Abstract
Aplastic anemia (AA) is the prototypical bone marrow failure syndrome. In the current era of readily available ‘molecular annotation’, application of comprehensive next-generation sequencing panels has generated novel insights into underlying pathogenetic mechanisms, potentially leading to improvements in personalized therapeutic approaches. New evidence has emerged as to the role of somatic loss of HLA class I allele expression in ‘immune-mediated’ AA, associated molecular aberrations, and risk of clonal evolution. A deeper understanding has emerged regarding the role of ‘myeloid’ gene mutations in this context, translating patho-mechanistic insights derived from wider clinical and translational research within the myeloid disorder arena. Here, we review contemporary ‘tools’ which aid in confirmation of a diagnosis of AA, with an additional focus on their potential in guiding therapeutic options. A specific emphasis is placed upon interpretation and integration of this detailed diagnostic information and how this may inform optimal transplantation strategies.
Similar content being viewed by others
Introduction: definition and epidemiology
Aplastic anemia (AA) is an acquired bone marrow failure disorder characterized by autoimmune-mediated destruction of hematopoietic stem and progenitor cells (HSPCs) [1]. The annual incidence of the disease in Europe is estimated at 3 cases/million and it affects both genders equally, rising to 7 cases/million in rural areas of Southeast Asia with a slight predominance amongst younger males [2]. Due to potential phenotypic overlap with inherited bone marrow failure syndromes (IBMFS), in particular those lacking a family history or evidence of classical congenital anomalies, the incidence of the disease may be estimated as higher during childhood due to difficulties in accurately distinguishing between the two groups. In adult patients, two peaks of incidence are reported: the first between 20 and 25 years, perhaps also encompassing a significant proportion of IBMFS with late onset and low disease expressivity, and the second after 60 years of age [3].
AA is a so-called diagnosis of exclusion and in over 70% of cases it is defined as “immune/idiopathic” in nature [4]. The pathogenetic mechanisms underlying disease development include several immunological processes including initial autoimmune destruction of HSPCs mediated by T cytotoxic lymphocytes, via the recognition of unknown human leukocyte antigen (HLA)-restricted peptides, leading to oligoclonal hematopoiesis promoted by selective advantage (Fig. 1) [5]. The latter may include on one hand the expansion of ‘immunologically privileged’ clones such as those harboring PIGA mutations, responsible for the development of paroxysmal nocturnal hemoglobinuria (PNH), or HLA aberrations. On the other hand, clonal selection of cells with skewed myeloid proliferative potential, characterized by aberrations in leukemic drivers e.g., splicing factors, may also underpin mechanisms of selective advantage [1, 5, 6].
Typically, a suspected diagnosis of AA is confirmed by bone marrow (BM) trephine biopsy, which is noted to be severely hypocellular (<25% or <50% if 30% of BM is represented by hematopoietic cells) with an absence of blasts and no evidence of fibrosis [7]. Clinical presentation frequently manifests as trilineage cytopenia following the immunological ‘attack’ of HSPCs via CD8 + T lymphocytes, and the subsequent risk of infectious and hemorrhagic complications is the major determinant of a mortality rate greater than 70% in the most severe forms, if left untreated [7].
According to the modified Camitta’s Criteria, severe AA (SAA) is defined when at least two laboratory alterations are present, including an absolute neutrophil count (ANC) < 500/mm3, platelet count <20,000/mm3 or reticulocyte count <20,000/mm3, while very severe AA (vSAA) is characterized by an ANC < 200/mm3 [8]. Correct classification is essential in guiding the treatment modality of choice, especially in deciding which patients should be considered for allogeneic hematopoietic cell transplantation (allo-HCT), and indeed when.
Therefore, an appropriate diagnostic framework is crucial not only for the differential diagnosis between acquired AA, IBMFS, and other cytopenic states such as myelodysplastic syndromes (MDS), but also to estimate the risk of clonal evolution, which is considerably higher than that of the general population [6, 9]. All these features represent essential elements for the discrimination between immune mediated AA vs other possible etiologies, including IBMFS or hypoplastic MDS (hMDS), and hence drive appropriate transplant or non-transplant treatment strategies [10].
Differential diagnosis and the identification of inherited bone marrow failure syndromes
The onset of the disease is often insidious and frequently represents a clinical challenge requiring an accurate and timely clinical and laboratory workup to facilitate appropriate treatment and limit life-threatening complications.
At the onset of the clinical picture, a detailed medical and family history is essential to exclude, as much as is feasible, the possibility of an inherited IBMFS within the family. Secondary and transitory forms of AA must also be excluded. Generally, these arise secondary to significant hematinic deficiencies, exposure to myelotoxic drugs, viral infections (in particular hepatitis C virus (HCV)), concomitant autoimmune diseases and certain solid organ or hematological neoplasms. Obtaining a detailed personal and family history plays a crucial role, in particular for pediatric and adolescent/ young adult (AYA) patients, to exclude the presence of long-standing cytopenia and potential of other affected family members. If an IBMFS is suspected, the medical history and examination should evaluate for the presence of recurrent infections, developmental anomalies and anatomical or tissue alterations characteristic of specific IBMFS (Table 1) [11].
Conventional karyotyping and fluorescence in situ hybridization (FISH) analysis from BM aspirates or occasionally peripheral blood (PB) facilitates detection of cytogenetic alterations, important for aiding the differential diagnosis with hMDS. However, cytogenetic alterations can also occur in AA patients, particularly deletion (del)13q, trisomy 8, and loss of heterozygosity of 6p. Notably, in pediatric/AYA patients the presence of chromosome 7 anomalies should trigger particularly close review to exclude concomitant MDS and constitutional syndromes, even if consistent phenotypes are absent. Conversely, identification of small PNH clones frequently supports the diagnosis of immune-mediated AA and sequential monitoring is essential to promptly detect secondary PNH evolution and hence limit risks of thrombotic complications [12, 13]. In all pediatric cases, genetic screening is crucial for accurate diagnostic classification, even when cytogenetic or molecular alterations characteristic of a specific disorder and/or small PNH clones are present. It is noteworthy that in young adults (≤40 years), IBMFS represent up to 15% of all AA cases, therefore this possibility must be excluded by specific tests according to both clinical suspicion and individual phenotype. (Table 1) If IBMFS is suspected, the only curative approach is an allo-HCT, with judicious selection of donors (inheritance of the disease and familial segregation) and dedicated (generally toxicity-sparing) conditioning regimens [14,15,16].
Extended molecular profiling (Next-Generation Sequencing, NGS) offers the possibility of identifying specific or common alterations that may be detected across the spectrum of AA, IBMFS as well as in myeloid neoplasia, and for this reason this analysis may be helpful to support the diagnosis [17]. Use of specific extended panels containing genes implicated in IBMFS pathogenesis coupled with telomere length assessment can help in identification of germline syndromes [18]. It is of utmost importance to confirm the presence of a germline variant in an appropriate source of DNA not contaminated by myeloid-derived blood cells (e.g., skin cultured fibroblasts).
Table 1 showcases the diagnostic work-up in a patient with suspected AA and the potential differential diagnoses.
Diagnosis and identification of immune-mediated aplastic anemia
-The role of PNH clone(s)
PNH is a rare chronic condition characterized by anemia due to intravascular hemolysis and an elevated risk of thrombosis. The disease is caused by acquired mutations of the PIGA gene, that leads to a glycosylphosphatidylinositol (GPI) deficiency on all cells deriving from the mutant stem cells [19, 20]. GPI synthesis is essential for the expression of GPI-anchored complement regulatory proteins CD55 (C3 convertases inhibitor) and CD59 (membrane attack complex formation inhibitor) on blood cells. Their absence generates an uncontrolled complement activation against red blood cells (causing hemolysis), granulocytes, monocytes and platelets (favouring thrombosis) [21].
PIGA-mutant blood cells may be found in healthy people (clone size can be very small <1%) with an absence of any (apparent) hematological alteration [22]. However, most of these are transient due to the absence of a clonal advantage and self-renewal capacity [23]. Indeed, PNH can be intrinsically linked to AA as commonly PIGA mutations are supposed to represent a mechanism of escape for the HSPCs from autoimmune cytotoxic attack. Besides, rare cases of spontaneous remissions, perhaps upon cessation of such stimuli, or other forms of clonal evolution, have also been described [24].
The detection of PNH clones is therefore useful in the workup of patients with AA as small clones, even if not clinically significant, may support the immune origin of the disease and seem to be associated with better disease outcomes and indeed response to immune suppressive therapies (IST) [6]. The gold standard assay to assess for the presence of a PNH clone is the use of multiparametric flow cytometry for the expression of GPI-anchored antigens (e.g., CD55 and CD59, among others) on granulocytes or monocytes [25, 26]. The addition of FLAER, a fluorochrome-conjugated inactive variant of aerolysin (a bacterial derived protein) able to tie to GPI-anchored antigens, has emerged as a valuable diagnostic tool, thanks to its diagnostic efficacy independent of cell maturation stage [12, 27, 28].
However, whilst useful in guiding AA diagnosis, the presence of PNH clone(s) is not specific as up to 20% of patients with MDS may also harbor small PNH clones [29]. Several studies have revealed the presence of a peripheral blood PNH clone in bone marrow failure syndromes, especially AA and MDS [30,31,32,33]. Generally, the majority of these cases never experience intravascular hemolysis, thereby defining a condition of subclinical PNH [34]. Of note, MDS harboring PNH clone(s) were usually categorized as refractory anemias, characterized by a hypocellular marrow, moderate to severe thrombocytopenia, normal karyotype, HLA-DR15 positivity and good clinical response to IST [32, 33]. Therefore, hMDS and AA may sometimes share the presence of small PNH clones, further ‘muddying the diagnostic waters’ between these conditions [13]. The prevalence of PNH clones is generally higher in AA than in lower risk MDS, with the clone size often being larger in AA [33, 35].
Identification of PNH clones may impart additional information regarding the risk of developing secondary hemolytic PNH, one of the two late clonal evolution events that AA patients may experience if treated with non-transplant strategies. A Japanese study retrospectively examined PNH clone size kinetics in bone marrow failure syndrome patients harboring a PNH clone <10% at baseline [36]. Based on dynamic longitudinal changes of PNH clone percentages, three groups were identified. The “expansion” group (13 cases) comprised patients whose clone became ≥10% at the time of last evaluation. Among these, eight progressed to classical hemolytic PNH. The “disappearance” group (mostly including cases with a PNH clone size originally <1%) comprised 18 cases in which the PNH clone became undetectable. The remaining 44 cases (80% of which characterized by a PNH clone <1%) had PNH clone(s) persistently <10% and thus were classified as belonging to the “persistent” group. The delineation that a PNH clone size ≥10% is associated with an increased risk of subsequent clinical PNH development, and that detection of PNH clones <1% generally guarantees long-term stability with no risk of clinically relevant PNH development, has also been confirmed in independent studies [37].
Given the aforementioned evidence, the presence of a PNH clone in AA may be considered a factor, among others including age, disease staging, molecular profile, donor availability, potentially favouring an IST approach [8, 10, 38].
-The role of myeloid genes profiling
Recent evidence stemming from application of NGS to large cohorts of patients with bone marrow failure syndromes and MDS has contributed to enhanced clarification of the diagnostic borders between these nosological entities, yet it is well established that some genomic overlap exists. An added layer of complexity for consideration is that myeloid gene mutations may be a result of the oligoclonal state following the immunological insult inherent to the pathophysiology of AA (sometimes in a “passenger fashion”), the by-product of normal aging (e.g., clonal hematopoiesis of indeterminate potential (CHIP)), or rather represent actual markers of myeloid neoplasia [17, 39, 40]. In this regard, pivotal studies have dissected the molecular profiles of AA and compared to that of hMDS and normo/hypercellular MDS, highlighting how the latter is enriched with mutations in spliceosome components and chromatin modifiers (e.g., SF3B1, SRSF2, ASXL1) [41]. In AA patients, besides PIGA, BCOR and BCORL mutations tend to be more frequent and generally occur in younger patients, and may be associated with a more favorable prognosis [6, 42]. As discussed above, the baseline molecular profile of an AA patient is important not only in aiding the initial diagnosis but also in estimating the risk of clonal evolution to MDS or acute myeloid leukemia (AML) following IST. IST is clearly well established as a potential treatment approach but paradoxically can also accelerate the process of clonal selection by inducing the repopulation of the BM with few residual stem cells possibly harboring myeloid mutations (a so called ‘bottleneck effect’) [17]. Indeed, patients with AA and myeloid mutations other than BCOR/BCORL at diagnosis have an increased risk for myeloid progression at a median of 4.5 years from initial diagnosis when treated with non-transplant strategies [6]. This risk is estimated to reach up to 40% at 10 years from AA onset and can potentially orientate the clinician to consideration of a transplant approach either at disease onset or in those cases demonstrating subsequent clonal evolution during follow-up [6, 9, 39, 43].
-The role of HLA and T-cell clonality
It is now well established that specific HLA constellations, allelic loss and presence of inactivating somatic mutations (of HLA-class I/II alleles) represent alterations underpinning disease development, immunological escape and clonal evolution [5, 44, 45].
Of particular interest is the enrichment in alleles structurally similar to DRB1*15:01, which may sustain the presence of cross reactive and autoreactive CD4+ specificities [45]. Some reports identified a patient-specific expansion of Influenza-A, cytomegalovirus (CMV), Epstein Barr virus (EBV) or mycobacterium-related T-cell specificities. These may be responsible for mechanisms of cross reactivity with self-antigens, sharing similar physiochemical characteristics with pathogen-associated epitopes [45].
Recently, Olson at al [46]. Identified 19 ‘risk alleles’ and 12 ‘protective alleles’ associated with AA pathogenesis. Approximately 60–85% of individuals affected by AA have HLA-A/B allelic variations, in particular, two alleles HLA-B 14:02 and HLA-B 40:02 have been classified as highly pathogenic and their presence, especially HLA-B 14:02, has been associated with an increased risk of MDS-clonal evolution predominantly in adult patients [46]. However, these HLA constellations do not appear to influence the outcome of patients undergoing IST or candidates for allo-HCT. Analogous to PNH development, loss of expression of some HLA alleles on the surface of HSPCs via genetic aberrancies or epigenetic mechanisms can propagate immune-privileged hematopoiesis [5]. Somatic HLA mutations have been found in both class I and II loci, highlighting the pressure of differing T-cell clones on HLA molecules [5]. Nonetheless, whether their acquisition modifies the trajectories of clonal evolution still remains a matter of debate, and longitudinal studies with prolonged follow up, at present, do not confirm an independent role in promoting malignant transformation [47, 48].
In addition to some known HLA alterations, such as copy number–neutral loss of heterozygosity of chromosome arm 6p (6p CN-LOH) and PNH clone(s) identification, the early diagnosis of AA can be also supported by evaluation of T cell clonality. In most cases of acquired bone marrow disorders (AA, PNH disease, MDS) it is common to find a typical bone marrow infiltrate by T lymphocytes (especially large granular lymphocytes (LGL)). Therefore, it is also possible to study the clonality of these T cell populations through T cell receptor (TCR) rearrangement analysis [49].
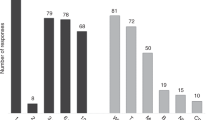
Shah et al. [50]. Evaluated the presence of PNH clones, 6p CN-LOH and TCRγ rearrangements in a cohort of 454 pediatric and adult patients with acquired aplastic disorders and IBMFS. Results highlighted that unlike detection of PNH clones and the 6p CN-LOH which have a specificity of 100% with a positive predictive value (PPV) of 100%, confirmation of T cell clonality does not represent a marker specific for the diagnosis of AA. However, clonal rearrangements of the TCRγ are more frequently detected in adult patients with acquired bone marrow disorders and in PNH disease or hMDS (prevalence >60%) [50].
Therapeutic considerations and role of transplantation
Once the diagnosis of immune-mediated AA has been established, the decision to proceed to transplant may be complex and necessitates consideration to many variables.
In fact, allo-HCT represents the only potentially curative option capable of reducing the risk of clonal evolution for patients with severe or very severe AA. However, we must bear in mind that post-transplant outcomes are influenced by both patient characteristics, such as age, performance status and co-morbidities, and type of donor. Generally, allo-HCT represents the first-line therapy for all young patients aged <40 years who have a matched sibling donor (MSD) [10, 15, 51]. In the case of patients aged >40 years or younger patients lacking a MSD, allo-HCT is in general used second line following failure of IST, frequently based on anti-thymocyte globulins (ATG) and cyclosporine A (CSA) [10, 15]. In patients with severe or very severe AA aged <20 years, allo-HCT should be considered the first choice, resorting if necessary to an unrelated donor. Transplants with alternative donors (mismatched related/unrelated or umbilical cord blood) can be considered on a case by case basis but generally are reserved for second or further line strategies even in pediatric or AYA populations [15].
As mentioned above, in patients treated with IST, clonal evolution can occur many years after diagnosis, therefore close long-term disease monitoring must be carried out in order to promptly diagnose MDS progression and rapidly proceed with allo-HCT. In the largest study so far reported, outcomes of patients developing MDS post-AA were best when patients were treated with low bulk disease (<5% BM blasts) while general overall survival was estimated at 40% at 5 years [6].
In the last decade, novel conditioning and graft-versus-host disease (GVHD) prophylaxis regimens have dramatically changed the scenario of patients undergoing allo-HCT, making this procedure increasingly accessible even in the absence of a MSD. Indeed, recent studies have demonstrated excellent outcomes for patients with AA lacking a suitable MSD undergoing allo-HCT utilising alternative HLA-mismatched donors and post-transplant cyclophosphamide (PTCy) for GVHD prophylaxis. Leveraging reduced-intensity conditioning including a total body irradiation dose of 400 cGy to reduce the risk of graft failure, outcomes from AA allo-HCT using HLA-haploidentical donors and PTCy have demonstrated optimal engraftment rates (exceeding 90%) and a very low incidence of GVHD (<10%) [52,53,54]. These results coupled with the high failure-free survival rates and abrogation of the risk of life-long clonal evolution, have questioned the treatment algorithm of patients with AA, favouring an early referral to consideration of allo-HCT. Furthermore, the recent results of the RACE trial, which added eltrombopag to standard IST and demonstrated clinically beneficial responses in 2/3 of cases by 6 months on treatment, generated more questions as to the optimal sequential strategy in AA [42]. Notably, the longer term follow-up of patients in this trial is still too limited to draw general conclusions regarding the risk of later clonal evolution and hence long-term outcomes are eagerly awaited.
While the presence of small PNH clones (generally <10%) in patients with AA associates with better outcomes after conservative strategies [35, 55,56,57,58,59], the lack of response to IST, numerous relapses, and the presence/new acquisition of cytogenetic and/or molecular aberrations represent elements in favor of allo-HCT as a possible curative therapy [6].
NGS analysis allows also a more accurate estimation of clonal evolution risk by assessing for the presence of oligoclonal or clonal hematopoiesis. Approximately 70% of patients affected by acquired AA may present with myeloid gene mutations typical of clonal hematopoiesis [6, 39], thus rapid identification of molecular mutations with an unfavorable prognosis is essential to define the most appropriate treatment, and timely referral of patients for allo-HCT [6, 43].
In the IBMFS landscape, allo-HCT plays an essential but controversial role. Indeed, while potentially curative for the hematological manifestations, it clearly cannot resolve extra-hematological alterations and does not allow adequate control of the risk of secondary neoplasms, which could be particularly high in several subsets of patients. Generally, in IBMFS the first choice is represented by allo-HCT from an unaffected MSD after appropriate evaluation and genetic screening. In very selected cases, resorting to umbilical cord blood has been attempted, while the choice of an alternative or haploidentical donor currently remains confined to clinical trials. The main aspect to consider is the high risk of early complications, driven by the toxicity of the conditioning, but also the increased risk of both acute and chronic GVHD and graft failure. For these reasons, fludarabine-based reduced intensity conditioning regimes are mainly used. Among the long-term complications, the high risk of second tumors requires judicious follow-up [16, 60].
Conclusive remarks and future perspectives
To date, AA remains an extremely complex diagnosis. However, accurate diagnostic work-up that includes comprehensive cytogenetic and molecular annotation can not only facilitate correct diagnostic classification, but can additionally inform on therapeutic choice/sequencing, especially in younger patients where differing therapeutic avenues exist. Among these, the identification of PNH clones, recurrent cytogenetic alterations, or aberrations such as loss of HLA alleles and somatic mutations of genes involved in the mechanisms of clonal evolution may be essential variables to consider. Moreover, genetic screening represents a fundamental diagnostic element in pediatric and AYA patients in order to identify forms of IBMFS, where specific consideration is necessary to personalise allo-HCT platforms in order to limit toxicity.
References
Gurnari C, Pagliuca S, Maciejewski JP. Clonal evolution in aplastic anemia: failed tumor surveillance or maladaptive recovery? Leuk Lymphoma. 2023;64:1389–99.
Li SS, Hsu YT, Chang C, Lee SC, Yen CC, Cheng CN, et al. Incidence and treatment outcome of aplastic anemia in Taiwan-real-world data from single-institute experience and a nationwide population-based database. Ann Hematol. 2019;98:29–39.
Vaht K, Göransson M, Carlson K, Isaksson C, Lenhoff S, Sandstedt A, et al. Incidence and outcome of acquired aplastic anemia: real-world data from patients diagnosed in Sweden from 2000-2011. Haematologica. 2017;102:1683–90.
Gurnari C, Maciejewski JP. Aplastic anemia: Quo vadis? Semin Hematol. 2022;59:54–5.
Pagliuca S, Gurnari C, Hercus C, Hergalant S, Nadarajah N, Wahida A, et al. Molecular landscape of immune pressure and escape in aplastic anemia. Leukemia. 2023;37:202–11.
Gurnari C, Pagliuca S, Prata PH, Galimard J-E, Catto LFB, Larcher L, et al. Clinical and molecular determinants of clonal evolution in aplastic anemia and paroxysmal nocturnal hemoglobinuria. J Clin Oncol. 2022;41:132–42.
Young NS. Aplastic anemia. N Engl J Med. 2018;379:1643–56.
Bacigalupo A, Hows J, Gluckman E, Nissen C, Marsh J, Van Lint MT, et al. Bone marrow transplantation (BMT) versus immunosuppression for the treatment of severe aplastic anaemia (SAA): a report of the EBMT SAA working party. Br J Haematol. 1988;70:177–82.
Gurnari C, Prata PH, Catto LFB, Durmaz A, Larcher L, Sébert M, et al. IPSS-M in myelodysplastic neoplasms arising from aplastic anemia and paroxysmal nocturnal hemoglobinuria. Blood. 2023;141:3122–5.
Bacigalupo A. How I treat acquired aplastic anemia. Blood. 2017;129:1428–36.
DeZern AE, Churpek JE. Approach to the diagnosis of aplastic anemia. Blood Adv. 2021;5:2660–71.
Gurnari C, Graham AC, Efanov A, Pagliuca S, Durrani J, Awada H, et al. Frequency and perturbations of various peripheral blood cell populations before and after eculizumab treatment in paroxysmal nocturnal hemoglobinuria. Blood Cells Mol Dis. 2021;87:102528.
Durrani J, Maciejewski JP. Idiopathic aplastic anemia vs hypocellular myelodysplastic syndrome. Hematol Am Soc Hematol Educ Program. 2019;2019:97–104.
Bejanyan N, Kim S, Hebert KM, Kekre N, Abdel-Azim H, Ahmed I, et al. Choice of conditioning regimens for bone marrow transplantation in severe aplastic anemia. Blood Adv. 2019;3:3123–31.
Bacigalupo A, Benintende G. Bone marrow transplantation for acquired aplastic anemia: what’s new. Best Pract Res Clin Haematol. 2021;34:101284.
Sakaguchi H, Yoshida N. Recent advances in hematopoietic cell transplantation for inherited bone marrow failure syndromes. Int J Hematol. 2022;116:16–27.
Ogawa S. Clonal hematopoiesis in acquired aplastic anemia. Blood. 2016;128:337–47.
Gálvez E, Vallespín E, Arias-Salgado EG, Sánchez-Valdepeñas C, Giménez Y, Navarro S, et al. Next-generation sequencing in bone marrow failure syndromes and isolated cytopenias: experience of the Spanish network on bone marrow failure syndromes. Hemasphere. 2021;5:e539.
Miyata T, Takeda J, Iida Y, Yamada N, Inoue N, Takahashi M, et al. The cloning of PIG-A, a component in the early step of GPI-anchor biosynthesis. Science. 1993;259:1318–20.
Miyata T, Yamada N, Iida Y, Nishimura J, Takeda J, Kitani T, et al. Abnormalities of PIG-A transcripts in granulocytes from patients with paroxysmal nocturnal hemoglobinuria. N. Engl J Med. 1994;330:249–55.
Gurnari C, Pagliuca S, Patel BJ, Awada H, Kongkiatkamon S, Terkawi L, et al. Implication of PIGA genotype on erythrocytes phenotype in Paroxysmal Nocturnal Hemoglobinuria. Leukemia. 2021;35:2431–4.
Araten DJ, Nafa K, Pakdeesuwan K, Luzzatto L. Clonal populations of hematopoietic cells with paroxysmal nocturnal hemoglobinuria genotype and phenotype are present in normal individuals. Proc Natl Acad Sci. 1999;96:5209–14.
Hu R, Mukhina GL, Piantadosi S, Barber JP, Jones RJ, Brodsky RA. PIG-A mutations in normal hematopoiesis. Blood. 2005;105:3848–54.
Gurnari C, Pagliuca S, Kewan T, Bahaj W, Mori M, Patel BJ, et al. Is nature truly healing itself? spontaneous remissions in paroxysmal nocturnal hemoglobinuria. Blood Cancer J. 2021;11:187.
Borowitz MJ, Craig FE, Digiuseppe JA, Illingworth AJ, Rosse W, Sutherland DR, et al. Guidelines for the diagnosis and monitoring of paroxysmal nocturnal hemoglobinuria and related disorders by flow cytometry. Cytom B Clin Cytom. 2010;78:211–30.
Hernández-Campo PM, Almeida J, Sánchez ML, Malvezzi M, Orfao A. Normal patterns of expression of glycosylphosphatidylinositol-anchored proteins on different subsets of peripheral blood cells: a frame of reference for the diagnosis of paroxysmal nocturnal hemoglobinuria. Cytom B Clin Cytom. 2006;70:71–81.
Brodsky RA, Mukhina GL, Li S, Nelson KL, Chiurazzi PL, Buckley JT, et al. Improved detection and characterization of paroxysmal nocturnal hemoglobinuria using fluorescent aerolysin. Am J Clin Pathol. 2000;114:459–66.
Sutherland DR, Illingworth A, Marinov I, Ortiz F, Andreasen J, Payne D, et al. ICCS/ESCCA consensus guidelines to detect GPI-deficient cells in paroxysmal nocturnal hemoglobinuria (PNH) and related disorders part 2 - reagent selection and assay optimization for high-sensitivity testing. Cytom B Clin Cytom. 2018;94:23–48.
Maciejewski JP, Rivera C, Kook H, Dunn D, Young NS. Relationship between bone marrow failure syndromes and the presence of glycophosphatidyl inositol-anchored protein-deficient clones. Br J Haematol. 2001;115:1015–22.
Schubert J, Vogt HG, Zielinska-Skowronek M, Freund M, Kaltwasser JP, Hoelzer D, et al. Development of the glycosylphosphatitylinositol-anchoring defect characteristic for paroxysmal nocturnal hemoglobinuria in patients with aplastic anemia. Blood. 1994;83:2323–8.
Griscelli-Bennaceur A, Gluckman E, Scrobohaci ML, Jonveaux P, Vu T, Bazarbachi A, et al. Aplastic anemia and paroxysmal nocturnal hemoglobinuria: search for a pathogenetic link. Blood. 1995;85:1354–63.
Wang H, Chuhjo T, Yasue S, Omine M, Nakao S. Clinical significance of a minor population of paroxysmal nocturnal hemoglobinuria-type cells in bone marrow failure syndrome. Blood. 2002;100:3897–902.
Raza A, Ravandi F, Rastogi A, Bubis J, Lim SH, Weitz I, et al. A prospective multicenter study of paroxysmal nocturnal hemoglobinuria cells in patients with bone marrow failure. Cytom B Clin Cytom. 2014;86:175–82.
Parker C, Omine M, Richards S, Nishimura J, Bessler M, Ware R, et al. Diagnosis and management of paroxysmal nocturnal hemoglobinuria. Blood. 2005;106:3699–709.
Fattizzo B, Ireland R, Dunlop A, Yallop D, Kassam S, Large J, et al. Clinical and prognostic significance of small paroxysmal nocturnal hemoglobinuria clones in myelodysplastic syndrome and aplastic anemia. Leukemia. 2021;35:3223–31.
Sugimori C, Mochizuki K, Qi Z, Sugimori N, Ishiyama K, Kondo Y, et al. Origin and fate of blood cells deficient in glycosylphosphatidylinositol-anchored protein among patients with bone marrow failure. Br J Haematol. 2009;147:102–12.
Bat T, Abdelhamid ON, Balasubramanian SK, Mai A, Radivoyevitch T, Clemente M, et al. The evolution of paroxysmal nocturnal haemoglobinuria depends on intensity of immunosuppressive therapy. Br J Haematol. 2018;182:730–3.
Fattizzo B, Gurnari C, Cassanello G, Bortolotti M, Awada H, Giammarco S, et al. Deciphering treatment patterns in non-severe/moderate aplastic anemia: an international observational study. Leukemia. 2023;37:2479–85.
Yoshizato T, Dumitriu B, Hosokawa K, Makishima H, Yoshida K, Townsley D, et al. Somatic mutations and clonal hematopoiesis in aplastic anemia. N Engl J Med. 2015;373:35–47.
Stanley N, Olson TS, Babushok DV. Recent advances in understanding clonal haematopoiesis in aplastic anaemia. Br J Haematol. 2017;177:509–25.
Kulasekararaj AG, Jiang J, Smith AE, Mohamedali AM, Mian S, Gandhi S, et al. Somatic mutations identify a subgroup of aplastic anemia patients who progress to myelodysplastic syndrome. Blood. 2014;124:2698–704.
Peffault de Latour R, Kulasekararaj A, Iacobelli S, Terwel SR, Cook R, Griffin M, et al. Eltrombopag added to immunosuppression in severe aplastic anemia. N Engl J Med. 2022;386:11–23.
Groarke EM, Patel BA, Shalhoub R, Gutierrez-Rodrigues F, Desai P, Leuva H, et al. Predictors of clonal evolution and myeloid neoplasia following immunosuppressive therapy in severe aplastic anemia. Leukemia. 2022;36:2328–37.
Pagliuca S, Gurnari C, Rubio MT, Visconte V, Lenz TL. Individual HLA heterogeneity and its implications for cellular immune evasion in cancer and beyond. Front Immunol. 2022;13:944872.
Pagliuca S, Gurnari C, Awada H, Kishtagari A, Kongkiatkamon S, Terkawi L, et al. The similarity of class II HLA genotypes defines patterns of autoreactivity in idiopathic bone marrow failure disorders. Blood. 2021;138:2781–98.
Olson TS, Frost BF, Duke JL, Dribus M, Xie HM, Prudowsky ZD, et al. Pathogenicity and impact of HLA class I alleles in aplastic anemia patients of different ethnicities. JCI Insight. 2022;7:e163040.
Babushok DV, Duke JL, Xie HM, Stanley N, Atienza J, Perdigones N, et al. Somatic HLA mutations expose the role of class I–mediated autoimmunity in aplastic anemia and its clonal complications. Blood Adv. 2017;1:1900–10.
Zaimoku Y, Patel BA, Adams SD, Shalhoub R, Groarke EM, Lee AAC, et al. HLA associations, somatic loss of HLA expression, and clinical outcomes in immune aplastic anemia. Blood. 2021;138:2799–809.
Huuhtanen J, Bhattacharya D, Lönnberg T, Kankainen M, Kerr C, Theodoropoulos J, et al. Single-cell characterization of leukemic and non-leukemic immune repertoires in CD8(+) T-cell large granular lymphocytic leukemia. Nat Commun. 2022;13:1981.
Shah YB, Priore SF, Li Y, Tang CN, Nicholas P, Kurre P, et al. The predictive value of PNH clones, 6p CN-LOH, and clonal TCR gene rearrangement for aplastic anemia diagnosis. Blood Adv. 2021;5:3216–26.
Bacigalupo A, Giammarco S, Sica S. Bone marrow transplantation versus immunosuppressive therapy in patients with acquired severe aplastic anemia. Int J Hematol. 2016;104:168–74.
DeZern AE, Zahurak M, Jones RJ, Brodsky RA. Uniform conditioning regardless of donor in bone marrow transplantation for severe aplastic anemia. Haematologica. 2023.
DeZern AE, Eapen M, Wu J, Talano JA, Solh M, Dávila Saldaña BJ, et al. Haploidentical bone marrow transplantation in patients with relapsed or refractory severe aplastic anaemia in the USA (BMT CTN 1502): a multicentre, single-arm, phase 2 trial. Lancet Haematol. 2022;9:e660–e9.
DeZern AE, Zahurak M, Symons HJ, Cooke KR, Huff CA, Jain T, et al. Alternative donor BMT with posttransplant cyclophosphamide as initial therapy for acquired severe aplastic anemia. Blood 2023;141:3031–8.
Sugimori C, Chuhjo T, Feng X, Yamazaki H, Takami A, Teramura M, et al. Minor population of CD55-CD59- blood cells predicts response to immunosuppressive therapy and prognosis in patients with aplastic anemia. Blood. 2006;107:1308–14.
Kulagin A, Lisukov I, Ivanova M, Golubovskaya I, Kruchkova I, Bondarenko S, et al. Prognostic value of paroxysmal nocturnal haemoglobinuria clone presence in aplastic anaemia patients treated with combined immunosuppression: results of two-centre prospective study. Br J Haematol. 2014;164:546–54.
Zhao X, Zhang L, Jing L, Zhou K, Li Y, Peng G, et al. The role of paroxysmal nocturnal hemoglobinuria clones in response to immunosuppressive therapy of patients with severe aplastic anemia. Ann Hematol. 2015;94:1105–10.
Yoshida N, Yagasaki H, Takahashi Y, Yamamoto T, Liang J, Wang Y, et al. Clinical impact of HLA-DR15, a minor population of paroxysmal nocturnal haemoglobinuria-type cells, and an aplastic anaemia-associated autoantibody in children with acquired aplastic anaemia. Br J Haematol. 2008;142:427–35.
Scheinberg P, Wu CO, Nunez O, Young NS. Predicting response to immunosuppressive therapy and survival in severe aplastic anaemia. Br J Haematol. 2009;144:206–16.
Dalle JH, Peffault de Latour R. Allogeneic hematopoietic stem cell transplantation for inherited bone marrow failure syndromes. Int J Hematol. 2016;103:373–9.
Acknowledgements
CG was supported by a grant from the Edward P. Evans Foundation. SP was supported by a grant from the Association HPN France—Aplasie medullaire and Foundation For Rare Diseases (FFRD).
Author information
Authors and Affiliations
Contributions
CG, SP, GC and ES wrote the manuscript. DM revised the manuscript. All authors read and approved the final version of the manuscript and are accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ciangola, G., Santinelli, E., McLornan, D.P. et al. Diagnostic evaluation in bone marrow failure disorders: what have we learnt to help inform the transplant decision in 2024 and beyond?. Bone Marrow Transplant 59, 444–450 (2024). https://doi.org/10.1038/s41409-024-02213-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-024-02213-6