Abstract
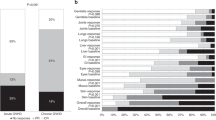
Steroid-refractory (SR) acute gastrointestinal (GI) graft-versus-host disease (GVHD) is associated with significant mortality in allogeneic hematopoietic cell transplantation recipients. We retrospectively evaluated the efficacy of tocilizumab for the treatment of SR biopsy-proven acute lower GI GVHD in 16 consecutive adult transplant recipients between October 2015 and July 2016. Tocilizumab 8 mg/kg was administered every 2 weeks until achievement of complete response, defined as resolution of all manifestations of GI GVHD, or until patients had progression or initiation of other therapy. Ten of 16 patients (62.5%; 95% CI, 0.39–82) achieved a complete response after a median time of 11 days (range, 2–28 days) from tocilizumab initiation. The median time to response onset (improvement in stage by at least 1) was 1 day (range, 1–4 days). Tocilizumab was administered at a median of 9 days (range, 3–75 days) from GVHD diagnosis and 10 days (range, 3–75 days) from initiation of high-dose steroids. At a median follow-up of 7.6 months (range, 0.8–27.7 months) from initiation of tocilizumab, 6/16 (37.5%) patients are alive and free of their underlying hematologic malignancy. Tocilizumab appears to be a highly active agent for the treatment of severe SR lower GI acute GVHD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
D’Souza A, Fretham C Current Uses and Outcomes of Hematopoietic Cell Transplantation (HCT): CIBMTR Summary Slides, 2017. Available at: http://www.cibmtr.org
Jagasia M, Arora M, Flowers ME, Chao NJ, McCarthy PL, Cutler CS, et al. Risk factors for acute GVHD and survival after hematopoietic cell transplantation. Blood. 2012;119:296–307.
Pavletic SZ, Fowler DH. Are we making progress in GVHD prophylaxis and treatment? Hematol Am Soc Hematol Educ Program. 2012;2012:251–64.
Xhaard A, Rocha V, Bueno B, de Latour RP, Lenglet J, Petropoulou A, et al. Steroid-refractory acute GVHD: Lack of long-term improved survival using new generation anticytokine treatment. Biol Blood Marrow Transplant. 2012;18:406–13.
Castilla-Llorente C, Martin PJ, McDonald GB, Storer BE, Appelbaum FR, Deeg HJ, et al. Prognostic factors and outcomes of severe gastrointestinal graft-vs.-host disease after allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2014;49:966–71.
Martin PJ, McDonald GB, Sanders JE, Anasetti C, Appelbaum FR, Deeg HJ, et al. Increasingly frequent diagnosis of acute gastrointestinal graft-versus-host disease after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2004;10:320–27.
Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta. 2011;1813:878–88.
Tvedt THA, Ersvaer E, Tveita AA, Bruserud O. Interleukin-6 in allogeneic stem cell transplantation: its possible importance for immunoregulation and as a therapeutic target. Front Immunol. 2017;8:1–15.
Chen X, Das R, Komorowski R, Beres A, Hessner MJ, Mihara M, et al. Blockade of interleukin-6 signaling augments regulatory T-cell reconstitution and attenuates the severity of graft-versus-host disease. Blood. 2009;114:891–900.
Tawara I, Koyama M, Liu C, Toubai T, Thomas D, Evers R, et al. Interleukin-6 modulates graft-versus-host responses after experimental allogeneic bone marrow transplantation. Clin Cancer Res. 2011;17:77–88.
Drobyski WR, Pasquini M, Kovatovic K, Palmer J, Douglas Rizzo J, Saad A, et al. Tocilizumab for the treatment of steroid refractory graft-versus-host disease. Biol Blood Marrow Transplant. 2011;17:1862–68.
Roddy JV, Haverkos BM, McBride A, Leininger KM, Jaglowski S, Penza S, et al. Tocilizumab for steroid refractory acute graft-versus-host disease. Leuk Lymphoma. 2016;57:81–5.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant. 1995;15:825–8.
Noguchi D, Wakita D, Ohkuri T, Tajima M, Chamoto K, Kitamura H, et al. Blockade of IL-6-signaling inhibits the pathogenesis of CD4+T cell-mediated lethal graft-versus-host reaction against minor histocompatibility antigen. Immuno Lett. 2011;136:146–55.
Bhatt S, Schulz G, Towerman A, Hente M, Shenoy S. Tocilizumab for the treatment of steroid refractory acute graft versus host disease: a pediatric experience. Biol Blood Marrow Transplant. 2016;22:S389–S390.
Baker KS, Allen RD, Roths JB, Sidman CL. Kinetic and organ-specific patterns of cytokine expression in acute graft-versus-host disease. Bone Marrow Transplant. 1995;15:595–603.
Jerkins JH, Hamadani M, Zook F, Epperla N, Shaw BE, Saber W, et al. Alpha-1-antitrypsin for the treatment of steroid-refractory acute gastrointestinal graft-versus-host disease. Am J Hematol. 2017;92:E610–E611.
Floisand Y, Lundin KEA, Lazarevic V, Kristiansen JD, Osnes LTN, Tjonnfjord GE, et al. Targeting integrin α4β7 in steroid-refractory intestinal graft-versus-host disease. Biol Blood Marrow Transplant. 2017;23:172–5.
Kennedy GA, Varelias A, Vuckovic S, Le Texier L, Gartlan KH, Zhang P, et al. Addition of interleukin-6 inhibition with tocilizumab to standard graft-versus-host disease prophylaxis after allogeneic stem-cell transplantation: a phase 1/2 trial. Lancet Oncol. 2014;15:1451–9.
Drobyski WR, Szabo A, Zhu F, Keever-Taylor C, Hebert KM, Dunn R, et al. Tocilizumab, tacrolimus, and methotrexate for the prevention of acute graft versus host disease: Low incidence of lower gastrointestinal tract disease. Haematologica. 2018;103:717–27.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ganetsky, A., Frey, N.V., Hexner, E.O. et al. Tocilizumab for the treatment of severe steroid-refractory acute graft-versus-host disease of the lower gastrointestinal tract. Bone Marrow Transplant 54, 212–217 (2019). https://doi.org/10.1038/s41409-018-0236-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-018-0236-z
This article is cited by
-
Current and Emerging Targeted Therapies for Acute Graft-Versus-Host Disease
BioDrugs (2021)
-
IL-6 trans-signaling promotes the expansion and anti-tumor activity of CAR T cells
Leukemia (2021)
-
Healthcare utilization and financial impact of acute-graft-versus host disease among children undergoing allogeneic hematopoietic cell transplantation
Bone Marrow Transplantation (2020)
-
Tocilizumab in transplantation
European Journal of Clinical Pharmacology (2020)
-
Tocilizumab
Reactions Weekly (2019)