Abstract
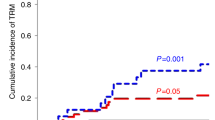
Why a new Perspective in allogeneic hematopoietic transplantation? A summary. Nowadays, for high-risk acute leukemia patients without an HLA-matched donor (sibling or volunteer), hematopoietic transplants that use HLA-haploidentical grafts combined with enhanced post transplant immune suppression (i.e., high-dose cyclophosphamide) are widely used. They are associated with low TRM rates. However, they are also associated with significant chronic GvHD while they only partially abrogate leukemia relapse rates. One may speculate that post-transplant immune suppression, required for GvHD prophylaxis, weakens the anti-leukemic potential of the graft. Historically, haploidentical transplants became feasible for the first time through transplantation of T cell-depleted peripheral blood hematopoietic progenitor cells. Lack of post-transplant immune suppression allowed the emergence of donor-versus-recipient NK-cell alloreactions that eradicated AML. In an attempt to improve these results we recently combined an age-adapted, irradiation-based conditioning regimen with transplant of T-cell-depleted grafts and infusion of regulatory and conventional T cells, without any post transplant immune suppression. With the obvious limitations of a single center experience, this protocol resulted in extremely low relapse and chronic GvHD rates and, consequently, in a remarkable 75% chronic GvHD/relapse-free survival in over 50 AML patients up to the age of 65 many of whom at high risk of relapse.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Appelbaum FR, Forman SJ, Negrin RS, Blume KG (eds). Thomas’ Hematopoietic Cell Transplantation. 4th ed. Wiley-Blackwell, Oxford, 2009.
Anasetti C, Aversa F, Velardi A. Hematopoietic cell transplantation from human leukocyte antigen partially matched related donors. In: Appelbaum FR, Forman SJ, Negrin RS, Blume KG (eds). Thomas’ Hematopoietic Cell Transplantation. 4th ed. Wiley-Blackwell, Oxford, 2009. pp 657-74.
Mancusi A, Ruggeri L, Velardi A. Haploidentical hematopoietic transplantation for the cure of leukemia: from its biology to clinical translation. Blood. 2016;128:2616–23. https://doi.org/10.1182/blood-2016-07-730564.
Kanakry CG, Fuchs EJ, Luznik L. Modern approaches to HLA-haploidentical blood or marrow transplantation. Nat Rev Clin Oncol. 2016;13:132. https://doi.org/10.1038/nrclinonc.2015.128.
O’Donnell PV, Luznik L, Jones RJ, Vogelsang GB, Leffell MS, Phelps M, et al. Nonmyeloablative bone marrow transplantation from partially HLA-mismatched related donors using posttransplantation cyclophosphamide. Biol Blood Marrow Transpl. 2002;8:377–86. https://doi.org/10.1053/bbmt.2002.v8.pm12171484.
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transpl. 2008;14:641–50. https://doi.org/10.1016/j.bbmt.2008.03.005.
McCurdy SR, Kanakry JA, Showel MM, Tsai HL, Bolaños-Meade J, Rosner GL, et al. Risk-stratified outcomes of nonmyeloablative HLA-haploidentical BMT with high-dose posttransplantation cyclophosphamide. Blood. 2015;125:3024–31. https://doi.org/10.1182/blood-2015-01-623991.
Ciurea SO, Zhang MJ, Bacigalupo AA, Bashey A, Appelbaum FR, Aljitawi OS, et al. Haploidentical transplant with posttransplant cyclophosphamide vs matched unrelated donor transplant for acute myeloid leukemia. Blood. 2015;126:1033–40. https://doi.org/10.1182/blood-2015-04-639831.
Solomon SR, St Martin A, Shah NN, Fatobene G, Al Malki MM, Ballen KK, et al. Myeloablative vs reduced intensity T-cell-replete haploidentical transplantation for hematologic malignancy. Blood Adv. 2019;3:2836–44. https://doi.org/10.1182/bloodadvances.2019000627.
Gooptu M, Romee R, St Martin A, Arora M, Al Malki M, Antin JH, et al. HLA-haploidentical vs matched unrelated donor transplants with posttransplant cyclophosphamide-based prophylaxis. Blood. 2021;138:273–82. https://doi.org/10.1182/blood.2021011281.
Raiola AM, Angelucci E, Sica S, Bacigalupo A. Haploidentical bone marrow transplants with post transplant cyclophosphamide on day + 3 + 5: The Genova protocol. Blood Rev. 2022;62:101031. https://doi.org/10.1016/j.blre.2022.101031.
Aversa F, Tabilio A, Velardi A, Cunningham I, Terenzi A, Falzetti F, et al. Treatment of high-risk acute leukemia with T-cell-depleted stem cells from related donors with one fully mismatched HLA haplotype. N. Engl J Med. 1998;339:1186–93. https://doi.org/10.1056/NEJM199810223391702.
Aversa F, Terenzi A, Tabilio A, Falzetti F, Carotti A, Ballanti S, et al. Full haplotype-mismatched hematopoietic stem-cell transplantation: a phase II study in patients with acute leukemia at high risk of relapse. J Clin Oncol. 2005;23:3447–54. https://doi.org/10.1200/JCO.2005.09.117.
Ciceri F, Labopin M, Aversa F, Rowe JM, Bunjes D, Lewalle P, et al. Acute Leukemia Working Party (ALWP) of European Blood and Marrow Transplant (EBMT) Group. A survey of fully haploidentical hematopoietic stem cell transplantation in adults with high-risk acute leukemia: a risk factor analysis of outcomes for patients in remission at transplantation. Blood. 2008;112:3574–81. https://doi.org/10.1182/blood-2008-02-140095.
Ruggeri L, Capanni M, Casucci M, Volpi I, Tosti A, Perruccio K, et al. Role of natural killer cell alloreactivity in HLA-mismatched hematopoietic stem cell transplantation. Blood. 1999;94:333–9. https://doi.org/10.1182/blood.V94.1.333.413a31_333_339.
Ruggeri L, Capanni M, Urbani E, Perruccio K, Shlomchik WD, Tosti A, et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science. 2002;295:2097–100. https://doi.org/10.1126/science.1068440.
Kärre K. Immunology. A perfect mismatch. Science. 2002;295:2029–31. https://doi.org/10.1126/science.1070538.
Ruggeri L, Mancusi A, Capanni M, Urbani E, Carotti A, Aloisi T, et al. Donor natural killer cell allorecognition of missing self in haploidentical hematopoietic transplantation for acute myeloid leukemia: challenging its predictive value. Blood. 2007;110:433–40. https://doi.org/10.1182/blood-2006-07-038687.
Velardi A, Ruggeri L, Mancusi A, Aversa F, Christiansen FT. Natural killer cell allorecognition of missing self in allogeneic hematopoietic transplantation: a tool for immunotherapy of leukemia. Curr Opin Immunol. 2009;21:525–30. https://doi.org/10.1016/j.coi.2009.07.015.
Vivier E, Raulet DH, Moretta A, Caligiuri MA, Zitvogel L, Lanier LL, et al. Innate or adaptive immunity? The example of natural killer cells. Science. 2011;331:44–49. https://doi.org/10.1126/science.1198687.
Parham P. MHC class I molecules and KIRs in human history, health and survival. Nat Rev Immunol. 2005;5:201–14. https://doi.org/10.1038/nri1570.
Kärre K, Ljunggren HG, Piontek G, Kiessling R. Selective rejection of H-2-deficient lymphoma variants suggests alternative immune defence strategy. Nature. 1986;319:675–8. https://doi.org/10.1038/319675a0.
Colonna M, Brooks EG, Falco M, Ferrara GB, Strominger JL. Generation of allospecific natural killer cells by stimulation across a polymorphism of HLA-C. Science. 1993;260:1121–4. https://doi.org/10.1126/science.8493555.
Haas P, Loiseau P, Tamouza R, Cayuela JM, Moins-Teisserenc H, Busson M, et al. NK-cell education is shaped by donor HLA genotype after unrelated allogeneic hematopoietic stem cell transplantation. Blood. 2011;117:1021–9. https://doi.org/10.1182/blood-2010-02-269381.
Leung W, Iyengar R, Turner V, Lang P, Bader P, Conn P, et al. Determinants of antileukemia effects of allogeneic NK cells. J Immunol. 2004;172:644–50. https://doi.org/10.4049/jimmunol.172.1.644.
Edinger M, Hoffmann P, Ermann J, Drago K, Fathman CG, Strober S, et al. CD4+CD25+ regulatory T cells preserve graft-versus-tumor activity while inhibiting graft-versus-host disease after bone marrow transplantation. Nat Med. 2003;9:1144–50. https://doi.org/10.1038/nm915.
Martelli MF, Di Ianni M, Ruggeri L, Falzetti F, Carotti A, Terenzi A, et al. HLA-haploidentical transplantation with regulatory and conventional T cell adoptive immunotherapy prevents acute leukemia relapse. Blood. 2014;124:638–44. https://doi.org/10.1182/blood-2014-03-564401.
Booth NJ, McQuaid AJ, Sobande T, Kissane S, Agius E, Jackson SE, et al. Different proliferative potential and migratory characteristics of human CD4+ regulatory T cells that express either CD45RA or CD45RO. J Immunol. 2010;184:4317–26. https://doi.org/10.4049/jimmunol.0903781.
Ruggeri L, Carotti A, Pierini A, Falzetti F, Terenzi A, Urbani E, et al. How adoptive immunotherapy with conventional T and regulatory T cells exerts a Gvl effect without GvHD, after haploidentical hematopoietic transplantation. Blood. 2018;132:3333. https://doi.org/10.1182/blood-2018-99-112512.
Pierini A, Ruggeri L, Carotti A, Falzetti F, Saldi S, Terenzi A, et al. Haploidentical age-adapted myeloablative transplant and regulatory and effector T cells for acute myeloid leukemia. Blood Adv. 2021;5:1199–208. https://doi.org/10.1182/bloodadvances.2020003739.
Wong JY, Liu A, Schultheiss T, Popplewell L, Stein A, Rosenthal J, et al. Targeted total marrow irradiation using three-dimensional image-guided tomographic intensity-modulated radiation therapy: an alternative to standard total body irradiation. Biol Blood Marrow Transpl. 2006;12:306–15. https://doi.org/10.1016/j.bbmt.2005.10.026.
Rosenthal J, Wong J, Stein A, Qian D, Hitt D, Naeem H, et al. Phase 1/2 trial of total marrow and lymph node irradiation to augment reduced-intensity transplantation for advanced hematologic malignancies. Blood. 2011;117:309–15. https://doi.org/10.1182/blood-2010-06-288357.
Jensen LG, Stiller T, Wong JYC, Palmer J, Stein A, Rosenthal J. Total marrow lymphoid irradiation/fludarabine/melphalan conditioning for allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transpl. 2018;24:301–7. https://doi.org/10.1016/j.bbmt.2017.09.019.
Di Ianni M, Falzetti F, Carotti A, Terenzi A, Castellino F, Bonifacio E, et al. Tregs prevent GVHD and promote immune reconstitution in HLA-haploidentical transplantation. Blood. 2011;117:3921–8. https://doi.org/10.1182/blood-2010-10-311894.
Fang M, Storer B, Estey E, Othus M, Zhang L, Sandmaier BM, et al. Outcome of patients with acute myeloid leukemia with monosomal karyotype who undergo hematopoietic cell transplantation. Blood. 2011;118:1490–4. https://doi.org/10.1182/blood-2011-02-339721.
Ciurea SO, Labopin M, Socie G, Volin L, Passweg J, Chevallier P, et al. Relapse and survival after transplantation for complex karyotype acute myeloid leukemia: a report from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation and the University of Texas MD Anderson Cancer Center. Cancer. 2018;124:2134–41. https://doi.org/10.1002/cncr.31311.
Walter RB, Gyurkocza B, Storer BE, Godwin CD, Pagel JM, Buckley SA, et al. Comparison of minimal residual disease as outcome predictor for AML patients in first complete remission undergoing myeloablative or nonmyeloablative allogeneic hematopoietic cell transplantation. Leukemia. 2015;29:137–44. https://doi.org/10.1038/leu.2014.173.
Araki D, Wood BL, Othus M, Radich JP, Halpern AB, Zhou Y, et al. Allogeneic hematopoietic cell transplantation for acute myeloid leukemia: time to move toward a minimal residual disease-based definition of complete remission? J Clin Oncol. 2016;34:329–36. https://doi.org/10.1200/JCO.2015.63.3826.
Stein A, Palmer J, Tsai NC, Al Malki MM, Aldoss I, Ali H, et al. Phase I trial of total marrow and lymphoid irradiation transplantation conditioning in patients with relapsed/refractory acute leukemia. Biol Blood Marrow Transpl. 2017;23:618–24. https://doi.org/10.1016/j.bbmt.2017.01.067.
Pierini A, Strober W, Moffett C, Baker J, Nishikii H, Alvarez M, et al. TNF-a priming enhances CD41FoxP31 regulatory T-cell suppressive function in murine GVHD prevention and treatment. Blood. 2016;128:866–71. https://doi.org/10.1182/blood-2016-04-711275.
Del Papa B, Ruggeri L, Urbani E, Baldoni S, Cecchini D, Zei T, et al. Clinical-grade-expanded regulatory T cells prevent graft-versus-host disease while allowing a powerful T cell-dependent graft-versus-leukemia effect in murine models. Biol Blood Marrow Transpl. 2017;23:1847–51. https://doi.org/10.1016/j.bbmt.2017.07.009.
Honaker Y, Hubbard N, Xiang Y, Fisher L, Hagin D, Sommer K, et al. Gene editing to induce FOXP3 expression in human CD41 T cells leads to a stable regulatory phenotype and function. Sci Transl Med. 2020;12:eaay6422. https://doi.org/10.1126/scitranslmed.aay6422.
Mielcarek M, Furlong T, O’Donnell PV, Storer BE, McCune JS, Storb R, et al. Post-transplantation cyclophosphamide for prevention of graft-versus-host disease after HLA-matched mobilized blood cell transplantation. Blood. 2016;127:1502–8. https://doi.org/10.1182/blood-2015-10-672071.
Nakamae H. Systematic overview of HLA-matched allogeneic hematopoietic cell transplantation with post-transplantation cyclophosphamide. Int J Hematol. 2022;116:465–81. https://doi.org/10.1007/s12185-022-03428-3.
Broers AEC, de Jong CN, Bakunina K, Hazenberg MD, van Marwijk Kooy M, de Groot MR, et al. Posttransplant cyclophosphamide for prevention of graft-versus-host disease: results of the prospective randomized HOVON-96 trial. Blood Adv. 2022;6:3378–85. https://doi.org/10.1182/bloodadvances.2021005847.
Mehta RS, Saliba RM, Rondon G, Al-Atrash G, Bashir Q, Hosing CM, et al. Post-Transplantation Cyclophosphamide Versus Tacrolimus and Methotrexate Graft-Versus-Host Disease Prophylaxis for HLA-Matched Donor Transplantation. Transpl Cell Ther. 2022;28:695.e1–695.e10. https://doi.org/10.1016/j.jtct.2022.07.021.
Nagler A, Labopin M, Swoboda R, Kulagin A, Labussière-Wallet H, Rovira M, et al. Allogeneic stem cell transplantation for patients with acute myeloid leukemia (AML) in second complete remission (CR2) transplanted from unrelated donors with post-transplant cyclophosphamide (PTCy). A study on behalf of the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Bone Marrow Transpl. 2023;58:552–7. https://doi.org/10.1038/s41409-023-01940-6.
Bolaños-Meade J, Hamadani M, Wu J, Al Malki MM, Martens MJ, Runaas L, et al. Post-transplantation cyclophosphamide-based graft-versus-host disease prophylaxis. N. Engl J Med. 2023;388:2338–48. https://doi.org/10.1056/NEJMoa2215943.
Pierini A, Ruggeri L, Saldi S, Tricarico S, Marzuttini F, Viglione V, et al. HLA-Matched Treg/Tcon allogeneic hematopoietic cell transplantation is safe and ensures remarkable chronic GvHD/leukemia free survival in high-risk leukemia patients. Blood. 2022;140:2133–4. https://doi.org/10.1182/blood-2022-169351.
Acknowledgements
LR is PI of the project “Adoptive immunotherapies with regulatory and conventional T cells and/or Natural Killer cells: safe and effective strategies to minimize the risk of leukemia relapse after allogeneic hematopoietic stem cell transplantation”, RF-2016-02364383 funded by Italian Ministry of Health. AP is PI of the project “Insights into Treg biology and T cell-based cancer immunotherapies”, START-UP grant number 20456 funded by Associazione Italiana per la Ricerca sul Cancro.
Author information
Authors and Affiliations
Contributions
AV wrote the article; AM, LR, and AP edited the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Velardi, A., Mancusi, A., Ruggeri, L. et al. How adoptive transfer of components of the donor immune system boosts GvL and prevents GvHD in HLA-haploidentical hematopoietic transplantation for acute leukemia. Bone Marrow Transplant 59, 301–305 (2024). https://doi.org/10.1038/s41409-024-02199-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-024-02199-1