Abstract
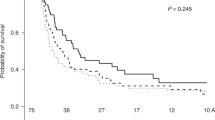
Haploidentical related donor transplantation (haplo-HCT) is associated with cytokine release syndrome (CRS). We conducted a multicenter retrospective study to analyze risk factors for CRS and outcomes after haplo-HCT. We included 451 patients from four academic centers receiving both peripheral blood and bone marrow grafts. Severe CRS was more common with PB vs. BM grafts (19.5% vs 4.9%, OR 2.9, p = 0.05). Multivariable analysis identified recipient CMV sero-positivity, prior transplant, HCT-CI score and donor–recipient sex mismatch as risk factors for severe CRS. Outcomes were analyzed with no CRS as the comparison group. Overall survival (OS) was superior with mild CRS (HR 0.64, p = 0.05) and worst with severe CRS (HR 2.12, p = 0.0038). Relapse risk was significantly decreased in both mild CRS (HR 0.38, p < 0.0001) and severe CRS (HR 0.17, p < 0.0001) groups. The risk of non-relapse mortality was notably higher in severe CRS group (HR 8.0, p < 0.0001), but not in mild CRS group. Acute GVHD was similar among groups. Chronic GVHD at 1 year was 18.5% for no CRS, 23% for mild CRS, and 4.3% for severe CRS (p = 0.0023), with the competing risk of early mortality and short follow up of surviving patients contributing to the low chronic GVHD rates in the severe CRS group.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant 2008;14:641–50.
Colson YL, Wren SM, Schuchert MJ, Patrene KD, Johnson PC, Boggs SS, et al. A nonlethal conditioning approach to achieve durable multilineage mixed chimerism and tolerance across major, minor, and hematopoietic histocompatibility barriers. J Immunol. 1995;155:4179–88.
Luznik L, O’Donnell PV, Fuchs EJ. Post-transplantation cyclophosphamide for tolerance induction in HLA-haploidentical bone marrow transplantation. Semin Oncol. 2012;39:683–93. https://doi.org/10.1053/j.seminoncol.2012.09.005.
Ciurea SO, Zhang MJ, Bacigalupo AA, Bashey A, Appelbaum FR, Aljitawi OS, et al. Haploidentical transplant with posttransplant cyclophosphamide vs matched unrelated donor transplant for acute myeloid leukemia. Blood. 2015;126:1033–40.
Kanate AS, Mussetti A, Kharfan-Dabaja MA, Ahn KW, Digilio A, Beitinjaneh A, et al. Reduced-intensity transplantation for lymphomas using haploidentical related donors vs HLA-matched unrelated donors. Blood. 2016;127:938–47.
Ghosh N, Karmali R, Rocha V, Ahn KW, DiGilio A, Hari PN, et al. Reduced-intensity transplantation for lymphomas using haploidentical related donors versus HLA-matched sibling donors: A center for international blood and marrow transplant research analysis. J Clin Oncol. 2016;34:3141–9.
Dreger P, Sureda A, Ahn KW, Eapen M, Litovich C, Finel H, et al. PTCy-based haploidentical vs matched related or unrelated donor reduced-intensity conditioning transplant for DLBCL. Blood Adv. 2019;3:360–9.
Bashey A, Zhang MJ, McCurdy SR, St Martin A, Argall T, Anasetti C, et al. Mobilized peripheral blood stem cells versus unstimulated bone marrow as a graft source for T-cell–replete haploidentical donor transplantation using post-transplant cyclophosphamide. J Clin Oncol. 2017;35:3002–9.
Bashey A, Zhang X, Sizemore CA, Manion K, Brown S, Holland HK, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol. 2013;31:1310–6.
Huselton E, Slade M, DiPersio JF, Westervelt P, Vij R, Uy GL, et al. Single institution experience with G-CSF mobilized T-cell replete haploidentical hematopoietic cell transplantation. Bone Marrow Transpl. 2017;52:769–71. http://www.nature.com/articles/bmt2016354
Rashidi A, Hamadani M, Zhang M, Wang H, Abdel-azim H, Aljurf M, et al. Outcomes of haploidentical vs matched sibling transplantation for acute myeloid leukemia in fi rst complete remission. Blood Adv. 2019;3:1826–36.
Tisoncik JR, Korth MJ, Simmons CP, Farrar J, Martin TR, Katze MG. Into the eye of the cytokine storm. Microbiol Mol Biol Rev. 2012;76:16–32.
Lee DW, Gardner R, Porter DL, Louis CU, Ahmed N, Jensen M. et al. Current concepts in the diagnosis and management of cytokine release syndrome. Blood. 2014;124:188–95.
Maude SL, Frey N, Shaw PA, Aplenc R, Barrett DM, Bunin NJ, et al. Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med. 2014;371:1507–17. http://www.nejm.org/doi/full/10.1056/NEJMoa1407222
Davila ML, Riviere I, Wang X, Bartido S, Park J, Curran K, et al. Efficacy and toxicity management of 19-28z CAR T cell therapy in B cell acute lymphoblastic leukemia. Sci Transl Med. 2014;6:224ra25. http://www.ncbi.nlm.nih.gov/pubmed/24553386
Grupp SA, Kalos M, Barrett D, Aplenc R, Porter DL, Rheingold SR, et al. Chimeric antigen receptor–modified t cells for acute lymphoid leukemia. N Engl J Med. 2013;368:1509–18. http://www.nejm.org/doi/abs/10.1056/NEJMoa1215134
Suntharalingam G, Perry MR, Ward S, Brett SJ, Castello-Cortes A, Brunner MD, et al. Cytokine storm in a phase 1 trial of the anti-CD28 monoclonal antibody TGN1412. N Engl J Med. 2006;355:1018–28. 2006/08/16
Wing MG, Moreau T, Greenwood J, Smith RM, Hale G, Isaacs J, et al. Mechanism of first-dose cytokine-release syndrome by CAMPATH 1-H: involvement of CD16 (FcgammaRIII) and CD11a/CD18 (LFA-1) on NK cells. J Clin Invest. 1996;98:2819–26. 1996/12/15
Winkler U, Jensen M, Manzke O, Schulz H, Diehl V, Engert A. Cytokine-release syndrome in patients with B-cell chronic lymphocytic leukemia and high lymphocyte counts after treatment with an anti-CD20 monoclonal antibody (rituximab, IDEC-C2B8). Blood. 1999;94:2217–24. 1999/09/25
Colvin GA, Berz D, Ramanathan M, Winer ES, Fast L, Elfenbein GJ, et al. Nonengraftment haploidentical cellular immunotherapy for refractory malignancies: tumor responses without chimerism. Biol Blood Marrow Transpl. 2009;15:421–31. https://doi.org/10.1016/j.bbmt.2008.12.503. [Internet]Available from
Abboud R, Keller J, Slade M, DiPersio JF, Westervelt P, Rettig MP, et al. Severe Cytokine-release syndrome after T cell–replete peripheral blood haploidentical donor transplantation is associated with poor survival and anti–IL-6 therapy is safe and well tolerated. Biol Blood Marrow Transpl. 2016;22:1851–60. https://doi.org/10.1016/j.bbmt.2016.06.010
Raj RV, Hamadani M, Szabo A, Pasquini MC, Shah NN, Drobyski WR, et al. Peripheral blood grafts for T cell–replete haploidentical transplantation increase the incidence and severity of cytokine release syndrome. Biol Blood Marrow Transpl. 2018;24:1664–70. https://doi.org/10.1016/j.bbmt.2018.04.010. [Internet]Available from
Mariotti J, Taurino D, Marino F, Bramanti S, Sarina B, Morabito L, et al. Pretransplant active disease status and HLA class II mismatching are associated with increased incidence and severity of cytokine release syndrome after haploidentical transplantation with posttransplant cyclophosphamide. Cancer Med. 2020;9:52–61.
Imus PH, Blackford AL, Bettinotti M, Luznik L, Fuchs EJ, Huff CA, et al. Severe cytokine release syndrome after haploidentical peripheral blood stem cell transplantation. Biol Blood Marrow Transplant. 2019;000:1–7.
O’Donnell P, Raj K, Pagliuca A. High fever occurring 4 to 5 days post-transplant of haploidentical bone marrow or peripheral blood stem cells after reduced-intensity conditioning associated with the use of post-transplant cyclophosphamide as prophylaxis for graft-versus-host disease. Biol Blood Marrow Transplant. 2015;21:197–8. http://linkinghub.elsevier.com/retrieve/pii/S1083879114006338
Austin PC, Tu JV. Bootstrap Methods for Developing Predictive Models. Am Stat. 2004;58:131–7.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transpl. 1995;15:825–8.
Schoemans HM, Lee SJ, Ferrara JL, Wolff D, Levine JE, Schultz KR, et al. EBMT−NIH−CIBMTR Task Force position statement on standardized terminology & guidance for graft-versus-host disease assessment. Bone Marrow Transplant. 2018;53:1401–15.
Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, et al. Validation and refinement of the Disease Risk Index for allogeneic stem cell transplantation. Blood. 2014;123:3664–71.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG. et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
Abid MB, Hamadani M, Szabo A, Hari PN, Graham MB, Frank MO, et al. Severity of cytokine release syndrome and its association with infections after T cell-replete haploidentical related donor transplantation. Biol Blood Marrow Transplant. 2020;26:1670–8.
Kennedy GA, Tey SK, Buizen L, Varelias A, Gartlan KH, Curley C, et al. A phase 3 double-blind study of the addition of tocilizumab vs placebo to cyclosporin/methotrexate GVHD prophylaxis. Blood. 2021;137:1970–9. https://ashpublications.org/blood/article/137/14/1970/475035/A-phase-3-double-blind-study-of-the-addition-of
Wachsmuth LP, Patterson MT, Eckhaus MA, Venzon DJ, Kanakry CG. Optimized timing of post-transplantation cyclophosphamide in MHC-haploidentical murine hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2020;26:230–41.
Ruggeri A, Labopin M, Battipaglia G, Chiusolo P, Tischer J, Diez-Martin JL, et al. Timing of post-transplantation cyclophosphamide administration in haploidentical transplantation: a comparative study on behalf of the acute leukemia working party of the European Society for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2020;26:1915–22.
McCurdy SR, Muth ST, Tsai HL, Symons HJ, Huff CA, Matsui WH, et al. Early fever after haploidentical bone marrow transplantation correlates with class II HLA-mismatching and myeloablation but not outcomes. Biol Blood Marrow Transplant. 2018;24:2056–64.
Acknowledgements
RA is supported by the American Society of Hematology Clinical Research Training Institute, the American Society of Hematology Research Training Award for Fellows, and the National Cancer Institute of the National Institutes of Health under Award Number R25 CA190190.
Author information
Authors and Affiliations
Contributions
RA and SC designed and performed research, analyzed data, and authored the manuscript. JM, MA, LC, RR, and MH performed research and critically reviewed the manuscript. WF analyzed data and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
RA has research funding from Incyte Corporation. MH has research support/funding from: Takeda Pharmaceutical Company; Spectrum Pharmaceuticals; Astellas Pharma. Consultancy: Janssen; Incyte Corporation; ADC Therapeutics; Celgene Corporation; Omeros, Verastem, MorphoSys. Speaker’s Bureau: Sanofi Genzyme, AstraZeneca, BeiGene. The authors have no other conflicts relevant to this publication.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Abboud, R., Wan, F., Mariotti, J. et al. Cytokine release syndrome after haploidentical hematopoietic cell transplantation: an international multicenter analysis. Bone Marrow Transplant 56, 2763–2770 (2021). https://doi.org/10.1038/s41409-021-01403-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-021-01403-w
This article is cited by
-
Impact of donor age and relationship on outcomes of peripheral blood haploidentical hematopoietic cell transplantation
Bone Marrow Transplantation (2023)
-
Acute kidney injury caused by haplostorm after allogenic hematopoietic stem cell transplant
Bone Marrow Transplantation (2022)