Abstract
There are disparities in outcomes for patients with multiple myeloma (MM). We evaluated the influence of sociodemographic factors on global disparities in outcomes for patients with MM. This rapid evidence assessment (PROSPERO, CRD42021248461) followed PRISMA-P guidelines and used the PICOS framework. PubMed and Embase® were searched for articles in English from 2011 to 2021. The title, abstract, and full text of articles were screened according to inclusion/exclusion criteria. The sociodemographic factors assessed were age, sex, race/ethnicity, socioeconomic status, and geographic location. Outcomes were diagnosis, access to treatment, and patient outcomes. Of 84 articles included, 48 were US-based. Worldwide, increasing age and low socioeconomic status were associated with worse patient outcomes. In the US, men typically had worse outcomes than women, although women had poorer access to treatment, as did Black, Asian, and Hispanic patients. No consistent disparities due to sex were seen outside the US, and for most factors and outcomes, no consistent disparities could be identified globally. Too few studies examined disparities in diagnosis to draw firm conclusions. This first systematic analysis of health disparities in patients with MM identified specific populations affected, highlighting a need for additional research focused on assessing patterns, trends, and underlying drivers of disparities in MM.
Similar content being viewed by others
Introduction
Multiple myeloma (MM) is a hematological malignancy characterized by the clonal proliferation of malignant plasma cells in the bone marrow, the production of monoclonal protein, and multiple organ damage [1, 2]. MM is the second most common hematological malignancy [1, 2]. Globally, the incidence rate is ~2 per 100,000 people but varies considerably [3,4,5]. The highest rates are found in more developed nations such as the United States (US) and those of Australasia and Western Europe (≥4 cases per 100,000 people) [3, 4], probably due to greater awareness of the disease and better and more available diagnostic techniques [2]. Correspondingly, incidence rates are lower in less developed nations, such as those in Latin America, Asia, and Africa, where incidence rates are ≤2 cases per 100,000 people [3, 4, 6].
The etiology of MM is unknown and may be multifactorial [2]. Disparities exist in MM incidence and outcomes, including deaths. These disparities are partly caused by sociodemographic factors, such as age, sex, race/ethnicity, socioeconomic status, and geographic location, affecting healthcare utilization patterns, trends in treatment including access to clinical trials, and outcomes [7,8,9,10]. For instance, in the US, Black patients have a twofold increased risk of MM and are diagnosed with MM at younger ages compared with White patients [9,10,11] (note that descriptions of race/ethnicity throughout this article are based on those reported in the studies that met the inclusion criteria and were included for assessment). Moreover, despite recent therapeutic advances [12], improvements in outcomes have not been uniform among racial and ethnic minorities [13,14,15,16] or in patients diagnosed at an older age [14, 17]. Therefore, as improvements in the treatment of MM continue with the development of new agents or treatment paradigms, it is important to further identify disparities among patients and to inform and implement strategies to ensure equitable treatment for all, improve access to clinical trials, and improve standards of care [7, 10].
To the best of our knowledge, no systematic reviews have previously evaluated the global effects of sociodemographic factors on disparities in outcomes for patients with MM. Due to this lack of synthesized evidence, we conducted a rapid evidence assessment as the first systematic review of the topic in the published literature. The aim of the rapid evidence assessment was to highlight the impact of different sociodemographic factors on outcomes in patients with MM. Further, the identified disparities will inform areas for future research to improve access to equitable treatment, standards of care, and clinical trials.
Materials and methods
The rapid evidence assessment was prospectively registered with the Prospective Register of Systematic Reviews (PROSPERO, registration number CRD42021248461; www.crd.york.ac.uk/prospero/) to avoid duplication and reduce potential reporting bias. The protocol followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocol (PRISMA-P) guidelines [18] and defined all the processes and methodologies used. The assessment was conducted using the PICOS (population, intervention, comparison, outcome, and study type) framework for study selection and inclusion. Observational and real-world evidence studies were included in the meta-analysis. Preclinical studies, clinical studies, case studies, notes, commentaries, editorials, opinions, economic model studies, meta-analyses, reviews, and congress abstracts were excluded. Full inclusion and exclusion criteria for the studies included in this rapid evidence assessment are listed in Table 1.
Search strategy
Searches for published articles in English from 2011 to 2021 were conducted in PubMed and Embase®, excluding congress abstracts. A hand search of reference lists from relevant systematic literature reviews was also conducted to identify any articles that did not appear in the database searches. After duplicates were identified and removed, returned articles were screened for eligibility at level 1 (title and abstract) by a single reviewer according to the inclusion and exclusion criteria, and 20% of all screened articles were quality checked by a second reviewer. Discrepancies were discussed between reviewers until a consensus was reached, and if no consensus was reached the article was moved to level 2 screening. At level 2 screening, a single reviewer screened the full text of articles against the same inclusion and exclusion criteria, and 20% of all screened articles were quality checked by a second reviewer. Reasons for exclusion were recorded and cross-checked between the two reviewers, and a third reviewer was consulted for any discrepancies. The quality of the studies was assessed using the Newcastle–Ottawa Scale (NOS), with studies scored out of 9 for quality; high scores indicated a low risk of bias, and scores <5 indicated a poor-quality study with a high risk of bias.
Data extraction and analysis
A single reviewer extracted data from studies that fulfilled all the inclusion criteria. All extracted data were then validated for accuracy by a second reviewer. The data elements extracted are listed in Supplementary Table 1. No inference analysis was conducted, and the data are descriptive only.
Results
Included studies, study characteristics, and quality assessment
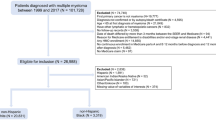
The PRISMA flow diagram for the study is shown in Fig. 1. Overall, 1696 articles were identified, and after the removal of duplicates and exclusion by level 1 (title and abstract) and level 2 (full text) screening, 84 articles were identified as meeting the inclusion criteria. Of these 84 articles, 48 were studies in the US [14,15,16, 19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62], and 36 were studies outside the US (non-US) [63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97]. The full list of all 84 included studies is shown in Supplementary Table 2. Most of the 48 US-based studies used data from the Surveillance, Epidemiology, and End Results (SEER) database (n = 28), the National Cancer Database (NCDB, n = 8), and Medicare records (n = 8). The geographic breakdown of the 36 non-US studies is shown in Fig. 2. Most non-US studies were conducted in Europe (n = 15), followed by Australia and New Zealand (n = 6), Asia (n = 5), and Latin America (n = 4). The most common sociodemographic factors assessed for disparity are shown in Fig. 3. In the US studies, the most common factors assessed were race/ethnicity (n = 43), sex (n = 36), insurance status (n = 17), age (n = 16), and income (n = 12). In the non-US studies, the most common factors assessed were age (n = 29), sex (n = 24), geography (n = 13), and socioeconomic status (n = 10). Assessment of study quality using the NOS showed that all US studies and all but one non-US study had scores ≥5, indicating that no studies were poor quality or at high risk of bias. One non-US study [88] assessed using a modified NOS for cross-sectional studies had a score of 4. This study presented data from a survey of hematologists rather than from a patient registry, therefore the results carry a higher risk of bias. A higher proportion of US studies (94%) were considered high-quality and low-risk (NOS score of 8 or 9) compared with non-US studies (71%).
Assessment of disparity
For the assessment of disparity, the following factors were selected: age, sex, race/ethnicity, socioeconomic status, and geography. These factors were assessed for the following outcomes: diagnosis, treatment access, and patient outcomes. Table 2 shows the number of studies evaluated for each factor by each outcome in the US studies and the studies from other countries/regions. Patient outcome was the most commonly assessed outcome (survival in 27 US and 21 non-US studies, and mortality in 13 US and 16 non-US studies), followed by access to treatment (24 US and 11 non-US studies). Few studies examined disparities in diagnosis (two US and four non-US studies). In the non-US studies, there was heterogeneity in the different measures of mortality, e.g., general mortality rate, early mortality, 5-year excess mortality rate ratio, and age-standardized mortality rate. Heterogeneity among both US and non-US studies was also noted regarding the different measures of access to treatment.
Diagnosis
Only two US studies [14, 26] and four non-US studies (one each in France, Latin America, Mexico, and China) [84, 88, 93, 97] reported on disparities in diagnosis, therefore no clear patterns were observed. Increasing age affected the likelihood of receiving compliant care, including diagnosis [84], and female patients were older at diagnosis than males [14]. Hispanic patients and Black patients were significantly younger at diagnosis than White patients [14, 26]. Compared with patients receiving public healthcare, patients receiving private healthcare had a greater range and availability of diagnostic tests [88], and were less likely to be diagnosed with advanced-stage disease [93]. Patients with higher education levels had a shorter time to diagnosis than those with lower education levels [97]. Finally, patients who lived closer to the center where staging and prognostic procedures were performed were more likely to receive compliant care, including diagnosis [84].
Access to treatment
Fifteen US studies and six non-US studies reported on age and disparities in access to treatment (Supplementary Table 3), with the majority showing that increasing age reduced access to treatment, including stem cell transplantation. Twelve US studies (Supplementary Table 4) and one study each in Europe and Canada reported on sex and access to treatment, most identifying better access to treatment in favor of men [31, 39, 40, 42, 43, 47, 54, 65, 80]. Access to stem cell transplantation was also reported to be worse in females [31, 40], except for one US study which reported that more Black women than Black men underwent autologous stem cell transplantation [26] and one Canadian study reporting no significant effect of sex on access to autologous stem cell transplantation [80]. For race/ethnicity and access to treatment, 19 US studies (Supplementary Table 5) and one study each in the United Kingdom and New Zealand were identified. Among the US studies, most reported worse access to treatment for Black [15, 21, 31, 32, 36, 37, 40, 42, 47, 54, 55], Asian [19, 31, 62], and Hispanic patients [15, 22, 31, 55] compared with White patients. In the US studies, there were trends suggesting that Hispanic patients and Black patients were less likely than White patients to receive stem cell transplantation [20, 22, 31, 32, 37, 40, 55] and that Black patients were more likely to experience delay in receiving stem cell transplantation compared with White patients [26]. In addition, one study in New Zealand observed significantly lower uptake of autologous stem cell transplantation in patients with Maori/Pasifika ethnicity compared with European or other ethnicities [66]. Twelve US studies and seven non-US studies reported on socioeconomic status and access to treatment (Supplementary Table 6), with mixed results. Lower socioeconomic status, whether defined by general socioeconomic status, household income, education level, or insurance status, was generally associated with worse access to treatment, including stem cell transplantation[27, 36, 37, 39, 40, 43, 50, 54, 58, 72, 80, 88, 93, 97], although this was not a universal finding [36, 42, 43, 47, 50, 54, 58, 60, 66, 96]. The effects of geography on access to treatment were reported in five US studies (Supplementary Table 7) and one study each in Canada and France [80, 84]. No consistent findings on differences in access to treatment, including stem cell transplantation, with respect to living in rural, urban, or metropolitan areas were found [40, 42, 43, 54, 80].
Patient outcomes
Twenty-four US and 14 non-US studies reported on age and disparities in survival (Supplementary Table 8), and three US and 11 non-US studies on age and disparities in mortality (Supplementary Table 9). Most studies reported that survival and mortality worsened with increasing age [14, 16, 22, 23, 25, 27, 29, 30, 35, 37, 38, 40, 41, 43, 45, 46, 48, 51, 55,56,57, 59, 61, 66, 67, 69, 71, 73,74,75, 77, 80, 82, 83, 85,86,87, 89, 90, 96, 98].
Nineteen US and 14 non-US studies reported on sex and survival (Supplementary Table 10), and six US and 10 non-US studies on sex and mortality (Supplementary Table 11). Most studies reported no effect of sex on survival or mortality [16, 25, 27, 32, 34, 38, 45, 56, 59, 63, 66, 68, 69, 74, 75, 80, 84, 90, 92, 97]. However, a subset of studies reported more favorable survival in women [14, 22, 29, 40, 41, 43, 48, 55, 61], and mortality rates were generally higher in men [29, 44, 46, 67, 70, 77, 82, 89, 92, 94, 98, 99].
Twenty-four US and four non-US studies reported on race/ethnicity and survival (Supplementary Table 12), and 11 US studies (Supplementary Table 13) and one study in New Zealand on race/ethnicity and mortality. Overall, no clear patterns emerged. A large proportion of studies reported no effect of race/ethnicity on survival or mortality [20, 22,23,24,25,26,27, 30, 32, 34, 38, 41, 45, 46, 55,56,57, 61, 66, 72]. Several studies reported better survival (as measured by overall survival [OS], myeloma-specific survival, 1-year OS, 5-year OS, or relative survival) for Black/African American patients versus White patients [14, 20, 23, 24, 40, 48, 51, 90], although Black/African American patients may have higher mortality rates (as measured by excess mortality, rate ratio, mortality rate, or risk of dying) than White patients [16, 33, 37, 44, 49, 52]. Some studies reported worse survival or mortality for Hispanic versus White patients [14,15,16, 29, 53], but this was not universally reported [15, 20, 23, 30, 34, 43, 46, 48, 53]. Asian patients were generally reported to have better survival versus White, Black/African American, or Hispanic patients [14, 23, 45].
Eleven US and eight non-US studies reported on socioeconomic status and survival (Supplementary Table 14), and three US and six non-US studies on socioeconomic status and mortality (Supplementary Table 15). Lower socioeconomic status, whether defined generally or specifically in terms of income, education level, or insurance status, was associated with worse survival and mortality [23, 27, 29, 35, 37, 38, 40, 41, 43, 44, 48, 56, 63, 66, 69, 72, 78, 90, 91, 93, 97].
Four US and five non-US studies reported on geography and survival (Supplementary Table 16), and two US [44, 46] and five non-US studies (Supplementary Table 17) on geography and mortality. No clear patterns emerged. Differences in survival or mortality for patients in rural versus urban versus metropolitan areas were variable [40, 41, 43, 48, 63, 69, 80, 81, 97, 98]. Comparison of different regions within individual countries, such as the US, Canada, China, and New Zealand, demonstrated varying survival or mortality rates [46, 66, 77, 94].
Discussion
In this rapid evidence assessment, we assessed disparities in MM on a global scale by examining variations in an array of sociodemographic factors such as age, sex, race/ethnicity, socioeconomic status, and geographic location on diagnosis, access to treatment, and patient outcomes. Published literature was assessed using a standardized, thorough, and transparent approach using the PICOS framework for study selection and inclusion. To the best of our knowledge, this is the first formal, comprehensive review of literature that has reported and compared disparities in MM at a global level. It highlights the heterogeneity of the data and the multifactorial nature of disparities in MM and identifies areas for future research to ensure that disparity among patients does not affect equitable treatment.
There were clear disparities in access to treatment and outcomes for some of the sociodemographic factors assessed, with agreement among studies indicative of a global problem. Increasing age was associated with worse access to treatment, and worse access typically occurred in Black, Asian, and Hispanic patients compared with White patients. In addition, Hispanic and Black patients in US studies were less likely to receive stem cell transplantation compared with White patients, and Black patients were more likely to experience delays in access to stem cell transplantation compared with White patients. Access to treatment was also generally worse for women. Increasing age was also associated with worse patient outcomes, as was lower socioeconomic status irrespective of how it was measured. The effect of age on patient outcomes is not necessarily surprising. MM usually affects older patients, and traditionally survival and mortality were worse for older patients because high-dose therapy followed by stem cell transplant was not a valid approach [100]. With the increasing availability of proteasome inhibitors, immunomodulatory drugs, and anti-CD38 therapies, the lack of barriers to their use in older patients, and the adoption of frailty-adapted therapy, the prognosis for older patients continues to improve [101]. Although survival for older patients still lags behind their younger counterparts [30, 102], the disparity in patient outcomes because of age may be potentially resolved in the future. Another clear finding was the disparity in access to treatment for women compared with men, further indicating the need for an increased focus on sex-stratified medicine [103].
Sometimes, no clear pattern could be observed among factors and outcomes. These inconsistent findings might be explained by heterogeneity among studies, for instance in outcome measures, study quality, database size, or type of analysis (e.g., univariate or multivariate), or the country(ies) involved in the study as reflected in patient populations or health systems. This inconsistency may also reflect the multifactorial nature of disparities in MM and the possibility that factors may be confounding and difficult to isolate. For instance, we should consider that identifying single predictive factors of disparity is difficult when it is likely that it is a combination of age, race/ethnicity, and low socioeconomic status, whether defined by income, education, or insurance status, that leads to lack of access to treatment or worse patient outcomes rather than each individual factor alone.
Some studies examining disparities due to race/ethnicity have previously demonstrated an effect of race/ethnicity [11, 13,14,15,16], but this has not been a universal finding [7, 10]. The results from our assessment further emphasize the variability among studies. As noted above, determining the contribution of a single factor such as race/ethnicity on any disparity is difficult because of the confounding nature of multiple, interacting factors. For instance, Black patients often face additional barriers in accessing MM care, leading to delayed diagnosis and later treatment initiation. Moreover, the biology of disease is an important consideration that may vary across different races and ethnicities. A recent study demonstrated superior survival in African American patients compared with White patients when both groups had equal access to healthcare [104], which may reflect differences in disease biology. Disease biology may also be an important consideration for other factors, such as age, and of particular relevance when considering treatment with immunomodulatory drugs.
This rapid evidence assessment is inherently limited by its descriptive nature. Searches were restricted to PubMed and Embase® between 2011 and 2021, and congress abstracts were not included. Only studies in the English language were included. Given the global nature of research into disparities in MM, relevant studies in other languages may have been missed. Data were descriptive only, and no inference analysis was conducted. Only a limited number of sociodemographic factors were assessed for disparity. Other anthropometric or behavioral factors, such as obesity, alcohol use, smoking, marital status, occupational exposure, disease stage, genetic factors, and comorbidities, were not examined and could be confounding factors for patient outcomes affecting the assessment of health disparities. Our study also found heterogeneity among studies in terms of measures for each outcome and type of analysis. Moreover, the US studies had to rely primarily on only a few databases (SEER, n = 28; NCDB, n = 8; Medicare records, n = 8) leading to possible patient overlap and duplication of populations.
This study identifies several areas for possible future research. Of the 84 studies that met the inclusion criteria, 63 (75.0%) were either in the US or Europe. Furthermore, for most outcomes, there was heterogeneity between studies, notably for measures of mortality and treatment access, that may benefit from standardization. New studies outside the US and Europe that utilize standardized outcomes and measures would not only enable the assessment of disparities on a global scale but also enable direct comparison among countries. We found clear disparities due to lower socioeconomic status, which is multifactorial in nature; and disparities due to variations in race/ethnicity may be indirectly affected by associated variations in socioeconomic status or access to treatment [8]. Some sociodemographic factors were assessed in this study, and confounding factors may also be pertinent for patient outcomes, such as those anthropometric or behavioral factors noted above [7]. This would help clinicians to further understand the complex multifactorial nature of MM where different factors may combine to affect patient outcomes, or different factors may influence each other. Given the well-documented improvements in survival over the past 10–20 years [105, 106], future research could focus on changes in disparity over time. Few studies in the US or elsewhere examined disparities in diagnosis, which is of particular importance given differences in the quality, availability, and delivery of diagnostic techniques among countries [2]. This study therefore identifies a clear need for increased research around disparities in diagnosis. Except for a few studies outside the US, for instance in New Zealand [66, 92], somewhat surprisingly the effects of race/ethnicity on disparities in MM have received little attention. Additional studies globally would improve our understanding of this phenomenon, and how to address it.
The disparities we have systematically identified in our rapid evidence assessment of global barriers to accessing treatment for patients with MM align with some of the previously mentioned barriers to accessing treatment and clinical trials such as age, sex, race/ethnicity, and socioeconomic status [7,8,9,10]. Improving access to clinical trials by overcoming some of these barriers would include designing more diverse clinical trials with evidence-based eligibility criteria that promote recruitment and retention, improving physician–patient communication, tailored patient education, and overcoming physical and transportation barriers to clinic visits through telemedicine and home visits [8]. Adopting some of these suggested changes to clinical trials could also improve access to MM treatment in general either directly, for example through improving physician–patient communication, or indirectly by increasing physician and patient confidence that new treatments are effective and appropriate for individual patients.
In conclusion, this study highlights specific populations of patients with MM that remain at a disadvantage and for whom there is potential scope for improvement in outcomes. The study also shows that data are heterogeneous and that certain factors uniformly cause disparity in access to treatment, namely being older, being female, or being Black, Asian, or Hispanic, whereas others are variable and multifactorial in nature, such as lower socioeconomic status. Acknowledging and addressing the causes and effects of disparities in patient outcomes may help to develop novel treatments or treatment strategies for MM, for instance through the enrollment of more diverse and representative patient populations in clinical trials [8], and to improve access to treatment and treatment facilities in the real world. Similarly, acknowledging and addressing the need for standardizing measures of mortality and treatment access across studies is important to improve the evaluation of access and outcomes across patient groups and treatment regimens. This rapid evidence assessment also highlights the need for more comprehensive evaluations of the barriers to treatment in MM. Ultimately, an improved understanding of disparities in MM should help to guide appropriate treatment choices, to ensure that there is equitable treatment for all and that patients derive maximum benefit.
Data availability
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions, and exceptions, Pfizer may also provide access to the related individual de-identified participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.
References
van de Donk N, Pawlyn C, Yong KL. Multiple myeloma. Lancet. 2021;397:410–27.
Kumar SK, Rajkumar V, Kyle RA, van Duin M, Sonneveld P, Mateos MV, et al. Multiple myeloma. Nat Rev Dis Primers. 2017;3:17046.
Cowan AJ, Allen C, Barac A, Basaleem H, Bensenor I, Curado MP, et al. Global burden of multiple myeloma: a systematic analysis for the Global Burden of Disease Study 2016. JAMA Oncol. 2018;4:1221–7.
Zhou L, Yu Q, Wei G, Wang L, Huang Y, Hu K, et al. Measuring the global, regional, and national burden of multiple myeloma from 1990 to 2019. BMC Cancer. 2021;21:606.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Curado MP, Oliveira MM, Silva DRM, Souza DLB. Epidemiology of multiple myeloma in 17 Latin American countries: an update. Cancer Med. 2018;7:2101–8.
Ailawadhi S, Bhatia K, Aulakh S, Meghji Z, Chanan-Khan A. Equal treatment and outcomes for everyone with multiple myeloma: are we there yet? Curr Hematol Malig Rep. 2017;12:309–16.
Habr D, Corsaro M. Reimagining diversity in multiple myeloma clinical trials. Hematol Oncol. 2022;40:689–94.
Kazandjian D. Multiple myeloma epidemiology and survival: a unique malignancy. Semin Oncol. 2016;43:676–81.
Ganguly S, Mailankody S, Ailawadhi S. Many shades of disparities in myeloma care. Am Soc Clin Oncol Educ Book. 2019;39:519–29.
Marinac CR, Ghobrial IM, Birmann BM, Soiffer J, Rebbeck TR. Dissecting racial disparities in multiple myeloma. Blood Cancer J. 2020;10:19.
Cowan AJ, Green DJ, Kwok M, Lee S, Coffey DG, Holmberg LA, et al. Diagnosis and management of multiple myeloma: a review. JAMA. 2022;327:464–77.
Waxman AJ, Mink PJ, Devesa SS, Anderson WF, Weiss BM, Kristinsson SY, et al. Racial disparities in incidence and outcome in multiple myeloma: a population-based study. Blood. 2010;116:5501–6.
Ailawadhi S, Aldoss IT, Yang D, Razavi P, Cozen W, Sher T, et al. Outcome disparities in multiple myeloma: a SEER-based comparative analysis of ethnic subgroups. Br J Haematol. 2012;158:91–8.
Ailawadhi S, Parikh K, Abouzaid S, Zhou Z, Tang W, Clancy Z, et al. Racial disparities in treatment patterns and outcomes among patients with multiple myeloma: a SEER-Medicare analysis. Blood Adv. 2019;3:2986–94.
Pulte D, Redaniel MT, Brenner H, Jansen L, Jeffreys M. Recent improvement in survival of patients with multiple myeloma: variation by ethnicity. Leuk Lymphoma. 2014;55:1083–9.
Kristinsson S, Anderson W, Landgren O. Improved long-term survival in multiple myeloma up to the age of 80 years. Leukemia. 2014;28:1346–8.
Page M, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Ailawadhi S, Advani P, Yang D, Ghosh R, Swaika A, Roy V, et al. Impact of access to NCI- and NCCN-designated cancer centers on outcomes for multiple myeloma patients: a SEER registry analysis. Cancer. 2016;122:618–25.
Ailawadhi S, Azzouqa AG, Hodge D, Cochuyt J, Jani P, Ahmed S, et al. Survival trends in young patients with multiple myeloma: a focus on racial-ethnic minorities. Clin Lymphoma Myeloma Leuk. 2019;19:619–23.
Ailawadhi S, Frank R, Ailawadhi M, Kanji Z, Jani P, Fiala M, et al. Utilization of radiation therapy in multiple myeloma: trends and changes in practice. Ann Hematol. 2021;100:735–41.
Ailawadhi S, Frank RD, Advani P, Swaika A, Temkit MH, Menghani R, et al. Racial disparity in utilization of therapeutic modalities among multiple myeloma patients: a SEER-Medicare analysis. Cancer Med. 2017;6:2876–85.
Ailawadhi S, Frank RD, Sharma M, Menghani R, Temkit M, Paulus S, et al. Trends in multiple myeloma presentation, management, cost of care, and outcomes in the Medicare population: a comprehensive look at racial disparities. Cancer. 2018;124:1710–21.
Ailawadhi S, Jagannath S, Lee HC, Narang M, Rifkin RM, Terebelo HR, et al. Association between race and treatment patterns and survival outcomes in multiple myeloma: a Connect MM Registry analysis. Cancer. 2020;126:4332–40.
Ailawadhi S, Jagannath S, Narang M, Rifkin RM, Terebelo HR, Toomey K, et al. Connect MM Registry as a national reference for United States multiple myeloma patients. Cancer Med. 2020;9:35–42.
Bhatnagar V, Wu Y, Goloubeva OG, Ruehle KT, Milliron TE, Harris CG, et al. Disparities in black and white patients with multiple myeloma referred for autologous hematopoietic transplantation: a single center study. Cancer. 2015;121:1064–70.
Chamoun K, Firoozmand A, Caimi P, Fu P, Cao S, Otegbeye F, et al. Socioeconomic factors and survival of multiple myeloma patients. Cancers. 2021;13:590.
Chhabra S, Thapa B, Szabo A, Konings S, D’Souza A, Dhakal B, et al. Utilization and cost implications of hematopoietic progenitor cells stored for a future salvage autologous transplantation or stem cell boost in myeloma patients. Biol Blood Marrow Transplant. 2020;26:2011–7.
Costa LJ, Brill IK, Brown EE. Impact of marital status, insurance status, income, and race/ethnicity on the survival of younger patients diagnosed with multiple myeloma in the United States. Cancer. 2016;122:3183–90.
Costa LJ, Brill IK, Omel J, Godby K, Kumar SK, Brown EE. Recent trends in multiple myeloma incidence and survival by age, race, and ethnicity in the United States. Blood Adv. 2017;1:282–7.
Costa LJ, Huang JX, Hari PN. Disparities in utilization of autologous hematopoietic cell transplantation for treatment of multiple myeloma. Biol Blood Marrow Transplant. 2015;21:701–6.
Derman BA, Jasielec J, Langerman SS, Zhang W, Jakubowiak AJ, Chiu BC-H. Racial differences in treatment and outcomes in multiple myeloma: a multiple myeloma research foundation analysis. Blood Cancer J. 2020;10:80.
DeSantis CE, Siegel RL, Sauer AG, Miller KD, Fedewa SA, Alcaraz KI, et al. Cancer statistics for African Americans, 2016: progress and opportunities in reducing racial disparities. CA Cancer J Clin. 2016;66:290–308.
Dhakal B, Miller S, Rein L, Pathak LK, Gloria L, Szabo A, et al. Trends in the use of therapeutic plasma exchange in multiple myeloma. J Clin Apher. 2020;35:307–15.
Evans LA, Go R, Warsame R, Nandakumar B, Buadi FK, Dispenzieri A, et al. The impact of socioeconomic risk factors on the survival outcomes of patients with newly diagnosed multiple myeloma: a cross-analysis of a population-based registry and a tertiary care center. Clin Lymphoma Myeloma Leuk. 2021;21:451–60.
Fakhri B, Fiala MA, Tuchman SA, Wildes TM. Undertreatment of older patients with newly diagnosed multiple myeloma in the era of novel therapies. Clin Lymphoma Myeloma Leuk. 2018;18:219–24.
Fiala MA, Finney JD, Liu J, Stockerl-Goldstein KE, Tomasson MH, Vij R, et al. Socioeconomic status is independently associated with overall survival in patients with multiple myeloma. Leuk Lymphoma. 2015;56:2643–9.
Fiala MA, Foley NC, Zweegman S, Vij R, Wildes TM. The characteristics, treatment patterns, and outcomes of older adults aged 80 and over with multiple myeloma. J Geriatr Oncol. 2020;11:1274–8.
Fiala MA, Gettinger T, Wallace CL, Vij R, Wildes TM. Cost differential associated with hospice use among older patients with multiple myeloma. J Geriatr Oncol. 2020;11:88–92.
Fiala MA, Wildes TM. Racial disparities in treatment use for multiple myeloma. Cancer. 2017;123:1590–6.
Hsieh RW, Go RS, Abeykoon JP, Kapoor P, Kumar SK, Gertz MA, et al. Characteristics of long-term survivors with multiple myeloma: a National Cancer Data Base analysis. Cancer. 2019;125:3574–81.
Jayakrishnan T, Bakalov V, Callander NS, Sadashiv S, Wagner R, Ailawadhi S. Impact of the Affordable Care Act on timeliness to treatment for patients with multiple myeloma. Anticancer Res. 2020;40:5727–34.
Jayakrishnan TT, Bakalov V, Chahine Z, Lister J, Wegner RE, Sadashiv S. Disparities in the enrollment to systemic therapy and survival for patients with multiple myeloma. Hematol Oncol Stem Cell Ther. 2021;14:218–30.
Kamath GR, Renteria AS, Jagannath S, Gallagher EJ, Parekh S, Bickell NA. Where you live can impact your cancer risk: a look at multiple myeloma in New York City. Ann Epidemiol. 2020;48:43–50.e44.
Kaya H, Peressini B, Jawed I, Martincic D, Elaimy AL, Lamoreaux WT, et al. Impact of age, race and decade of treatment on overall survival in a critical population analysis of 40,000 multiple myeloma patients. Int J Hematol. 2012;95:64–70.
Kumar V, Ailawadhi M, Dutta N, Abdulazeez M, Aggarwal CS, Quintero G, et al. Trends in early mortality from multiple myeloma: a population-based analysis. Clin Lymphoma Myeloma Leuk. 2021;21:e449–55.
Kumar V, Alhaj-Moustafa M, Bojanini L, Sher T, Roy V, Manochakian R, et al. Timeliness of initial therapy in multiple myeloma: trends and factors affecting patient care. JCO Oncol Pract. 2020;16:e341–9.
Makhani SS, Shively D, Castro G, Rodriguez de la Vega P, Barengo NC. Association of insurance disparities and survival in adults with multiple myeloma: a non-concurrent cohort study. Leuk Res. 2021;104:106542.
Marron MM, Ives DG, Boudreau RM, Harris TB, Newman AB. Racial differences in cause-specific mortality between community-dwelling older black and white adults. J Am Geriatr Soc. 2018;66:1980–6.
Pan D, Coltoff A, Ozbek U, Lin JY, Afshar S, Galitzeck Z, et al. Evaluating race and time to transplantation in multiple myeloma: the Mount Sinai hospital experience. Clin Lymphoma Myeloma Leuk. 2021;21:439–43.
Patel BG, Luo S, Wildes TM, Sanfilippo KM. Frailty in older adults with multiple myeloma: a study of US veterans. JCO Clin Cancer Inform. 2020;4:117–27.
Pinheiro PS, Medina H, Callahan KE, Kwon D, Ragin C, Sherman R, et al. Cancer mortality among US blacks: variability between African Americans, Afro-Caribbeans, and Africans. Cancer Epidemiol. 2020;66:101709.
Pulte D, Redaniel M, Brenner H, Jeffreys M. Changes in survival by ethnicity of patients with cancer between 1992-1996 and 2002–2006: is the discrepancy decreasing? Ann Oncol. 2012;23:2428–34.
Salgado LR, Chang S, Ru M, Moshier E, Ghiassi-Nejad Z, Lazarev S, et al. Utilization patterns of single fraction radiation therapy for multiple myeloma. Clin Lymphoma Myeloma Leuk. 2019;19:e238–46.
Schriber JR, Hari PN, Ahn KW, Fei M, Costa LJ, Kharfan-Dabaja MA, et al. Hispanics have the lowest stem cell transplant utilization rate for autologous hematopoietic cell transplantation for multiple myeloma in the United States: a CIBMTR report. Cancer. 2017;123:3141–9.
Sun T, Wang S, Sun H, Wen J, An G, Li J. Improved survival in multiple myeloma, with a diminishing racial gap and a widening socioeconomic status gap over three decades. Leuk Lymphoma. 2018;59:49–58.
Uprety D, Adhikari J, Arjyal L, Naglak MC, Seidman M. Racial differences in the survival of elderly patients with multiple myeloma in pre-and post-novel agent era. J Geriatr Oncol. 2017;8:125–7.
Warren JL, Harlan LC, Stevens J, Little RF, Abel GA. Multiple myeloma treatment transformed: a population-based study of changes in initial management approaches in the United States. J Clin Oncol. 2013;31:1984–9.
Wildes TM, Fiala MA. Falls in older adults with multiple myeloma. Eur J Haematol. 2018;100:273–8.
Wildes TM, Tuchman SA, Klepin HD, Mikhael J, Trinkaus K, Stockerl-Goldstein K, et al. Geriatric assessment in older adults with multiple myeloma. J Am Geriatr Soc. 2019;67:987–91.
Yusuf AA, Natwick T, Werther W, Felici D, Mahue M, Bridges KR, et al. A retrospective analysis to examine factors associated with mortality in Medicare beneficiaries newly diagnosed with multiple myeloma. Curr Med Res Opin. 2016;32:1989–96.
Zhou J, Sweiss K, Nutescu EA, Han J, Patel PR, Ko NY, et al. Racial disparities in intravenous bisphosphonate use among older patients with multiple myeloma enrolled in medicare. JCO Oncol Pract. 2021;17:e294–12.
Afshar N, English DR, Blakely T, Thursfield V, Farrugia H, Giles GG, et al. Differences in cancer survival by area-level socio-economic disadvantage: a population-based study using cancer registry data. PLoS ONE. 2020;15:e0228551.
Auner HW, Pavlu J, Szydlo R, Giles C, Kanfer E, Macdonald D, et al. Autologous haematopoietic stem cell transplantation in multiple myeloma patients from ethnic minority groups in an equal access healthcare system. Br J Haematol. 2012;157:125–7.
Auner HW, Szydlo R, Hoek J, Goldschmidt H, Stoppa AM, Morgan GJ, et al. Trends in autologous hematopoietic cell transplantation for multiple myeloma in Europe: increased use and improved outcomes in elderly patients in recent years. Bone Marrow Transplant. 2015;50:209–15.
Chan HSH, Milne RJ. Impact of age, sex, ethnicity, socio-economic deprivation and novel pharmaceuticals on the overall survival of patients with multiple myeloma in New Zealand. Br J Haematol. 2020;188:692–700.
Chang-Chan DY, Rios-Tamayo R, Rodriguez Barranco M, Redondo-Sanchez D, Gonzalez Y, Marcos-Gragera R, et al. Trends of incidence, mortality and survival of multiple myeloma in Spain. A twenty-three-year population-based study. Clin Transl Oncol. 2021;23:1429–39.
El Husseiny NM, Kasem N, El Azeeim HA, Mattar MW. Multiple myeloma: a descriptive study of 217 Egyptian patients. Ann Hematol. 2014;93:141–5.
Harwood M, Dunn N, Moore J, Mollee P, Hapgood G. Trends in myeloma relative survival in Queensland by treatment era, age, place of residence, and socioeconomic status. Leuk Lymphoma. 2020;61:721–7.
Hsu P, Lin TW, Gau JP, Yu YB, Hsiao LT, Tzeng CH, et al. Risk of early mortality in patients with newly diagnosed multiple myeloma. Medicine. 2015;94:e2305.
Ilic M, Ilic I. Malignant lymphatic and hematopoietic neoplasms mortality in Serbia, 1991-2010: a joinpoint regression analysis. PLoS ONE. 2014;9:e109379.
Intzes S, Symeonidou M, Zagoridis K, Bezirgiannidou Z, Pentidou A, Vrachiolias G, et al. Socioeconomic status is an independent prognostic factor for overall survival in patients with multiple myeloma: real-world data from a cohort of 223 patients. Clin Lymphoma Myeloma Leuk. 2020;20:704–11.
Jones A, Bowcock S, Rachet B. Survival trends in elderly myeloma patients. Eur J Haematol. 2021;106:126–31.
Jurczyszyn A, Nahi H, Avivi I, Gozzetti A, Niesvizky R, Yadlapati S, et al. Characteristics and outcomes of patients with multiple myeloma aged 21-40 years versus 41-60 years: a multi-institutional case-control study. Br J Haematol. 2016;175:884–91.
Kim K, Lee JH, Kim JS, Min CK, Yoon SS, Shimizu K, et al. Clinical profiles of multiple myeloma in Asia-An Asian Myeloma Network study. Am J Hematol. 2014;89:751–6.
Lin L, Yan L, Liu Y, Yuan F, Li H, Ni J. Incidence and death in 29 cancer groups in 2017 and trend analysis from 1990 to 2017 from the Global Burden of Disease Study. J Hematol Oncol. 2019;12:96.
Liu J, Liu W, Mi L, Zeng X, Cai C, Ma J, et al. Incidence and mortality of multiple myeloma in China, 2006-2016: an analysis of the Global Burden of Disease Study 2016. J Hematol Oncol. 2019;12:136.
Mahumud RA, Alam K, Dunn J, Gow J. Emerging cancer incidence, mortality, hospitalisation and associated burden among Australian cancer patients, 1982–2014: an incidence-based approach in terms of trends, determinants and inequality. BMJ Open. 2019;9:e031874.
Manyega KM, Lotodo TC, Oduor MA, Namaemba DF, Omondi AA, Oyolo YL, et al. Retrospective analysis of presentation, treatment, and outcomes of multiple myeloma at a large public referral hospital in Eldoret, Kenya. JCO Glob Oncol. 2021;7:391–9.
Mian HS, Seow H, Wildes TM, Kouroukis CT, Pond GR, Sivapathasundaram B, et al. Disparities in treatment patterns and outcomes among younger and older adults with newly diagnosed multiple myeloma: a population-based study. J Geriatr Oncol. 2021;12:508–14.
Ng TF, Burrow S, Leahy M, Augustson B, Trentino K, De Kraa R, et al. Patients with multiple myeloma over a large catchment of 2.5 million square kilometres: a Western Australia retrospective survival review. Intern Med J. 2020;50:869–72.
Pastor-Barriuso R, Lopez-Abente G. Changes in period and cohort effects on haematological cancer mortality in Spain, 1952-2006. BMC Cancer. 2014;14:250.
Pulte D, Jansen L, Castro FA, Emrich K, Katalinic A, Holleczek B, et al. Trends in survival of multiple myeloma patients in Germany and the United States in the first decade of the 21st century. Br J Haematol. 2015;171:189–96.
Puyade M, Defossez G, Guilhot F, Leleu X, Ingrand P. Age-related health care disparities in multiple myeloma. Hematol Oncol. 2018;36:224–31.
Quaresma M, Coleman MP, Rachet B. 40-year trends in an index of survival for all cancers combined and survival adjusted for age and sex for each cancer in England and Wales, 1971-2011: a population-based study. Lancet. 2015;385:1206–18.
Radocha J, Hájek R, Brožová L, Pour L, Špička I, Minařík J, et al. Simplified novel prognostic score for real-life older adults with multiple myeloma-registry-based analysis. Ann Hematol. 2019;98:951–62.
Riva E, Bove V, Villano F, Mori M, Cordoba C, Noria A, et al. From guidelines to real world: results from the National Multiple Myeloma Registry in Uruguay on 222 newly diagnosed multiple myeloma patients from 2012 to 2015. Curr Med Res Opin. 2019;35:1197–203.
Riva E, Schütz N, Peña C, Ruiz-Argüelles G, Hopkins CR, Bove V, et al. Significant differences in access to tests and treatments for multiple myeloma between public and private systems in Latin America. Results of a Latin American survey. GELAMM (Grupo de Estudio Latino Americano de Mieloma Múltiple). Ann Hematol. 2020;99:1025–30.
Rosso T, Malvezzi M, Bertuccio P, Negri E, La Vecchia C, Decarli A. Cancer mortality in Italy, 2008, and predictions for 2012. Tumori. 2012;98:559–67.
Samy EF, Ross J, Bolton E, Morris EJ, Oliver SE. Variation in incidence and survival by ethnicity for patients with myeloma in England (2002-2008). Leuk Lymphoma. 2015;56:2660–7.
Smailyte G, Jasilionis D, Vincerzevskiene I, Shkolnikov VM. Education, survival, and avoidable deaths in Lithuanian cancer patients, 2001-2009. Acta Oncol. 2016;55:859–64.
Sneyd MJ, Cox B, Morison IM. Trends in myeloma incidence, mortality and survival in New Zealand (1985-2016). Cancer Epidemiol. 2019;60:55–59.
Tarín-Arzaga L, Arredondo-Campos D, Martínez-Pacheco V, Martínez-González O, Ramírez-López A, Gómez-De León A, et al. Impact of the affordability of novel agents in patients with multiple myeloma: real-world data of current clinical practice in Mexico. Cancer. 2018;124:1946–53.
Tsang M, Le M, Ghazawi FM, Cyr J, Alakel A, Rahme E, et al. Multiple myeloma epidemiology and patient geographic distribution in Canada: a population study. Cancer. 2019;125:2435–44.
Vanthomme K, Vandenheede H, Hagedoorn P, Gadeyne S. Evolution of socioeconomic inequalities in site-specific cancer mortality among Belgian women between 1991 and 2008 using a fundamental cause approach. Cancer Causes Control. 2017;28:829–40.
Vargas-Serafin C, Acosta-Medina AA, Ordonez-Gonzalez I, Martinez-Banos D, Bourlon C. Impact of socioeconomic characteristics and comorbidities on therapy initiation and outcomes of newly diagnosed multiple myeloma: real-world data from a resource-constrained setting. Clin Lymphoma Myeloma Leuk. 2021;21:182–7.
Xu L, Wang X, Pan X, Wang X, Wang Q, Wu B, et al. Education level as a predictor of survival in patients with multiple myeloma. BMC Cancer. 2020;20:737.
Chen JH, Chung CH, Wang YC, Hsu SN, Huang WY, Chien WC. Prevalence and mortality-related factors of multiple myeloma in Taiwan. PLoS ONE. 2016;11:e0167227.
Siegal R, Miller K, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67:7–30.
Cavo M, Rajkumar SV, Palumbo A, Moreau P, Orlowski R, Blade J, et al. International Myeloma Working Group consensus approach to the treatment of multiple myeloma patients who are candidates for autologous stem cell transplantation. Blood. 2011;117:6063–73.
Li J, Chan H. Management of multiple myeloma in older patients. EMJ Hematol. 2021;9:69–81.
Binder M, Nandakumar B, Rajkumar SV, Kapoor P, Buadi FK, Dingli D, et al. Mortality trends in multiple myeloma after the introduction of novel therapies in the United States. Leukemia. 2022;36:801–8.
Westergaard D, Moseley P, Sørup FKH, Baldi P, Brunak S. Population-wide analysis of differences in disease progression patterns in men and women. Nat Commun. 2019;10:666.
Fillmore NR, Yellapragada SV, Ifeorah C, Mehta A, Cirstea D, White PS, et al. With equal access, African American patients have superior survival compared to white patients with multiple myeloma: a VA study. Blood. 2019;133:2615–8.
Gulla A, Anderson KC. Multiple myeloma: the (r)evolution of current therapy and a glance into future. Haematologica. 2020;105:2358–67.
Pan D, Richter J. Where we stand with precision therapeutics in myeloma: prosperity, promises, and pipedreams. Front Oncol. 2021;11:819127.
Acknowledgements
This study was sponsored by Pfizer. Database searches were conducted by Catherine Rolland, and screening, data extraction, and quality assessment by Catherine Rolland and Karen Smoyer of Curo (part of the Envision Pharma Group), funded by Pfizer. Medical writing support was provided by David Cope, PhD, of Engage Scientific Solutions, and funded by Pfizer.
Author information
Authors and Affiliations
Contributions
DA conceived the study and study design. All authors had access to the underlying data, interpreted the data, drafted the manuscript or critically revised it for important intellectual content, and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
MVM reports receiving fees derived from lectures and participation in advisory boards from Janssen, Celgene, Takeda, Amgen, GSK, AbbVie, Pfizer, Regeneron, Roche, Sanofi, Oncopeptides, and Seagen. SA reports providing consultancy services for GSK, Sanofi, Bristol-Myers Squibb, Takeda, Beigene, Pharmacyclics, Amgen, Janssen, AstraZeneca, and Regeneron; and receiving research support to his institution from GSK, Bristol-Myers Squibb, Pharmacyclics, Amgen, Janssen, Cellectar, Xencor, AbbVie, Medimmune, and Ascentage. LJC reports receiving honoraria from Janssen, Amgen, Sanofi, Bristol-Myers Squibb, and Adaptive Biotechnologies; participating in scientific advisory boards for Janssen, Amgen, Bristol-Myers Squibb, and Sanofi; and receiving research support from Janssen, Amgen, and Bristol-Myers Squibb. SJG reports receiving research funding from the National Cancer Institute at the National Institutes of Health (5-K12-CA120780-13 and 1 R03 AG074030-01). LK reports no conflicts of interest. MM reports receiving honoraria from or providing consultancy services to Adaptive Biotechnologies, Amgen, Bristol-Myers Squibb, Celgene, Janssen, Takeda, Novartis, Sanofi, and Stemline; and research funding from Janssen and Sanofi. DA is an employee of and has stock or stock options in Pfizer. SZU reports receiving consulting/advisory fees, grant support, and Speakers’ Bureau fees from Amgen, Takeda, Janssen, Sanofi, and Bristol-Myers Squibb; consulting/advisory fees and grant support from Bristol-Myers Squibb, Celgene, GSK, Merck, Seattle Genetics, and Skyline Diagnostics; grant support and Speakers’ Bureau fees from Sanofi; grant support from Array BioPharma and Pharmacyclics; and consulting/advisory fees from Karyopharm Therapeutics, AbbVie, Oncopeptides, Genentech, and Gilead.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mateos, MV., Ailawadhi, S., Costa, L.J. et al. Global disparities in patients with multiple myeloma: a rapid evidence assessment. Blood Cancer J. 13, 109 (2023). https://doi.org/10.1038/s41408-023-00877-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41408-023-00877-9