Abstract
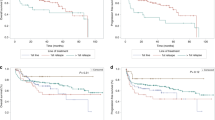
Thiotepa/carmustine (TT-BCNU) is a commonly used autologous transplant (ASCT) conditioning regimen for primary DLBCL of the CNS (PCNSL). The total thiotepa dose varies among TT-BCNU recipients, with some centers administering a total dose of 20 mg/kg, while others using 10 mg/kg. We retrospectively assessed the impact of thiotepa dose intensity on ASCT outcomes in 218 adult PCNSL patients who underwent a first ASCT with TT-BCNU conditioning and received either a total thiotepa dose of 10 mg/kg (TT-10 group; N = 90), or 20 mg/kg (TT-20 group; N = 128). The median follow-up of survivors was 22 months. The cumulative incidence of 1-year non-relapse mortality (NRM) for TT-10 and TT-20 cohorts were 6% (95%CI = 2–12%) vs. 4% (95%CI = 1–8%), respectively (p = 0.66). The 3-year cumulative incidence of relapse (15% vs. 13%; p = 0.67), progression-free survival (PFS) (71% vs. 80%; p = 0.25) and overall survival (OS) (79% vs. 83%; p = 0.56) were similar in the TT-10 and TT-20 groups, respectively. On multivariate analysis compared to TT-10, the TT-20 cohort was not associated with significantly different risk of NRM (Hazard ration [HR] = 0.77; p = 0.64), relapse/progression (HR = 0.87; p = 0.74), PFS (HR = 0.80; p = 0.48) or OS (HR = 1.10; p = 0.80). In conclusion thiotepa dose-intensity in TT-BCNU conditioning does not impact ASCT outcomes of PCNSL patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Glass J, Won M, Schultz CJ, Brat D, Bartlett N, Suh J. et al. Phase I and II Study of Induction Chemotherapy With Methotrexate, Rituximab, and Temozolomide, Followed By Whole-Brain Radiotherapy and Postirradiation Temozolomide for Primary CNS Lymphoma: NRG Oncology RTOG 0227. J Clin Oncol. 2016;34:1620–5. https://doi.org/10.1200/jco.2015.64.8634.
Ferreri AJ, Cwynarski K, Pulczynski E, Ponzoni M, Deckert M, Politi L, et al. Chemoimmunotherapy with methotrexate, cytarabine, thiotepa, and rituximab (MATRix regimen) in patients with primary CNS lymphoma: results of the first randomisation of the International Extranodal Lymphoma Study Group-32 (IELSG32) phase 2 trial. Lancet Haematol. 2016;3:e217–27. https://doi.org/10.1016/s2352-3026(16)00036-3.
Ferreri AJM, Cwynarski K, Pulczynski E, Fox C, Schorb E, Rosee P, et al. Whole-brain radiotherapy or autologous stem-cell transplantation as consolidation strategies after high-dose methotrexate-based chemoimmunotherapy in patients with primary CNS lymphoma: results of the second randomisation of the International Extranodal Lymphoma Study Group-32 phase 2 trial. Lancet Haematol. 2017;4:e510–e523. https://doi.org/10.1016/s2352-3026(17)30174-6.
Ferreri AJM, Cwynarski K, Pulczynski E, Fox C, Schorb E, Celico C, et al. Long-term efficacy, safety and neurotolerability of MATRix regimen followed by autologous transplant in primary CNS lymphoma: 7-year results of the IELSG32 randomized trial. Leukemia. 2022;36:1870–8. https://doi.org/10.1038/s41375-022-01582-5.
Batchelor T, Giri S, Ruppert AS, Bartlett N, His E, Cheson B, et al. Myeloablative versus non-myeloablative consolidative chemotherapy for newly diagnosed primary central nervous system lymphoma: Results of CALGB 51101 (Alliance). J Clin Oncol. 2021;39:7506–7506. https://doi.org/10.1200/JCO.2021.39.15_suppl.7506.
Illerhaus G, Ferreri AJM, Binder M, Borchmann P, Hasenkamp J, Stilgenbauer S, et al. Effects on Survival of Non-Myeloablative Chemoimmunotherapy Compared to High-Dose Chemotherapy Followed By Autologous Stem Cell Transplantation (HDC-ASCT) As Consolidation Therapy in Patients with Primary CNS Lymphoma—Results of an International Randomized Phase III Trial (MATRix/IELSG43). Blood. 2022;140:LBA-3–LBA-3. https://doi.org/10.1182/blood-2022-171733.
Steffanoni S, Calimeri T, Marktel S, Nitti R, Foppoli M, Ferreri AJM. Diagnosis and Treatment Using Autologous Stem-Cell Transplantation in Primary Central Nervous System Lymphoma: A Systematic Review. Cancers (Basel). 2023;15 https://doi.org/10.3390/cancers15020526.
Epperla N, Reljic T, Chowdhury SM, Ferreri AJM, Kumar A, Hamadani M. Autologous hematopoietic cell transplantation versus whole-brain radiotherapy consolidation in primary central nervous system lymphoma: A systematic review and meta-analysis. Hematol Oncol. 2023;41:88–96. https://doi.org/10.1002/hon.3083.
Houillier C, Taillandier L, Dureau S, Lamy T, Laadhari M, Chinot O. et al. Radiotherapy or Autologous Stem-Cell Transplantation for Primary CNS Lymphoma in Patients 60 Years of Age and Younger: Results of the Intergroup ANOCEF-GOELAMS Randomized Phase II PRECIS Study. J Clin Oncol. 2019;37:823–33. https://doi.org/10.1200/jco.18.00306.
Scordo M, Wang TP, Ahn KW, Chen Y, Ahmed S, Awan F et al. Outcomes Associated With Thiotepa-Based Conditioning in Patients With Primary Central Nervous System Lymphoma After Autologous Hematopoietic Cell Transplant. JAMA Oncol. 2021;7:993–1003. https://doi.org/10.1001/jamaoncol.2021.1074.
Khurana A, Micallef IN, LaPlant BR, O’Neill B, Habermann T, Ansell S, et al. Outcomes of Autologous Stem Cell Transplant Consolidation in Primary Central Nervous System Lymphoma: A Mayo Clinic Experience. Biol Blood Marrow Transplant. 2020;26:2217–22. https://doi.org/10.1016/j.bbmt.2020.08.012.
Web address: https://cibmtr.org/Manuscript/a020h00001HH9E5AAL/P-5398. Last Assessed 6/29/2023.
Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz L, Zucca E, et al. Recommendations for Initial Evaluation, Staging, and Response Assessment of Hodgkin and Non-Hodgkin Lymphoma: The Lugano Classification. J Clin Oncol. 2014;32:3059–67. https://doi.org/10.1200/jco.2013.54.8800.
Commenges D, Andersen PK. Score test of homogeneity for survival data. Lifetime Data Anal. 1995;1:145–56. https://doi.org/10.1007/bf00985764.
Zhang X, Loberiza FR, Klein JP, Zhang MJ. A SAS macro for estimation of direct adjusted survival curves based on a stratified Cox regression model. Comput Methods Programs Biomed. 2007;88:95–101. https://doi.org/10.1016/j.cmpb.2007.07.010.
Zhang X, Zhang M-J. SAS macros for estimation of direct adjusted cumulative incidence curves under proportional subdistribution hazards models. Comput Methods Programs Biomed. 2011;101:87–93. https://doi.org/10.1016/j.cmpb.2010.07.005.
Illerhaus G, Marks R, Ihorst G, Guttenberger R, Ostertag C, Derigs G. et al. High-dose chemotherapy with autologous stem-cell transplantation and hyperfractionated radiotherapy as first-line treatment of primary CNS lymphoma. J Clin Oncol. 2006;24:3865–70. https://doi.org/10.1200/jco.2006.06.2117.
Phillips AA, Smith DA. Health Disparities and the Global Landscape of Lymphoma Care Today. Am Soc Clin Oncol Educ Book. 2017;37:526–34. https://doi.org/10.1200/edbk_175444.
Shenoy PJ, Malik N, Nooka A, Sinha R, Ward K, Brawley O et al. Racial differences in the presentation and outcomes of diffuse large B-cell lymphoma in the United States. Cancer. 2011;117:2530–40. https://doi.org/10.1002/cncr.25765.
Tao L, Foran JM, Clarke CA, Gomez SL, Keegan TH. Socioeconomic disparities in mortality after diffuse large B-cell lymphoma in the modern treatment era. Blood. 2014;123:3553–62. https://doi.org/10.1182/blood-2013-07-517110.
Curry LD, Munker R, Li N, Yan D, Pryor P, Nozad S, et al. Performance status, comorbidities, and cycles of methotrexate exert the greatest influence on outcomes of primary and secondary CNS lymphomas: the Lexington experience. Ann Hematol. 2023;102:141–54. https://doi.org/10.1007/s00277-022-05018-z.
Roetzer T, Furtner J, Gesperger J, Seebrecht L, Bandke D, Brada M, et al. Sex-Specific Differences in Primary CNS Lymphoma. Cancers (Basel). 2020;12. https://doi.org/10.3390/cancers12061593.
Acknowledgements
This dataset was collected by the Center for International Blood and Marrow Transplant Research which is supported primarily by the Public Health Service U24CA076518 from the National Cancer Institute (NCI), the National Heart, Lung and Blood Institute (NHLBI) and the National Institute of Allergy and Infectious Diseases (NIAID); 75R60222C00011 from the Health Resources and Services Administration (HRSA); N00014-21-1-2954 and N00014-23-1-2057 from the Office of Naval Research; the Medical College of Wisconsin and the National Marrow Donor Program.
Author information
Authors and Affiliations
Contributions
Conception and design: MH. Financial support: None. Collection and assembly of data: FX, KWA, MK, and MH. Data analysis: FX, KWA. Interpretation: All authors. Paper writing: First draft prepared by SA and MH and edited by all the authors. Final approval of paper: All authors.
Corresponding author
Ethics declarations
Competing interests
MH reports Consultancy: Incyte Corporation, MorphoSys, SeaGen, Gamida Cell, Novartis, Legend Biotech, Kadmon, ADC Therapeutics; Omeros, CRISPR, Genmab, Kite, BMS, Caribou, Abbvie. Speaker’s Bureau: Sanofi Genzyme, AstraZeneca, BeiGene, ADC Therapeutics, Kite. DMC: Myeloid Therapeutics, Inc, Genentech. MS served as a paid consultant for McKinsey & Company, Angiocrine Bioscience, Inc., and Omeros Corporation; received research funding from Angiocrine Bioscience, Inc., and Omeros Corporation; served on ad hoc advisory boards for Kite—A Gilead Company; and received honoraria from i3Health and Medscape for CME-related activity. CSS has served as a paid consultant: Juno Therapeutics, Sanofi-Genzyme, Spectrum Pharmaceuticals, Novartis, Genmab, Precision Biosciences, Kite/a Gilead Company, Celgene/BMS, Gamida Cell, Karyopharm Therapeutics, Ono Pharmaceuticals, MorphoSys, CSL Behring, Syncopation Life Sciences, CRISPR Therapeutics and GSK. He has received research funds for clinical trials from: Juno Therapeutics, Celgene/BMS, Bristol-Myers Squibb, Precision Biosciences, Actinium Pharmaceuticals, Sanofi-Genzyme and NKARTA. FTA has provided consultancy to: Genentech, Astrazeneca, Abbvie, Janssen, Pharmacyclics, Gilead sciences, Kite pharma, Celgene, Karyopharm, MEI Pharma, Verastem, Incyte, Beigene, Johnson and Johnson, Dava Oncology, BMS, Merck, Cardinal Health, ADCT therapeutics, Epizyme, Caribou Biosciences, Cellecter Bisosciences, Loxo Oncology, Adaptive Biotechnologies, and received research funding from Pharmacyclics.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arshad, S., Fang, X., Ahn, K.W. et al. Impact of thiotepa dose-intensity in primary diffuse large B-cell lymphoma of the central nervous system undergoing autologous hematopoietic cell transplant with thiotepa/carmustine conditioning. Bone Marrow Transplant 58, 1203–1208 (2023). https://doi.org/10.1038/s41409-023-02071-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-02071-8