Abstract
Introduction Minimally invasive dentistry has been promoted as the contemporary approach to the operative management of dental caries. Operative intervention should be undertaken on cavitated lesions which are actively progressing. However, there may be large variability in the restorative intervention thresholds and care plans of general dental practitioners (GDPs).
Aims To investigate restorative threshold and treatment decisions for occlusal and proximal carious lesions in a cohort of GDPs in London. To investigate potential differences based on number of years since graduation and attendance on a caries management course.
Materials and methods A previously used, validated caries questionnaire was distributed to foundation dentists, general practice dentists and practising educational supervisors in NHS London dental practices.
Results Two hundred and seventeen GDPs participated in the study. For occlusal lesions, nine (9.1%) newly-qualified dentists selected to intervene surgically on lesions confined to enamel, compared to 24 (29.8%) dentists who have been qualified for more than five years (p <0.05). In addition, a greater number of dentists who had attended a training course were more likely to do a minimally invasive preparation for a proximal lesion (38.2%), compared to 19.8% of those who had not (p <0.05). The majority of all participants (74.2%) chose to restore a proximal lesion using resin composite. Despite this material choice, 58.5% of those graduating within five years opted to prepare a traditional Black's class II cavity.
Conclusion A practitioner's restorative intervention threshold and their choice of treatment appears to be negatively affected by the number of years post-qualification, and positively influenced by attending a caries management course.
Similar content being viewed by others
Key points
-
Explores restorative intervention thresholds and treatment decisions of general dental practitioners working in London.
-
Investigates differences based on years since qualification and attendance on caries management courses.
-
Highlights the need for further training on contemporary caries management which may aid the restorative decisions of general dental practitioners.
Introduction
Minimally invasive dentistry has been promoted in the dental literature for the past 20 years as the modern approach to the management of dental caries.1 Dawson and Makinson first published work on minimally invasive dentistry in 1992.2 It involves conservative operative management of cavitated lesions.1 Successful implementation of minimally invasive operative caries management and the provision of the optimal adhesive restoration relies on a thorough understanding of the following factors: the histology of the dental substrate being treated, the chemistry/handling of adhesive materials and consideration of the practical operative techniques available to minimally remove caries, as well as the patient factors in maintaining the tooth-restoration complex.3
Deciding when to intervene operatively when practising minimally invasive dentistry is guided by the underlying tenet of maximal preservation of natural tooth structure. Further to this, the patient's caries risk and depth of the lesion are to be considered when deciding whether to treat using non-invasive techniques, such as topical fluoride, resin infiltration and fissure sealants, or minimally invasive restorative techniques.4,5 Operative intervention should be undertaken when the lesion is actively progressing, even with non-operative prevention regimes in place, and should involve selective carious tissue removal.1,6 For example in very deep lesions approximating to the pulp, selective carious tissue removal up to the leathery, scratchy and sticky affected dentine is recommended to avoid pulp exposure, leaving the retained carious tissue sealed in using an adhesive restoration.7 The evidence shows that caries underneath a technically well-placed adhesive restoration does not clinically or radiographically progress over at least 10 years, thus supporting the selective removal and sealing principle.4 However, it is important to remember that the enamel and dentine at the enamel-dentine junction must be clear from caries ideally to achieve an optimal bond and seal at the periphery of the restoration.
Prior to this, dentists' restorative decisions were guided purely surgically by Black's principles.8 This was the traditional approach whereby removing all carious tooth tissue was considered the gold standard.9 It also involved creating a predetermined cavity shape based on the physical and retentive properties of amalgam as the main restorative material.1
However, since the advent of adhesive restorative biomaterials and an increased knowledge and understanding of the caries process, clinical practice has changed favouring a minimum intervention approach to caries and patient management.4,10
There is large variability in restorative intervention thresholds and management of carious lesions by dentists.11 Potential influencing operator factors include the dentist's age, years of experience and educational background.12 Although the restorative intervention threshold of dentists has been studied in a range of countries,13,14,15,16,17 there is limited recent information about practitioners in the United Kingdom (UK). Therefore, the aim of this study was to investigate restorative intervention threshold decisions for occlusal and proximal carious lesions in a cohort of general dental practitioners in London. In addition, the restorative intervention thresholds were compared between recently graduated and more experienced dentists and separately, those dentists who had attended a postgraduate course on caries management and those who had not. The null hypothesis proposed that the restorative intervention threshold would not be influenced by years post qualification and continuing education in caries management.
Materials and methods
A validated caries restorative threshold questionnaire was used to enable clear comparisons between this and previous studies. The questionnaire was developed by Espelid et al.,13,14 and has been used in a number of other studies outside of the UK to investigate the restorative intervention thresholds of dentists.15,16,17
The questionnaire was distributed to foundation dentists, practice dentists and practising educational supervisors at educational conferences between February and October 2018, in England. Participants could either fill in a hard copy of the questionnaire or a web-based form. The study population included dentists in the London (North East, North Central, North West and South West) dental foundation training schemes. This comprised of 94 foundation dentists and 141 trainers. The survey was also distributed to an unknown number of associate dentists working at each of these trainer's practices.
The following demographics were collected as part of the questionnaire: age, sex, job role, years post-qualification, and if the participant had attended any courses in the discipline of cariology/caries management during the past 5 years.
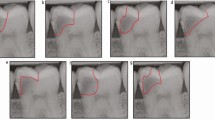
Participants were initially asked whether it was most important to restore all carious teeth (accepting the risk of some unnecessary restorations), most important not to restore sound teeth unnecessarily (accepting the risk of not restoring some carious lesions) or whether these risks of errors are of equal importance. All clinical questions were based on hypothetical carious lesions on a 20-year-old patient who visits the dentist annually, has good oral hygiene and uses a fluoride toothpaste. Participants were shown different radiographic stages and clinical photographs of proximal (Fig. 1) and occlusal (Fig. 2) carious lesion progression and asking participants when they would operatively intervene. Participants were then asked which type of preparation they would prefer to use and the restorative material they would choose for the smallest proximal lesions that they would restore.
Statistical analysis
The variables analysed were the subjective reporting of overall importance of whether it is more important to restore a carious lesion or not, restorative threshold intervention for proximal lesions, restorative threshold for occlusal lesions, preparations for each lesion and restorative material of choice for each lesion. Data was assessed according to years post qualification and whether or not they had attended a postgraduate caries management course. All data were initially assessed using descriptives and chi-squared tests. To investigate the characteristics of those who would treat a lesion confined to enamel, binary logistic regressions were performed using gender, years post-qualification, job role, importance to restore or not to restore and whether or not they had attended a postgraduate caries management course as the outcome variables. All analysis was performed in SPSS version 24 (IBM Corporation, Armonk, New York) and significance was inferred at p <0.05.
Results
Demographics
A total of 217 general dental practitioners participated in the study. The response rate was 84% and 44% for foundation dentists and trainers respectively. The year of graduation of participants ranged from 1976-2018. A total of 99 (45.6%) of these graduated <5 years ago, 53 (24.4%) dentists had graduated 15 years ago and 65 (30%) more than 15 years ago. One hundred and three participants were male (47.5%) and 114 were female (52.5%). Overall, 136 dentists (62.7%) had attended a course on caries management. Eight respondents had felt it was important to fill, 119 had reported it was important to not fill and 90 had reported they were of equal importance. The majority of dentists (n = 146, 67.3%) would treat lesions only when they had progressed to dentine whereas 71 participants (32.7%) would treat lesions confined to enamel. Of these, 59 participants would treat proximal lesions confined to enamel and 33 would treat occlusal lesions confined to enamel.
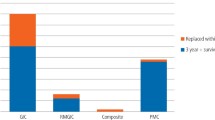
Descriptives reporting differences in restorative treatment depending on the number of years post- qualification are reported in Table 1. When assessing the preferred preparation type to restore proximal lesions, 49.8% of participants chose a traditional class II cavity preparation. This was compared to 31.3% who preferred saucer-shaped preparations and 18.9% preferring tunnel preparations. However, the year post-qualification and preferred preparation for proximal lesions was shown to be statistically significant (p <0.05), with more recently qualified dentists favouring traditional class II preparations. The majority of all participants (74.2%) chose resin composite to restore the proximal lesion with no statistically significant differences between the groups.
There were no differences in the year post-qualification and preferred preparation for occlusal lesions. However, a higher proportion of newly-qualified dentists favoured resin composite for restoring these lesions. When comparing the restorative intervention threshold of dentists for both proximal and occlusal lesions, the year of qualification was statistically significant for occlusal lesions only (p <0.05), with fewer newly-qualified dentists intervening on lesions confined to enamel.
Descriptives reporting differences in restorative treatment depending on whether they had done a postgraduate course on caries management in the last 5 years are reported in Table 2.
A greater proportion of those who had attended a course opted for a biologically-driven saucer preparation for a proximal cavity (38.2%), compared to 19.8% of those who had not and this was statistically significant (p = 0.001). A greater number of participants who had attended caries management courses also chose resin composite as their material of choice for occlusal restorations (p = 0.003). Attending a caries management course did not influence the restorative intervention threshold for both proximal and occlusal lesions (p >0.05).
In the multivariate analysis, those who were >15 years qualified were 4.65 times more likely to treat an occlusal carious lesion confined to enamel (OR 4.65 [95% CI 1.3316.24], p = 0.016). Those who placed importance on not restoring sound teeth were 88% less likely to treat an occlusal carious lesion confined to enamel (OR 0.12 [95% CI 0.020.63], p = 0.024) than those who deemed it more important to restore carious teeth. Interestingly, those who considered them to be of equal importance were also 80% less likely to treat an occlusal carious lesion confined to enamel (OR 0.20 [95% CI 0.430.91], p = 0.038). This is reported in Table 3.
Discussion
There were differences in the restorative intervention threshold between recently qualified dentists and more experienced dentists which was not attenuated by continuing postgraduate education in caries management courses, therefore the null hypothesis was rejected.
This study highlighted the lack of standardisation of restorative intervention thresholds that remain to this day, especially with occlusal lesions. More experienced dentists were likely to intervene sooner than more recently qualified dentists. This may be attributed to the lack of experience of recently qualified dentists or their desire to be as conservative as possible.
These findings are in line with other studies which have shown experience to be an important factor in restorative intervention thresholds.17 Unfortunately, there are limited studies investigating this and they tend to be relatively older. When comparing the restorative intervention threshold of occlusal lesions with other countries, French and Californian dentists tended to intervene at earlier stages in the caries process than the participants of this study. Literature suggests that the lack of financial remuneration for non-invasive approaches has influenced the early restorative intervention of French and Californian clinicians.16,18 However, with the increasing evidence showing the efficacy, benefits and cost-effectiveness of minimally invasive dentistry, there is increased training in dental schools.1,19,20 More up-to-date studies have shown that French dentists are now intervening at a later stage of progression.18 The non-invasive approach has now formed part of several best practice recommendations in France which may explain this trend.18
Despite the majority of participants in this study choosing to restore the proximal lesion with resin composite, they still opted to prepare a traditional class II cavity. This traditional preparation is unnecessarily more invasive if restoring with resin composite when compared to a more biologically-driven, saucer preparation guided primarily by the histology of the tissues and not the physical properties of the restorative material. The results highlighted that dentists who had attended caries management courses were more likely to opt for the less invasive biologically-driven, saucer-shaped preparation. This may indicate that there still may be some confusion about the need for material-specific cavity preparations amongst general dental practitioners. It was also found that more recently qualified dentists were opting for the traditional class II cavity. This may be explained by the fact that although outdated, Black's cavity preparation principles are still being taught, perhaps erroneously, in some dental schools. A classification described by Mount in 2009 categorised lesions by site and size,21 which is descriptive yet not prescriptive of specific cavity preparations, and may be a more relevant classification to use given modern materials, techniques and understanding. Although classifications for cavity preparations exist, cavity preparations should be guided biologically by the clinical presentation of carious dentine and the clinician's approach to carious tissue removal.22 In comparison to other countries, studies in France and Norway have shown the saucer shaped preparation to the be the preferred preparation for the majority of participants,9 whilst dentists in Kuwait and California preferred a traditional class II cavity.16
In terms of the preparation of occlusal carious lesions, this study found that the majority of participants preferred a less invasive, conservative approach, only opting to remove the carious tooth tissue. Kuwaiti and Californian surveys also found that participants favoured a more conservative occlusal preparation and more invasive proximal preparation.16 This study found that the occlusal preparation preferred by participants was not associated with the year since qualification or if the participant had attended a caries management course. In comparison, more experienced French dentists tended to over extend their occlusal cavity preparations.15
Resin composite was the preferred material for both proximal and occlusal carious lesions for the majority of participants. This was also found to be the preferred material choice of majority of French, Kuwaiti and Californian dentists.13,14,15,16,17 This is likely to be driven by its improved aesthetics and the more conservative, biologically-driven cavity preparation design of resin composite restorations, but may also be partly influenced more recently by the outcomes of the Minamata Convention and Treaty, phasing down the use of and disposal of mercury in the environment.23 The year since qualification was shown to be associated with the material of choice used to restore occlusal lesions with more experienced dentists favouring resin-modified glass-ionomer cement (RMGIC). This could be due to the reduced procedural time of RMGIC placement, coupled with time pressures faced by NHS general dental practitioners. In comparison, more experienced dentists in France preferred amalgam15 to restore occlusal lesions.
There are several limitations in this study that mean that its generalisability is limited. Firstly, only recently qualified dentists and dentists working in training practices with a focus on continuing education were assessed. Ninety-two percent of participants had read an article on caries management and 62% had attended a course on caries management. There may be selection bias and the answers given by the dentists who opted to participate in this study may be different to the dentists who did not participate in this study. This study investigated a London-based cohort which may or may not be generalisable to the general dental population. A further limitation of this study is that we are relying on the self-reporting of participants. It has been shown that there is little correlation between dentists stated restorative intervention thresholds and actual decisions in clinical practice.24 All scenarios used in the questionnaire were based on a 20-year-old patient who was a regular attender with good oral hygiene and therefore the results of this study only reflect the intervention thresholds and treatment decisions of this scenario. It has been reported in the literature that the restorative intervention threshold of dentists will change depending on the caries risk of the patient.16 Despite these limitations, several interesting findings were observed and the results may be of interest to both newly qualified dentists and dentists with >15 years' experience.
Conclusions
It is positive to see that the majority of participants would not treat enamel lesions with interventive dentistry. However, it is clear that there is still great variability of restorative intervention thresholds and treatment plans between general dental practitioners.
Irrespective of year of qualification and if the participant had attended a caries management course, further training and potential development of modern caries management guidelines may be beneficial to general practitioners. There is a need for further research on a larger scale throughout the UK to ascertain the restorative intervention threshold and treatment plans of general dental practitioners to guide standardisation.
References
Banerjee A. 'MI'opia or 20/20 vision? Br Dent J 2013; 214: 101-105. DOI: 10.1038/sj.bdj.2013.105.
Domejean S, Banerjee A, Featherstone J D B. Caries risk/ susceptibility assessment: its value in minimum intervention oral health care. Br Dent J 2017; 223: 191-197. DOI: 10.1038/sj.bdj.2017.665.
Banerjee A. Minimal intervention dentistry: part 7. Minimally invasive operative caries management: rationale and techniques. Br Dent J 2013; 214: 107-111. DOI: 10.1038/sj.bdj.2013.106.
Schwendicke F, Frencken J E, Bjørndal L et al. Managing carious lesions: Consensus recommendations on carious tissue removal. Adv Dent Res 2016; 28: 58-67. DOI: 10.1177/0022034516639271.
Banerjee A. 'Minimum intervention' - MI inspiring future oral healthcare? Br Dent J 2017; 223: 133-135. DOI: 10.1038/sj.bdj.2017.644.
Banerjee A, Frencken J E, Schwendicke F, Innes N P T. Contemporary operative caries management: consensus recommendations on minimal caries removal. Br Dent J 2017; 223: 215-222. DOI: 10/1038/sj.bdj.2017.672.
Banerjee A. Selective removal of carious dentine. In Scwendicke F, ed. Management of deep carious lesions. Switzerland: Springer International Publishing AG; 2018. pp. 55-70. DOI: 10/1007/9783319613703_5.
Black G. A work on operative dentistry: The technical procedures in filling teeth. Chicago: MedicoDental Publishing Company; 1908.
Domejean-Orliaguet S, Banerjee A, Gaucher C, Miletic I, Basson M RE. Minimum intervention treatment plan: a practical implementation in general dental practice. J Minim Interv Den. 2009; 2: 103-123.
Banerjee A, Domejean S. The contemporary approach to tooth preservation: minimum intervention caries management in general practice. Prim Dent J 2013; 2: 30-37.
Bader J D, Shugars D A. What do we know about how dentists make caries-related treatment decisions? Community Dent Oral Epidemiol 1997; 25: 97-103.
Kay E J, Locker D. Variations in restorative treatment decisions: an international comparison. Community Dent Oral Epidemiol 1996; 24: 376-379. DOI: 10.1111/j.1600-0528.1996.tb00882.x.
Espelid I, Tveit A B, Mejàre I, Sundberg H, Hallonsten A L. Restorative treatment decisions on occlusal caries in Scandinavia. Acta Odontol Scand 2001; 59: 21-27. DOI: 10.1080/000163501300035724.
Tveit A B, Espelid I, Skodje F. Restorative treatment decisions on approximal caries in Norway. Int Dent J 1999; 49: 165-172. DOI: 10.1002/j.1875-1595X.1999.tb00902.x.
Domejean-Orilaguet S, Tubert-Jeannin S, Riordan P J, Espelid I, Tveit A. French dentists' restorative treatment decisions. Oral Health Prev Dent 2004; 2: 125-131.
Rechmann P, Doméjean S, Rechmann B M T, Kinsel R, Featherstone J D B. Approximal and occlusal carious lesions. Restorative treatment decisions by California dentists. J Am Dent Assoc 2016; 147: 328-338. DOI: 10.1016/j.adaj.2015.10.006.
Khalaf M E, Alomari Q D, Ngo H, Doméjean S. Restorative treatment thresholds: Factors influencing the treatment thresholds and modalities of general dentists in Kuwait. Med Princ Pract 2014; 23: 357-362. DOI: 10.1159/000363184.
Domejean S, Leger S, Maltrait M, Espelid E, Tveit A B, Tubert-Jeannin S. Changes in Occlusal Caries Lesion Management in France from 2002 to 2012: A Persistent Gap between Evidence and Clinical Practice. Caries Res 2015; 49: 408-416.
Curtis B, Warren E, Pollicino C, Evans R W, Schwarz E, Sbarini A. The Monitor Practice Programme: is non-invasive management of dental caries in private practice cost-effective? Aust Dent J 2011; 56: 48-55. DOI: 10.1111/]j.1834-7819.2010.01286.x.
Schwendicke F, Paris S, Stolpe M. Cost-effectiveness of caries excavations in different risk groups - a micro-simulation study. BMC Oral Health 2014; 14: 153.
Mount G J. Minimal intervention dentistry: cavity classification & preparation. J Minimal Interv Dent 2009; 2: 150-162.
Innes N, Schwendicke F, Frencken J. An agreed terminology for carious tissue removal. Monogr Oral Sci 2018; 27: 155-161. DOI: 10.1159/000487842.
United Nations. What is the Minamata Convention on mercury?. 2018. Available online at http://ask.un.org/faq/192079 (accessed 13 March 2019).
Kay E J, Nuttall N M. Relationship between dentists'treatment attitudes and restorative decisions made on the basis of simulated bitewing radiographs. Community Dent Oral Epidemiol 1994; 22: 71-74. DOI: 10.1111/j.1600-0528.1994.tb01575.x.
Acknowledgements
The authors thank Dr Sophie Domejean for providing the questionnaire used in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chana, P., Orlans, M., O’Toole, S. et al. Restorative intervention thresholds and treatment decisions of general dental practitioners in London. Br Dent J 227, 727–732 (2019). https://doi.org/10.1038/s41415-019-0849-7
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0849-7
This article is cited by
-
General dental practice and improved oral health: is there a win-win for both the professional establishment and government?
British Dental Journal (2020)
-
Minimum intervention oral healthcare delivery - is there consensus?
British Dental Journal (2020)