Abstract
Involvement of lower gastrointestinal tract (LGI) occurs in 60% of patients with graft-versus-host-disease (GVHD). Complement components C3 and C5 are involved in GVHD pathogenesis. In this phase 2a study, we evaluated the safety and efficacy of ALXN1007, a monoclonal antibody against C5a, in patients with newly diagnosed LGI acute GVHD receiving concomitant corticosteroid. Twenty-five patients were enrolled; one was excluded from the efficacy analysis based upon negative biopsy. Most patients (16/25, 64%) had acute leukemia; 52% (13/25) had an HLA-matched unrelated donor; and 68% (17/25) received myeloablative conditioning. Half the patients (12/24) had a high biomarker profile, Ann Arbor score 3; 42% (10/24) had high-risk GVHD per Minnesota classification. Day-28 overall response was 58% (13/24 complete response, 1/24 partial response), and 63% by Day-56 (all complete responses). Day-28 overall response was 50% (5/10) in Minnesota high-risk and 42% (5/12) in high-risk Ann Arbor patients, increasing to 58% (7/12) by Day-56. Non-relapse mortality at 6-months was 24% (95% CI 11–53). The most common treatment-related adverse event was infection (6/25, 24%). Neither baseline complement levels (except for C5), activity, nor inhibition of C5a with ALXN1007 correlated with GVHD severity or responses. Further studies are needed to evaluate the role of complement inhibition in GVHD treatment.
Similar content being viewed by others
Introduction
Acute graft-versus-host disease (aGVHD) is one of the most common complications of allogeneic hematopoietic cell transplantation (HCT) [1,2,3], occurring in up to 60–75% of patients. GVHD develops when donor T cells recognize the recipient as foreign, initiating an immune response that may involve a variety of organs. Involvement of the lower gastrointestinal (LGI) tract is observed in ~60% of patients with aGVHD [4].
The standard first-line therapy for aGVHD is high-dose corticosteroids, although only 25–40% of patients achieve durable responses [5]. LGI aGVHD is less responsive to steroids than other organs [6, 7]; and ~75% of patients with stage 3 and 4 LGI GVHD are steroid-refractory [6]. The addition of immunosuppressants to steroid therapy, including mycophenolate mofetil [8, 9]; pentostatin [9], denileukin diftitox [9], etanercept [9], daclizumab [10], anti-interleukin-2 receptor monoclonal antibody [11], infliximab [12], or anti-thymocyte globulin [13], have not shown additional benefits in multiple randomized trials. Novel treatments for LGI aGVHD are therefore needed.
The long-held view is that alloreactive donor cytotoxic lymphocytes and host antigen-presenting cells (APC) are necessary and sufficient in the pathophysiology of aGVHD [14]; recently, the complement cascade has also been implicated. The complement system can be activated via three independent pathways – classical, alternative and lectin – all of which generate C3 convertase which cleaves C3 into C3a and C3b. The latter binds other components to form C5 convertase, which cleaves C5 into C5b and C5a. C5a is a potent anaphylatoxin that recruits phagocytes to the site of inflammation [15].
Multiple preclinical studies have shown an association between complement components C3 [16, 17] and C5 [16, 18, 19] and GVHD, but this has not been systematically investigated in clinical trials. We previously found C3 deposition (which correlates with C5 activation [20, 21] in the skin and lip biopsies of patients with cutaneous GVHD and showed that the inhibition of C3 activation decreased proliferation of CD4+ and CD8+ T cells and inhibited Th1/Th17 polarization in activated human CD4+ T cells [22]. Other preclinical studies suggest that antigen-presenting cells synthesize and secrete complement activation products C3a and C5a locally, which provide costimulatory signals to effector T cells that express C3a receptor (C3aR) and C5a receptor (C5aR) on their surfaces [17, 23,24,25]. Antagonism of C3aR and C5aR dampens T cell alloresponses [25, 26] and induces functional human Foxp3+ regulatory T cells [18, 27], which have a protective role against GVHD [28]. Inhibition of C5a has been shown to inhibit GVHD in T-cell C5aR knockout mice and mice treated with C5a inhibitors [18, 25, 29, 30].
ALXN1007 (Alexion, AstraZeneca Rare Disease, Boston, MA, USA) is a recombinant humanized monoclonal antibody that binds to C5a and its metabolite C5adesArg. Preclinical data and data from phase 1 studies in healthy volunteers suggest that ALXN1007 is highly specific for its epitope, is a potent antagonist of C5a-mediated signaling, and depletes levels of circulating C5a (data on file). ALXN1007 binds to C5a and C5adesArg with a high affinity (affinity dissociation constant [KD] ≈ 60 pM) and to the native full-length C5 with a lower affinity (KD ≈ 5 nM) (data on file). Thus, ALXN1007 may function as a complete antagonist of C5a and C5adesArg and a partial antagonist of C5 in vivo. In this phase 2a study, we assess the safety, tolerability, pharmacokinetics (PK)/pharmacodynamics (PD), and efficacy of ALXN1007 in patients newly diagnosed with LGI aGVHD.
Patients and methods
This was an open-label phase 2a, multicenter, non-randomized study designed to evaluate the safety, tolerability, PK, PD, and efficacy of ALXN1007 in patients with LGI aGVHD (Clinicaltrials.gov registry number: NCT02245412). Patients ≥18 years of age with LGI aGVHD occurring within 180 days of HCT and receiving systemic corticosteroids for ≤3 days were enrolled. Gastrointestinal (GI) biopsies were performed within 7 days of screening, but the biopsy results were not required before ALXN1007 treatment. Patients receiving other systemic treatments for aGVHD, with absolute neutrophil count ≤ 500/μL, signs of chronic GVHD, active uncontrolled infection, history of HIV, hepatitis B or C, relapsed or persistent malignancy, recipient of donor lymphocyte infusion, unresolved hepatic sinusoidal obstruction syndrome, or creatinine clearance <40 mL/min/1.73 m2 were excluded from the study. This study was conducted in accordance with the Declaration of Helsinki and all participants provided written informed consent prior to participation. The research was approved by the relevant institutional review boards or ethics committees.
Study drug dosing schedule
The study included three sequential cohorts. The first cohort (n = 17) received ALXN1007 10 mg/kg intravenously (IV) once weekly (QW) for 8 weeks. An interim PK/PD modeling performed in 10 patients indicated that ALXN1007 clearance was about 30% higher than in healthy volunteers, likely due to protein-losing enteropathy in GI GVHD patients [31, 32] that can lead to loss of therapeutic proteins [33, 34]. Only 10/15 patients had maximal suppression of C5a (level below the limit of quantification) lasting for a week after the first dose. Ninety percent inhibitory concentration (IC90) for C5a suppression was at least 15-fold higher than in healthy volunteers, presumably due to a higher C5a formation rate. Simulation-based PK/PD modeling indicated that at a dose of 20 mg/kg twice weekly (BIW), trough concentrations for ALXN1007 would be at the lower limit of the 90% confidence interval (CI) and be above the IC90 of C5a suppression. A second cohort receiving ALXN1007 20 mg/kg IV QW for 8 weeks (n = 6) was added. After reviewing the safety and tolerability data on the first 3 patients in cohort 2 by Day 28 and based on the modeled PK/PD data from both cohorts, a third cohort of ALXN1007 20 mg/kg IV BIW for 8 weeks was added. The study planned for enrollment of up to 36 patients, with a maximum of 18 patients in cohort 1 and 3–6 patients in each subsequent cohort (maximum dose 40 mg/kg/week for 8 weeks). After 25 patients were enrolled (17 in cohort 1, 6 in cohort 2, and 2 in cohort 3), the study was terminated early at the Sponsor’s discretion.
Drug administration, concurrent medications, and supportive care
ALXN1007 solution in 0.9% sodium chloride was administered via an IV infusion over 60 ± 10 min (10 mg/kg dose) or 120 ± 10 min (20 mg/kg dose). All patients received corticosteroids at a suggested starting dose of prednisone (or methylprednisolone equivalent) 2 mg/kg/day, with a taper as per institutional practices. Before starting ALXN1007, all patients were required to receive prophylaxis against encapsulated organisms (including N. meningitidis), which was continued until six weeks after the last dose. Other prophylactic antimicrobials as well as pre-emptive monitoring and treatment for cytomegalovirus (CMV) followed institutional practices.
Endpoints
The primary safety endpoint was the incidence and severity of adverse events (AEs), graded as per the National Cancer Institute Common Terminology Criteria for Adverse Events (version 4.03). The primary efficacy endpoint was the LGI aGVHD overall response rate by Day 28, defined as the proportion of patients achieving either complete (CR) or partial response (PR). Secondary efficacy endpoints included LGI aGVHD overall response rate, and CR, PR, no response (NR) by Day 56. Responses [35] and staging [36] were assessed as per standard criteria. Non-relapse mortality, progression-free survival, and overall survival at 1 year were also evaluated. The protocol was written prior to the development of the consortium criteria for aGVHD [37] and therefore, used the accepted criteria at the time [36]. Also, apart from the ability to estimate stool output based on number of episodes per day and the inclusion of severe pain/ frank blood as stage 4, staging between these two methods are comparable. Using the consortium criteria for aGVHD may in fact result in up staging this population and thus does not distract from the findings as presented. Patients who received second-line therapies were considered treatment failures. Response to additional lines of therapy were not collected in this multicenter trial.
Correlative analysis
Pharmacokinetic parameters included Cmax, Ctrough, time to maximum observed concentration in plasma (tmax), area under the plasma concentration, time curve from time 0 to 168 h (AUC0-168), and apparent linear phase half-life (t½). Pharmacodynamic analyses included changes in C5 and C5a levels from baseline determined by an enzyme-linked immunosorbent (ELISA) assay. A limited number of samples were also assayed for complement activity using the 50% hemolytic complement (CH50) assay, which measured the capacity of the patient serum to lyse chicken red blood cells. The assay is sensitive to reduction of any complement component, and thus a marker of functional activity of both classical and terminal pathways. Undetectable CH50 activity was defined as CH50 ≤ 20% of normal values [38]. Plasma for three GVHD-related biomarkers – soluble tumor necrosis factor receptor 1 (sTNFR1), suppressor of tumorigenicity 2 (ST2), and regenerating islet-derived protein 3 alpha (REG3α) were also collected to determine baseline Ann Arbor (AA) scores [39]. Patients with AA scores 1 and 2 were categorized as a standard-risk and an AA score of 3 as high-risk.
Statistical analysis
A stopping rule for excess mortality by Day 56 was applied after every six patients. A mortality rate of 40% by Day 56 was considered unacceptable as compared to the historical rate of ~20%. The study was to be stopped at an interim evaluation (t) if the number of deaths was ≥Xt, as detailed in Supplementary Table S1. Patients who received at least 1 dose of ALXN1007 were included in the safety analyses. Efficacy analyses were done on a per-protocol basis, and patients with biopsy-confirmed LGI GVHD who received at least 1 dose of ALXN1007 were included.
Non-compartmental PK methods were used to estimate parameters of interest. Descriptive analyses were performed to summarize baseline characteristics. All outcomes were measured from the first day of ALXN1007 administration. The cumulative incidence of non-relapse mortality was determined using relapse as a competing risk. Overall survival was estimated using the Kaplan–Meier method. Competing risk regression analysis was used to evaluate predictors of response by Day 28 and 56 using relapse/progression of the underlying malignancy at Day 28 and 56 as competing risk. Statistical analyses were performed using STATA 14 (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp L) and significance was set at P ≤ 0.05.
Results
Patient characteristics
Between November 14, 2014 and December 6, 2016, 36 patients were screened (Fig. 1). Eleven patients failed screening (positive Clostridium difficile test [n = 4], participation in another trial [n = 2], no corticosteroid treatment [n = 2], patient unwilling to undergo biopsy to confirm GVHD [n = 2], other [n = 1]). Twenty-five patients met the eligibility criteria and were enrolled (safety analysis set). One patient in cohort 1 was excluded from the efficacy analysis (n = 24) after receiving one dose of ALXN1007; GVHD was not confirmed on biopsy.
A total of 36 patients were screened for eligibility. Eleven were excluded mainly for not meeting inclusion criteria (n = 10). A total of 25 patients were enrolled and received treatment. Eight discontinued treatment due to physician decision (2), patient withdrawal (2), GVHD not confirmed by biopsy (1), death (2), and other (1). A total of 24 of the 25 enrolled patients were included in efficacy analysis with 1 patient removed from analysis after receiving 1 dose and biopsy result confirming an alternative diagnosis.
Overall, the median age was 60 years (range, 25–72) and 56% of patients were male (Table 1). Most patients had acute myeloid leukemia (10/25, 40%) or acute lymphocytic leukemia (6/25, 24%). About half of the patients (13/25, 52%) had a human leukocyte antigen matched unrelated donor. Sixty-eight percent of patients (17/25) had received myeloablative conditioning and 72% (18/25) a peripheral blood graft. Twelve patients received calcineurin inhibitor and mycophenolate mofetil-based GVHD prophylaxis. About half had stage 3–4 LGI GVHD (10/25) and AA score 3 (12/25), and 42% (10/24) had high-risk GVHD per Minnesota classification [40]. The median time from HCT to LGI GVHD was 48 days (range, 16–184). The median follow-up was 9.2 months (range 0.2–12.7).
Safety/toxicity
Sixty-eight percent (17/25; cohort 1 [n = 12], cohort 2 [n = 3], cohort 3 [n = 2]) completed 8 weeks of treatment. No scheduled infusions were interrupted. All patients experienced at least one AE. AEs were considered possibly ALXN1007-related in 12 patients (48%). The most frequent ALXN1007-related AE was infection (6/25, 24%), including CMV (n = 1), Epstein–Barr virus (n = 3) and bronchopulmonary aspergillosis (n = 1). Two patients experienced three ALXN1007-related serious AES (two respiratory syncytial virus infections, one influenza-like illness) (Table 2). There were no ALXN1007-related deaths. Ten patients (40%) died during the study period at a median of 110 days (range, 22–316), due to underlying disease relapse (n = 4), GVHD (n = 4), or other causes (one aspiration pneumonia-related respiratory failure, and one ascites).
GVHD response and other outcomes
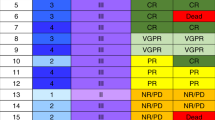
In the primary efficacy analysis, 14/24 patients (58%) had an overall response with 13 (54%) CR and 1 (4%) PR at Day 28. Seven patients (29%) had NR and 3 (13%) had GVHD progression. All patients (100%) who attained CR by Day 28 had a durable response and remained in CR at Day 56. Additionally, two patients with NR by Day 28 attained CR by Day 56. Thus, Day 56 overall response was 63% (15/24) with all 15 patients having CR (Table 3).
Day 28 overall response was 50% (4/10 CR, 1/10 PR) among Minnesota high-risk patients and 50% (4/10 CR, 1/10 PR) patients with stage 3–4 LGI aGVHD. In patients with high-risk AA score, the overall response was 42% (5/12, all CR) at Day 28 which increased to 58% (7/12, all CR) by Day 56. Among patients with standard-risk AA, 80% had an overall response (7/10 CR, 1/10 PR) by Day 28 and 70% (7/10 CR, 0/10 PR) by Day 56 (Supplementary Table S2). In univariate analysis (including age, gender-mismatch, donor type, graft source, GVHD prophylaxis, treatment cohort, LGI GVHD stage, AA score, baseline C5 and C5a levels), we found no significant predictors of overall response except baseline C5 (Supplementary Table S3). Patients with baseline C5 levels lower than the median had a superior OR rate as compared to those with the higher levels (80% vs 33%, P = 0.04), at Day 28 but not at Day 56. Baseline C5a level had no impact on the GVHD response. The median baseline C5 level in patients who achieved CR or PR at day 28 (n = 11) was 121 µg/mL (range 81.3–561) vs 143 µg/mL (range 81.4–613) in those who did not (n = 8) (Fig. 2). The median baseline C5a level in patients who achieved CR or PR at day 28 (n = 11) was 0.68 ng/mL (range 0.3–2.4) vs 0.68 ng/mL (range 0.2–3.3) in those who did not (n = 9) (Fig. 2).
The cumulative incidence of non-relapse mortality by Day 180 was 24% (95% CI, 11–53). One year post-HCT, the estimated progression-free survival was 45% (95% CI, 22–65), overall survival was 49% (95% CI, 25–69), and non-relapse mortality was 31% (95% CI, 12–52) (Fig. 3 and Supplementary Table S4).
PK, PD, and correlative analyses
Plasma free ALXN1007 exposure increased with increasing dose from 10 to 20 mg/kg QW (AUC ratio = 2.0, Cmax ratio = 2.0) as predicted by modeling. The t1/2 of ALXN1007 was 84 h (cohort 1) and 172 h (cohort 2) (Supplementary Table S5).
At baseline, 9/12 (75%) patients had detectable complement activity (CH50 > 20%; range 28.7–93.8%). After one dose, 5/7 tested patients achieved complement activity (CH50) < 20% within 24 h of infusion. All three biomarkers (sTNFR1, ST2 and REG3α) were elevated at baseline in 22 patients (data not shown). The median baseline free plasma C3, C4, and C5 levels did not differ significantly by the LGI aGVHD severity (Supplementary Table S6).
The median baseline free plasma C5a level (n = 20) was 0.68 (range, 0.2–3.3) ng/mL. Free plasma C5a inhibition increased with 20 mg/kg QW compared to 10 mg/kg QW dose. By the end of the first infusion, C5a was undetectable in 21/23 (91%) patients; one patient each in cohorts 1 and 2 had detectable C5a. By Day 7, 18/23 (78%) patients had undetectable C5a; it was detectable in five patients (all in cohort 1), of whom four previously had an undetectable C5a level. In cohort 3, one patient had high baseline C5a (3.29 ng/mL) and needed two doses to make C5a undetectable. The second patient in cohort 3 had a low baseline C5a value (0.938 ng/mL), which became and remained undetectable throughout the dosing period. Among patients with undetectable C5a by Day 7 (18/23), 10 (56%) attained CR or PR by Day 28. The five patients with detectable C5a (all cohort 1) attained CR or PR by Day 28.
Discussion
This prospective phase 2a study demonstrated that ALXN1007 is safe and potentially effective when added to systemic corticosteroids for the treatment of LGI aGVHD. Patients on treatment with ALXN1007 and corticosteroids experience a similar proportion of treatment-related AEs as that reported in patients with aGVHD receiving corticosteroid treatment alone (48% vs ~50% [41]. The most frequent AEs related to ALXN1007 were infections (n = 6, 24%), mostly viral, including CMV (n = 1) and Epstein–Barr virus (n = 3), and one bronchopulmonary aspergillosis. The safety of ALXN1007 is further supported by the 6-month non-relapse mortality rate, which was 24.0% in our study that included predominantly patients with an AA score 2 or 3 (a group with a predicted non-relapse mortality rate of 27% and 46%, respectively) [39].
Published data suggest that only about half of the patients with grade II-IV aGVHD respond to steroids [7,8,9, 42, 43], and that patients with LGI aGVHD are even less likely to respond, with an expected response rate of about 40% [7]. Generally, only about 25% of the patients with stage 3–4 LGI aGVHD respond by Day 14 of steroids and another 25% require additional therapy to attain response. About half of those who do attain a response will eventually have a flare of GVHD [6]. The overall response by Day 28 in our study was 58% and CRs at Day 28 were sustained through Day 56 in all patients (13/13). Overall response by Day 28 was 50% (5/10) in patients with stage 3–4 LGI aGVHD and 50% (5/10) in Minnesota high-risk group, slightly higher than the predicted overall response of 44% [40]. Comparable to other upfront trials [44], the number of patients with stage 3–4 LGI aGVHD in our study was 10/25. Due to the relatively small sample size, the day 28 CR (50%) needs to be interpreted cautiously in comparison to the published response rate for high risk acute GVHD (~45%). Similarly, as compared to the predicted CR rate of 25–30% in patients with high-risk AA score 3 [39], 40% (4/10) in our study achieved a CR by Day 28 and 56. These results are encouraging considering prior data suggesting a lack of durable responses in most patients with LGI aGVHD. For instance, it has been previously been reported that only 13% of patients with AA scores 3 exhibit a response at 6-months [39]. Higher responses (75% by Day 28) were reported in a trial evaluating natalizumab, an alpha integrin monoclonal antibody [44].
We prospectively examined the role of complement and its activity in patients with LGI aGVHD – a concept that until now has not been studied in a clinical setting, despite a multitude of preclinical data suggesting that targeting C3 or C5 complement components may ameliorate GVHD [17,18,19, 22,23,24,25, 27,28,29]. Focal or diffuse C4d deposition has been noted in colonic biopsies of patients with acute [45] or chronic [45, 46] GVHD [45]. One study noted activation of classical complement pathway post-HCT in 44% of the patients, as measured by at least 50% reduction in C3 and C4 levels, which correlated with the development of GI GVHD [47]. In contrast, and corroborating data from other studies [48, 49], a majority of patients in our study had normal C3 (17/24, 71%) and C4 (20/24, 83%) levels at baseline and detectable complement activity (CH50 > 20%; 9/12 [75%]). This suggests that systemic complement activation is unlikely in the majority of patients with LGI aGVHD, although, as acute phase reactants, the measured levels may not be a true reflection of complement pathway activity. Also, the baseline C3, C4 and C5 levels in our study did not correlate with the severity of LGI aGVHD. Low baseline C5 level was associated with improved responses at day 28 but not at day 56. Moreover, neither the baseline C5a level, nor C5a suppression to undetectable levels by ALXN1007 correlated with responses. Although C5a declined to undetectable levels in 21/23 patients (91%) immediately after the first dose, this inhibition was lost in 23% of patients by Day 7, all from cohort 1, suggesting that a higher dose was required to inhibit the ongoing production of C5a. In cohort 2, 83.3% of patients had undetectable C5a levels immediately after the first infusion sustained through 72 h post-infusion, and C5a was undetectable in all patients by Day 7. Yet, only 50% of patients had CR/PR by Day 28. No firm conclusions can be made from these findings, which should be interpreted with caution given a relatively small number of patients in these subgroups.
The poor correlation between C5a inhibition and GVHD response may be explained by several factors. Previous studies indicate that C5a can be generated in the absence of C3 by serine proteases such as thrombin, independent of general complement activation [50, 51], and also secreted locally by APCs, which provide costimulatory signals for effector T cells carrying C5a receptors [23, 24]. Studies in patients with inflammatory bowel disease provide further evidence for local complement activation at the luminal surface of the epithelium, which occurs partly due to mucosal synthesis of complement components [52,53,54,55,56]. Although we monitored systemic C5a levels, it is unclear how these correlate with locally produced C5a. Monitoring local complement components via novel fecal studies could provide a more specific analysis of the mucosal complement activity. Additionally, it is hypothetically possible that even low levels (below the detection limit of the assay; 0.156 ng/mL) of the potent anaphylatoxin C5a, may contribute to the ongoing inflammatory damage. Also, C5adesArg which also has signaling activity, although at a lower potency at both C5a receptors [57, 58], was not measured in this study. Therefore, it is possible that there is incomplete inhibition of C5adesArg in patients with LGI aGVHD treated with ALXN1007, and that false-positive C5a levels were detected using the ELISA assay [59]. Obtaining a false undetectable level is also possible due to the short half-life of C5a (<1 min) [60].
Conclusion
Overall, ALXN1007 was safe, well tolerated, and without any added risk of infections, non-relapse mortality or relapse of the underlying malignancy in patients with LGI aGVHD when ALXN1007 was given in combination with corticosteroids. The complete response rate of 63% by Day 56 for patients with LGI GVHD is encouraging and merits further study in controlled clinical trials. Systemic complement baseline levels (except C5), complement activity, and the inhibition of C5a with ALXN1007 did not correlate with GVHD severity or responses. Further studies examining the role of the complement pathway in the pathophysiology of aGVHD as well as examining targets of inhibition are justified.
Data availability
Alexion will consider requests for disclosure of clinical study participant-level data provided that participant privacy is assured through methods like data de-identification, pseudonymization, or anonymization (as required by applicable law), and if such disclosure was included in the relevant study informed consent form or similar documentation. Qualified academic investigators may request participant-level clinical data and supporting documents (statistical analysis plan and protocol) pertaining to Alexion-sponsored studies. Further details regarding data availability and instructions for requesting information are available in the Alexion Clinical Trials Disclosure and Transparency Policy at https://alexionclinicaltrials.com/Disclosure-and-Transparency-Policy. Link to Data Request Form (https://alexion.com/contact-alexion/medical-information).
References
Martin PJ, McDonald GB, Sanders JE, Anasetti C, Appelbaum FR, Deeg HJ, et al. Increasingly frequent diagnosis of acute gastrointestinal graft-versus-host disease after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transpl. 2004;10:320–7.
Nash RA, Antin JH, Karanes C, Fay JW, Avalos BR, Yeager AM, et al. Phase 3 study comparing methotrexate and tacrolimus with methotrexate and cyclosporine for prophylaxis of acute graft-versus-host disease after marrow transplantation from unrelated donors. Blood. 2000;96:2062–8.
Ratanatharathorn V, Nash RA, Przepiorka D, Devine SM, Klein JL, Weisdorf D, et al. Phase III study comparing methotrexate and tacrolimus (prograf, FK506) with methotrexate and cyclosporine for graft-versus-host disease prophylaxis after HLA-identical sibling bone marrow transplantation. Blood. 1998;92:2303–14.
McDonald GB. How I treat acute graft-versus-host disease of the gastrointestinal tract and the liver. Blood. 2016;127:1544–50.
Antin JH, Chen AR, Couriel DR, Ho VT, Nash RA, Weisdorf D. Novel approaches to the therapy of steroid-resistant acute graft-versus-host disease. Biol Blood Marrow Transpl. 2004;10:655–68.
Castilla-Llorente C, Martin PJ, McDonald GB, Storer BE, Appelbaum FR, Deeg HJ, et al. Prognostic factors and outcomes of severe gastrointestinal GVHD after allogeneic hematopoietic cell transplantation. Bone Marrow Transpl. 2014;49:966–71.
MacMillan ML, Weisdorf DJ, Wagner JE, DeFor TE, Burns LJ, Ramsay NK, et al. Response of 443 patients to steroids as primary therapy for acute graft-versus-host disease: comparison of grading systems. Biol Blood Marrow Transpl. 2002;8:387–94.
Bolanos-Meade J, Logan BR, Alousi AM, Antin JH, Barowski K, Carter SL, et al. Phase 3 clinical trial of steroids/mycophenolate mofetil vs steroids/placebo as therapy for acute GVHD: BMT CTN 0802. Blood. 2014;124:3221–7. quiz 3335
Alousi AM, Weisdorf DJ, Logan BR, Bolanos-Meade J, Carter S, Difronzo N, et al. Etanercept, mycophenolate, denileukin, or pentostatin plus corticosteroids for acute graft-versus-host disease: a randomized phase 2 trial from the Blood and Marrow Transplant Clinical Trials Network. Blood. 2009;114:511–7.
Lee SJ, Zahrieh D, Agura E, MacMillan ML, Maziarz RT, McCarthy PL Jr, et al. Effect of up-front daclizumab when combined with steroids for the treatment of acute graft-versus-host disease: results of a randomized trial. Blood. 2004;104:1559–64.
Cahn JY, Bordigoni P, Tiberghien P, Milpied N, Brion A, Widjenes J, et al. Treatment of acute graft-versus-host disease with methylprednisolone and cyclosporine with or without an anti-interleukin-2 receptor monoclonal antibody. A multicenter phase III study. Transplantation. 1995;60:939–42.
Couriel DR, Saliba R, de Lima M, Giralt S, Andersson B, Khouri I, et al. A phase III study of infliximab and corticosteroids for the initial treatment of acute graft-versus-host disease. Biol Blood Marrow Transpl. 2009;15:1555–62.
Cragg L, Blazar BR, Defor T, Kolatker N, Miller W, Kersey J, et al. A randomized trial comparing prednisone with antithymocyte globulin/prednisone as an initial systemic therapy for moderately severe acute graft-versus-host disease. Biol Blood Marrow Transpl. 2000;6:441–7.
Holtan SG, Pasquini M, Weisdorf DJ. Acute graft-versus-host disease: a bench-to-bedside update. Blood. 2014;124:363–73.
Janeway C, Travers P, Walport M. MJS immunobiology: the immune system in health and disease. 5 ed. New York: Garland Science; 2001.
Maus MV, Grupp SA, Porter DL, June CH. Antibody-modified T cells: CARs take the front seat for hematologic malignancies. Blood. 2014;123:2625–35.
Heeger PS, Lalli PN, Lin F, Valujskikh A, Liu J, Muqim N, et al. Decay-accelerating factor modulates induction of T cell immunity. J Exp Med. 2005;201:1523–30.
Wang Y, Lai P, Chen X, He C, Huang X, Geng S, et al. Attenuation of cGVHD by C5a/C5aR blockade is associated with increased frequency of Treg. Sci Rep. 2017;7:3603.
Chen X, Lai P, Wang Y, He C, Wu S, Huang X, et al. Emerging role of C5a/C5aR IL-17A axis in cGVHD. Am J Transl Res. 2018;10:2148–57.
Von Zabern I, Nolte R, Vogt W. Incompatibility between complement components C3 and C5 of guinea-pig and man, an indication of their interaction in C5 activation by classical and alternative C5 convertases. Scand J Immunol. 1979;9:69–74.
Vogt W, Schmidt G, Von Buttlar B, Dieminger L. A new function of the activated third component of complement: binding to C5, an essential step for C5 activation. Immunology. 1978;34:29–40.
Ma Q, Li D, Carreno R, Patenia R, Tsai KY, Xydes-Smith M, et al. Complement component C3 mediates Th1/Th17 polarization in human T-cell activation and cutaneous GVHD. Bone Marrow Transpl. 2014;49:972–6.
Lalli PN, Strainic MG, Yang M, Lin F, Medof ME, Heeger PS. Locally produced C5a binds to T cell-expressed C5aR to enhance effector T-cell expansion by limiting antigen-induced apoptosis. Blood. 2008;112:1759–66.
Strainic MG, Liu J, Huang D, An F, Lalli PN, Muqim N, et al. Locally produced complement fragments C5a and C3a provide both costimulatory and survival signals to naive CD4+ T cells. Immunity. 2008;28:425–35.
Cravedi P, Leventhal J, Lakhani P, Ward SC, Donovan MJ, Heeger PS. Immune cell-derived C3a and C5a costimulate human T cell alloimmunity. Am J Transpl. 2013;13:2530–9.
Nguyen H, Kuril S, Bastian D, Kim J, Zhang M, Vaena SG, et al. Complement C3a and C5a receptors promote GVHD by suppressing mitophagy in recipient dendritic cells. JCI Insight. 2018;3:e121697.
Strainic MG, Shevach EM, An F, Lin F, Medof ME. Absence of signaling into CD4(+) cells via C3aR and C5aR enables autoinductive TGF-beta1 signaling and induction of Foxp3(+) regulatory T cells. Nat Immunol. 2013;14:162–71.
Beres AJ, Drobyski WR. The role of regulatory T cells in the biology of graft versus host disease. Front Immunol. 2013;4:163.
Kwan WH, Hashimoto D, Paz-Artal E, Ostrow K, Greter M, Raedler H, et al. Antigen-presenting cell-derived complement modulates graft-versus-host disease. J Clin Invest. 2012;122:2234–8.
Nishimura J-I, DeOliveira D, Chen BJ, Kanakura Y, Rother RP, Chao NJ. Prevention of graft-versus-host disease in mouse model using anti-mouse C5 antibody. Blood. 2007;110:3245.
van der Meij BS, de Graaf P, Wierdsma NJ, Langius JA, Janssen JJ, van Leeuwen PA, et al. Nutritional support in patients with GVHD of the digestive tract: state of the art. Bone Marrow Transpl. 2013;48:474–82.
Papadopoulou A, Lloyd DR, Williams MD, Darbyshire PJ, Booth IW. Gastrointestinal and nutritional sequelae of bone marrow transplantation. Arch Dis Child. 1996;75:208–13.
Fasanmade AA, Adedokun OJ, Olson A, Strauss R, Davis HM. Serum albumin concentration: a predictive factor of infliximab pharmacokinetics and clinical response in patients with ulcerative colitis. Int J Clin Pharm Ther. 2010;48:297–308.
Chaudhury C, Brooks CL, Carter DC, Robinson JM, Anderson CL. Albumin binding to FcRn: distinct from the FcRn-IgG interaction. Biochemistry. 2006;45:4983–90.
MacMillan ML, DeFor TE, Weisdorf DJ. The best endpoint for acute GVHD treatment trials. Blood. 2010;115:5412–7.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant. 1995;15:825–8.
Harris AC, Young R, Devine S, Hogan WJ, Ayuk F, Bunworasate U, et al. International, multicenter standardization of acute graft-versus-host disease clinical data collection: a report from the Mount Sinai Acute GVHD International Consortium. Biol Blood Marrow Transpl. 2016;22:4–10.
Hillmen P, Hall C, Marsh JC, Elebute M, Bombara MP, Petro BE, et al. Effect of eculizumab on hemolysis and transfusion requirements in patients with paroxysmal nocturnal hemoglobinuria. N Engl J Med. 2004;350:552–9.
Levine JE, Braun TM, Harris AC, Holler E, Taylor A, Miller H, et al. A prognostic score for acute graft-versus-host disease based on biomarkers: a multicentre study. Lancet Haematol. 2015;2:e21–29.
MacMillan ML, Robin M, Harris AC, DeFor TE, Martin PJ, Alousi A, et al. A refined risk score for acute graft-versus-host disease that predicts response to initial therapy, survival, and transplant-related mortality. Biol Blood Marrow Transpl. 2015;21:761–7.
Mielcarek M, Furlong T, Storer BE, Green ML, McDonald GB, Carpenter PA, et al. Effectiveness and safety of lower dose prednisone for initial treatment of acute graft-versus-host disease: a randomized controlled trial. Haematologica. 2015;100:842–8.
Martin PJ, Schoch G, Fisher L, Byers V, Anasetti C, Appelbaum FR, et al. A retrospective analysis of therapy for acute graft-versus-host disease: initial treatment. Blood. 1990;76:1464–72.
Weisdorf D, Haake R, Blazar B, Miller W, McGlave P, Ramsay N, et al. Treatment of moderate/severe acute graft-versus-host disease after allogeneic bone marrow transplantation: an analysis of clinical risk features and outcome. Blood. 1990;75:1024–30.
Kekre N, Kim HT, Hofer J, Ho VT, Koreth J, Armand P, et al. Phase II trial of natalizumab with corticosteroids as initial treatment of gastrointestinal acute graft-versus-host disease. Bone Marrow Transpl. 2021;56:1006–12.
Cherry MA, Parekh H, Lerner M, Yu Z, Vesely S, Selby G, et al. The role of complement system in graft versus host disease. J Blood Disorders Transfusion. 2015;6:1–7.
Zhang PL, Wilkerson ML, Schworer CM. C4d staining is a valuable marker in identifying chronic GVHD in colonic biopsies following BMT. Bone Marrow Transpl. 2008;42:209–11.
Rubio MT, Durey-Dragon MA, Wang Y, Blouin J, Jacquelin S, Milpied P, et al. Prognostic significance of complement system activation after allogeneic hematopoietic stem cell transplantation. Blood. 2009;114:1166.
Varga L, Poros A, Puskas E, Panya A, Kramer J, Gyodi E, et al. Clinical significance of longitudinal complement measurements in recipients of bone marrow transplant. Bone Marrow Transpl. 1995;15:509–14.
Noel DR, Witherspoon RP, Storb R, Atkinson K, Doney K, Mickelson EM, et al. Does graft-versus-host disease influence the tempo of immunologic recovery after allogeneic human marrow transplantation? An observation on 56 long-term survivors. Blood. 1978;51:1087–105.
Huber-Lang M, Sarma JV, Zetoune FS, Rittirsch D, Neff TA, McGuire SR, et al. Generation of C5a in the absence of C3: a new complement activation pathway. Nat Med. 2006;12:682–7.
Burwick RM, Burwick NR, Feinberg BB. Eculizumab fails to inhibit generation of C5a in vivo. Blood. 2014;124:3502–3.
Sugihara T, Kobori A, Imaeda H, Tsujikawa T, Amagase K, Takeuchi K, et al. The increased mucosal mRNA expressions of complement C3 and interleukin-17 in inflammatory bowel disease. Clin Exp Immunol. 2010;160:386–93.
Laufer J, Oren R, Goldberg I, Horwitz A, Kopolovic J, Chowers Y, et al. Cellular localization of complement C3 and C4 transcripts in intestinal specimens from patients with Crohn’s disease. Clin Exp Immunol. 2000;120:30–37.
Halstensen TS, Mollnes TE, Garred P, Fausa O, Brandtzaeg P. Surface epithelium related activation of complement differs in Crohn’s disease and ulcerative colitis. Gut. 1992;33:902–8.
Ahrenstedt O, Knutson L, Nilsson B, Nilsson-Ekdahl K, Odlind B, Hallgren R. Enhanced local production of complement components in the small intestines of patients with Crohn’s disease. N Engl J Med. 1990;322:1345–9.
Halstensen TS, Mollnes TE, Garred P, Fausa O, Brandtzaeg P. Epithelial deposition of immunoglobulin G1 and activated complement (C3b and terminal complement complex) in ulcerative colitis. Gastroenterology. 1990;98:1264–71.
Manthey HD, Woodruff TM, Taylor SM, Monk PN. Complement component 5a (C5a). Int J Biochem Cell Biol. 2009;41:2114–7.
Scola AM, Higginbottom A, Partridge LJ, Reid RC, Woodruff T, Taylor SM, et al. The role of the N-terminal domain of the complement fragment receptor C5L2 in ligand binding. J Biol Chem. 2007;282:3664–71.
Volokhina EB, Bergseth G, van de Kar NC, van den Heuvel LP, Mollnes TE. Eculizumab treatment efficiently prevents C5 cleavage without C5a generation in vivo. Blood. 2015;126:278–9.
Wagner JL, Hugli TE. Radioimmunoassay for anaphylatoxins: a sensitive method for determining complement activation products in biological fluids. Anal Biochem. 1984;136:75–88.
Acknowledgements
The authors would like to thank the investigators from the study sites: Zaid Al-Kadhimi (Emory University Hospital, Atlanta, GA, USA), George Liwei Chen (Roswell Park Cancer Institute, Buffalo, NY, USA), Iskra Pusic (Washington University School of Medicine, St. Louis MO, USA), Michele Donato (John Theurer Cancer Center, Hackensack University Medical Center, Hackensack, NJ, USA), and Stéphane Vigouroux (Centre F. Magendie, Hospital Haut-Leveque, France). The authors thank John Levine, James Ferrara, (Icahn School of Medicine at Mount Sinai, New York, NY), and Susan Abraham (University of Texas MD Anderson Cancer Center, Houston, TX) for contributions to the biomarker analyses. The authors also thank from Alexion Pharmaceuticals: Richard Riese, Susan Faas, and Mittie Doyle for contributions to study design, Kaushik Patra and Fanny O’Brien for extensive review of the data, and Rima Saliba for providing statistical guidance. This study was supported by research funding from Alexion Pharmaceuticals Inc. Medical writing support was provided by Bioscript Group, Macclesfield, UK, funded by Alexion Pharmaceuticals Inc.
Author information
Authors and Affiliations
Contributions
RSM, interpreted the data and wrote the manuscript. BO, helped manage clinical trial as research nurse and reviewed manuscript critically for important intellectual content. AM, KA, YD, BY helped design the study, interpret the data, and reviewed the manuscript. AA, helped design the study, interpreted the data and wrote the manuscript. JYC, ES, SH, HA, RC helped enroll patients, interpret the data, and review the manuscript. VR, SG, GS helped design the study, enrolled patients, interpreted data, and reviewed the manuscript. All authors contributed to the manuscript content, approved the final version of the manuscript and agreed to be accountable for questions related to the accuracy and integrity of the work.
Corresponding author
Ethics declarations
Competing interests
RSM received research funding from CSLBehring, Kadmon and Incyte. HA has received consulting fees from Incyte and BMS. YD, and AM are employees and stockholders of Alexion Pharmaceuticals Inc (now Alexion, Astrazeneca Rare Disease). BY and KA were employees and stockholders of Alexion Pharmaceuticals Inc during the development phase of this manuscript. GS received a research grant from Alexion Pharamceuticals. SH has received consulting fees/honoraria from Incyte, Generon and served participated in a Data Safety Monitoring Board/Advisory Board for CSl Behring. JYC declares receiving honoraria for participating in an Advisory Board for Alexion Pharmaceuticals. BO, VR, SG, RC, and ES declare no competing interests. AA has received research support, and honoraria for participating in an Advisory Board for Alexion Pharmaceuticals.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mehta, R.S., Ali, H., Dai, Y. et al. A prospective phase 2 clinical trial of a C5a complement inhibitor for acute GVHD with lower GI tract involvement. Bone Marrow Transplant 58, 991–999 (2023). https://doi.org/10.1038/s41409-023-01996-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-01996-4