Abstract
Bleaching has changed the way the world looks at teeth, with lighter teeth becoming the norm due to the ease and simplicity of tray bleaching. The resultant lighter teeth have changed prosthodontics in that there is less need for some types of restoration, less aggressive preparation design, as well as new techniques for shade selection, caries control and managing gingival health.
Similar content being viewed by others
Key points
-
Provides an updated review of tray bleaching.
-
Demonstrates changes in prosthodontic treatment due to the impact of bleaching.
-
Introduces relatively new techniques for single dark teeth, caries control, and improving gingival health with carbamide peroxide.
Introduction
Approximately 30 years ago, bleaching became more readily available to patients, by almost all dentists, through the introduction of tray bleaching with 10% carbamide peroxide (CP).1 Since that time, many variations on the process have been introduced and there has also been a resurgence in the older in-office bleaching techniques.2 Due to the ever increasing popularity of bleaching and the resultant changed smile for patients, many 'over-the-counter' products have also been introduced, as well as different products proposed for bleaching. However, the most cost-efficient, safest and most easily used technique which works very well in many different situations has remained the tray bleaching technique with 10% carbamide peroxide (Figs 1 and 2).
Many areas of the tray technique have been researched and explored. Carbamide peroxide has been found to penetrate intact enamel and travel through the dentine to the pulp in 5-15 minutes.3 The colour of the tooth is found primarily in the dentine, and the dentine is changed by bleaching.4 This easy passage of peroxide also accounts for the sensitivity some patients experience.5 Teeth darkened by age or genetically discoloured generally take from three nights to six weeks of nightly treatment to be bleached to their maximum lightest colour. However, not every patient will achieve the same endpoint; teeth vary in their response to bleaching, both in how fast they change colour as well as the final outcome of the colour change. Teeth stained by nicotine may take one to three months of overnight treatment (Figs 3 and 4), while teeth discoloured by tetracycline ingestion can take from two to six months of nightly treatment (Figs 5 and 6).6 Higher concentrations of CP have more side effects, and once the rate of change of the tooth has been reached the additional percentages merely contribute to tooth sensitivity and gingival irritation.7
Tray design has varied from the original non-scalloped no-reservoir design, which works well for 10% CP, to scalloped trays with reservoirs for higher concentrations. Ten percent CP is made to go on to tissue and gingival health improves during bleaching; however, higher concentrations will tend to burn the tissue causing sensitivity, so a different tray design is used. Sensitivity to the teeth is related to the easy passage of the peroxide to the pulp, creating a reversible pulpitis. The higher the concentration, the greater the sensitivity. This sensitivity is best treated with potassium nitrate (PN), which also penetrates enamel and dentine in approximately 30 minutes.8 The PN can be included in the bleaching material, used independently before and after bleaching or applied in a toothpaste.
Not only has the increased popularity and use of tray bleaching impacted patients, it has also impacted other dental treatments as well. One area that has been affected is prosthodontics. Some of the changes in prosthodontic treatment from the impact of bleaching are described as follows.
Bleaching avoids unnecessary veneers or crowns when only a colour change of the teeth is needed
A uniform colour of all the visible teeth is generally more aesthetically pleasing than having some teeth darker than other teeth. Generally, the maxillary incisors are the same colour and match the colour of the first premolar, with the canine being at most a half shade darker. When the canine is significantly darker by several shades than the premolar and lateral incisor it detracts from a natural smile. Bleaching such that the canine more closely matches the adjacent teeth provides a more natural smile. Bleaching the canines also demonstrates that bleaching is changing the genetic colour of the tooth by changing the dentine (Figs 7 and 8).
The first case of bleaching reported in the literature was to avoid preparing six anterior teeth for porcelain veneers when the teeth only needed a colour change. With the advent of bleaching, much tooth structure has been saved from preparations to improve colour. Veneers are indicated for form or function as well as certain aesthetic situations, but a simple colour change of a tooth should first be addressed with bleaching. Since enamel is designed to last a lifetime and all restorative materials have some finite life, the more tooth structure that is retained by conservative bleaching the more long-lasting the teeth will be (Figs 9 and 10).
A successful restoration will demonstrate an ability to perform as expected over a certain observation period. Systematic reviews showed an estimated five-year survival rate of 94.4% for conventional tooth-supported FDPs,9 93.3% for all ceramic single crowns and 95.6% for metal-ceramic single crowns.10 Furthermore, a 12-year retrospective study showed survival rate of 94.4% for laminate veneers.11 On the other hand, maintaining tooth structure is fundamental in the choice a restoring dentist would consider when addressing the patient's aesthetic concerns. In a study to measure the amount of tooth structure removed for metal-ceramic crowns and traditional veneers,12 the authors found the preparation removed up to 72.1% of the coronal tooth structure to receive a metal-ceramic crown and 16.6% for a veneer. The patient can always proceed to the more aggressive preparations if needed, but never can go back, so the first treatment of choice should be bleaching.
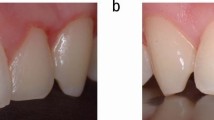
Bleaching will harmonise tooth colour before the restoration of an adjacent tooth with a crown
When porcelain veneer or composite resin restorations are indicated over discolorations or mismatched teeth, the restorative will mimic the natural tooth structure better if the underlying tooth is as light as possible. Bleaching before placing restorations provides a simpler colour matching option. For porcelain veneers, a thickness of 0.3 mm is required for each shade change, so bleaching will allow for a lighter substrate and less removal of enamel to alter the colour.13 Also, when a single tooth needs to be crowned, it is best to bleach the adjacent teeth first to provide the best outcome for the shade match of the crown (Figs 11 and 12).
It is not necessary to crown a single dark anterior tooth that has received endodontic therapy, so it can be bleached
One of the major shifts in dental treatment is the determination that anterior endodontically treated teeth no longer need a crown because of endodontic treatment. While posterior teeth that have received endodontic therapy should have a crown to avoid fracture, the anterior teeth survive just as long without a crown as with a crown. In a retrospective study14 which looked into the survival rate of 1,273 endodontically treated teeth (range 1-25 years), it was significantly evident that endodontically treated posterior teeth should receive full coverage crowns but this is not necessary for anterior teeth with enough dentine support or relatively sound anterior teeth.15 The reasons are related to occlusion, anatomy and position in the mouth. The posterior teeth have occlusal forces three times that of anterior teeth, and are directed down the long axis of multi-rooted teeth, so they are prone to fracture or split. The anterior teeth have single roots, with occlusal forces one third that of posterior teeth and directed laterally. What determines the success or fracture of an anterior tooth is the amount of remaining dentine. If the tooth is reduced for an aesthetic crown in addition to the endodontic therapy, the tooth is significantly more weakened than not providing a crown, so it is better to bleach than to crown, unless the tooth needs a crown regardless of the endodontic therapy. Anterior teeth now differ from posterior teeth concerning the need for prosthodontic treatment, with more internal and external bleaching indicated rather than crowns (Figs 13 and 14).
A single dark tooth which has not received a root canal does not need endodontic therapy in order to bleach it
A single dark tooth that does not need a root canal, as in the case of calcific metamorphosis, can be bleached from the 'outside-in' using a single-tooth bleaching tray.16 Since the peroxide passes through intact enamel and dentine to the pulp in 5-15 minutes, there is no need to create a pulp chamber or perform endodontic therapy to obtain access to the inside of the tooth. The tooth can be bleached just as easily from the 'outside-in' as from the 'inside-out'. The bleaching technique for the tray fabrication is similar to a full tray but a special 'single-tooth' tray is fabricated that only allows the bleaching material to contact the single dark tooth without changing the colour of the adjacent teeth. The tray design would extend onto tissue and require a low 10% concentration of carbamide peroxide. If the dark tooth does not lighten sufficiently to match the adjacent teeth, the adjacent teeth would not be bleached. If the dark tooth bleaches lighter than the adjacent teeth, then a conventional tray can be used to slowly titrate the colour of the adjacent teeth to match the single dark tooth (Figs 15 and 16).
Bleaching will restore teeth darkened by age that were originally matched to adjacent PFM crowns to the original shade to match the crowns
One aesthetic challenge is that over time the teeth will darken, both from ageing as well as diet and lifestyle habits. Smoking, coffee, wine and other food stuffs, alongside the deposition of more yellow secondary dentine, will darken teeth. Ceramic crowns, teeth or plastic teeth on a removable partial denture will not change colour, so eventually there is a mismatch in the shade of the prosthesis from the original colour of the tooth. With bleaching, the adjacent natural teeth can be re-lightened to the original shade of the crowns. This is especially helpful if the teeth were originally bleached before the crown or removable partial denture (RPD) shade selection, because the endpoint for bleaching is known. Even if the teeth were not bleached originally, bleaching the darkened teeth will still be a benefit. Care must be taken to titrate the bleaching process back to the unbleached shade. Occasionally, the potential for having overall lighter teeth will prompt a patient to bleach to the maximum lightening, then replace the now darker appearing crown (Figs 17, 18, 19, 20).
Bleaching can lighten teeth under veneers if the existing shade of the veneer is too dark, which may avoid replacing the veneers
One of the goals of a porcelain veneer is to have the 'life-like' translucency of the natural tooth. This means there is a certain amount of transparency in the veneer to avoid a 'dead' look. The problem when the original tooth colour is dark is that discoloration is transmitted through the veneers to make the veneers darker. If the veneers were placed over dark teeth, then the teeth can be bleached from the lingual, with the tray application of 10% carbamide peroxide.17 Bleaching will not have an effect on the ceramic veneer nor on the resin cement, but as the tooth lightens the veneer will appear to lighten, providing a more aesthetic outcome (Figs 21 and 22). Should the teeth relapse over time, they can be re-bleached from the lingual to the original shade making the veneers the original shade.
Bleaching can provide a supplement to good oral hygiene and supportive periodontal care in maintaining gingival health, avoiding root caries and stopping recurrent decay at the crown margins, especially in a full-mouth restoration patient
Often an indication for a full-mouth reconstruction with crowns and fixed partial dentures is the extensive decay a patient may have experienced over their lifetime. However, their tendency to get decay, as well as the advancing age and resultant medications causing dry mouth, can result in recurrent decay at the margins of otherwise excellent restorations. Dentine and cementum are more susceptible to decay than enamel, with dentine dissolving at pH 6.8 and enamel dissolving at pH 5.5. In order to maintain a full-mouth reconstruction, a bleaching tray with 10% carbamide peroxide can be used every night to elevate the pH above which tooth decay can occur in dentine or enamel, reduce the plaque from the teeth, and kill some of the bacteria that cause decay.18,19,20,21,22,23,24,25,26,27 The application of peroxide gel through a tray as an adjunct to scaling and root planning during periodontal follow-up appointments significantly reduced bleeding on probing for 66 refractory patients.28
Carbamide peroxide can be considered an effective and affordable alternative to topical antibiotic application in periodontal refractory cases, in patients with good oral hygiene who maintain regular recalls of professional periodontal care. It is for this reason that an oxidising gel of 1.7% hydrogen peroxide (Perio Gel, QNT Anderson, Bismarck, ND) was developed to be delivered intraorally using a closed tray. In a randomised clinical trial for six months, Putt and Proskin found clinical improvement in pocket depth reduction and bleeding index when a 1.7% hydrogen peroxide gel was used with scaling and root planning comparing to SRP alone.29 There is no impact on the prosthesis or cements, and there is an improvement on the gingival health as well, since 10% carbamide peroxide was originally used as an oral antiseptic for wound healing. In all the bleaching research that evaluated gingival health as well as tooth colour change, there is improvement during bleaching. However, it is necessary to stress the importance of meticulous oral hygiene and maintaining regular recalls, as this will be the only way to ensure plaque removal and the detection of gingival/periodontal deterioration.
Bleaching will irrigate and clean tissue around implants to avoid peri-implantitis
Longitudinal studies of 22 years show implant survival rates from 87%-99.2%.30 This high percentage of survival dose not hide the high percentage of peri-implant mucositis (43%) (Fig. 23) and peri-implantitis (22%) (Fig. 24) in a recent meta-analysis.31 There is strong evidence supporting the idea that regular recalls for periodontal supportive therapy will reduce the chance of developing peri-implantitis.32 Recalls are particularly important in patients with a history of treated aggressive periodontitis, due to the high susceptibility of this patient's category to develop periodontal and peri-implant diseases.33
Ten percent carbamide peroxide has a long history of use as an oral antiseptic to improve gingival health.34 When the implant-surrounding soft tissues develop an inflammatory lesion due to plaque accumulation, an early non-surgical intervention is important to avoid the progression of the disease into the supportive bone. In addition to the regular non-surgical methods of scaling and polishing, systemic and local antibiotics, and air-powder jets, the clinician can utilise the additional benefit of using tray application of carbamide peroxide 10% as it has been proven that teeth whitening improves gingival health.35 Curtis et al. found a reduction in plaque index when carbamide peroxide was compared with a placebo gel.36 This could be explained by the bacterial (Streptococcus mutans and Lactobacilli) inhibitory effect of 10% carbamide peroxide when applied for two hours.37 More longitudinal randomised clinical trials are necessary to prove the additional benefit of using carbamide peroxide, along with good oral hygiene.
Bleaching can disinfect exposed titanium surfaces to treat peri-implantitis
Hydrogen peroxide (HP) as an oxidising agent is considered as one of the implant surface detoxification agents.38 When used for subgingival irrigation, HP was efficient in suppressing the growth of Actinomyces actinomycetemcomitans (AA).39 The impact of 10% hydrogen peroxide in conjunction with antibiotics was studied to clean implant surfaces under flap procedure,40 the study showed a 58% drop in gingival bleeding for five years following-up (Fig. 25).
Bleaching teeth before veneering or crowning will allow the use of more translucent aesthetic materials instead of opaque materials in discoloured teeth
All-ceramic restorations provide a wide range of value and translucency, more than porcelain fused to metal (PFM) restorations.41 This ability gives all-ceramic restorations the ability to mimic natural teeth. However, different ceramic systems provide various degrees of translucencies.42 Glass ceramics are more translucent than the strong and opaque polycrystalline ceramics (alumina- and zirconia-based restorations). This feature makes glass ceramics (such as lithium disilicate and feldspathic glass) a preferred choice when restoring anterior teeth. To understand the effect of tooth shade on the final aesthetics of the dental restoration, we can refer to the importance of communicating the stump shade of the prepared tooth to the lab technician, since the stump shade may affect the chroma and value of the produced restoration if a translucent material is used.43 This phenomenon could be adjusted by bleaching the teeth which will be restored, which will increase the value and reduce the chroma of the teeth, allowing the use of the highly aesthetic glass-ceramic restorations instead of trying to mask the colour of dark teeth with opaque systems like metal-ceramics and polycrystalline ceramics (Fig. 26).
With the advent of bleaching, we no longer are required to teach chairside 'stain and glaze' to match cracks and older teeth in the dental school curriculum
Traditional prosthodontic teaching involves staining and glazing porcelain fused to metal crowns to match aged or disfigured teeth. Chairside staining is a tedious process which has been made more difficult with the infection control procedures needed in clinic. Now a more reasonable approach would be to bleach first to minimise defects, then provide a lighter crown without the aging effects.
Because of bleaching, ceramic shade choices for porcelain materials and denture teeth are now lighter than B1 (Vita classic shade guide)
Hands and teeth tend to reveal a person's age, so an adult may look ten years younger with lighter teeth. The influence of television and movies on the world is to create a desire for lighter teeth; since those people with lighter teeth are perceived to be more intelligent, attractive and fun to be around.44
With the population having lighter teeth worldwide, there is not as much demand for the darker A4-type shades in ceramics or in denture teeth. Patients desire lighter teeth, so the companies have begun to produce shade tabs and porcelains as well as denture teeth lighter than B1 for many people's desires (Figs 27 and 28). This may also result in the need to bleach natural teeth to match the lighter denture tooth shades (Figs 29 and 30).
Because of lighter teeth from bleaching and more translucent all ceramic crowns, fibre posts are replacing metal posts
Teeth that require restorations after bleaching will require a lighter shade ceramic. Also, teeth that are bleached retain their natural translucency and vitality, so more translucent ceramic shades and materials are being used for anterior teeth. As all ceramic restorations are becoming more popular and able to replicate the translucency of teeth, there is the possibility of the colour of the preparation or post/core showing through to alter the colour of the crown. In order to minimise the show through of metal posts under all-ceramic crowns, more fibre posts are being used. The main advantage of a fibre post over a metal post is the aesthetics as well as the avoidance of any dark metal altering the shade of the translucent ceramic restoration.
Utilise tray bleaching as a diagnostic shade tool before major oral reconstructions
In aesthetically demanding cases where the patient is not clear about the final tooth shade desired, tray bleaching could be utilised as a conservative diagnostic tool to bleach the natural teeth to the desired tooth shade before initiating the rehabilitation. This bleaching approach will be more reliable than using mock-ups with PMMA or BIS-GMA, as these materials has different shade values than the definitive ceramic prosthesis. Also, if the patient is in a PMMA provisional restoration during bleaching, the PMMA may turn yellow.45
Bleaching materials will remove chlorhexidine staining around provisional restorations before cementation of crowns
The use of newer bis-acryl provisional materials, especially when used for porcelain veneer provisional restoration, can result in occasional leakage at the margins. If the patient was using chlorohexidine to improve tissue health, further staining can occur. Using a cotton swap with 10% carbamide peroxide to clean the preparation before cementation of veneers or crowns has been show to easily clean without damaging tissue and without compromising bond strengths of the resin cements (Figs 31 and 32).46
A word of caution about bleaching
In spite of the benefits of bleaching and the impact on conventional prosthodontics, there is at least one contraindication to bleaching involving prosthodontics. When older patients already have crowns in place that match their adjacent discoloured teeth, they may be interested in bleaching to look younger. Since no prosthetic material changes colour from bleaching, the process would cause a mismatch of the older crown with the now whiter teeth, indicating a new crown needed for aesthetic balance. This would also occur if the bleaching material was used for caries control around existing crowns.47 The need for new crowns incurs much expense. Even if the patient has the finances to replace all their crowns to a lighter shade, sometimes the removal of an old crown that was on a cracked tooth or had a post may jeopardise the success of the new crown. Generally, patients with extensive fixed prosthetics, especially on cracked or compromised teeth, are not good candidates for bleaching. When they need a replacement crown, the darker shades would be required to avoid replacing all their crowns.
Conclusions
Bleaching has changed the way the world looks at teeth, with lighter teeth becoming the norm due to the ease and simplicity of tray bleaching. The resultant lighter teeth have changed prosthodontics in that there is less need for some types of restoration, less aggressive preparation design, as well as new techniques for shade selection, caries control and managing gingival health.
References
Haywood V B, Heymann H O. Nightguard vital bleaching. Quintessence Int 1989; 20: 173-176.
Haywood V B, Sword R J. Bleaching Tetracycline-Stained Teeth. 2018. Available at https://www.aegisdentalnetwork.com/id/2018/01/bleaching-tetracycline--stained-teeth (accessed April 2019).
Cooper J S, Bokmeyer T J, Bowles W H. Penetration of the pulp chamber by carbamide peroxide bleaching agents. J Endod 1992; 18: 315-317.
McCaslin A J, Haywood V B, Potter B J, Dickinson G L, Russell C M. Assessing dentin color changes from nightguard vital bleaching. J Am Dent Assoc 1999; 130: 1485-1490.
Pashley D H, Tay F R, Haywood V B, Collins M A, Drisko C L. Consensus-based recommendations for the diagnosis and management of dentin hypersensitivity. Compend Contin Educ Dent 2008; 29 (Spec Iss): 1-35.
Haywood V B. The "Bottom Line" on Bleaching 2008. Inside Dentistry 2008; 4: 82-89.
Matis B A. Tray whitening: what the evidence shows. Compend Contin Educ Dent 2003; 24: 354-362.
Kwon S R, Dawson D V, Wertz P W. Time Course of Potassium Nitrate Penetration into the Pulp Cavity and the Effect of Penetration Levels on Tooth Whitening Efficacy. J Esthet Restor Dent 2016; 28 (Spec Iss): S14-S22.
Pjetursson B E, Sailer I, Makarov N A, Zwahlen M, Thoma D S. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part II: Multiple-unit FDPs. Dent Mater 2015; 31: 624-639.
Pjetursson B E, Sailer I, Zwahlen M, Hammerle C H. A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part I: single crowns. Clin Oral Implants Res 2007; 18 (Spec Iss): 73-85.
Fradeani, M, Rooedemagni, M, and Corrado M. Porcelain laminate veneers: 6to 12-year clinical evaluation-a retrospective study. Int J Periodontics Restorative Dent. 2005; 25: 9-17.
Edelhoff D, Sorenson J A. Tooth structure removal associated with various preparation designs for anterior teeth. J Prosthet Dent 2002; 87: 503-509.
McLaren E A. Porcelain Veneer Preparations: To Prep or Not to Prep. 2006. Available at https://www.aegisdentalnetwork.com/id/2006/05/lab-talk-porcelain-veneer-preparations-to-prep-or-not-to-prep (accessed April 2019).
Sorensen.J A, Martinoff J T. Intracoronal reinforcement and coronal coverage: a study of endodontically treated teeth. J Prosthet Dent 1984; 51: 780-784.
Goodacre C J, Spolnik K J. The prosthodontic management of endodontically treated teeth: a literature review. Part III. Tooth preparation considerations. J Prosthodont 1995; 4: 122-128.
Haywood V B, DiAngelis A J. Bleaching the Single Dark Tooth. Inside Dentistry 2010; 6: 42-52.
Haywood V B, Parker M H. Nightguard vital bleaching beneath existing porcelain veneers: a case report. Quintessence Int 1999; 30: 743-747.
Shapiro W B, Kaslick R S, Chasens A l, Eisenberg R. The influence of urea peroxide gel on plaque, calculus and chronic gingival inflammation. J Periodontol 1973; 44: 636-639.
Reddy J, Salkin L M. The effect of a urea peroxide rinse on dental plaque and gingivitis. J Periodontol 1976; 47: 607-610.
Zinner D D, Duany L F, Chilton N W. Controlled study of the clinical effectiveness of a new oxygen gel on plaque, oral debris and gingival inflammation. Pharmacol Ther Dent 1970; 1: 7-15.
Shipman B, Cohen E, Kaslick R S. The effect of a urea peroxide gel on plaque deposits and gingival status. J Periodontol 1971; 42: 283-285.
Gomes D C, Shakun M L, Ripa L W. Effect of rinsing with a 1.5 percent hydrogen peroxide solution (Peroxyl) on gingivitis and plaque in handicapped and nonhandicapped subjects. Clin Prev Dent 1984; 6: 21-25.
Kleinberg I. Effect of urea concentration on human plaque pH levels in situ. Arch Oral Biol 1967; 12: 1475-1484.
Firestone A R, Schmid R, Mühlemann H R. Effect of topical application of urea peroxide on caries incidence and plaque accumulation in rats. Caries Res 1982; 16: 112-117.
Zinner D D, Duany L F, Llorente M. Effects of urea peroxide in anhydrous glycerol on gingivitis and dental plaque. J Prev Dent 1978; 5: 38-40.
Tartakow D J, Smith R S, Spinelli J A. Urea Peroxide solution in the treatment of gingivitis in orthodontics. Am J Orthod 1978; 73: 560-563.
dos Santos Medeiros M C, de Lima K C. Effectiveness of nightguard vital bleaching with 10% carbamide peroxidea clinical study. J Can Dent Assoc 2008; 74: 163e.
Cochrane R B, Sindelar B. Case Series Report of 66 Refractory Maintenance Patients Evaluating the Effectiveness of Topical Oxidizing Agents. J Clin Dent 2015; 26: 109-114.
Putt M S, Proskin H M. Custom tray application of peroxide gel as an adjunct to scaling and root planing in the treatment of periodontitis: a randomized, controlled three-month clinical trial. J Clin Dent 2012; 23: 48-56.
Coli P, Christiaens V, Sennerby L, Bruyn H. Reliability of periodontal diagnostic tools for monitoring peri-implant health and disease. Periodontol 2000 2017; 73: 203-217.
Derks, J, Tomasi C. Peri-implant Health and Disease. A systematic review of current epidemiology. J Clin Periodontol 2015; 42 (Spec Iss): S158-S171.
Costa F O, Takenaka-Martinez S, Cota L O, Ferreira S D, Silva G L, Costa J E. Peri-implant disease in subjects with and without preventive maintenance: a 5year follow-up. J Clin Periodontol 2012; 39: 173-181.
Jepsen S, Berglundh T, Genco R et al. Primary prevention of peri-implantitis: managing peri-implant mucositis. J Clin Periodontol 2015; 42 (Spec Iss): S152-S157.
Lazarchik D A, Haywood V B. Use of tray-applied 10 percent carbamide peroxide gels for improving oral health in patients with special-care needs. J Am Dent Assoc 2010; 141: 639-646.
Reinhardt J W, Eivins S C, Swift E J, Denehy G E. A clinical study of nightguard vital bleaching. Quintessence Int 1993; 24: 379-384.
Curtis J W, Dickinson G L, Downey M C et al. Assessing the effects of 10 percent carbamide peroxide on oral soft tissues. J Am Dent Assoc 1996; 127: 1218-1223.
Bentley C D, Leonard R H, Crawford J J. Effect of whitening agents containing carbamide peroxide on carcinogenic bacteria. J Esthet Dent 2000; 12: 33-37.
Suarez F, Monje A, Galindo-Moreno P, Wang H L. Implant surface detoxi cation: a comprehensive review. Implant Dent 2013; 22: 465-473.
Quirynen M, Teughels W, De Soete M, van Steenberghe D. Topical antiseptics and antibiotics in the initial therapy of chronic adult periodontitis: microbiological aspects. Periodontol 2000 2002; 28: 72-90.
Leonhardt A, Dahlén G, Renvert S. Five-year clinical, microbiological, and radiological outcome following treatment of peri-implantitis in man. J Periodontol 2003; 74: 1415-1422.
Kelly J R. Dental ceramics: what is this stuff anyway? J Am Dent Assoc 2008; 139 (Spec Iss): 4S-7S.
Barizon K T, Bergeron C, Vargas M A et al. Ceramic materials for porcelain veneers: part II. Effect of material, shade, and thickness on translucency. J Prosthet Dent 2014; 112: 864-870.
Chu S J. Clinical steps to predictable colour management in aesthetic restorative dentistry. Dent Clin North Am 2007; 51: 473-485.
Khalid A, Quinonez C. Straight, white teeth as a social prerogative. Sociol Health Illn 2015; 37: 782-796.
Robinson F G, Haywood V B, Myers M. Effect of 10 percent carbamide peroxide on colour of provisional restoration materials. J Am Dent Assoc 1997; 128: 727-731.
Cooper J R 3rd, Young N B, Haywood V B, Mettenburg D, Callan R S, Rueggeberg F A. Effect of Short-Duration, Localized Carbamide Peroxide Application to Remove Enamel Staining on Bond Strength of Resin Cement to Enamel. J Esthet Restor Dent 2016; 28: 190-196.
Haywood V B. Bleaching and caries control in elderly patients. 2009. Available at https://www.dentistry.co.uk/2009/02/19/bleaching-and-caries-control-elderly-patients/ (accessed April 2019).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haywood, V., Al Farawati, F. Bleaching update and the future impact on prosthodontics. Br Dent J 226, 753–760 (2019). https://doi.org/10.1038/s41415-019-0314-7
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0314-7