Abstract
The Myeloma X trial provided a platform to explore genetics in relation to systematic assessment of patient-reported outcomes at key points during salvage treatment in multiple myeloma (MM) patients. Blood DNA was obtained in 191 subjects for single nucleotide polymorphism (SNP) genotyping. By univariable analysis, the non-coding rs2562456 SNP, upstream of LINC00664, was associated with several relevant pain and health-related quality-of-life (HRQoL) scores at 100 days after allocation to consolidation with autologous stem cell transplantation or weekly cyclophosphamide. Presence of the minor (C) allele was associated with lower pain interference (p = 0.014) and HRQoL pain (p = 0.003), and higher HRQoL global health status (p = 0.011) and physical functioning (p = 0.007). These effects were not modified by treatment arm and were no longer significant at 6 months. Following induction therapy, the rs13361160 SNP near the CCT5 and FAM173B genes was associated with higher global health (p = 0.027) and physical functioning (p = 0.013). This exploratory study supports associations between subjective parameters in MM with SNPs previously identified in genome-wide association studies of pain. Conversely, SNPs in candidate genes involved in opioid and transporter pathways showed no effect. Further studies are warranted in well-defined cancer populations, and potentially assisted by whole genome sequencing with germline analysis in routine diagnostics in haematological cancers.
Similar content being viewed by others
Introduction
Multiple myeloma (MM) forms ~10% of haematological cancers and is largely incurable. However, therapeutic advances in the last two decades have led to major extension of survival. With improving survival, MM is being experienced by an increasing proportion of patients as a chronic illness, and therefore supportive and symptomatic care is a cornerstone of disease management, particularly in relation to pain control. There is a significant symptom burden at all stages of disease, including pain, fatigue and other elements which impact directly on health-related quality of life (HRQoL) [1,2,3].
Pain in myeloma arises not only from infiltration of the bone marrow by malignant plasma cells, bone osteolysis and fracture, but also from side effects of treatments, particularly chemotherapy-induced peripheral neuropathy, and may continue to be significant in patients with stable disease who are off active treatment [4]. In animal models and clinical studies of patients with bone-related malignancy, experience of pain and other symptoms are the result of the interactions between a) host/tumour factors such as cytokines operating locally within the bone where the plasma cells are multiplying [5, 6]; b) the acute and chronic effects of anti-myeloma therapy [4, 7]; c) long-term potentiation and sensitisation in the ascending pain pathways in the spinal cord and brain, balanced by descending modulatory controls [8]; d) pharmacokinetic and pharmacodynamic consequences of analgesic absorption and metabolism [9]; e) a range of other circulating pathophysiological factors, ranging from renal function, endocrine, dietary as well as cytokines and mediators of inflammation which can impact on physiological mechanisms of pain [4, 10]
Examples of genetic factors contributing to pain experience include the three main opioid receptors (mu, kappa and delta) whose genes contain inherited variants that occur relatively frequently in human populations [11,12,13,14]. Such genetic variation has been associated with gender differences in the response to experimentally induced pain [15,16,17], and higher requirements for mu agonist drugs such as morphine and higher quantities of potentially toxic metabolites of morphine [18, 19]. While little is known about the effects of their SNPs in humans, kappa and delta-opioid receptors are considered important mediators in chronic pain situations and patients carrying alleles showing abnormal expression or function may also demonstrate aberrant pain experience. Like many other drugs, the absorption of opioids from the gastrointestinal tract into blood and thence across the blood-brain barrier is regulated by transporter proteins, and the function of these and subsequent drug metabolism also have a genetic basis [20, 21].
Genome-wide association studies (GWAS) carried out to date have not included cancer-related pain, but GWAS of post-surgical and chronic widespread pain have generated some potentially relevant candidate gene regions [22, 23]. Previous genetic studies of cancer pain have usually been carried out in patients with mixed tumour types, often in the advanced stages of illness, when many other factors can aggravate pain experience and confound the measurement of pain response. However, there are currently no published studies of SNPs or other genetic determinants and their effects on pain and analgesic response in patients with MM. There is a need for studies to be done in more tightly controlled populations with well-circumscribed treatments.
The UK National Cancer Research Institute Myeloma X trial was a phase III randomised controlled trial which recruited relapsed myeloma patients from 2008 to 2012. Its aims were to determine the role of a second or ‘salvage’ autologous stem cell transplant (sASCT) as a novel consolidation therapy in patients at first relapse following prior high-dose chemotherapy and ASCT. Myeloma X provided definitive evidence of the efficacy of a sASCT in terms of significantly improved time to progression, progression-free survival and overall survival, compared to conventional non-transplant consolidation (NTC) [24, 25]. A secondary aim of Myeloma X was to evaluate the impact of sASCT as compared to NTC with weekly oral cyclophosphamide on PROs relating to HRQoL and pain [26]. This linked HRQoL study confirmed that patients randomised to sASCT experienced a comparative reduction in quality of life and greater impact of treatment side-effects lasting for 6 months and for increased pain up to 2 years, after which patients who had received sASCT reported better outcomes than those receiving conservative treatment.
Myeloma X provided the only comprehensive picture of HRQoL before and after sASCT in patients with relapsed MM and highlighted the need to improve symptom management in the peri-transplant period [26]. The trial also provided a source of biological material by which the genetic basis of pain and analgesic response could be investigated in a well-defined homogeneous population of myeloma patients in conjunction with standard prospective assessments of pain, HRQoL, analgesic dosage and other symptom variables.
Materials and methods
Regulatory and ethical approval
Collection of pain and HRQoL data was intrinsic to the Myeloma X trial and consent for the use of translational research samples in additional genetic studies was incorporated to cover this and other studies associated with the trial (Multicentre Research Ethics Committee, UK; REC number: 07/S0703/66). The Myeloma X trial is registered with ClinicalTrials.gov, number NCT00747877 and European Clinical Trials Database, number 2006–005890–24.
Patients and assessments
Details of the Myeloma X trial population are summarised in previous publications [24,25,26]. Between 16 April 2008 and 19 November 2012, of 297 patients registered, 288 patients consented to the QoL sub-study and 174 patients were randomly assigned to receive sASCT (n = 89; 88 consenting to QoL studies) or NTC (n = 85; 83 consenting)). Baseline demographic and disease characteristics were well balanced between the treatment groups, except for a higher proportion of patients with International Staging System III in the transplant group.
A secondary aim of Myeloma X was to determine the impact of the treatment strategies on pain and HRQoL [26]. These were variables collected from the outset of the Myeloma X trial, thus allowing exploratory analysis of these variables in relation to SNP genotypes. With respect to pain, the key outcome measures for pain were the Brief Pain Inventory (short form) (BPI-SF) [27], a well-established, validated instrument to assess pain severity (and its impact on several aspects of daily living). Key outcome measures for HRQoL relevant to this paper were the EORTC-QLQ-C30 [28] and its physical functioning, pain and fatigue scales. Questions 29 and 30 in the EORTC-QLQ-C30 are combined to give scores from 0–100 for ‘global health-related quality of life’. These key parameters were used as dependent variables in the main genetic analyses, alongside BPI scores. In both arms of the Myeloma X trial pain and quality of life questionnaires were administered at registration, after completion of induction chemotherapy, pre-randomisation and at 100 days, 6 months and 12 months post-randomisation and annually thereafter. Although attempts had been made to collect data on opioid and other analgesic consumption, the dataset was not sufficiently complete and therefore these variables were not included in the analysis.
Patient samples
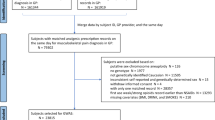
Blood DNA was available for 191 subjects for genotyping. Table 1 provides a summary of those with both successful genotyping and the relevant pain and QoL scores at the four-time points. The Haematological Malignancy Diagnostic Service laboratory in Leeds collected and managed all the tissue and blood samples from Myeloma X trial in full compliance with GLP standards. DNA was extracted from frozen whole blood using the Flexigene kit (Qiagen).
Genotyping
SNPs were selected in candidate genes relating to pain pathways (notably opioid receptors OPRM1, OPRD, TRPV1) and genes relating to drug absorption and metabolism (ABCB1, COMT), based on previous reports of association with pain and QoL in the literature, including two SNPs identified in GWAS of pain in non-cancer populations (rs2562456 near LINC00664, rs13361160 near CCT5, FAM173B). The selected SNPs and corresponding assays used are listed in Table 2.
Genotyping was carried out for each consenting patient registered in Myeloma X and with blood DNA available using the Applied Biosystems Taqman platform (Thermo Fisher Scientific). The assay for rs9479757 gave poor allelic discrimination and these data were not included, but call rates for all other SNPs were >98%. Nineteen (~10%) of samples were duplicated on the assay plates for all SNPs, and there was 1 discrepancy in genotype calls amongst the duplicates (<0.1%).
Hypotheses and statistical analysis
We hypothesised that inherited genetic variants of relevant pain receptor pathways previously reported to be associated with pain and quality of life outcomes are associated with BPI pain scores and HRQoL in patients with relapsed MM. To test this hypothesis, pain (worst, least, average pain and pain interference from BPI-SF) [27] and HRQoL variables (Global Health Status, Physical Functioning, Pain and Fatigue in QLQ-C30) [28] were used.
Exploratory univariable linear regression with SNP genotype as explanatory variable was carried out for eight SNPs and eight pain and quality of life variables at four time points; study registration, end PAD, 100 days post-randomisation and 6 months post randomisation. SNP genotypes were coded as 0, 1, 2 for common homozygous, heterozygous and rare homozygous genotypes respectively. Multivariable regression was carried out to control for treatment arm, with NTC as the reference group. Statistical analyses were carried out in Stata Version 12 and all statistical tests were two-sided. The eight SNPs represent independent tests, but many of the outcome variables are correlated with one another. A guideline Bonferroni-adjusted p value threshold to help identify effects of interest would be 0.05/8 = 0.006. All p values are two-sided and are shown unadjusted.
Results
Association between inherited variants and pain and quality of life scores
A summary of the age and gender distributions of consenting patients with SNP genotype and BPI Pain/HRQoL scores available is shown in Table 1. In the exploratory univariable analysis, there was suggestive evidence that the non-coding rs2562456 SNP upstream of LINC00664 on chromosome 19 was associated with a number of pain and HRQoL scores at 100 days after randomisation to sASCT or NTC (Fig. 1 and Table 3; full results in Supplementary Table 1). The presence of the minor C allele was associated with lower BPI pain interference score (p = 0.014) and HRQoL pain score (p = 0.003), and higher HRQoL global health status (p = 0.011) and physical functioning scores (p = 0.007). The graphs in Fig. 1 suggest a dominant genetic effect, in other words, carriage of one, or two, copies of the C allele have a similar effect on pain and HRQoL, although numbers of rare homozygous individuals are too small to formally test this hypothesis. No significant associations remained at 6 months (Supplementary Table 1). These results suggest that patients carrying at least one copy of the C allele of rs2562456 experienced less pain and better quality of life compared to those of the more common TT genotype at 100 days after randomisation, but that these genetic differences in outcomes disappeared by 6 months.
Box and whisker plots by SNP genotype for a BPI pain interference score, b HRQoL pain score, c HRQoL global health status score, and d HRQoL physical functioning score, at 100 days. The X-axes show SNP genotype group and the number of individuals of each genotype in brackets. Regression p values for univariable analyses are as follows. a: 0.014; b: 0.011; c. 0.007; d: 0.003; see Table 3.
We reported previously that global health status scores were better in the NTC group at 100 days post-randomisation [26]. We, therefore, explored whether the above rs2562456 SNP effects were modified by treatment arm. Table 3 therefore also shows the results of univariable regression models for treatment, together with the SNP effects where both SNP and treatment are included in the model. Based on these analyses, there is no evidence to suggest that the SNP effects are substantially modified by treatment.
We also identified some less significant SNP effects with individual pain and HRQoL scores at other time points (highlighted in Supplementary Table 1). Of these, only one SNP yielded nominally significant p values across more than one pain or HRQoL score. Following induction therapy, the minor C allele of the rs13361160 SNP near the CCT5 and FAM173B genes was associated with higher global health (p = 0.027) and physical functioning scores (p = 0.013) at this time point (Fig. 2 and Table 3). Other nominally significant findings (p < 0.05) included the association of rs1799971 in OPRM1 with BPI Least Pain score and rs2562456 upstream of LINC00664 with HRQoL fatigue score, after induction therapy, and rs2035282 in ABCB1 with BPI Average Pain, and rs8065080 in TRPV1 with Pain Interference score, at registration (Supplementary Table 1).
Box and whisker plots by SNP genotype for a: HRQoL global health status and b: HRQoL physical functioning post-induction therapy. The X-axes show SNP genotype group and the number of individuals of each genotype in brackets. Regression p values for univariable analyses are as follows. a: 0.027, b: 0.013; see Table 3.
Discussion
The Myeloma X trial provided us a unique opportunity to study pain and HRQoL in a well-defined relatively homogenous cancer population all receiving a set of acute standardised anti-cancer interventions. A key difference between our study and previous ones in cancer and many other long-term conditions is that we have focused on a relatively earlier stage of disease and in the context of a well-defined clinical scenario, namely myeloma in first relapse undergoing consolidation treatment with sASCT or weekly cyclophosphamide.
Our exploratory study has provided evidence to support a role for some candidate SNPs identified in previous GWAS for pain, but, interestingly, we found only very minimal support for SNPs in candidate pain pathways such as opioid receptors. Because we also studied a range of HRQoL endpoints, we were able to identify gene associations beyond the pain outcomes that are normally reported.
Our previous results from the Myeloma X trial showed that at 100 days after randomisation global health scores were better in the NTC arm compared to the sASCT arm [26]. Interestingly, the more convincing SNP associations with pain and HRQoL were also observed at this time point. We found the minor (C) allele of the non-coding rs2562456 SNP upstream of the long non-coding RNA LINC00664 was associated with lower pain scores and higher global health status and physical functioning scores at 100 days, and there was no significant evidence of any difference between treatment arms, although power to test this is low. Somewhat consistent with this result, this SNP was previously identified in a small GWAS examining acute post-operative pain following dental surgery, which found that subjects who were homozygous for the minor allele of rs2562456 experienced a longer time before they required post-operative analgesia [29]. Further work needs to be done to understand the potential role of this SNP in cancer populations.
A SNP in rs13361160 SNP near the CCT5 and FAM173B genes has previously been shown to be important in GWAS study of patients who had chronic widespread pain. We have now also identified this as being potentially relevant in MM patients, although it was associated not with pain scores, but rather with higher global health and physical functioning scores.
The results for both SNPs need to be interpreted with caution due to the large number of comparisons carried out in this exploratory study, and further research specifically in myeloma cohorts is required, in order to validate the present findings. The potential mechanisms of action are not clear, as non-coding SNPs may act by altering the expression of genes that are distant from the SNP in the genome. Thus, if the findings are validated, the next steps will be to identify the target genes through functional genomics, and to tease out the precise genetic models and biological mechanisms.
In contrast to the above results for two SNPs identified through GWAS, many of the positive gene associations with pain that have previously been reported in cancer patients were negative in this study. This may result from a lack of statistical power in the present study, as others have been larger. Alternatively, it may reflect the much more defined population and very specific treatments in the present study, compared to previous studies which have been in more heterogeneous settings. The Myeloma X trial did not standardise the opioid regimens for pain management which could explain why we failed to identify associations between pain outcomes and specific opioid receptor pathways. However, it should be noted that previously published studies exploring genetic influences on pain have mostly used heterogeneous samples of non-cancer populations, and in cancer, mixed primary sites and patients at different stages of disease and on differing anti-cancer or analgesic treatments [18]. Not surprisingly, therefore, the results of individual studies have been mixed and most later systematic reviews have concluded that only a few salient genetic signals stood out consistently [30, 31]. These include SNPs in genes associated with the pain pathways (notably opioid receptors) and genes relating to drug absorption and metabolism [32, 33]. It should be noted that there have been relatively few GWAS studies of pain to date, and none so far have been conducted in the cancer setting.
This study is subject to several limitations including an open-label design where lack of blinding may have relevance in relation to subjectively reported endpoints, using paper-based questionnaires subject to adherence, especially when patients are experiencing periods of increased illness and attrition rates as a possible source of bias. The sample size for this study was not specified a priori, and therefore results should be interpreted with caution. We have previously reported that randomisation to sASCT led to a significantly worse short-term HRQoL and pain outcomes compared to standard treatment; in addition, those patients who reported more acute treatment-related side effects experienced different HRQoL outcomes [26]. It is possible that by pooling both treatment arms for the current analysis, some potential signals may have been lost. However, compared to the full dataset of our earlier publication, the sample size for this study was judged to be too small for such subgroup comparisons. As stated above, it was not feasible to standardise the analgesic regimens for all the Myeloma X trial sites, and although attempts had been made to collect data on significant pharmacological parameters, such as opiates and other analgesia, the dataset was not sufficiently complete and therefore these variables were not accounted for and may have had an overriding or confounding influence.
In conclusion, although exploratory, with uncertain generalisability and reproducibility at present, our study paves the way for further research of HRQoL, pain and other symptomatology both in MM and potentially other cancers associated with pain. The ultimate benefit of this and subsequent research will be to identify patients who are more at risk of developing pain and other symptoms, or who are more likely to have variant responses to conventional medical analgesic interventions, in order to improve the patient experience as well as enhance survival. Further exploration is warranted to increase our understanding and provide therapeutic benefits in personalised care, both in myeloma-specific and in broader cancer settings. This may be assisted by whole genome sequencing with germline analysis in routine diagnostics in haematological and other cancers.
Data availability
The datasets generated during and/or analysed during the current study are available from the authors on reasonable request (via corresponding author). No data were deposited for this specific exploratory study, Previous relevant Myeloma X clinical trial publications are fully referenced.
References
Snowden JA, Ahmedzai SH, Ashcroft J, D’Sa S, Littlewood T, Low E, et al. Guidelines for supportive care in multiple myeloma 2011. Br J Haematol. 2011;154:76–103.
Snowden JA, Greenfield DM, Bird JM, Bowland E, Bowcock S, Fisher A, et al. Guidelines for screening and management of late and long-term consequences of myeloma and its treatment. Br J Haematol. 2017;176:888–907.
Pratt G, Morris TC. Review of the NICE guidelines for multiple myeloma. Int J Lab Hematol. 2017;39:3–13.
Boland E, Eiser C, Ezaydi Y, Greenfield DM, Ahmedzai SH, Snowden JA. Living with advanced but stable multiple myeloma: a study of the symptom burden and cumulative effects of disease and intensive (hematopoietic stem cell transplant-based) treatment on health-related quality of life. J Pain Symptom Manag. 2013;46:671–80.
Ahmedzai SH, Boland J. Opioids for chronic pain: molecular and genomic basis of actions and adverse effects. Curr Opin Support Palliat Care. 2007;1:117–25.
Mantyh P. Bone cancer pain: causes, consequences, and therapeutic opportunities. Pain. 2013;154:S54–62.
Boland EG, Selvarajah D, Hunter M, Ezaydi Y, Tesfaye S, Ahmedzai SH, et al. Central pain processing in chronic chemotherapy-induced peripheral neuropathy: a functional magnetic resonance imaging study. PLoS One. 2014;9:e96474.
Kucharczyk MW, Derrien D, Dickenson AH, Bannister K. Stage-specific plasticity descending modulatory controls a rodent model cancer-induced bone pain. Cancers. 2020;12:3286
De Gregori S, De Gregori M, Ranzani GN, Allegri M, Minella C, Regazzi M. Morphine metabolism, transport and brain disposition. Metab Brain Dis. 2012;27:1–5.
Greenfield DM, Boland E, Ezaydi Y, Ross RJ, Ahmedzai SH, Snowden JA, Late Effects Group (2014). Endocrine, metabolic, nutritional and body composition abnormalities are common in advanced intensively-treated (transplanted) multiple myeloma. Bone Marrow Transpl. 2014;49:907–12.
Zubieta JK, Smith YR, Bueller JA, Xu Y, Kilbourn MR, Jewett DM, et al. Regional mu opioid receptor regulation of sensory and affective dimensions of pain. Science. 2001;293:311–5.
Lotsch J, Stuck B, Hummel T. The human mu-opioid receptor gene polymorphism 118A>G decreases cortical activation in response to specific nociceptive stimulation. Behav Neurosci. 2006;120:1218–24.
Fillingim RB, Kaplan L, Staud R, Ness TJ, Glover TL, Campbell CM, et al. The A118G single nucleotide polymorphism of the mu-opioid receptor gene (OPRM1) is associated with pressure pain sensitivity in humans. J Pain. 2005;6:159–67.
Ross JR, Rutter D, Welsh K, Joel SP, Goller K, Wells AU, et al. Clinical response to morphine in cancer patients and genetic variation in candidate genes. Pharmacogenom J. 2005;5:324–36.
Zubieta JK, Smith YR, Bueller JA, Xu Y, Kilbourn MR, Jewett DM, et al. Mu-opioid receptor-mediated antinociceptive responses differ in men and women. J Neurosci. 2002;22:5100–7.
Oertel B, Lötsch J. Genetic mutations that prevent pain: implications for future pain medication. Pharmacogenomics. 2008;9:179–94.
Holtman JR Jr, Wala EP. Characterization of the antinociceptive effect of oxycodone in male and female rats. Pharamcol Biochem Behav. 2006;83:100–8.
Klepstad P, Rakvag TT, Kaasa S, Holthe M, Dale O, Borchgrevink PC, et al. The 118A>G polymorphism in the human mu-opioid receptor gene may increase morphine requirements in patients with pain caused by malignant disease. Acta Anaesthesiol Scand. 2004;48:1232–9.
Chou WY, Yang LC, Lu HF, Ko JY, Wang CH, Lin SH, et al. Association of mu-opioid receptor gene polymorphism (A118G) with variations in morphine consumption for analgesia after total knee arthroplasty. Acta Anaesthesiol Scand. 2006;50:787–92.
Kharasch ED. Current concepts in methadone metabolism and transport. Clin Pharm Drug Dev. 2017;6:125–34.
Campa D, Gioia A, Tomei A, Poli P, Barale R. Association of ABCB1/MDR1 and OPRM1 gene polymorphisms with morphine pain relief. Clin Pharm Ther. 2008;83:559–66.
Kim H, Clark D, Dionne RA. Genetic contributions to clinical pain and analgesia: avoiding pitfalls in genetic research. J Pain. 2009;10:663–93.
Peters MJ, Broer L, Willemen HLDM, Eiriksdottir G, Hocking LJ, Holliday KL, et al. Genome-wide association study meta-analysis of chronic widespread pain: evidence for involvement of the 5p15.2 region. Ann Rheum Dis. 2013;72:427–36.
Cook G, Williams C, Brown JM, Cairns DA, Cavenagh J, Snowden JA, et al. High-dose chemotherapy plus autologous stem-cell transplantation as consolidation therapy in patients with relapsed multiple myeloma after previous autologous stem-cell transplantation (NCRI Myeloma X Relapse [Intensive trial]): a randomised, open-label, phase 3 trial. Lancet Oncol. 2014;15:874–85.
Cook G, Ashcroft AJ, Cairns DA, Williams CD, Brown JM, Cavenagh JD, et al. The effect of salvage autologous stem-cell transplantation on overall survival in patients with relapsed multiple myeloma (final results from BSBMT/UKMF Myeloma X Relapse [Intensive]): a randomised, open-label, phase 3 trial. Lancet Haematol. 2016;3:e340–51.
Ahmedzai SH, Snowden JA, Ashcroft AJ, Cairns DA, Williams C, Hockaday A, et al. Patient-reported outcome results from the open-label, randomized phase III myeloma X trial evaluating salvage autologous stem-cell transplantation in relapsed multiple myeloma. J Clin Oncol. 2019;37:1617–28. National Cancer Research Institute Haemato-Oncology Clinical Studies Group.
Cleeland CS. The measurement of pain from metastatic bone disease: capturing the patient’s experience. Clin Cancer Res. 2006;12:6236s–42s.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76.
Kim H, Neubert JK, San Miguel A, Xu K, Krishnaraju RK, Iadarola MJ, et al. Genetic influence on variability in human acute experimental pain sensitivity associated with gender, ethnicity and psychological temperament. Pain. 2004;109:488–96.
Muralidharan A, Smith MT. Pain, analgesia and genetics. J Pharm Pharm. 2011;63:1387–400.
Kim H, Ramsay E, Lee H, Wahl S, Dionne RA. Genome-wide association study of acute post-surgical pain in humans. Pharmacogenomics. 2009;10:171–9.
Lacroix-Fralish ML, Mogil JS. Progress in genetic studies of pain and analgesia. Annu Rev Pharm Toxicol. 2009;49:97–121.
Reyes-Gibby CC, Shete S, Rakvåg T, Bhat SV, Skorpen F, Bruera E, et al. Exploring joint effects of genes and the clinical efficacy of morphine for cancer pain: OPRM1 and COMT gene. Pain. 2007;130:25–30.
Nielsen LM, Christrup LL, Sato H, Drewes AM, Oleson AE. Genetic influences of OPRM1, OPRD1 and COMT on morphine analgesia in a multi-modal, multi-tissue human experimental pain model. Basic Clin Pharm Toxicol. 2017;121:6–12.
Crist RC, Clarke T-K. OPRD1 genetic variation and human disease. Handb Exp Pharm. 2018;247:131–45.
Beer B, Erb R, Pavlic M, Ulmer H, Giacomuzzi S, Riemer Y, et al. Association of polymorphisms in pharmacogenetic candidate genes (OPRD1, GAL, ABCB1, OPRM1) with opioid dependence in European population: a case-control study. PLoS One. 2013;8:e75359.
Acknowledgements
We thank all the patients who took part in the study as well as all the principal investigators and other study staff at the >50 recruiting centres throughout the United Kingdom. The Myeloma X (Relapse) study was funded by Cancer Research UK [CRUK/06/018] with unrestricted educational grants from Janssen-Cilag and Chugai Pharma UK. The industry partners had no part in the design, running or analysis of the study. This work was supported by Core Clinical Trials Unit Infrastructure from Cancer Research UK (C7852/A25447). The study was coordinated by the Clinical Trials Research Unit (CTRU), University of Leeds. We are grateful to all current and past members of CTRU staff for their hard work and commitment to these studies. This research was supported by the National Institute for Health Research (NIHR) infrastructure at Leeds, UK. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health. Genotypic analyses were supported by Sheffield Hospitals Charity.
Author information
Authors and Affiliations
Consortia
Contributions
Conception and design: JAS, SHA, AC, TCM and GC. Collection and assembly of data: All authors. Data analysis and interpretation: JAS, SHA, AC, DAC, AJA, IB, TCM and GC. Manuscript writing: All authors. Final approval of manuscript and accountability: All authors.
Corresponding author
Ethics declarations
competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Congress Presentation: This study was presented in part as a poster at The American Society of Haematology Annual Meeting, Orlando FL, 2015.
Supplementary information
41409_2022_1738_MOESM1_ESM.xlsx
Supplementary table 1. Complete regression results organised by time point and by SNP with the results mentioned in the text highlighted.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Snowden, J.A., Ahmedzai, S.H., Cox, A. et al. Association of genetic variants with patient reported quality of life and pain experience in patients in the UK NCRI Myeloma X Relapse [Intensive]) trial; an exploratory study. Bone Marrow Transplant 57, 1507–1513 (2022). https://doi.org/10.1038/s41409-022-01738-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01738-y
This article is cited by
-
SNPs and PROs in myeloma: the most ambitious crossover of all time?
Bone Marrow Transplantation (2022)