could be to recommend hand sanitiser as the norm unless there is visible contamination.34
With regards to use of soap, HTM 01-05 specifically forbids the use of it in bar form (bar soap); however, there is no justification given for this. Use of bar soap cuts down on packaging waste so it is a more environmentally sustainable method of delivery than liquid soap. It is unclear why the use of bar soap is contraindicated - there is no supporting reference. Presumably there is a risk of contamination of the soap between uses; however, this recommendation conflicts with a 1988 paper by Heinse who showed no risk of bacterial transfer using bar soap.35
HTM 01-05 also mandates that refillable soap dispensers are not used, again because of the risk of reinfection. Research demonstrates that washing with contaminated soap from bulk-soap-refillable dispensers can increase the number of opportunistic pathogens on the hands and may play a role in the transmission of bacteria in public settings.36 Soap dispensers further add to the environmental impact of using liquid soaps and are another reason to consider recommending sanitisers over soap.
Helix test
We know from the running of an autoclave generates around 20 seconds of DALYs loss.13 We would hope therefore that there was good evidence as to how often we should run a Helix or Bowie-Dick tests.
A daily steam penetration test is recommended for vacuum autoclaves by both HTM 01-05 and ISO (International Organisation for Standardisation) 17665-1:2006, alongside daily recording of maximum temperature reached and pressure achieved in a logbook. In terms of specific evidence for daily steam penetration tests, there is no reference included in HTM 01-05 and nor was any supporting literature identified. The tests are recommended daily to identify a malfunctioning autoclave as early as possible and therefore prevent potentially contaminated instruments being used on patients. Like many of our sections, more research is needed to support the necessity of these types of tests.
Log book
HTM 01-05 advises the use of log books to record the various aspects of decontamination.
The jury is still out as to what is better, paper or electronic copies. We found one review in 201437 and one paper written in 2020.38 The first paper showed that electronic communication was associated with a smaller impact on the environment than printed communication when the reading time is short, which is probably the case for the reading of decontamination literature. This environmental saving will also increase as energy mix of countries increasingly becomes more renewable.
In contrast, in the second paper by Suksuwan showed that a paper notebook performed better from an environmental perspective compared with the tablets in the most environmental categories.38
We recommend further work in this area.
Plastic bags versus plastic reusable containers: sending products to a laboratory
HTM 01-05 suggests that if the device is to be returned to a supplier (etc) a label should be used (etc) and affixed to the package. Although HTM 01-05 doesn't mention the type of product/packaging that should be used in transporting a product back and forth from the laboratory, the instrument to be returned should be decontaminated firstly and placed in paper wrapping or plastic to prevent damage in transit and then in a hard plastic sealed box so it cannot puncture through. It is then labelled, which may also include a sharps warning.
To summarise, we believe that most anecdotally would use a combination of plastic bags in plastic containers.
From an environmental perspective, there is a significant impact of using plastic bags compared with/or alongside usable containers. According to 'time for change' a plastic bag generates about 33 grams of CO2,39whereas the carbon footprint of a half-litre container of has a total carbon footprint equal to 2.5 times this: 82.8 grams of carbon dioxide.40 Any comparison of carbon footprints should be taken with some caution; however, in keeping with the evidence presented in the rest of the paper, clinicians should be using washable reusable containers. The literature confirms that disinfection and microbiological monitoring and validation of reusable waste containers is not indicated and that washing with hot water and detergent, using visual criteria for cleanliness and due diligence with regard to contractor selection, enable reusable containers to be safely used.41 As well as reducing landfill waste, costs and environmental emissions, the use of a reusable container also reduces sharp injury risk to healthcare workers.42,43
The other environmental issue here is the production, use and disposal of labels. We advocate that reusable containers should be used with minimal packaging to transport products back and forth from the label. Healthcare providers could consider writing using wipeable pen on the container to save this environmental cost.
Personal protective equipment: disposable versus reusable visors
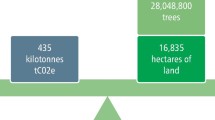
HTM 01-05 says that 'disposable visors are available and may be used' with no reference to their planetary effect. In a study within dentistry comparing plastic reusable visors versus disposable visors, there was clear environmental advantages using reusable visors6 (see Figure 1). This study of the high environmental footprint associated with visors agrees with a recent paper by Rizan, where reusing visors provided definite environmental advantages.11
Personal protective equipment: gloves
HTM 01-05 states that appropriate PPE should be worn during decontamination procedures and specifically references both disposable clinical gloves and household gloves.1 Gloves are needed to protect hands from becoming contaminated with organic matter and microorganisms; to protect hands from chemicals that adversely affect skin, such as caustic chemical agents used in disinfection; and to minimise the risks of cross-infection by preventing the transfer of organisms from staff to patients and vice-versa.1
However, there is growing evidence detailing the environmental impact of clinical gloves, specifically nitrile gloves, typically manufactured from plastics or petroleum-based synthetic rubbers.11 Rizan et al. highlighted the significant contribution that clinical gloves made to the environmental impact of healthcare during the first six months of the COVID-19 pandemic: nearly 48,000 tonnes of carbon dioxide equivalents (CO2e). The estimated damage to human health of using gloves as part of PPE was 108 DALYs, equating to a loss of 0.21 species per year if describing the impact on ecosystems.
Risk assessment of glove use is necessary to mitigate the substantial environmental impacts. The World Health Organisation (WHO) limits the use of medical gloves to examination (non-sterile or sterile) or surgical procedures requiring specific characteristics.44 WHO explicitly states that inappropriate glove use represents a waste of resources if not contributing to a reduction of cross-transmission and may result in missed opportunities for hand hygiene.45
Crucially, HTM 01-05 does offer household gloves as an option for decontamination, recommending weekly pairs of domestic household gloves if washed with detergent and hot water and left to dry after each use. These gloves, therefore, should not be sterile and could meaningfully reduce the impact of decontamination as non-sterile gloves have the least environmental impact across gloves used in dentistry.45
Sterile gloves can be made from natural rubber (latex) or synthetic rubber and research by Jamal et al. describes how the climate change impact of sterile latex gloves was 11.6 times higher than non-sterile gloves.45 Household gloves are commonly made from these two same natural and synthetic rubbers but recently have been manufactured in durable silicone due to the prevalence of latex sensitivities. Silicone has a low chemical reactivity, has a broad range of thermal stability and is resistant to growth of microorganisms.46
It could be suggested that swapping disposable nitrile gloves in favour of durable reusable silicone gloves for decontamination purposes could reduce the environmental impact of dental glove use. There is also considerable variation in permeability of nitrile gloves observed when testing disposable nitrile gloves potentially due to differences in movement of the operator's hands.47These factors should be taken into consideration when favouring the convenience and disposability of say, nitrous gloves over the reusability and protection of reusable silicone gloves.48 This same reasoning could be applied to the practice of some routine dentistry where the necessity of gloves may be called into question, but this is outside the scope of this paper.
To conclude, the clinician needs to consider the need for glove use and if they are using gloves, choose the most sustainable ones. There is increasing information to help clinicians in this task.
Personal protective equipment: plastic aprons/gowns and disposable or reusable clothing
The recommendation by HTM 01-05 to use plastic disposable clothing does not come without consequences. Vozzolla showed that using reusable gowns rather than disposable gowns lowered energy (64%), carbon dioxide equivalent emissions (66%), water consumption (83%) and solid waste (84%).49
According to Rizan,11 the carbon footprint of a plastic apron is 65 grams. Within their research, they demonstrated that aprons accounted for 27% of the carbon footprint of NHS PPE.11
There are other advantages in considering reusable (washable) clothing compared with disposable clothing. Disposable gowns do not for example always meet specifications for impact penetration water resistance.50
Remote decontamination unit
Although HTM 01-05 is a guide to decontamination within the dental practice, some practices may opt to outsource the reprocessing of their instruments to other organisations. The vehicle emissions that result from transporting instruments to and from dental practices are harmful to the population, contributing to air pollution (particulate matter, carbon monoxide and nitrogen dioxide) and atmospheric carbon dioxide and other greenhouse gases. In 2001, remote decontamination facilities were used by 8% of dental practices in the UK but it is not known how this proportion has changed over the last 20 years.51Further research is also needed to quantify the distances that instruments travel between dental practices and reprocessing facilities and the impact that this transportation has on the environment. As an example, a Leeds facility provides instrument reprocessing services to medical and dental services as far afield as Manchester. The 145 km round trip in a light commercial vehicle would result in 8.7 seconds worth of DALYs lost from the population for every kilogram of products transported (based on ecoinvent data). Multiple trips per week from healthcare services across the region mean the DALYs would quickly accumulate. DALYs from travel to remote decontamination facilities occur in addition to the environmental and human health impacts of the decontamination process, with no appreciable benefits to patient safety. For this reason, we cannot recommend remote instrument decontamination and recommend more evidence on their benefits in terms of resource use/savings.
Single use instruments (including single use trays)
HTM 01-05 suggests that difficult-to-clean reusable instruments and those for which a reliable cleaning regimen is not available should be replaced with single-use instruments. However, considerable research on the environmental impact of single-use instruments emphasises the environmental consequences of this practice. An LCA by Rizan and Bhutta (2021) evaluated the environmental impact of hybrid laparoscopic instruments (single use and reusable components) and their single use equivalents.12They found that the carbon footprint of using hybrid instruments was 76% lower than using the single-use equivalent, saving 5.4 kg CO2e per operation. Similarly, Sherman et al. (2018) conducted a LCA to compare reusable and single-use laryngoscopes and found that single use devices generated 16-18 times more life cycle carbon dioxide equivalents than reusable alternatives.52 It was concluded that reusable instruments had a significantly lower environmental impact. Lastly, Byrne et al. compared the impact of reusable and disposable dental examination kits.10Through a life cycle analysis, they concluded that the disposable dental examination kits had a three-fold increase in DALY impact compared to the reusable kits, accounting for approximately 11 seconds of lost human life, primarily attributed to global warming. As such, we conclude that single use items that pose no appreciable benefit to patient safety should not be recommended.
Single use wipes
Like most decontamination processes the healthcare operator needs to consider both the environmental. In a recent ecoinvent LCA (undertaken for a textbook the authors are writing), it was shown that the reusable wipes contributed a high environmental footprint, with the worst single use wipe (quantity per patient four wipes) contributing 0.45 grams of carbon equivalent emissions. Converting this, along with other environmental impacts shows that a wipe can cause 4.5 seconds of DALY loss.53
There is only limited evidence to suggest that single use/disposable wipes are better from a decontamination perspective than the reusable wipes.
Single use wipes come already impregnated with disinfectant solution, with a constant wipe to disinfectant ratio.54 In addition, these cloths do not require the environmental cost of regular laundry. However, despite this, there is a greater environmental impact associated with the production, procurement, storage and disposal of single use wipes.55
Reusable wipes have the benefit of being multiple use and relatively inexpensive if made from recycled cloths.56 Laundering these wipes may potentially be ineffective in eliminating all microbes leading to a risk of contamination of surfaces.57 The evidence also suggests that reusable cloths may be incompatible with certain disinfectant solutions.58Furthermore, the process of regular laundry of reusable wipes has an environmental impact, associated with transport as well as the process of the laundry itself.
More research is needed to examine the reusable/disposable surface decontamination to weigh up the benefits in terms of the patient safety/environmental consequence.
Cleaning products (for example, sodium hypochlorite)
There are probably more sustainable products to replace the various cleaning products for example, hypochlorite that we use but a literature review is required on this. Within the LCA ecoinvent-based research we undertook for our textbook, we found that the environmental consequences of the disinfection product came from the water bottle, both in its material, manufacture and disposal (see Figure 2). These impacts need to be considered, with any recommendations of products such as this also informing health professionals of the need to purchase products in higher concentrations (less packaging) or better, more environmentally sensitive packaging.
Thermal and/or disinfection cleaning; results from our LCA
HTM 01-05 states that uniforms and workwear should be washed at the hottest temperature suitable for the fabric to reduce any potential microbial contamination- assume this would be the same for non-disposable hand drying towels.
Our life cycle analysis compared the DALYS of thermal disinfection (71 degrees), chemo-thermal disinfection (50 degrees) and chemical disinfection (25 degrees) of washing one kilogram of clothing. The biggest problem with using these chemicals is their associated carbon footprint and water consumption. The highest contributor to DALYS is chemo-thermal disinfection. According to the LCA results, thermal disinfection resulted in significant less DALY seconds (18 seconds) lost compared to the other methods of disinfection (chemo thermal); 18 seconds and just chemical, 27 seconds. We therefore do not recommend the use of chemothermal disinfection over thermal.
Wrapping of instruments
Sterile barrier systems are needed to prevent microbial contamination of sterile dental instruments.59
Most research into sterilisation barrier systems focuses on blue single use wrapping in operating theatres but in dental practices sealable plastic and paper pouches are most used.
Sterile pouches can be separated into their constituent parts and recycled60 but reuse is not recommended. However, there is some evidence that if packaging integrity is maintained instruments can be used clinically and sterilised up to three times and stored for 6 months without internal microbial contamination of the pouch.61
Opportunities exist for dentists to use reusable sterilisation packaging. Rigid containers can be used for sterilisation, transportation and storage of instruments with as previously discussed a much lower environmental footprint. However, these containers can be bulky and hold large volume of instruments that may be unsuitable for dental practices and may not fit standard autoclaves.
Food and Drug Administration-registered reusable instrument pouches have also been developed and are in use clinically in the USA; however, these require ISO certification before they can be used in the UK.62
Reusable instrument wraps are a viable alternative, however, may have a larger environmental impact than disposable wraps due to the laundering process.63 An LCA is needed to compare the environmental impact of all the available packaging options and make recommendations to clinicians.
HTM 01-05 recommend that wrapped sterilised instruments can be stored for up to 12 months before they must be reprocessed. These recommendations may be too restrictive and the evidence supporting this time-related shelf life is limited. Setting an expiry date has consequences for the availability of resources and harms to the environment and to human health. Dental instruments sterilised and cultured at intervals over a period of a year showed no increased likelihood of contamination with increasing time.64 After one year, only 3 out of the 300 sterilised instruments showed any microbial growth at all and because this was not time dependent, the authors suggest that the recontamination may have occurred during the culturing process. Similar studies of medical instruments showed maintenance of sterility from six months up to two years and in one case up to ten years.65 However the methodologies used vary and some limitations including only small numbers of instruments being tested at longer time intervals. Recontamination of instruments may be affected by how the wrapped instruments are stored (humidity, temperature, wrapping material etc) and the choice of wrapping material.
There is evidence that a move towards event-related shelf life may be a more appropriate, sustainable and efficient approach to maintaining instrument sterility. Instruments should be sterile unless their packaging is compromised. Event-related shelf life is used in decontamination guidance from Australia,18 New Zealand,15 Scotland16and Canada.13 These policies reduce the need for reprocessing unused instruments with the associated environmental impact; however, such change would require policies and procedures that ensure sterility is maintained, for example labels which encourage staff to check packaging integrity before opening and rotation of instruments in storage.
HTM 01-05 states that unwrapped instruments require reprocessing after one week if stored away from clinical areas and 1oneday if stored in the clinic. A literature review is needed to determine if these expiry dates are evidence based.
More research to investigate and understand the various modalities of instrument wrapping is needed, both from an infection control and resource use perspective.
Conclusion
From an environmental sustainability perspective, the world is quite a different place from when HTM 01-05 was updated eight years ago. We are increasingly aware of the impact our resource manufacture, use and disposal have on both planetary health and in turn, human health. We urge the department of health and other similar organisations internationally to consider our thoughts on environmental sustainability.
References
NHS England. (HTM 01-01) Decontamination of surgical instruments. 2021. Available at https://www.england.nhs.uk/publication/decontamination-of-surgical-instruments-htm-01-01/ (accessed October 2021).
Richardson J, Grose J, Manzi S et al. What's in a bin: A case study of dental clinical waste composition and potential greenhouse gas emission savings. Br Dent J 2016; 220: 61-66.
Almutairi W, Saget S, McDonnell J et al. The planetary health effects of COVID-19 in dental care (life cycle assessment approach). Br Dent J 2022; 233: 309-316.
Lenzen M, Malik A, Li M et al. The environmental footprint of health care: a global assessment. Lancet Planet Health 2020; DOI: 10.1016/S2542-5196(20)30121-2.
Duane B, Stancliffe R, Miller F A, Sherman J, Pasdeki-Clewer E. Sustainability in Dentistry: A Multifaceted Approach Needed. J Dent Res 2020; 99: 998-1003.
NHS England. Delivering a net zero NHS. Available at https://www.england.nhs.uk/greenernhs/a-net-zero-nhs/ (accessed July 2022).
The Intergovernmental Panel on Climate Change. Available at https://www.ipcc.ch/ (accessed November 2021).
United Nations. UN Report: Nature's Dangerous Decline 'Unprecedented'; Species Extinction Rates 'Accelerating'. Available at https://www.un.org/sustainabledevelopment/blog/2019/05/nature-decline-unprecedented-report/ (accessed December 2021).
World Wildlife Fund. Water scarcity: Overview. Available at https://www.worldwildlife.org/threats/water-scarcity#:~:text=Billions%20of%20People%20Lack%20Water,may%20be%20facing%20wa (accessed December 2021).
Byrne D, Saget S, Davidson A et al. Comparing the environmental impact of reusable and disposable dental examination kits: a life cycle assessment approach. Br Dent J 2022; 233: 317-325.
Rizan C, Reed M, Bhutta M F. Environmental impact of personal protective equipment distributed for use by health and social care services in England in the first six months of the COVID-19 pandemic. J R Soc Med 2021; 114: 250-263.
Rizan C, Bhutta M F. Environmental impact and life cycle financial cost of hybrid (reusable/single-use) instruments versus single-use equivalents in laparoscopic cholecystectomy. Surg Endosc 2021; 36: 4067-4078.
Canadian Dental Association. Infection Prevention and Control in the Dental Office. 2006. Available at https://www.yumpu.com/en/document/read/11540682/infection-prevention-and-control-in-the-dental-office-saskatchewan- (accessed December 2021).
Dental Council of Ireland. Code of Practice Relating to: Infection Prevention and Control. 2015. Available at http://www.dentalcouncil.ie/files/IPC%20Code%20-%20Final%20-%2020150402.pdf (accessed December 2021).
Dental Council of New Zealand. Infection Prevention and Control Practice Standard. 2015. Available at https://www.dcnz.org.nz/assets/Uploads/Consultations/2015/Infection-prevention-and-control-practice-standard-effective1May16.pdf (accessed December 2021).
Scottish Dental Clinical Effectiveness Programme. Decontamination Into Practice. Available at https://www.sdcep.org.uk/published-guidance/decontamination/ (accessed December 2021).
Centers for Disease Control and Prevention. Summary of Infection Prevention Practices in Dental Settings. Available at https://www.cdc.gov/oralhealth/infectioncontrol/pdf/safe-care2.pdf (accessed December 2021).
Australian Dental Association. Guidelines for Infection Prevention and Control. 2021. Available at https://www.ada.org.au/Dental-Professionals/Publications/Infection-Control/Guidelines-for-Infection-Control/Guidelines-for-Infection-Control-V4.aspx (accessed December 2021).
Ecoinvent. Ecoinvent Database (version 3.7.1). Available at https://ecoinvent.org/the-ecoinvent-database/data-releases/ecoinvent-3-7-1/ (accessed December 2021).
OpenLCA. Available at https://www.openlca.org/ (accessed December 2021).
European Commission. Environmental Footprint and Material Efficiency Support for Product Policy. 2015. Available at http://publications.jrc.ec.europa.eu/repository/bitstream/JRC95187/lb-na-27200-en-n.pdf (accessed December 2021).
McDonnell G, Burke P. Disinfection: is it time to reconsider Spaulding? J Hosp Infect 2011; 78: 163-170.
Rutala W A, Weber D J. How to assess risk of disease transmission to patients when there is a failure to follow recommended disinfection and sterilization guidelines. Infect Control Hosp Epidemiol 2007; 28: 146-155.
Roy K M, Ahmed S, Cameron S O et al. Patient notification exercise following a dentist's admission of the periodic use of unsterilized equipment. J Hosp Infect 2005; 60: 163-168.
Mason B W, Cartwright J, Sandham S, Whiteside C, Salmon R L. A patient notification exercise following infection control failures in a dental surgery. Br Dent J 2008; DOI: 10.1038/sj.bdj.2008.656.
Redd J T, Baumbach J, Kohn W, Nainan O, Khristova M, Williams I. Patient-to-patient transmission of hepatitis B virus associated with oral surgery. J Infect Dis 2007; 195: 1311-1314.
Bradley K, Fox J, Wilson J, Harris T, VanBuskirk K, Schaefli N. Investigation of Healthcare-Associated Hepatitis C Virus Transmission in a Dental Surgical Clinic - Oklahoma, 2013. Presented at Council of State and Territorial Epidemiologists Conference. Pasadena: California, 2013.
European Commission. Life Cycle Assessment using ReCiPe. Available at https://ec.europa.eu/environment/biodiversity/business/assets/pdf/case-studies/Case%20study%2016_ReCiPe%20Hand%20drying%20systems_final.pdf (accessed December 2021).
International Trade Administration. Netherlands - Country Commercial Guide. Available at https://www.trade.gov/country-commercial-guides/netherlands-energy (accessed December 2021).
Pitt S J, Crockett S L, Andreou G M. The contribution of hand drying in prevention of transmission of microorganisms: comparison of the efficacy of three hand drying methods in the removal and distribution of microorganisms. J Infect Prev 2018; 19: 310-317.
Mutters R, Warnes S L. The method used to dry washed hands affects the number and type of transient and residential bacteria remaining on the skin. J Hosp Infect 2019; 101: 408-413.
Reynolds K A, Sexton J D, Norman A, McClelland D J. Comparison of electric hand dryers and paper towels for hand hygiene: a critical review of the literature. J Appl Microbiol 2021; 130: 25-39.
Gendron L M, Trudel L, Moineau S, Duchaine C. Evaluation of bacterial contaminants found on unused paper towels and possible postcontamination after handwashing: a pilot study. Am J Infect Control 2012; DOI: 10.1016/j.ajic.2011.07.007.
Duane B, Pilling J, Saget S, Ashley P, Pinhas A R, Lyne A. Hand hygiene with hand sanitizer versus handwashing. What are the planetary health consequences? Environ Sci Pollut Res Int 2022; 29: 48736-48747.
Heinze J E, Yackovich F. Washing with contaminated bar soap is unlikely to transfer bacteria. Epidemiol Infect 1988; 101: 135-142.
Zapka C A, Campbell E J, Maxwell S L et al. Bacterial hand contamination and transfer after use of contaminated bulk-soap-refillable dispensers. Appl Environ Microbiol 2011; 77: 2898-2904.
Schmidt J, Pizzol M. Critical review of four comparative life cycle assessments of printed and electronic communication. 2014. Available at https://lca-net.com/files/Review_of_four_LCAs_on_printed_versus_electronic_media.pdf (accessed December 2021).
Suksuwan A, Matossian A, Zhou Y, Chacko P, Skerlos S. Environmental LCA on three note-taking devices. Procedia CIRP 2020; 90: 310-315.
Time for Change. Plastic bags and plastic bottles - CO2 emissions during their lifetime. Available at https://timeforchange.org/plastic-bags-and-plastic-bottles-co2-emissions-during-their-lifetime/ (accessed December 2021).
Sciencing. What Is the Carbon Footprint of a Plastic Bottle? Available at https://sciencing.com/carbon-footprint-plastic-bottle-12307187.html (accessed December 2021).
Grimmond T. Using reusable containers for hospital waste: is there an infection risk? S A J Epidemiol Infect 2013; 28: 197-201.
Grimmond T, Rings T, Taylor C et al. Sharps injury reduction using Sharpsmart - a reusable sharps management system. J Hosp Infect 2003; 54: 332-238.
Grimmond T, Bylund S, Anglea C et al. Sharps injury reduction using a sharps container with enhanced engineering: a 28 hospital nonrandomized intervention and cohort study. Am J Infect Control 2010; 38: 799-805.
World Health Organisation. Glove use Information Leaflet. Available at https://cdn.who.int/media/docs/default-source/integrated-health-services-(ihs)/infection-prevention-and-control/hand-hygiene/tools/glove-use-information-leaflet.pdf?sfvrsn=13670aa_10&download=true (accessed December 2021).
Jamal H, Lyne A, Ashley P, Duane B. Non-sterile examination gloves and sterile surgical gloves: which are more sustainable? J Hosp Infect 2021; 118: 87-95.
Best Silicone Reviews. Silicone Vs Rubber: What's The Difference And Which Is Better. Available at https://bestsiliconereviews.com/silicone-vs-rubber/ (accessed December 2021).
Brown B C, Dubrovskiy A, Gvetadze A R, Phalen R N. Chemical permeation of similar disposable nitrile gloves exposed to volatile organic compounds with different polarities: Part 1: Product variation. J Occup Environ Hyg 2020; 17: 165-171.
Phalen R N, Wong W K. Chemical resistance of disposable nitrile gloves exposed to simulated movement. J Occup Environ Hyg 2012; 9: 630-639.
Vozzola E, Overcash M, Griffing E. An Environmental Analysis of Reusable and Disposable Surgical Gowns. AORN J 2020; 111: 315-325.
McQuerry M, Easter E, Cao A. Disposable versus reusable medical gowns: A performance comparison. Am J Infect Control 2021; 49: 563-570.
Coulter W A, Chew-Graham C A, Cheung S W, Burke F J. Autoclave performance and operator knowledge of autoclave use in primary care: a survey of UK practices. J Hosp Infect 2001; 48: 180-185.
Sherman J D, Raibley L A 4th, Eckelman M J. Life Cycle Assessment and Costing Methods for Device Procurement: Comparing Reusable and Single-Use Disposable Laryngoscopes. Anesth Analg 2018; 127: 434-443.
Duane B. Sustainable Dentistry: Making a Difference. 2022. Available at https://link.springer.com/book/9783031080012 (accessed August 2022).
Sattar S A, Maillard J-Y. The crucial role of wiping in decontamination of high-touch environmental surfaces: review of current status and directions for the future. Am J Infect Control 2013; DOI: 10.1016/j.ajic.2012.10.032.
Boyce J M. A review of wipes used to disinfect hard surfaces in health care facilities. Am J Infect Control 2021; 49: 104-114.
Diab-Elschahawi M, Assadian O, Blacky A et al. Evaluation of the decontamination efficacy of new and reprocessed microfiber cleaning cloth compared with other commonly used cleaning cloths in the hospital. Am J Infect Control 2010; 38: 289-292.
Sifuentes L Y, Gerba C P, Weart I, Engelbrecht K, Koenig D W. Microbial contamination of hospital reusable cleaning towels. Am J Infect Control 2013; 41: 912-915.
Infection Control Today. Optimizing Disinfectant Application in Healthcare Facilities. 2006. Available at https://www.infectioncontroltoday.com/view/optimizing-disinfectant-application-healthcare-facilities (accessed July 2022).
British Standards Institution. Packaging for terminally sterilized medical devices - Requirements for materials, sterile barrier systems and packaging systems. 2020. Available at https://knowledge.bsigroup.com/products/packaging-for-terminally-sterilized-medical-devices-requirements-for-materials-sterile-barrier-systems-and-packaging-systems-1/standard (accessed December 2021).
Perfection Plus. Protect+ Self-Seal Sterilisation Pouches. Available at https://perfectionplus.com/shop/infection-control/cleaning-sterilisation/protect-self-seal-sterilisation-pouches/ (accessed December 2021).
Klumdeth J, Jantaratnotai N, Thaweboon S, Pachimsawat P. Sterility maintenance of reused disposable paper/plastic sterilization pouches in actual clinical practice. Heliyon 2020; DOI: 10.1016/j.heliyon.2020.e03672.
Enviropouch. EnviroPouch Reusable Steam Sterilization Pouches. Available at https://www.enviropouch.com/ (accessed December 2021).
Hart J. Not As "Green" As It Seems: Reusable Sterilization Wrap. 2012. Available at https://www.greenhealthcare.ca/images/publications/ReusableWrapCanada-JaneHart.pdf (accessed December 2021).
Schwartz R, Davis R. Safe storage times for sterile dental packs. Oral Surg Oral Med Oral Pathol 1990; 70: 297-300.
Lakhan P, Faoagali J, Steinhardt R, Olesen D. Shelf life of sterilized packaged items stored in acute care hospital settings: factors for consideration. Healthcare Infect 2013; 18: 121-129.
Author information
Authors and Affiliations
Contributions
Brett Duane is corresponding author, developed the paper idea, wrote the paper, formatted the introduction, edited each section, supported LCA, analysed the HTM 01-05 document and produced the paper towel section. Darshini Ramasubbu produced the Helix Test section. Mark Johnstone supported the writing of the introduction and provided information on decontamination within CDS. Taylor McKerlie supported the LCA and provided analysis of other countries documents. Amarantha Fennell- Wells produced the sections on autoclave and disinfection. Brian Maloney supported LCA and provided analysis of other countries documents. John Crotty produced the section on autoclave and disinfection. Sheryl Wilmott produced the section on travel. Paul Ashley jointly wrote the introduction, reviewed the manuscript and produced the hand hygiene section.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
Supplementary Information
Rights and permissions
About this article
Cite this article
Duane, B., Ashley, P., Ramasubbu, D. et al. A review of HTM 01-05 through an environmentally sustainable lens. Br Dent J 233, 343–350 (2022). https://doi.org/10.1038/s41415-022-4903-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-022-4903-5