Abstract
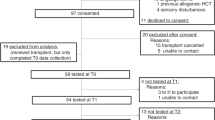
Hematopoietic cell transplant (HCT) is an increasingly common and curative treatment strategy to improve survival among individuals with malignant and nonmalignant diseases, with over one million HCTs having been performed worldwide. Neurocognitive dysfunction is a common and untoward consequence of HCT for many recipients, although few studies have examined the profile of neurocognitive impairments in HCT or their association with clinical features, such as frailty, or the incidence of pre-HCT neurocognitive impairments across all ages, which may influence post-HCT neurocognitive impairments. We examined the pattern and correlates of pre-transplant neurocognitive dysfunction in a prospective sample of adults undergoing HCT. Neurocognition was assessed using the Montreal Cognitive Assessment Battery. Frailty was assessed using the Short Physical Performance Battery. Linear regression analysis was used to examine the associations between neurocognitive performance and frailty. Neurocognitive screening profiles were also examined by partitioning MoCA into domain scores, including Executive Function and Memory. We also examined the associations between neurocognition, frailty, and clinical outcomes, including length of transplant hospitalization and survival. One hundred and ten adults were evaluated across a wide age range (range: 19–75; mean age = 54.7 [SD = 14.1]). Neurocognitive performance tended to fall below published normative levels (mean MoCA = 25.5 [SD = 4.1]), with 17% of participants demonstrating impaired performance compared with medical normative data (MoCA ≤ 22) and 34% exhibiting impaired performance relative to healthy samples (MoCA ≤ 25). Mild impairments (MoCA ≤ 25) were common across age ranges, including middle-aged patients (23% for age < 50; 35% for age 50–60, 41% for age ≥ 60), particularly for items assessing Executive Function. Greater levels of frailty associated with lower neurocognitive screening scores (r = −0.29, P < 0.01) and Executive Functioning (r = −0.24, P < 0.01), whereas greater age was associated with poorer Memory performance only (r = −0.33, P < 0.01). Greater levels of frailty prior to transplant associated with longer length of stay (β = 0.10, P = 0.046), but were not associated with survival. Neurocognitive impairments are common among adults undergoing HCT and the pattern of performance varies by age. Pre-transplant frailty is associated with neurocognitive functioning and may portend worse post-transplant early clinical outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Abel GA, Buckstein R. Integrating Frailty, Comorbidity, and Quality of Life in the Management of Myelodysplastic Syndromes. Am Soc Clin Oncol Educ Book. 2016;35:e337–344. https://doi.org/10.14694/EDBK_158639. 10.1200/EDBK_158639.
Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42:2672–713. https://doi.org/10.1161/STR.0b013e3182299496. e-pub ahead of print 2011/07/23.
Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011;10:819–28.
Plassman BL, Williams JW, Burke JR, Holsinger T, Benjamin S. Systematic review: factors associated with risk for and possible prevention of cognitive decline in later life. Ann Intern Med. 2010;153:182–93.
Kelly DL, Buchbinder D, Duarte RF, Auletta JJ, Bhatt N, Byrne M, et al. Neurocognitive Dysfunction in Hematopoietic Cell Transplant Recipients: Expert Review from the Late Effects and Quality of Life Working Committee of the Center for International Blood and Marrow Transplant Research and Complications and Quality of Life Working Party of the European Society for Blood and Marrow Transplantation. Biol Blood Marrow Transpl. 2018;24:228–41. https://doi.org/10.1016/j.bbmt.2017.09.004.
Buchbinder D, Kelly DL, Duarte RF, Auletta JJ, Bhatt N, Byrne M, et al. Neurocognitive dysfunction in hematopoietic cell transplant recipients: expert review from the late effects and Quality of Life Working Committee of the CIBMTR and complications and Quality of Life Working Party of the EBMT. Bone Marrow Transpl. 2018;53:535–55. https://doi.org/10.1038/s41409-017-0055-7.
Holmes HM, Des Bordes JK, Kebriaei P, Yennu S, Champlin RE, Giralt S, et al. Optimal screening for geriatric assessment in older allogeneic hematopoietic cell transplantation candidates. J Geriatr Oncol. 2014;5:422–30. https://doi.org/10.1016/j.jgo.2014.04.004.
Muffly LS, Kocherginsky M, Stock W, Chu Q, Bishop MR, Godley LA, et al. Geriatric assessment to predict survival in older allogeneic hematopoietic cell transplantation recipients. Haematologica. 2014;99:1373–9. https://doi.org/10.3324/haematol.2014.103655.
Fraz MA, Warraich FH, Warraich SU, Tariq MJ, Warraich Z, Khan AY, et al. Special considerations for the treatment of multiple myeloma according to advanced age, comorbidities, frailty and organ dysfunction. Crit Rev Oncol Hematol. 2019;137:18–26. https://doi.org/10.1016/j.critrevonc.2019.02.011.
Atakul E, Akyar I. Frailty Prevalence and Characteristics in Older Adults with Hematologic Cancer: a Descriptive Study. Asia Pac J Oncol Nurs. 2019;6:43–9. https://doi.org/10.4103/apjon.apjon_35_18.
Hegde A, Murthy HS. Frailty: the missing piece of the pre- hematopoietic cell transplantation assessment? Bone Marrow Transpl. 2018;53:3–10. https://doi.org/10.1038/bmt.2017.192.
Arora M, Sun CL, Ness KK, Teh JB, Wu J, Francisco L, et al. Physiologic Frailty in Nonelderly Hematopoietic Cell Transplantation Patients: results From the Bone Marrow Transplant Survivor Study. JAMA Oncol. 2016;2:1277–86. https://doi.org/10.1001/jamaoncol.2016.0855.
Quinlan N, Marcantonio ER, Inouye SK, Gill TM, Kamholz B, Rudolph JL. Vulnerability: the crossroads of frailty and delirium. J Am Geriatr Soc. 2011;59:S262–268. https://doi.org/10.1111/j.1532-5415.2011.03674.x. Suppl 2.
Bellelli G, Moresco R, Panina-Bordignon P, Arosio B, Gelfi C, Morandi A, et al. Is Delirium the Cognitive Harbinger of Frailty in Older Adults? A Review about the Existing Evidence. Front Med (Lausanne). 2017;4:188. https://doi.org/10.3389/fmed.2017.00188.
Sargent L, Nalls M, Amella EJ, Slattum PW, Mueller M, Bandinelli S, et al. Shared mechanisms for cognitive impairment and physical frailty: A model for complex systems. Alzheimers Dement (N.Y). 2020;6:e12027. https://doi.org/10.1002/trc2.12027. e-pub ahead of print 2020/07/21.
Mayo S, Messner HA, Rourke SB, Howell D, Victor JC, Kuruvilla J, et al. Relationship between neurocognitive functioning and medication management ability over the first 6 months following allogeneic stem cell transplantation. Bone Marrow Transpl. 2016;51:841–7. https://doi.org/10.1038/bmt.2016.2.
Rodrigues M, de Souza PMR, de Oliveira Muniz Koch L, Hamerschlak N. The use of comprehensive geriatric assessment in older patients before allologeneic hematopoietic stem cell transplantation: a cross-sectional study. J Geriatr Oncol. 2020;11:100–6. https://doi.org/10.1016/j.jgo.2019.05.022. e-pub ahead of print 2019/06/25.
Pavasini R, Guralnik J, Brown JC, di Bari M, Cesari M, Landi F, et al. Short Physical Performance Battery and all-cause mortality: systematic review and meta-analysis. BMC Med. 2016;14:215. https://doi.org/10.1186/s12916-016-0763-7.
Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–231. https://doi.org/10.1093/gerona/55.4.m221.
Courtwright AM, Zaleski D, Tevald M, Adler J, Singer JP, Cantu EE, et al. Discharge frailty following lung transplantation. Clin Transpl. 2019:e13694. https://doi.org/10.1111/ctr.13694.
Venado A, McCulloch C, Greenland JR, Katz P, Soong A, Shrestha P, et al. Frailty trajectories in adult lung transplantation: a cohort study. J Heart Lung Transpl. 2019;38:699–707. https://doi.org/10.1016/j.healun.2019.03.006.
Williams FR, Vallance A, Faulkner T, Towey J, Durman S, Kyte D, et al. Home-Based Exercise in Patients Awaiting Liver Transplantation: a feasibility study. Liver Transpl. 2019;25:995–1006. https://doi.org/10.1002/lt.25442.
Rozenberg D, Mathur S, Wickerson L, Chowdhury NA, Singer LG. Frailty and clinical benefits with lung transplantation. J Heart Lung Transpl. 2018;37:1245–53. https://doi.org/10.1016/j.healun.2018.06.005.
Singer JP, Soong A, Bruun A, Bracha A, Chin G, Hays SR, et al. A mobile health technology enabled home-based intervention to treat frailty in adult lung transplant candidates: a pilot study. Clin Transpl. 2018;32:e13274. https://doi.org/10.1111/ctr.13274.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94.
Perracini MR, Mello M, de Oliveira Maximo R, Bilton TL, Ferriolli E, Lustosa LP, et al. Diagnostic Accuracy of the Short Physical Performance Battery for Detecting Frailty in Older People. Phys Ther. 2020;100:90–8. https://doi.org/10.1093/ptj/pzz154. e-pub ahead of print 2019/10/16.
Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–9.
Smith T, Gildeh N, Holmes C. The Montreal Cognitive Assessment: validity and utility in a memory clinic setting. Can J Psychiatry Rev Canadienne de Psychiatr. 2007;52:329–32.
Wefel JS, Vardy J, Ahles T, Schagen SB. International Cognition and Cancer Task Force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncol. 2011;12:703–8. https://doi.org/10.1016/S1470-2045(10)70294-1. e-pub ahead of print 2011/03/01.
Koll TT, Sheese AN, Semin J, Ernst W, High R, Wildes TM, et al. Screening for cognitive impairment in older adults with hematological malignancies using the Montreal Cognitive Assessment and neuropsychological testing. J Geriatr Oncol. 2020;11:297–303. https://doi.org/10.1016/j.jgo.2019.11.007. e-pub ahead of print 2019/12/14.
Smith PJ, Blumenthal JA, Hoffman BM, Davis RD, Palmer SM. Postoperative cognitive dysfunction and mortality following lung transplantation. Am J Transpl. 2018;18:696–703. https://doi.org/10.1111/ajt.14570.
Roman DD, Holker EG, Missov E, Colvin MM, Menk J. Neuropsychological functioning in heart transplant candidates. Clin Neuropsychol. 2016:1–20. https://doi.org/10.1080/13854046.2016.1212096.
Bhat G, Yost G, Mahoney E. Cognitive function and left ventricular assist device implantation. J Heart Lung Transpl. 2015;34:1398–405. https://doi.org/10.1016/j.healun.2015.05.015.
Montero-Odasso M, Almeida QJ, Bherer L, Burhan AM, Camicioli R, Doyon J, et al. Consensus on Shared Measures of Mobility and Cognition: from the Canadian Consortium on Neurodegeneration in Aging (CCNA). J Gerontol A Biol Sci Med Sci. 2019;74:897–909. https://doi.org/10.1093/gerona/gly148. e-pub ahead of print 2018/08/14.
Montero-Odasso M, Almeida QJ, Burhan AM, Camicioli R, Doyon J, Fraser S, et al. SYNERGIC TRIAL (SYNchronizing Exercises, Remedies in Gait and Cognition) a multi-Centre randomized controlled double blind trial to improve gait and cognition in mild cognitive impairment. BMC Geriatr. 2018;18:93. https://doi.org/10.1186/s12877-018-0782-7.
Bartoli M, Palermo S, Cipriani GE, Amanzio M. A Possible Association Between Executive Dysfunction and Frailty in Patients With Neurocognitive Disorders. Front Psychol. 2020;11:554307. https://doi.org/10.3389/fpsyg.2020.554307. e-pub ahead of print 2020/12/03.
Lorenzo-Lopez L, Blanco-Fandino J, Cibeira N, Bujan A, Lopez-Lopez R, Maseda A, et al. Clinical and Neuropsychological Correlates of Prefrailty Syndrome. Front Med (Lausanne). 2020;7:609359. https://doi.org/10.3389/fmed.2020.609359. e-pub ahead of print 2020/11/27.
Yoon DH, Lee JY, Song W. Effects of Resistance Exercise Training on Cognitive Function and Physical Performance in Cognitive Frailty: a Randomized Controlled Trial. J Nutr Health Aging. 2018;22:944–51. https://doi.org/10.1007/s12603-018-1090-9.
Coen RF, Robertson DA, Kenny RA, King-Kallimanis BL. Strengths and Limitations of the MoCA for Assessing Cognitive Functioning: findings From a Large Representative Sample of Irish Older Adults. J Geriatr Psychiatry Neurol. 2016;29:18–24. https://doi.org/10.1177/0891988715598236. e-pub ahead of print 2015/08/08.
Freitas S, Simoes MR, Maroco J, Alves L, Santana I. Construct Validity of the Montreal Cognitive Assessment (MoCA). J Int Neuropsychol Soc. 2012;18:242–50. https://doi.org/10.1017/S1355617711001573. e-pub ahead of print 2011/11/26.
Duro D, Simoes MR, Ponciano E, Santana I. Validation studies of the Portuguese experimental version of the Montreal Cognitive Assessment (MoCA): confirmatory factor analysis. J Neurol. 2010;257:728–34. https://doi.org/10.1007/s00415-009-5399-5. e-pub ahead of print 2009/11/26.
Smith CR, Cavanagh J, Sheridan M, Grosset KA, Cullen B, Grosset DG. Factor structure of the Montreal Cognitive Assessment in Parkinson disease. Int J Geriatr Psychiatry. 2020;35:188–94. https://doi.org/10.1002/gps.5234. e-pub ahead of print 2019/11/19.
Spano G, Caffo AO, Lanciano T, Curci A, Bosco A. Visuospatial/executive abilities and mood affect the reliability of a subjective memory complaints measure. Aging Clin Exp Res. 2020;32:1317–26. https://doi.org/10.1007/s40520-019-01307-2. e-pub ahead of print 2019/08/21.
Benge JF, Balsis S, Madeka T, Uhlman C, Lantrip C, Soileau MJ. Factor structure of the Montreal Cognitive Assessment items in a sample with early Parkinson’s disease. Parkinsonism Relat Disord. 2017;41:104–8. https://doi.org/10.1016/j.parkreldis.2017.05.023. e-pub ahead of print 2017/06/03.
Foster R, Walker S, Brar R, Hiebert B, Komenda P, Rigatto C, et al. Cognitive Impairment in Advanced Chronic Kidney Disease: The Canadian Frailty Observation and Interventions Trial. Am J Nephrol. 2016;44:473–80. https://doi.org/10.1159/000450837. e-pub ahead of print 2016/11/01.
Pendlebury ST, Cuthbertson FC, Welch SJ, Mehta Z, Rothwell PM. Underestimation of cognitive impairment by mini-mental state examination versus the montreal cognitive assessment in patients with transient ischemic attack and stroke: a population-based study. Stroke. 2010;41:1290–3.
Phillips KM, McGinty HL, Cessna J, Asvat Y, Gonzalez B, Cases MG, et al. A systematic review and meta-analysis of changes in cognitive functioning in adults undergoing hematopoietic cell transplantation. Bone Marrow Transpl. 2013;48:1350–7. https://doi.org/10.1038/bmt.2013.61.
Smith PJ, Rivelli S, Waters A, Reynolds J, Hoyle A, Flowers M, et al. Neurocognitive changes after lung transplantation. Ann Am Thorac Soc. 2014;11:1520–7. https://doi.org/10.1513/AnnalsATS.201406-232OC.
Smith PJ, Blumenthal JA, Carney RM, Freedland KE, O’Hayer CVF, Trulock EP, et al. Neurobehavioral functioning and survival following lung transplantation. Chest. 2014;145:604–11. https://doi.org/10.1378/chest.12-2127.
Dew MA, DiMartini AF, Dobbels F, Grady KL, Jowsey-Gregoire SG, Kaan A, et al. The 2018 ISHLT/APM/AST/ICCAC/STSW recommendations for the psychosocial evaluation of adult cardiothoracic transplant candidates and candidates for long-term mechanical circulatory support. J Heart Lung Transpl. 2018;37:803–23. https://doi.org/10.1016/j.healun.2018.03.005.
Panza F, D’Introno A, Colacicco AM, Capurso C, Parigi AD, Capurso SA, et al. Cognitive frailty: Predementia syndrome and vascular risk factors. Neurobiol Aging. 2006;27:933–40.
Aliberti MJR, Cenzer IS, Smith AK, Lee SJ, Yaffe K, Covinsky KE. Assessing Risk for Adverse Outcomes in Older Adults: the Need to Include Both Physical Frailty and Cognition. J Am Geriatr Soc. 2019;67:477–83. https://doi.org/10.1111/jgs.15683.
Peng LN, Chou MY, Liang CK, Lee WJ, Kojima T, Lin MH, et al. Association between serum activin A and metabolic syndrome in older adults: Potential of activin A as a biomarker of cardiometabolic disease. Exp Gerontol. 2018;111:197–202. https://doi.org/10.1016/j.exger.2018.07.020.
Liu Z, Hsu FC, Trombetti A, King AC, Liu CK, Manini TM, et al. Effect of 24-month physical activity on cognitive frailty and the role of inflammation: the LIFE randomized clinical trial. BMC Med. 2018;16:185. https://doi.org/10.1186/s12916-018-1174-8.
Summers MJ, Rainero I, Vercelli AE, Aumayr G, de Rosario H, Monter M, et al. The My Active and Healthy Aging (My-AHA) ICT platform to detect and prevent frailty in older adults: Randomized control trial design and protocol. Alzheimers Dement (N. Y). 2018;4:252–62. https://doi.org/10.1016/j.trci.2018.06.004.
Wood WA, Weaver M, Smith-Ryan AE, Hanson ED, Shea TC, Battaglini CL. Lessons learned from a pilot randomized clinical trial of home-based exercise prescription before allogeneic hematopoietic cell transplantation. Support Care Cancer. 2020;28:5291–8. https://doi.org/10.1007/s00520-020-05369-1. e-pub ahead of print 2020/03/01.
Rupnik E, Skerget M, Sever M, Zupan IP, Ogrinec M, Ursic B, et al. Feasibility and safety of exercise training and nutritional support prior to haematopoietic stem cell transplantation in patients with haematologic malignancies. BMC Cancer. 2020;20:1142. https://doi.org/10.1186/s12885-020-07637-z. e-pub ahead of print 2020/11/26.
Bongers BC, Klaase JM, van Meeteren NLU. Prehabilitation vs Postoperative Rehabilitation for Frail Patients. JAMA Surg. 2020;155:896–7. https://doi.org/10.1001/jamasurg.2020.1801. e-pub ahead of print 2020/06/26.
Gritsenko K, Helander E, Webb MPK, Okeagu CN, Hyatali F, Renschler JS, et al. Preoperative frailty assessment combined with prehabilitation and nutrition strategies: Emerging concepts and clinical outcomes. Best Pr Res Clin Anaesthesiol. 2020;34:199–212. https://doi.org/10.1016/j.bpa.2020.04.008. e-pub ahead of print 2020/07/28.
Dezube AR, Cooper L, Jaklitsch MT. Prehabilitation of the Thoracic Surgery Patient. Thorac Surg Clin. 2020;30:249–58. https://doi.org/10.1016/j.thorsurg.2020.04.004. e-pub ahead of print 2020/07/01.
Norris CM, Close JCT. Prehabilitation for the frailty syndrome: improving outcomes for our most vulnerable patients. Anesth Analg. 2020;130:1524–33. https://doi.org/10.1213/ANE.0000000000004785. e-pub ahead of print 2020/05/10.
Subramaniam A, Tiruvoipati R, Lodge M, Moran C, Srikanth V. Frailty in the older person undergoing elective surgery: a trigger for enhanced multidisciplinary management - a narrative review. ANZ J Surg. 2020;90:222–9. https://doi.org/10.1111/ans.15633. e-pub ahead of print 2020/01/10.
Urits I, Orhurhu V, Jones M, Hoyt D, Seats A, Viswanath O. Current Perspectives on Postoperative Cognitive Dysfunction in the Ageing Population. Turk J Anaesthesiol Reanim. 2019;47:439–47. https://doi.org/10.5152/TJAR.2019.75299. e-pub ahead of print 2019/12/13.
Kow AW. Prehabilitation and Its Role in Geriatric Surgery. Ann Acad Med Singap. 2019;48:386–92. e-pub ahead of print 2020/01/22.
Czobor NR, Lehot JJ, Holndonner-Kirst E, Tully PJ, Gal J, Szekely A. Frailty In Patients Undergoing Vascular Surgery: a Narrative Review Of Current Evidence. Ther Clin Risk Manag. 2019;15:1217–32. https://doi.org/10.2147/TCRM.S217717. e-pub ahead of print 2019/12/06.
Author information
Authors and Affiliations
Contributions
PJS collected the data, analyzed the data, wrote the paper, revised the paper, and secured funding for the project; ML collected the data, analyzed the data, revised the paper; YL collected the data, analyzed the data, and revised the paper; KR collected the data, analyzed the data, and revised the paper; JCT collected the data, analyzed the data, and revised the paper; LB collected the data, analyzed the data, and revised the paper; AP collected the data and revised the paper; AA collected the data, analyzed the data, and revised the paper; SR collected the data, analyzed the data, and revised the paper; TC revised the paper; CG revised the paper; MH revised the paper; GL revised the paper; RL revised the paper; DR revised the paper; SS revised the paper; KS revised the paper; NC revised the paper; ADS analyzed the data, revised the paper, and secured funding for the project.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Smith, P.J., Lew, M., Lowder, Y. et al. Cognitive impairment in candidates for allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 57, 89–94 (2022). https://doi.org/10.1038/s41409-021-01470-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-021-01470-z