Abstract
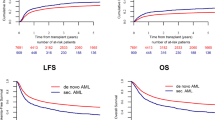
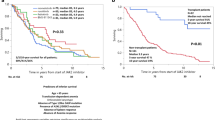
Allogeneic hematopoietic cell transplantation (allo-HCT) is curative for myelofibrosis (MF) but assessing risk-benefit in individual patients is challenging. This complexity is amplified in CALR-mutated MF patients, as they live longer with conventional treatments compared to other molecular subtypes. We analyzed outcomes of 346 CALR-mutated MF patients who underwent allo-HCT in 123 EBMT centers between 2005 and 2019. After a median follow-up of 40 months, the estimated overall survival (OS) rates at 1, 3, and 5 years were 81%, 71%, and 63%, respectively. Patients receiving busulfan-containing regimens achieved a 5-year OS rate of 71%. Non-relapse mortality (NRM) at 1, 3, and 5 years was 16%, 22%, and 26%, respectively, while the incidence of relapse/progression was 11%, 15%, and 17%, respectively. Multivariate analysis showed that older age correlated with worse OS, while primary MF and HLA mismatched transplants had a near-to-significant trend to decreased OS. Comparative analysis between CALR- and JAK2-mutated MF patients adjusting for confounding factors revealed better OS, lower NRM, lower relapse, and improved graft-versus-host disease-free and relapse-free survival (GRFS) in CALR-mutated patients. These findings confirm the improved prognosis associated with CALR mutation in allo-HCT and support molecular profiling in prognostic scoring systems to predict OS after transplantation in MF.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Tefferi A. Primary myelofibrosis: 2023 update on diagnosis, risk-stratification, and management. Am J Hematol. 2023;98:801–21.
Bewersdorf JP, Sheth AH, Vetsa S, Grimshaw A, Giri S, Podoltsev NA, et al. Outcomes of allogeneic hematopoietic cell transplantation in patients with myelofibrosis—a systematic review and meta-analysis. Transpl Cell Ther. 2021;27:873.e1–e13.
McLornan D, Eikema DJ, Czerw T, Kroger N, Koster L, Reinhardt HC, et al. Trends in allogeneic haematopoietic cell transplantation for myelofibrosis in Europe between 1995 and 2018: a CMWP of EBMT retrospective analysis. Bone Marrow Transpl. 2021;56:2160–72.
Rumi E, Pietra D, Pascutto C, Guglielmelli P, Martinez-Trillos A, Casetti I, et al. Clinical effect of driver mutations of JAK2, CALR, or MPL in primary myelofibrosis. Blood. 2014;124:1062–9.
Passamonti F, Mora B, Giorgino T, Guglielmelli P, Cazzola M, Maffioli M, et al. Driver mutations’ effect in secondary myelofibrosis: an international multicenter study based on 781 patients. Leukemia. 2017;31:970–3.
Cervantes F, Dupriez B, Pereira A, Passamonti F, Reilly JT, Morra E, et al. New prognostic scoring system for primary myelofibrosis based on a study of the International Working Group for Myelofibrosis Research and Treatment. Blood. 2009;113:2895–901.
Passamonti F, Cervantes F, Vannucchi AM, Morra E, Rumi E, Pereira A, et al. A dynamic prognostic model to predict survival in primary myelofibrosis: a study by the IWG-MRT (International Working Group for Myeloproliferative Neoplasms Research and Treatment). Blood. 2010;115:1703–8.
Gangat N, Caramazza D, Vaidya R, George G, Begna K, Schwager S, et al. DIPSS plus: a refined Dynamic International Prognostic Scoring System for primary myelofibrosis that incorporates prognostic information from karyotype, platelet count, and transfusion status. J Clin Oncol. 2011;29:392–7.
Mosquera-Orgueira A, Perez-Encinas M, Hernandez-Sanchez A, Gonzalez-Martinez T, Arellano-Rodrigo E, Martinez-Elicegui J, et al. Machine learning improves risk stratification in myelofibrosis: an analysis of the Spanish registry of myelofibrosis. Hemasphere. 2023;7:e818.
Guglielmelli P, Lasho TL, Rotunno G, Mudireddy M, Mannarelli C, Nicolosi M, et al. MIPSS70: mutation-enhanced international prognostic score system for transplantation-age patients with primary myelofibrosis. J Clin Oncol. 2018;36:310–8.
Tefferi A, Guglielmelli P, Lasho TL, Gangat N, Ketterling RP, Pardanani A, et al. MIPSS70+ version 2.0: mutation and karyotype-enhanced international prognostic scoring system for primary myelofibrosis. J Clin Oncol. 2018;36:1769–70.
Passamonti F, Giorgino T, Mora B, Guglielmelli P, Rumi E, Maffioli M, et al. A clinical-molecular prognostic model to predict survival in patients with post polycythemia vera and post essential thrombocythemia myelofibrosis. Leukemia. 2017;31:2726–31.
Kroger NM, Deeg JH, Olavarria E, Niederwieser D, Bacigalupo A, Barbui T, et al. Indication and management of allogeneic stem cell transplantation in primary myelofibrosis: a consensus process by an EBMT/ELN international working group. Leukemia. 2015;29:2126–33.
Gagelmann N, Ditschkowski M, Bogdanov R, Bredin S, Robin M, Cassinat B, et al. Comprehensive clinical-molecular transplant scoring system for myelofibrosis undergoing stem cell transplantation. Blood. 2019;133:2233–42.
Tamari R, McLornan DP, Ahn KW, Estrada-Merly N, Hernandez-Boluda JC, Giralt SA, et al. A simple prognostic system in myelofibrosis patients undergoing allogeneic stem cell transplant: a CIBMTR/EBMT analysis. Blood Adv. 2023;7:3993–4002.
Kroger N, Panagiota V, Badbaran A, Zabelina T, Triviai I, Araujo Cruz MM, et al. Impact of molecular genetics on outcome in myelofibrosis patients after allogeneic stem cell transplantation. Biol Blood Marrow Transpl. 2017;23:1095–101.
Gagelmann N, Salit RB, Schroeder T, Badbaran A, Rautenberg C, Panagiota V, et al. High molecular and cytogenetic risk in myelofibrosis does not benefit from higher intensity conditioning before hematopoietic cell transplantation: an international collaborative. Anal Hemasphere. 2022;6:e784.
Panagiota V, Thol F, Markus B, Fehse B, Alchalby H, Badbaran A, et al. Prognostic effect of calreticulin mutations in patients with myelofibrosis after allogeneic hematopoietic stem cell transplantation. Leukemia. 2014;28:1552–5.
Holtan SG, DeFor TE, Lazaryan A, Bejanyan N, Arora M, Brunstein CG, et al. Composite end point of graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation. Blood. 2015;125:1333–8.
Copelan E, Casper JT, Carter SL, van Burik JA, Hurd D, Mendizabal AM, et al. A scheme for defining cause of death and its application in the T cell depletion trial. Biol Blood Marrow Transpl. 2007;13:1469–76.
Hernandez-Boluda JC, Pereira A, Kroger N, Beelen D, Robin M, Bornhauser M, et al. Determinants of survival in myelofibrosis patients undergoing allogeneic hematopoietic cell transplantation. Leukemia. 2021;35:215–24.
Hernandez-Boluda JC, Pereira A, Kroger N, Cornelissen JJ, Finke J, Beelen D, et al. Allogeneic hematopoietic cell transplantation in older myelofibrosis patients: a study of the chronic malignancies working party of EBMT and the Spanish Myelofibrosis Registry. Am J Hematol. 2021;96:1186–94.
Ali H, Aldoss I, Yang D, Mokhtari S, Khaled S, Aribi A, et al. MIPSS70+ v2.0 predicts long-term survival in myelofibrosis after allogeneic HCT with the Flu/Mel conditioning regimen. Blood Adv. 2019;3:83–95.
Tamari R, Rapaport F, Zhang N, McNamara C, Kuykendall A, Sallman DA, et al. Impact of high-molecular-risk mutations on transplantation outcomes in patients with myelofibrosis. Biol Blood Marrow Transpl. 2019;25:1142–51.
Murthy GSG, Kim S, Estrada-Merly N, Abid MB, Aljurf M, Assal A, et al. Association between the choice of the conditioning regimen and outcomes of allogeneic hematopoietic cell transplantation for myelofibrosis. Haematologica. 2023;108:1900–8.
Holmstrom MO, Riley CH, Svane IM, Hasselbalch HC, Andersen MH. The CALR exon 9 mutations are shared neoantigens in patients with CALR mutant chronic myeloproliferative neoplasms. Leukemia. 2016;30:2413–6.
Tvorogov D, Thompson-Peach CAL, Fosselteder J, Dottore M, Stomski F, Onnesha SA, et al. Targeting human CALR-mutated MPN progenitors with a neoepitope-directed monoclonal antibody. EMBO Rep. 2022;23:e52904.
Handlos Grauslund J, Holmstrom MO, Jorgensen NG, Klausen U, Weis-Banke SE, El Fassi D, et al. Therapeutic cancer vaccination with a peptide derived from the calreticulin exon 9 mutations induces strong cellular immune responses in patients with CALR-mutant chronic myeloproliferative neoplasms. Front Oncol. 2021;11:637420.
Gigoux M, Holmstrom MO, Zappasodi R, Park JJ, Pourpe S, Bozkus CC, et al. Calreticulin mutant myeloproliferative neoplasms induce MHC-I skewing, which can be overcome by an optimized peptide cancer vaccine. Sci Transl Med. 2022;14:eaba4380.
Plo I, Nakatake M, Malivert L, de Villartay JP, Giraudier S, Villeval JL, et al. JAK2 stimulates homologous recombination and genetic instability: potential implication in the heterogeneity of myeloproliferative disorders. Blood. 2008;112:1402–12.
Marty C, Lacout C, Droin N, Le Couedic JP, Ribrag V, Solary E, et al. A role for reactive oxygen species in JAK2 V617F myeloproliferative neoplasm progression. Leukemia. 2013;27:2187–95.
Tefferi A, Lasho TL, Finke CM, Knudson RA, Ketterling R, Hanson CH, et al. CALR vs JAK2 vs MPL-mutated or triple-negative myelofibrosis: clinical, cytogenetic and molecular comparisons. Leukemia. 2014;28:1472–7.
Christopeit M, Badbaran A, Zabelina T, Zeck G, Fehse B, Ayuk F, et al. Similar outcome of calreticulin type I and calreticulin type II mutations following RIC allogeneic haematopoietic stem cell transplantation for myelofibrosis. Bone Marrow Transpl. 2016;51:1391–3.
Author information
Authors and Affiliations
Contributions
JCHB, DJE, GB, NP, TC, IYA and DMcL were involved in study design, analysis and writing of the paper. LK was the data manager. All other co-authors contributed data to the study, critically revised the paper and approved the submitted and final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This retrospective study was approved by the Chronic Malignancies Working Party (CMWP) of EBMT.
Informed consent
Informed consent for inclusion in the EBMT registry was obtained in all patients.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hernández-Boluda, J.C., Eikema, DJ., Koster, L. et al. Allogeneic hematopoietic cell transplantation in patients with CALR-mutated myelofibrosis: a study of the Chronic Malignancies Working Party of EBMT. Bone Marrow Transplant 58, 1357–1367 (2023). https://doi.org/10.1038/s41409-023-02094-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-02094-1
This article is cited by
-
CALR mutations possess unique prognostic relevance in myelofibrosis—before and after transplant
Bone Marrow Transplantation (2023)