Abstract
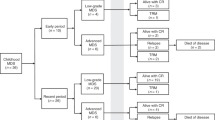
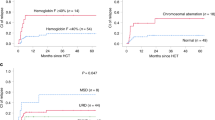
Allogeneic hematopoietic stem cell transplantation (HSCT) is the only curable treatment option for adolescent and young adult (AYA) patients with myelodysplastic syndrome (MDS). The study aim was to evaluate epidemiological data and identify prognostic factors for AYA patients with MDS undergoing allogeneic HSCT. Here, 645 patients were selected from patients enrolled in a multicenter prospective registry for HSCT from 2000 to 2015. The primary endpoint was 3-year overall survival (OS). Survival rates were estimated using the Kaplan–Meier method. Prognostic factors were identified using the multivariable Cox proportional hazards model. The 3-year OS was 71.2% (95% confidence interval [CI]: 67.4–74.6%). In multivariable analysis, active disease status (adjusted hazard ratio: 1.54, 95% CI: 1.09–2.18, p = 0.016), poor cytogenetic risk (1.62, 1.12–2.36, p = 0.011), poor performance status (2.01, 1.13–3.56, p = 0.016), human leukocyte antigen (HLA)-matched unrelated donors (2.23, 1.39–3.59, p < 0.001), HLA-mismatched unrelated donors (2.16, 1.09–4.28, p = 0.027), and cord blood transplantation (2.44, 1.43–4.17, p = 0.001) were significantly associated with poor 3-year OS. In conclusion, in AYA patients with MDS the 3-year OS following allogeneic HSCT was 71.2%. Active disease status, poor cytogenetic risk, poor performance status, and donor sources other than related donors were associated with poor 3-year OS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Lindsley RC, Saber W, Mar BG, Redd R, Wang T, Haagenson MD, et al. Prognostic mutations in myelodysplastic syndrome after stem-cell transplantation. N. Engl J Med. 2017;376:536–47.
de Witte T, Hermans J, Vossen J, Bacigalupo A, Meloni G, Jacobsen N, et al. Haematopoietic stem cell transplantation for patients with myelo-dysplastic syndromes and secondary acute myeloid leukaemias: a report on behalf of the Chronic Leukaemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT). Br J Haematol. 2000;110:620–30.
Sierra J, Pérez WS, Rozman C, Carreras E, Klein JP, Rizzo JD, et al. Bone marrow transplantation from HLA-identical siblings as treatment for myelodysplasia. Blood. 2002;100:1997–2004.
Aoki K, Ishikawa T, Ishiyama K, Aoki J, Itonaga H, Fukuda T, et al. Allogeneic haematopoietic cell transplantation with reduced-intensity conditioning for elderly patients with advanced myelodysplastic syndromes: a nationwide study. Br J Haematol. 2015;168:463–6.
Park S-S, Jeon Y-W, Min GJ, Park S, Yahng S-A, Yoon J-H, et al. Graft-versus-host disease-free, relapse-free survival after allogeneic stem cell transplantation for myelodysplastic syndrome. Biol Blood Marrow Transpl J Am Soc Blood Marrow Transpl. 2019;25:63–72.
Lim Z, Brand R, Martino R, van Biezen A, Finke J, Bacigalupo A, et al. Allogeneic hematopoietic stem-cell transplantation for patients 50 years or older with myelodysplastic syndromes or secondary acute myeloid leukemia. J Clin Oncol J Am Soc Clin Oncol. 2010;28:405–11.
Itonaga H, Ishiyama K, Aoki K, Aoki J, Ishikawa T, Uchida N, et al. Increased opportunity for prolonged survival after allogeneic hematopoietic stem cell transplantation in patients aged 60-69 years with myelodysplastic syndrome. Ann Hematol. 2019;98:1367–81.
Genovese G, Kähler AK, Handsaker RE, Lindberg J, Rose SA, Bakhoum SF, et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. N Engl J Med. 2014;371:2477–87.
Fenaux P, Haase D, Sanz GF, Santini V, Buske C.ESMO Guidelines Working Group Myelodysplastic syndromes: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol J Eur Soc Med Oncol. 2014;25:iii57–69.
Miyazaki Y. JSH Guideline for Tumors of Hematopoietic and Lymphoid Tissues: Leukemia: 6. Myelodysplastic syndromes (MDS). Int J Hematol. 2017;106:151–9.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–55.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–88.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M, et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transpl J Am Soc Blood Marrow Transpl. 2009;15:367–9.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transpl J Am Soc Blood Marrow Transpl. 2009;15:1628–33.
Davies SM, Kollman C, Anasetti C, Antin JH, Gajewski J, Casper JT, et al. Engraftment and survival after unrelated-donor bone marrow transplantation: a report from the national marrow donor program. Blood. 2000;96:4096–102.
Bensinger WI, Martin PJ, Storer B, Clift R, Forman SJ, Negrin R, et al. Transplantation of bone marrow as compared with peripheral-blood cells from HLA-identical relatives in patients with hematologic cancers. N Engl J Med. 2001;344:175–81.
Sullivan KM, Agura E, Anasetti C, Appelbaum F, Badger C, Bearman S, et al. Chronic graft-versus-host disease and other late complications of bone marrow transplantation. Semin Hematol. 1991;28:250–9.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant. 1995;15:825–8.
Yucel OK, Saliba RM, Rondon G, Ahmed S, Alousi A, Bashir Q, et al. Cytogenetics and comorbidity predict outcomes in older myelodysplastic syndrome patients after allogeneic stem cell transplantation using reduced intensity conditioning. Cancer. 2017;123:2661–70.
Barba P, Martino R, Zhou Q, Cho C, Castro-Malaspina H, Devlin S, et al. CD34+ cell selection versus reduced-intensity conditioning and unmodified grafts for allogeneic hematopoietic cell transplantation in patients age >50 years with acute myelogenous leukemia and myelodysplastic syndrome. Biol Blood Marrow Transpl J Am Soc Blood Marrow Transpl. 2018;24:964–72.
Atallah E, Logan B, Chen M, Cutler C, Deeg J, Jacoby M et al. Comparison of patient age groups in transplantation for myelodysplastic syndrome: The Medicare Coverage With Evidence Development Study. JAMA Oncol. 2019. https://doi.org/10.1001/jamaoncol.2019.5140.
Tomizawa D, Tanaka S, Kondo T, Hashii Y, Arai Y, Kudo K, et al. Allogeneic hematopoietic stem cell transplantation for adolescents and young adults with acute myeloid leukemia. Biol Blood Marrow Transpl J Am Soc Blood Marrow Transpl. 2017;23:1515–22.
Sorror ML, Storb RF, Sandmaier BM, Maziarz RT, Pulsipher MA, Maris MB, et al. Comorbidity-age index: a clinical measure of biologic age before allogeneic hematopoietic cell transplantation. J Clin Oncol J Am Soc Clin Oncol. 2014;32:3249–56.
Yanada M, Takami A, Yamasaki S, Arai Y, Konuma T, Uchida N, et al. Allogeneic hematopoietic cell transplantation for adults with acute myeloid leukemia conducted in Japan during the past quarter century. Ann Hematol. 2020;99:1351–60.
Pavlů J, Labopin M, Niittyvuopio R, Socié G, Yakoub-Agha I, Wu D, et al. Measurable residual disease at myeloablative allogeneic transplantation in adults with acute lymphoblastic leukemia: a retrospective registry study on 2780 patients from the acute leukemia working party of the EBMT. J Hematol OncolJ Hematol Oncol. 2019;12:108.
Gerds AT, Woo Ahn K, Hu Z-H, Abdel-Azim H, Akpek G, Aljurf M, et al. Outcomes after umbilical cord blood transplantation for myelodysplastic syndromes. Biol Blood Marrow Transpl J Am Soc Blood Marrow Transpl. 2017;23:971–9.
Scheid C, de Wreede L, van Biezen A, Koenecke C, Göhring G, Volin L, et al. Validation of the revised IPSS at transplant in patients with myelodysplastic syndrome/transformed acute myelogenous leukemia receiving allogeneic stem cell transplantation: a retrospective analysis of the EBMT chronic malignancies working party. Bone Marrow Transpl. 2017;52:1519–25.
Saber W, Cutler CS, Nakamura R, Zhang M-J, Atallah E, Rizzo JD, et al. Impact of donor source on hematopoietic cell transplantation outcomes for patients with myelodysplastic syndromes (MDS). Blood. 2013;122:1974–82.
Robin M, Ruggeri A, Labopin M, Niederwieser D, Tabrizi R, Sanz G, et al. Comparison of unrelated cord blood and peripheral blood stem cell transplantation in adults with myelodysplastic syndrome after reduced-intensity conditioning regimen: a collaborative study from Eurocord (Cord blood Committee of Cellular Therapy & Immunobiology Working Party of EBMT) and Chronic Malignancies Working Party. Biol Blood Marrow Transpl J Am Soc Blood Marrow Transpl. 2015;21:489–95.
Kennedy JA, Ebert BL. Clinical implications of genetic mutations in myelodysplastic syndrome. J Clin Oncol J Am Soc Clin Oncol. 2017;35:968–74.
Alter BP. Inherited bone marrow failure syndromes: considerations pre- and posttransplant. Blood. 2017;130:2257–64.
Shimamura A, Alter BP. Pathophysiology and management of inherited bone marrow failure syndromes. Blood Rev. 2010;24:101–22.
Perl AE, Martinelli G, Cortes JE, Neubauer A, Berman E, Paolini S, et al. Gilteritinib or chemotherapy for relapsed or refractory FLT3-mutated AML. N Engl J Med. 2019;381:1728–40.
DiNardo CD, Stein EM, de Botton S, Roboz GJ, Altman JK, Mims AS, et al. Durable remissions with ivosidenib in IDH1-mutated relapsed or refractory AML. N. Engl J Med. 2018;378:2386–98.
Lehmann S, Bykov VJN, Ali D, Andrén O, Cherif H, Tidefelt U, et al. Targeting p53 in vivo: a first-in-human study with p53-targeting compound APR-246 in refractory hematologic malignancies and prostate cancer. J Clin Oncol J Am Soc Clin Oncol. 2012;30:3633–9.
Platzbecker U. Treatment of MDS. Blood. 2019;133:1096–107.
Tremolada M, Bonichini S, Taverna L, Basso G, Pillon M. Health-related quality of life in AYA cancer survivors who underwent HSCT compared with healthy peers. Eur J Cancer Care. 2018;27:e12878.
Husson O, Huijgens PC, van der Graaf WTA. Psychosocial challenges and health-related quality of life of adolescents and young adults with hematologic malignancies. Blood. 2018;132:385–92.
Gerstl B, Sullivan E, Chong S, Chia D, Wand H, Anazodo A. Reproductive outcomes after a childhood and adolescent young adult cancer diagnosis in female cancer survivors: a systematic review and meta-analysis. J Adolesc Young Adult Oncol. 2018. https://doi.org/10.1089/jayao.2018.0036.
Fernandez C, Fraser GAM, Freeman C, Grunfeld E, Gupta A, Mery LS, et al. Principles and recommendations for the provision of healthcare in Canada to adolescent and young adult-aged cancer patients and survivors. J Adolesc Young Adult Oncol. 2011;1:53–9.
Acknowledgements
The authors thank the medical and nursing staff of our institution and would like to express their gratitude to the Japan Society of Clinical Research (http://www.japanscr.org/) for valuable support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shimomura, Y., Hara, M., Konuma, T. et al. Allogeneic hematopoietic stem cell transplantation for myelodysplastic syndrome in adolescent and young adult patients. Bone Marrow Transplant 56, 2510–2517 (2021). https://doi.org/10.1038/s41409-021-01324-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-021-01324-8
This article is cited by
-
Impact of gene alterations on clinical outcome in young adults with myelodysplastic syndromes
Scientific Reports (2023)
-
Identifying the optimal conditioning intensity for stem cell transplantation in patients with myelodysplastic syndrome: a machine learning analysis
Bone Marrow Transplantation (2023)
-
Clinical trials: design, endpoints and interpretation of outcomes
Bone Marrow Transplantation (2022)