Abstract
Respiratory protection in the dental setting has become more important to protect healthcare professionals, their household members and their patients. As dental practices become increasingly independent in managing their respiratory protection requirements, the need for an in-depth understanding of the principles of respiratory protection is warranted. This article aims to enhance the awareness of dental professionals about the principles of respiratory protection and equipment, including designs, classification and levels of protection afforded to wearers. Determining the adequacy and suitability of respiratory protection, along with ensuring safe selection of appropriate equipment for protection of both wearer and patient, is described. Moreover, a detailed review of fit testing principles, procedures and governance are described. This comprehensive review should ensure that dental professionals are ideally placed to understand the implications of respiratory protection and safely apply it in their workplaces.
Key points
-
Describes the principles of respiratory protection in the dental workplace.
-
Details the characteristics of different respiratory protective equipment, including the appropriateness of each in dental settings.
-
Explains the fundamental principles of fit testing.
Similar content being viewed by others
Introduction
The most recent hazard affecting dental professionals is severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing coronavirus disease 2019 (COVID-19). It can spread in droplets via three main modes:1
-
Direct or indirect contact
-
Droplet spray; for example, coughing and sneezing
-
Airborne transmission; for example, aerosols.
Self-protection from SARS-CoV-2 includes following advice on repeated washing of hands and thorough cleaning of surfaces, which have long been commonplace in healthcare settings.2 Ear, nose and throat surgeons, ophthalmologists, anaesthetists and dentists operate in positions where social distancing is largely impossible, but respiratory protection may at least mitigate the risks of social distancing limitations.3 There remains much debate on the potential of aerosols created from dental equipment transferring the virus and the science is still developing, but at the time of writing, we are assuming that virus-containing aerosols may be inhaled and potentially transmit the SARS-CoV-2 virus.4,5 Faced with an airborne hazard in the dental workplace, using the right personal protective equipment (PPE) also includes the appropriate understanding, training and selection of respiratory protective equipment (RPE).6
Respiratory protective equipment
RPE is a form of PPE that is used to protect the individual wearer against the inhalation of hazardous substances in the workplace environment.7 This is different from a surgical mask, which is a fluid-resistant barrier that is not designed to protect the wearer. Although some larger droplets may be prevented from penetrating a surgical mask, its main function is protecting the patient from the wearer.8
In contrast, a respirator is designed to protect the wearer's respiratory tract. It acts as an air-filtering device and requires a seal to optimally protect the individual wearing it. RPE must not be used as a single mitigating factor. Routine use of rubber dam, high-volume suction, ventilation, and the use of air purifiers and negative pressure environments could also reduce the hazard.9 Current guidance has not suggested that these additional measures of risk management are enough to render respiratory protection unnecessary.
Types of respiratory protective equipment
There are six main types of respirators with particle filters:
-
1.
Disposable half-mask/filtering facepiece (FFP) (Fig. 1a)
-
2.
Reusable half-mask (Fig. 1b)
-
3.
Full-face mask (Fig. 1c)
-
4.
Powered half-mask
-
5.
Powered full-face mask
-
6.
Loose-fitting powered facepieces (Fig. 1d).
In the case of SARS-CoV-2, an airborne microbial biohazard, there is a lack of evidence on the true level of the ambient hazard and the concentration of the hazardous particles in the workplace air that can be accepted, otherwise known as the workplace exposure limit (WEL). In relation to dentistry, guidelines from Public Health England (PHE) state that equipment fitted with the highest efficiency of filtering capacity possible must be used to maintain exposure to the lowest possible levels. Such efficiency is determined by an assigned protection factor (APF) which is the level of protection that a respirator can be expected to provide 95% of the time. An FFP3 respirator has an APF of 20, meaning that the respirator can be used safely in an atmosphere that has a hazardous concentration of up to 20 times the WEL.10 PHE have declared that this category of respirator, that would require fit-testing to ensure the selected facepiece fits the wearer correctly, should be worn in addition to other PPE, such as long-sleeve disposable gowns, gloves and eye protection.11 The World Health Organisation (WHO) recommends at least an FFP2 respirator for aerosol generating procedures (AGPs) and PHE has stated that, in the absence of availability of FFP3 respirators, FFP2 respirators are an acceptable alternative.12 FFP2 respirators are also tight-fitting facepieces therefore would also require fit testing.
There is a variation on how RPE is classified across the world. In the US, for example, respirators carry an 'N95' classification. An equivalent respirator in China would carry a 'KN95' classification. These classify the level of filtering capacity that the respirator carries. KN95 and N95 laboratory testing does not, however, take into account inward leakage from the seal around the edges of the respirator.13 In the European Union (EU), filtering capacity is not the only standard by which respirators are classified; they are additionally tested on their ability to create a seal to the face by testing with paraffin oil, which is thought to be the most appropriate simulation of the particle size of the SARS-CoV-2 virus. N95 masks are not eligible to be sold legally in the UK unless they have gone through an assessment and fast-tracking by the EU, at which point they would be reclassified as an FFP2 respirator. KN95 masks are not eligible to be sold in the UK at all.14
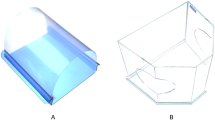
Classification of respirators according to filtering capacity only
Respirators that are classified in China or the US are assessed according to their filtering capacity. KN95 or KN99 respirators are Chinese in origin (Fig. 2a) and N95 or N99 respirators have been classified in the US (Fig. 2b). They are essentially identical. A KN95/N95 respirator carries a filtering capacity of approximately 95% and a KN99/N99 respirator carries a filtering capacity of approximately 99%.12,13 No respirator offers a 100% filtering capacity.
Classification of respirators according to the seal on the face
In the UK and Europe, the filtering capacity alone is not sufficient to pass the classification standards. In addition to the filtering capacity, the respirator must also be assessed for its performance as a facepiece - that is to say, how well it seals to the skin of the face. A respirator with a decent filtering capacity that does not seal adequately to the skin of the face is considered substandard, as the loose fit is considered to allow the hazardous substance to pass through the side of the facepiece and into the oral cavity through to the respiratory system. The seal to the skin is what defines the respirator as a facepiece and therefore the term 'filtering facepiece' (FFP) is given to the respirator.13
Once assessed for the suitability of the seal to the face, the facepiece is then further classified by its filtering capability. An FFP2 respirator carries a filtering capacity of approximately 94% and an FFP3 respirator carries a filtering capacity of approximately 99% (Fig. 2c).
Equivalence
When considering filtering capacity alone, KN95, N95 and FFP2 respirators are considered equivalent, and KN99, N99 and FFP3 respirators are also considered equivalent. KN95 respirators have been deemed by the Health and Safety Executive (HSE) as unsuitable for use in the UK;14 however, if an N95 mask undergoes further assessment by UK/European standards, its ability to seal the face can be determined. If a mask classified according to its filtering capacity alone is further tested for its face-fitting standard and passes, it would then be reclassified. An N95 mask would be reclassified as an FFP2 respirator and an N99 mask would be reclassified as an FFP3 respirator. It is for this reason that perfectly viable N95 and N99 respirators are found in the UK market.
Ear loops and head straps
Respirators come with ear loops or head straps. The success of a fit test and the subsequent use depends on the stability and reproducibility of the position of the respirator. The occipital bone provides a much greater level of stability than the ears. Some suppliers have produced straps that can extend between the loops across the back of the head to secure the respirator more firmly.
Disposable respirators
A disposable respirator is made of cloth-like filtering material and is designed for single use. That is not to say that it must necessarily be replaced for every patient, but once the face seal has been broken, it is considered to be less effective. A disposable respirator can be worn for sessional use for multiple patients as long it does not become wet or soiled.11 The use of an overlying face shield may be useful in protecting the surface of the respirator from splatter. Disposable respirators must not be shared between clinicians.
Valves
A valved respirator (Fig. 3a) will allow the wearer to exhale more easily than a valveless respirator (Fig. 3b). This could be particularly useful for an FFP3 respirator as the increased resistance of the filter makes it more difficult to breathe. It does, however, mean that, although the wearer is protected from the patient, the patient is less protected from the wearer than if they were wearing a valveless respirator.15 Some professional bodies have advocated placing a surgical mask over a valved respirator to afford additional protection to the patient from the wearer (Fig. 3c).16 Valves also reduce the build-up of moisture, lengthening the lifespan of the respirator.
Counterfeit respirators
The PPE market has unfortunately become infiltrated with counterfeit respirators, putting wearers at risk. As with any counterfeit product, differentiating a counterfeit from a genuine one comes with experience. Any respirator should have specified markings on it to state it conforms to EU/UK standards (Fig. 4):17
-
1.
Manufacturer name/logo
-
2.
EU standard number; for example, EN149:2001+A1:2009
-
3.
EU certification mark: CE
-
4.
Notified Body number (that is, 2797) responsible for product certification next to CE mark
-
5.
Manufacturer model number
-
6.
Type of respirator; for example, FF = filtering facepiece, NR = non-reusable, R = reusable.
Reusable respirators
In contrast, a reusable respirator is made of silicone or neoprene rubber and is designed to be worn for multiple patient uses, sterilised and disinfected between use. As a reusable respirator will last for longer, it is likely to be more cost-effective.
Cleaning a reusable respirator
Reusable respirators have protocols for storage, cleaning and maintaining, and as the filters may come with a covering, there is less concern about droplet contamination as they can simply be wiped clean. Manufacturers' instructions must be followed when cleaning the respirator, using the recommended cleaning products. Cleaning should be carried out away from the clinical environment to avoid contamination and should involve dismantling the removal parts of the respirator so that each part can be cleaned separately (Figures 5a and 5b).
Gloves, another respirator and eye protection could be worn while cleaning the respirators, and hands should then be washed. Reusable respirators can be shared among clinicians as long as strict disinfection measures are adhered to.
Maintenance of reusable respirators
Maintenance is important when using respirators and must be carried out by trained personnel who understand their legal and professional obligations. Thorough maintenance that involves dismantling the device should be carried out at least once a month, but a superficial inspection must also be completed before each use. Such inspections must include careful examination of the head straps, valve, facepiece, diaphragm and filters. Techniques on maintenance and inspections of a respirator must be taught to the wearer by the fit-tester so that they can be carried out in accordance with the manufacturers' instructions.
Maintenance records must be kept and must include details of the examination, repairs and any replacements that have taken place. Tasks that should be recorded and are key for maintaining respirators include:18
-
1.
Changing replaceable filters
-
2.
Cleaning the device
-
3.
Valve maintenance and replacement
-
4.
Checking the straps for damage
-
5.
Checking the battery charge and flow rate for powered devices.
All dental practices should have a local infection control policy,2 and this should have a section dedicated to how PPE should be worn and changed. For respirators, local policy should also be dedicated to how they are worn, stored and maintained.
Once cleaned, the reusable respirators must be stored responsibly, ideally in a sealed box and away from any clinical area to avoid any contamination.18
Reusable masks come with detachable filters (Fig. 6) that have a limited capacity and can become clogged, making breathing difficult for the wearer. Filters must therefore be replaced following manufacturers' instructions, or when the wearer feels that they are no longer effective. Typically, filters need replacing after 28 days of eight-hour daily use.
If any parts need to be replaced, then they should be sourced from the original manufacturer. This will ensure that the replaced parts continue to allow the respirator to continue to work in the same way it was designed. Any modifications or use of parts that are not recommended by the manufacturer are a risk and are likely to void the warranty.
Difficulties with wearing a respirator
Inevitably, the facial barrier will affect the tone of our voice and the facial expressions we portray. This has been of little relevance to industries where respiratory protection has so far been traditionally used. For healthcare providers delivering invasive treatments under local anaesthesia to conscious patients, communication with empathy is vital.19 Changes in practice will inevitably be required as well as changes in patient expectations.
Some wearers have reported claustrophobia, disorientation and difficulty in breathing.20,21 This may be a genuine inability to tolerate the facepiece or it may be a matter of time until the wearer becomes accustomed to it with increased experience in use. The facepieces are filtering devices, rather than obstructive to airflow, and are not associated with hypoxia. It is difficult to wear a respirator for much more than an hour, partly due to the increased effort it takes to breathe, but also because the wearer may (by then) be tempted to touch and adjust the respirator and break the seal.22 Some reusable respirators sit rather high over the bridge of the nose, meaning spectacles and loupes cannot be worn in the correct position (Figures 7a, 7b and 7c). Tight-fitting facepieces may be associated with facial bruising after prolonged wear (Fig. 8).
Loose-fitting respirators
The alternative to the tight-fitting FFP is the loose-fitting powered air-purifying respirator (PAPR) (Fig. 1d). There is no need to be clean-shaven when using a PAPR and it does not cause bruises to the face of the wearer. This is a vitally important advantage to wearers who are unable or unwilling to be clean-shaven for religious, cultural or dermatological reasons. As PAPRs do not depend on a tight seal to the skin of the face, they do not require fit testing.18 They do, however, come with other challenges to overcome, such as: the waist-worn power pack impeding the operator's chair and causing postural discomfort;23 the loupes-mounted light reflecting off the inside of the hood shield; and an inability to use microscopes.24 They are also rather expensive. Wearers have reported facing difficult decision-making dilemmas on having to avoid performing AGPs.25
Loose-fitting respirators can be shared among clinicians as long as strict disinfection measures are adhered to.
Fit testing
Once a wearer selects a respirator, they must check that it fits them correctly, as brands vary in how well they fit and therefore how effective their function would be. While a tight-fitting facepiece may feel comfortable, assessing the effectiveness of the seal to the wearer's face with formal fit testing is essential. It is a legal requirement that workers using tight-fitting RPE (facepieces/masks) are fit-tested by a competent person.18,22 A dental professional can be appropriately trained and supported through practical mentorship in safely gaining experience and competency in performing facepiece fit testing. Fit testers must be indemnified to perform the task and this service may be offered by existing professional indemnity policies or through public liability insurance. The fit tester must seek advice from their providers before embarking on cases.
The need for fit testing
The performance of tight-fitting facepieces depends on achieving good contact between the wearer's skin and the face seal of the facepiece. Individuals' faces vary significantly in shape and size, so it is unlikely that one particular make and model or size of RPE facepiece will fit everyone.
The fit test is a vitally important method of determining the effectiveness of a tight-fitting respirator on individual wearers. There are some countries worldwide that do not adhere to this gold standard when selecting a respirator of use; however, the UK does. In modern clinical practice, with the variation of respiratory diseases and range of healthcare worker demographics, testing respirators for a suitable fit has become ever more important.
Fit testing procedures
In 2019, the HSE produced the helpful and timely Guidance on respiratory protective equipment (RPE) fit testing which clearly describes procedures to follow concerning face fit testing.26 There are two main methods applied to fit testing. The most common test is a qualitative test, which involves a taste test and relies on the person's taste perception. A quantitative test utilises a particle-counting machine, which will record the ambient particle count both outside of the respirator and within the respirator while it is fitted. Both methods are recognised ways of assessing the fit of half-mask disposable or reusable respirators, but a full-face respirator can only be quantitatively fit-tested.27
A passed fit-test not only assures compliance, but also reassures the wearer of the effective protection from the surrounding hazard. A failed fit-test caused by an ill-fitting or incorrectly worn respirator demonstrates that there is a leakage, suggesting the airborne hazard can pass through to the oral cavity. The fit-test would illustrate this to the wearer and can be utilised as a learning opportunity to help ensure a depth of understanding in respiratory protection concepts, in the hope of stronger compliance in use as instructed
The qualitative fit test method
This is the most commonly practised method of fit testing and utilises a method of aerosolising either saccharine or a bitter fluid called Bitrex around the respirator under controlled conditions to check if the wearer can taste it. Not tasting the Bitrex means that it hasn't breached the seal of the respirator and therefore hasn't entered the wearer's oral cavity.
The individual being tested wears a dosing hood that creates a confined space in which the solution can be introduced. The sensitivity solution is administered without the wearing of the respirator to check that the individual can indeed taste it and to check their sensitivity threshold. Once this is confirmed and 30 minutes has elapsed for the taste sensation to have disappeared, the fit test is conducted while wearing the respirator (Fig. 9). The wearer is asked to perform a series of seven controlled exercises mimicking routine face and head movements during the procedure. If at any point the wearer can taste the solution, then that implies that the seal of the respirator is not tight-fitting to the skin of the face and therefore does not fit. The exercises are: normal breathing; deep breathing; head side to side; head up and down; talking out loud; bending forward; and lastly normal breathing again. During the talking exercise, the wearer is asked to read 'the rainbow passage', a short paragraph containing wording with a variety of vowels and consonants to encourage full movement of the muscles of facial expression during speech. An alternative is to ask the subject to count downwards from 100. An optional add-on to the end is the 'reveal'. This is to verify the process; the respirator is then released while the wearer is still wearing the hood and they should confirm that the taste has now appeared.25
The quantitative fit test method
The qualitative fit testing method is subjective and relies on the wearer's taste sensation. Where there is any doubt, the quantitative method can be deployed. This utilises a machine that can detect particle counts both inside and outside the mask during wear (Fig. 10).28
Fit checking respirators
Fit testing must not be confused with fit checking (Fig. 11).29 A fit test should be carried out by the method described as part of the initial selection of RPE, and is specific to the type and model tested. Fit checking, otherwise known as a 'user seal check', is the responsibility of the wearer to ensure their RPE has been donned correctly every time they wear it.18 As well as checking that facepiece and straps are not in any way damaged or disturbed, the fit check comprises a combination of an inward negative pressure and exhalation positive pressure check for any leakages in the seal.
Facial hair
To create an adequate seal for a tight-fitting respirator, it must be in close contact with the skin. The HSE performed a study to show the effect that only one day of facial hair growth may lead to unacceptable levels of inward leakage.30 An unshaven face is defined as that which has 'hair which has not been shaved within the previous 8-hour period prior to the work shift'. PHE has also provided some visual guidance on what facial hairstyles are acceptable.31 If the wearer is unable or unwilling to shave for religious, cultural or dermatological reasons, then the wearer should consider alternative control measures such as the PAPR.
Working environment
Ideally, the conditions in which the wearer normally works should be mimicked during the test. This may include the wearing of the PPE that would be expected during patient care. If the clinician normally wears loupes, spectacles or a visor, then these should be worn during the test, as incompatibility may become apparent.
Validity of fit test
In the UK, the fit test is valid for a recommended maximum of two years. In the US, it is a legal requirement for the fit test to be repeated annually.32 A retaking of the test would also be required if there is a change in either the choice of respirator or if there are any changes in the facial features of the wearer.18 Such changes include but are not limited to:
-
Significant weight gain or loss
-
Changing loupes or spectacles
-
Changes in the facial structure.
The result of the fit test must be a written document that is recorded and kept in the wearer's personal governance file for the duration of its validity. A photograph of the respirator on which the wearer has passed may also be useful for the file.33
Fit test failures
Respiratory protection has not been required to such an extent in the medical and dental profession until recently. Previously, individuals that were routinely exposed to hazardous airborne substances were typically those that worked in industries such as construction, pest control or firefighters, for example. Stereotypically, these individuals tend to be male and of a relatively large stature, so manufacturing companies have developed supplies to cater for the market as it has thus far presented to them. Unfortunately, the stereotypically conversely petite female healthcare worker is not the type of individual the market has so far catered for, so the respirators tend not to fit this type of face. This current anomaly makes it vitally important for individuals to adhere to the regulations of fit testing their respirators.34 The onus is on manufacturers now to produce RPE suitable for the demographic range of healthcare workers requiring them.
Fit testers
There are several accredited fit testers nationwide,35 some of whom are dentists and some who have recently gained some experience in the clinical settings, which indeed varies greatly from working environments previously synonymous with hazardous airborne substances. Dental professionals are also encouraged to train to become fit testers themselves through accredited training courses,36 meaning they can offer their workplaces sustainability with their ongoing needs. Healthcare professionals must seek advice from their indemnity providers about the cover they have in place to perform the fit testing procedure and under what terms and conditions.37 A good-quality fit test training course would include both a didactic and practical element and ongoing mentorship to achieve competency.
Competency in fit testing
It is a legal requirement that workers using tight-fitting RPE (facepieces/masks) must be fit-tested by a competent person such as those accredited by the British Safety Industry Federation (BSIF). The law states that an individual performing fit testing must be certified as competent by an accredited body, but not necessarily be accredited themselves.
Fit testers should be competent in:18
-
Assisting in the selection of adequate and suitable RPE
-
Examination of RPE and the ability to identify poorly maintained and poorly fitting facepieces
-
Ability to correctly fit a facepiece and perform pre-use wearer seal checks
-
Awareness of external factors that may affect the fit of the facepiece or the fit test result
-
The differences between, and the appropriate use of, quantitative and qualitative testing methods
-
The purpose of the fit test exercises
-
Capabilities and limitations of the fit test equipment
-
How to perform a correct fit test
-
Awareness and knowledge of how to prevent and correct problems during fit testing
-
Interpretation of fit test results.
Conclusion
Infection prevention and control measures are already deeply engrained habits within the dental profession, arguably second only to healthcare workers in operating theatre settings. While thus far concentrating predominantly on protecting patients from potential hazards, efforts are now being additionally directed at protecting the clinical team from a threatening global airborne respiratory virus. For healthcare workers who operate in close proximity to patients' faces, therefore rendering social distancing impossible, the enhanced risk of viral transmission necessitates the need for enhanced protective measures in the form of RPE, the choice and use of which is dependent on the wearer's specific individual requirements.
References
Moriyama M, Hugentobler W J, Iwasaki A. Annual review of virology seasonality of respiratory viral infections. Annu Rev Virol 2020; 7: 83-101.
Department of Health. Health Technical Memorandum 05-01: Decontamination in primary care dental practices. Leeds: Department of Health, 2013.
Li R W K, Leung K W C, Sun F C S, Samaranayake L P. Severe Acute Respiratory Syndrome (SARS) and the GDP. Part II: Implications for GDPs. Br Dent J 2004; 197: 130-134.
van Doremalen N, Bushmaker T, Morris D H et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med 2020; 382: 1564-1567.
Stadnytskyi V, Bax C E, Bax A, Anfinrud P. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc Natl Acad Sci U S A 2020; 117: 11875-11877.
Shembesh T. What you need to know: PPE and fit-testing. 2020. Available at https://www.bda.org/news-centre/blog/what-you-need-to-know-ppe-and-fit-testing (accessed December 2020).
Health and Safety Authority. A Guide to Respiratory Protective Equipment. 2010. Available at https://www.hsa.ie/eng/Publications_and_Forms/Publications/Chemical_and_Hazardous_Substances/Respiratory%20Protective%20Equipment.pdf (accessed December 2020).
Health and Safety Executive. BS EN 14683:2019 - Medical face masks. Requirements and test methods. 2019. Available online at https://www.en-standard.eu/bs-en-14683-2019-medical-face-masks.-requirements-and-test-methods/ (accessed December 2020).
Al-Sehaibany F S. Middle east respiratory syndrome in children: Dental considerations. Saudi Med J 2017; 38: 339-343.
BSi British Standards. BS EN 529:2005 - Respiratory protective devices - Recommendations for selection, use, care and maintenance - Guidance document. 2005. Available at https://www.breathesafety.com/files/EN5292005RespiratoryProtectiondevices.pdf (accessed December 2020).
Public Health England. COVID-19 personal protective equipment (PPE). 2020. Available online at https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe#main-changes-to-previous-guidance (accessed April 2020).
Health and Safety Executive. Rapid evidence review: Delivered by HSE for the Government Chief Scientific Advisor- Part one: Equivalence of N95 and FFP2 masks - Part two: Aprons, gowns and eye protection. 2020. Available at https://www.hse.gov.uk/coronavirus/assets/docs/face-mask-equivalence-aprons-gown-eye-protection.pdf (accessed December 2020).
JSP. Comparison of International Disposable Dustmask Standards. 2020. Available online at https://guide.jsp.co.uk/covid-19/standards-compare/ (accessed December 2020).
Health and Safety Executive. Use of Face Masks Designated KN95. 2020. Available at https://www.hse.gov.uk/safetybulletins/use-of-face-masks-designated-kn95.htm (accessed December 2020).
3M. Filtering Facepiece Respirators FAQ: General Public. 2020. Available at https://multimedia.3m.com/mws/media/1791526O/respiratory-protection-faq-general-public-tb.pdf (accessed December 2020).
BAOMS & BAOS. FFP3 Masks With Valves should be avoided to reduce risk to patients during close interactions when a clinician is unknowingly COVID Positive. 2020. Available at https://www.baos.org.uk/wp-content/uploads/2020/05/15-May-BAOS-and-BAOMS-FFP3-masks-with-Valves.pdf (accessed December 2020).
BOHS. Spotting a Fake Respirator. 2020. Available online at https://www.bohs.org/app/uploads/2020/11/Spotting-a-Fake-Understanding-FFP-Markings-Branded-14_07_2020.pptx (accessed December 2020).
Health and Safety Executive. Respiratory protective equipment at work: A practical guide. 2013. Available online at https://www.hse.gov.uk/pubns/books/hsg53.htm (accessed December 2020).
Waylen A. The importance of communication in dentistry. Dent Update 2017; 44: 774-780.
Radonovich L J, Cheng J, Shenal B V, Hodgson M, Bender B S. Respirator tolerance in health care workers. JAMA 2009; 301: 36-38.
Moore D M, Gilbert M, Saunders S, Bryce E, Yassi A. Occupational health and infection control practices related to severe acute respiratory syndrome: health care worker perceptions. AAOHN J 2005; 53: 257-266.
Gosch M E, Shaffer R E, Eagan A E, Roberge R J, Davey V J, Radonovich L J. B95: A new respirator for health care personnel. Am J Infect Control 2013; 41: 1224-1230.
Matharu K. Beards and masks. Br Dent J 2020; 228: 814.
Singh G. Coronavirus: Why PAPR hoods are not the solution Sikh dentists need. 2020. Available at https://bda.org/news-centre/blog/coronavirus-why-papr-hoods-are-not-the-solution-sikh-dentists-need (accessed December 2020).
Rehman I. Facial hair revisited. Br Dent J 2020; 229: 699-700.
Health and Safety Executive. Guidance on respiratory protective equipment (RPE) fit testing. 2019. Available at https://www.hse.gov.uk/pubns/indg479.pdf (accessed December 2020).
Health and Safety Executive. RR1029 - Review of fit test pass criteria for Filtering Facepieces Class 3 (FFP3) Respirators. 2019. Available online at https://www.hse.gov.uk/research/rrhtm/rr1029.htm (accessed December 2020).
BSIF. Fit2Fit Companion to HSE INDG 479 Guidance on Respiratory Protective Equipment (RPE) fit testing: Qualitative Method. 2019. Available at https://www.fit2fit.org/wp-content/uploads/2019/04/Guidance-document-Qualitative.pdf (accessed December 2020).
Danyluk Q, Hon C Y, Neudorf M et al. Health care workers and respiratory protection: Is the user seal check a surrogate for respirator fit-testing? J Occup Environ Hyg 2011; 8: 267-270.
Frost S, Harding A-H. The effect of wearer stubble on the protection given by Filtering Facepieces Class 3 (FFP3) and Half Masks. Buxton: HSE Books Health and Safety Executive, 2015.
Public Health England. Facial Hair and FFP3 Respirators. 2020. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/877532/Facial_hair_and_FFP3_respirators_220320.pdf (accessed December 2020).
Occupational Safety and Health Administration. 1910.134 - Respiratory Protection. Available at https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.134 (accessed December 2020).
Rollings L. FFP3 respirator face fit testing - what is it all about? Br Dent J 2020; 229: 112-114.
Clayton M, Vaughan N. Fit for purpose? The role of fit testing in respiratory protection. Ann Occup Hyg 2005; 49: 545-548.
Fit2Fit. Fit2Fit Accredited RPE Fit Test Provider. 2020. Available online at https://www.fit2fit.org (accessed December 2020).
Fit2Fit. Fit2Fit Approved Training Courses. 2020. Available at https://www.fit2fit.org/fit2fit-approved-training-providers (accessed December 2020).
Dental Protection. Fit testing of masks - Dental Protection position statement. 2020. Available at https://www.dentalprotection.org/uk/articles/fit-testing-of-masks-dental-protection-position-statement (accessed December 2020).
Acknowledgements
All clinicians and patients appearing in the photographs have consented to do so. The authors are most grateful to them for their participation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Four of the five authors are dental professionals who are also officially accredited fit testers by the British Safety Industry Federation (BSIF). The other is a Senior Intensive Care Physician at one of the UK's leading COVID centres. All authors declare that they have no conflicts of interest in writing this article and have received no financial support for doing so.
Rights and permissions
About this article
Cite this article
Darwish, S., El-Boghdadly, K., Edney, C. et al. Respiratory protection in dentistry. Br Dent J 230, 207–214 (2021). https://doi.org/10.1038/s41415-021-2657-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-021-2657-0
This article is cited by
-
An evaluation of the impact of COVID-19 on the leadership behaviour of dental practice managers in England
BDJ Team (2022)
-
Respiratory protection clarification
British Dental Journal (2021)