Abstract
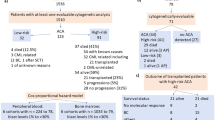
Chromosome analysis is a powerful prognostic tool in myeloid malignancies. Recipients who experience relapse after allogeneic hematopoietic cell transplantation (allo-HCT) often show chromosomal changes between diagnosis and relapse. However, the clinical impact of chromosomal changes and the efficacy of post-relapse treatment according to chromosomal changes have not been fully investigated. We retrospectively analyzed 72 recipients who had experienced relapse after allo-HCT for acute myeloid leukemia or myelodysplastic syndrome. We categorized them into two groups: with or without clonal chromosomal changes at relapse after allo-HCT. Post-relapse survival was shorter in the clonal chromosomal change group (median 117 days vs 275 days, P = 0.019). Moreover, acquisition of chromosome 7 abnormality or complex changes tended to be associated with inferior survival in a univariate analysis (median 92 days vs median 173 days, P = 0.043), and this adverse impact was confirmed in a multivariate analysis (hazard ratio 2.07, P = 0.024). The patterns of chromosomal changes from diagnosis to relapse after allo-HCT were heterogenous, and further investigations are required to clarify the effect of individual chromosomal changes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article (and its supplementary information files).
References
Grimwade D, Ivey A, Huntly BJ. Molecular landscape of acute myeloid leukemia in younger adults and its clinical relevance. Blood 2016;127:29–41.
Bochtler T, Fröhling S, Krämer A. Role of chromosomal aberrations in clonal diversity and progression of acute myeloid leukemia. Leukemia 2015;29:1243–52.
de Lima M, Porter DL, Battiwalla M, Bishop MR, Giralt SA, Hardy NM, et al. Proceedings from the National cancer institute’s second international workshop on the biology, prevention, and treatment of relapse after hematopoietic stem cell transplantation: Part III. Prevention and treatment of relapse after allogeneic transplantation. Biol Blood Marrow Transpl. 2014;20:4–13.
Yuasa M, Yamamoto H, Mitsuki T, Kageyama K, Kaji D, Taya Y, et al. Prognostic impact of cytogenetic evolution on the outcome of allogeneic stem cell transplantation in patients with acute myeloid leukemia in nonremission: A single-institute analysis of 212 recipients. Biol Blood Marrow Transpl. 2020;26:2262–70.
Ertz-Archambault N, Kosiorek H, Slack JL, Lonzo ML, Greipp PT, Khera N, et al. Cytogenetic evolution in myeloid neoplasms at relapse after allogeneic hematopoietic cell transplantation: Association with previous chemotherapy and effect on survival. Biol Blood Marrow Transpl. 2017;23:782–9.
Karrman K, Sallerfors B, Lenhoff S, Fioretos T, Johansson B. Cytogenetic evolution patterns in CML post-SCT. Bone Marrow Transpl. 2007;39:165–71.
Kern W, Haferlach T, Schnittger S, Ludwig WD, Hiddemann W, Schoch C. Karyotype instability between diagnosis and relapse in 117 patients with acute myeloid leukemia: implications for resistance against therapy. Leukemia 2002;16:2084–91.
Bacher U, Haferlach T, Alpermann T, Zenger M, Kröger N, Beelen DW, et al. Comparison of cytogenetic clonal evolution patterns following allogeneic hematopoietic transplantation versus conventional treatment in patients at relapse of AML. Biol Blood Marrow Transpl. 2010;16:1649–57.
Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, et al. Validation and refinement of the Disease Risk Index for allogeneic stem cell transplantation. Blood 2014;123:3664–71.
Mitelman F. ISCN 1995: An international system for human cytogenetic nomenclature (1995): Recommendations of the International Standing Committee on Human Cytogenetic Nomenclature: Memphis, TN, USA, October 9-13, 1994.
Shaffer LG, Tommerup N. ISCN 2005: an international system for human cytogenetic nomenclature (2005): Recommendations of the International Standing Committee on Human Cytogenetic Nomenclature.
International Standing Committee on HumanCytogenetic N, Shaffer LG, Slovak ML, Campbell LJ. ISCN 2009: An international system for human cytogenetic nomenclature (2009): Recommendations of the International Standing Committee on Human Cytogenetic Nomenclature.
Shaffer LG, McGowan-Jordan J, Schmid M. ISCN 2013: An international system for human cytogenetic nomenclature (2013): Recommendations of the International Standing Committee on Human Cytogenetic Nomenclature.
McGowan-Jordan J, Simons A, Schmid M. ISCN 2016: An international system for human cytogenomic nomenclature (2016).
McGowan-Jordan J, Hastings RJ, Moore S. ISCN 2020: An international system for human cytogenomic nomenclature (2020).
Fungtammasan A, Walsh E, Chiaromonte F, Eckert KA, Makova KD. A genome-wide analysis of common fragile sites: what features determine chromosomal instability in the human genome? Genome Res. 2012;22:993–1005.
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 2017;129:424–47.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Solé F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood 2012;120:2454–65.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–8.
Schanz J, Tüchler H, Solé F, Mallo M, Luño E, Cervera J, et al. New comprehensive cytogenetic scoring system for primary myelodysplastic syndromes (MDS) and oligoblastic acute myeloid leukemia after MDS derived from an international database merge. J Clin Oncol. 2012;30:820–9.
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children’s Leukaemia Working Parties. Blood 1998;92:2322–33.
Ding L, Ley TJ, Larson DE, Miller CA, Koboldt DC, Welch JS, et al. Clonal evolution in relapsed acute myeloid leukaemia revealed by whole-genome sequencing. Nature 2012;481:506–10.
Willers H, Dahm-Daphi J, Powell SN. Repair of radiation damage to DNA. Br J Cancer. 2004;90:1297–301.
Samoylov AS, Bushmanov AY, Udalov YD, Galstyan IA, Nugis VY, Kozlova MG, et al. Acute myeloid leukemia, prostate and skin cancer in acute radiation syndrome survivor after the 1986 chernobyl nuclear accident: Case report. Radiat Prot Dosim. 2018;182:85–9.
Nagayama H, Misawa K, Tanaka H, Ooi J, Iseki T, Tojo A, et al. Transient hematopoietic stem cell rescue using umbilical cord blood for a lethally irradiated nuclear accident victim. Bone Marrow Transpl. 2002;29:197–204.
Awa AA, Sofuni T, Honda T, Itoh M, Neriishi S, Otake M. Relationship between the radiation dose and chromosome aberrations in atomic bomb survivors of Hiroshima and Nagasaki. J Radiat Res. 1978;19:126–40.
Sloand EM, Pfannes L, Ling C, Feng X, Jasek M, Calado R, et al. Graft-versus-host disease: Role of inflammation in the development of chromosomal abnormalities of keratinocytes. Biol Blood Marrow Transpl. 2010;16:1665–73.
Vago L, Perna SK, Zanussi M, Mazzi B, Barlassina C, Stanghellini MT, et al. Loss of mismatched HLA in leukemia after stem-cell transplantation. N. Engl J Med. 2009;361:478–88.
Papaemmanuil E, Gerstung M, Bullinger L, Gaidzik VI, Paschka P, Roberts ND, et al. Genomic classification and prognosis in acute myeloid leukemia. N. Engl J Med. 2016;374:2209–21.
Schmidt-Hieber M, Blau IW, Richter G, Türkmen S, Bommer C, Thiel G, et al. Cytogenetic studies in acute leukemia patients relapsing after allogeneic stem cell transplantation. Cancer Genet Cytogenet. 2010;198:135–43.
Garson OM, Hagemeijer A, Sakurai M, Reeves BR, Swansbury GJ, Williams GJ, et al. Cytogenetic studies of 103 patients with acute myelogenous leukemia in relapse. Cancer Genet Cytogenet. 1989;40:187–202.
Waisertreiger I, Barlow J. Fragile site instability: Measuring more than breaks. Oncoscience 2020;7:60–7.
Arlt MF, Durkin SG, Ragland RL, Glover TW. Common fragile sites as targets for chromosome rearrangements. DNA Repair (Amst). 2006;5:1126–35.
Patel JP, Gönen M, Figueroa ME, Fernandez H, Sun Z, Racevskis J, et al. Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. N. Engl J Med. 2012;366:1079–89.
Acknowledgements
We would like to thank donors, recipients, and physicians for their contributions.
Author information
Authors and Affiliations
Contributions
YO designed the study, collected, and analyzed data, and wrote the manuscript. HN designed the study, analyzed data, and wrote the manuscript. YN, MK, S Kawamura, JT, NY, YM, KY, SM, AG, TK, YA, MK, KK, AT, MT, S Kimura, S Kobayashi, and S Kako collected clinical data. FK and YK advised on the methods, wrote the manuscript, and were responsible for the projects.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Okada, Y., Nakasone, H., Nakamura, Y. et al. Prognostic impact of chromosomal changes at relapse after allogeneic hematopoietic cell transplantation for acute myeloid leukemia or myelodysplastic syndrome. Bone Marrow Transplant 57, 810–816 (2022). https://doi.org/10.1038/s41409-022-01635-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01635-4