Abstract
Patients with hematologic malignancies (HM) have demonstrated impaired immune responses following SARS-CoV-2 vaccination. Factors associated with poor immunogenicity remain largely undetermined. A literature search was conducted using PubMed, EMBASE, Cochrane, and medRxiv databases to identify studies that reported humoral or cellular immune responses (CIR) following complete SARS-CoV-2 vaccination. The primary aim was to estimate the seroconversion rate (SR) following complete SARS-CoV-2 vaccination across various subtypes of HM diseases and treatments. The secondary aims were to determine the rates of development of neutralizing antibodies (NAb) and CIR following complete vaccination and SR following booster doses. A total of 170 studies were included for qualitative and quantitative analysis of primary and secondary outcomes. A meta-analysis of 150 studies including 20,922 HM patients revealed a pooled SR following SARS-CoV-2 vaccination of 67.7% (95% confidence interval [CI], 64.8–70.4%; I2 = 94%). Meta-regression analysis showed that patients with lymphoid malignancies, but not myeloid malignancies, had lower seroconversion rates than those with solid cancers (R2 = 0.52, P < 0.0001). Patients receiving chimeric antigen receptor T-cells (CART), B-cell targeted therapies or JAK inhibitors were associated with poor seroconversion (R2 = 0.39, P < 0.0001). The pooled NAb and CIR rates were 52.8% (95% CI; 45.8–59.7%, I2 = 87%) and 66.6% (95% CI, 57.1–74.9%; I2 = 86%), respectively. Approximately 20.9% (95% CI, 11.4–35.1%, I2 = 90%) of HM patients failed to elicit humoral and cellular immunity. Among non-seroconverted patients after primary vaccination, only 40.5% (95% CI, 33.0–48.4%; I2 = 87%) mounted seroconversion after the booster. In conclusion, HM patients, especially those with lymphoid malignancies and/or receiving CART, B-cell targeted therapies, or JAK inhibitors, showed poor SR after SARS-CoV-2 vaccination. A minority of patients attained seroconversion after booster vaccination. Strategies to improve immune response in these severely immunosuppressed patients are needed.
Similar content being viewed by others
Introduction
Since the first emerging cluster of pneumonia in China in December 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has infected more than 600 million people and caused over 6 million deaths worldwide [1]. Patients with hematologic malignancies, especially acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS), are at high risk of mortality from SARS-CoV-2 infection [2]. Furthermore, hematologic malignancy patients suffer higher mortality from coronavirus disease 2019 (COVID-19) than solid cancer patients [3].
Vaccines against SARS-CoV-2 have shown effectiveness in the prevention of symptomatic infection and in the reduction of hospitalization and mortality from COVID-19 [4,5,6,7]. Unfortunately, patients with hematologic malignancies demonstrated poor seroconversion rates following SARS-CoV-2 vaccination compared to healthy people. Furthermore, various treatment modalities variedly affected the ability to mount humoral immune responses in hematologic malignancy patients [8]. Recent systematic review and meta-analysis studies demonstrated that approximately two-thirds of hematologic malignancies attained anti-spike (anti-S) SARS-CoV-2 IgG seroconversion following complete SARS-CoV-2 vaccination (2 doses of mRNA vaccines or ChAdOx1 nCoV-19 or a single dose of Ad26.COV2.S). In contrast, approximately 90% of patients with solid cancers achieved seroconversion after complete vaccination. Hematologic malignancies comprise diverse subgroups of diseases that may have variable immune responses after immunization. Additionally, different treatment modalities can affect immune function resulting in heterogeneous immunogenicity following vaccination [9, 10].
Hematologic malignancy patients who mount SARS-CoV-2 specific cell-mediated immune responses without reaching seroconversion have improved survival suggesting that cellular immune responses to SARS-CoV-2 vaccination may provide protection in patients who have impaired humoral immunity [11]. However, SARS-CoV-2-specific T-cell responses are rarely evaluated in most studies. Therefore, cellular immune responses following SARS-CoV-2 vaccination in hematologic malignancies remain indeterminate.
Due to limited immune response, a booster dose has been offered to patients with negative seroconversion following a complete vaccination. However, studies in solid organ transplantation demonstrated unsatisfying seroconversion rates following booster vaccination [12]. The impact of a booster dose on seroconversion in diverse subgroups of hematologic malignancies remains largely undefined.
Currently, there has been a growing amount of available data on immunogenicity following SARS-CoV-2 vaccination including after a booster dose. We conducted a systematic review and meta-analysis to assess immunogenicity and factors associated with poor immune responses following vaccination against SARS-CoV-2 in hematologic malignancies.
Methods
The protocol for this review was prespecified and registered in PROSPERO (CRD42022346853). The study was subsequently conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [13]. The primary objective of this study was to estimate the proportion of seroconversion following complete primary vaccination in SARS-CoV-2-naive hematologic malignancies patients.
Data source, search strategy, and study selection
A systematic search of electronic databases was performed using PubMed, EMBASE, Cochrane Library Database and the preprint server (medRxiv) from inception to May 1, 2022 and was updated on August 30, 2022 to identify studies reporting humoral immune responses and/or cellular immune responses in hematologic malignancy patients following complete vaccination using this following search strategy: ((((vaccin*[tw] OR immuni*[tw])) AND (((hemato*[tw] OR haemato*[tw] OR blood[tw] OR marrow[tw] OR “plasma cell”[tw]) AND (neoplasm[tw] OR cancer[tw] OR malig*[tw] OR oncolog*[tw])) OR (myeloid[tw] OR lymphoid[tw] OR leukemia*[tw] OR leukaemia[tw] OR lymphoma[tw] OR myeloma[tw] OR myelodysplastic[tw] OR myeloproliferative[tw]))) AND ((immun*[tw] OR sero*[tw] OR antibod*[tw] OR humoral[tw] OR response[tw]))) AND ((“Novel coronavirus 2019”[tw] OR “COVID-19”[tw] OR “SARS-CoV-2”[tw] OR “2019-nCoV”[tw])). The inclusion criteria for eligible studies were as follows: (1) studies containing adult patients with hematologic malignancies, (2) assessing humoral or cellular immune responses of COVID-19 vaccines, and (3) inclusion of at least 20 hematologic malignancy patients.
Non-original articles (such as reviews, commentaries, or guidelines) and duplicated studies were excluded. There were no language restrictions. Two authors (N.U. and P.P.) independently searched the literature, screened titles and abstracts, and reviewed full texts to identify potentially eligible studies. Disagreements were resolved by consensus or by a third reviewer (N.T.) when necessary. Selection results were reported according to the PRISMA flowchart.
Data extraction
Two authors (N.U. and P.P.) independently reviewed full data from individual selected studies including supplementary materials and independently extracted prespecified data. Disagreements of extracted data were resolved by consensus or a third reviewer (N.T.) when necessary.
The primary objective of this study was to estimate the pooled seroconversion rate following complete primary vaccination (2 doses of mRNA vaccines [BNT162b2 or mRNA-1273], adenoviral vector vaccines [ChAdOx nCoV-19 or rAD26/rAD5], inactivated vaccines [CoronaVac, BBIBP-CorV, or BBV152] and protein subunit vaccine [NVX-CoV23] or a single dose of Ad26.COV.2S) in hematologic malignancy patients without prior SARS-CoV-2 infection. Seroconversion was defined using detectable anti-S SARS-CoV-2 antibody levels above the cut-off of individual studies. Seroconversion rates in healthy participants or patients with solid cancers were compared if they were reported concomitantly. Secondary outcomes were to determine neutralizing antibody development, cell-mediated immune responses, and vaccine efficacy. Subgroup analyses were performed to assess the impact of hematologic malignancy subtypes, treatment modalities, and vaccine platforms on seroconversion rates if there were sufficient data. Additional analysis of the effect of a booster dose on seroconversion was performed if sufficient data were available.
For each study, the following data were extracted: study design, study population, number of participants, types, and doses of vaccines, subtypes of hematologic malignancies, treatment modalities, methods used for detecting anti-S antibodies, numbers or proportion of seroconversion, development of neutralizing antibody, development of cellular immune response following primary vaccinations and seroconversion following booster vaccination.
Quality assessment
The methodological quality assessment of included studies for meta-analysis was performed independently by two authors (N.U. and P.P.) using the Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analysis [14]. The tool contains 3 domains and 8 items assessing the selection, comparability, and outcomes of the study. For each item, a study can receive a maximum of one star for each numbered item within the selection and outcome domains. A maximum of two stars can be given for the comparability domain. The studies were classified based on the given stars as poor (0–3), fair (4–6), or good (7–9) quality.
Data analysis
The meta-analysis was performed using Comprehensive Meta-analysis (Version 3; Biostat, Englewood, NJ, USA). The pooled seroconversion rate and other immunological response rates of each outcome were calculated using random-effects model and reported as the pooled proportion with a 95% confidence interval (CI). The pooled risk ratio (RR) was calculated using the Mantel-Haenszel method with random-effects model and reported as RR with 95% CI. Meta-regression analysis was performed to assess factors associated with seroconversion rates. Statistical heterogeneity was assessed using I2 statistic, which measured the inconsistency across study results. Inter-study heterogeneity was assigned as insignificant (I2 = 0–25%), low (I2 = 26–50%), moderate (I2 = 51–75%), and high (I2 > 75%) [15]. The funnel plot and the Egger regression were used to evaluate publication bias. Publication bias was considered significant if a P-value was <0.1.
Results
Study characteristics
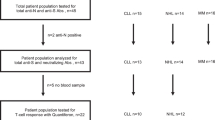
The study report was prepared according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (Supplementary Table S1). The PRISMA flow diagram is shown (Supplementary Fig. 1). The literature search yielded 4,468 articles. After duplicates were removed, a total of 1641 unique studies were screened by titles and abstracts. Of these, 1371 were excluded, and 270 full texts were screened for eligibility. Eventually, 170 studies [16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179,180,181,182,183,184,185] met the eligibility criteria and were included in the qualitative and quantitative synthesis. The risk of bias in each study was individually assessed. Of 170 analyzed studies, 77 were assigned good quality, while 93 were assigned fair quality (Supplementary Table S2). The main characteristics of the 170 included studies are summarized in Supplementary Table S3. The publication bias was assessed using a funnel plot and Egger regression. The funnel plot showed a symmetrical distribution indicating the absence of publication bias (Supplementary Fig. S2). No publication bias was detected by Egger regression intercept analysis (P = 0.38).
Seroconversion rate following complete primary vaccination in hematologic malignancy patients
Of 170 included studies, 150 studies [16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32, 34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59, 62,63,64,65,66,67, 70, 71, 73,74,75,76, 78,79,80,81, 83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98, 100,101,102,103,104, 106,107,108,109,110,111,112,113,114, 116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137, 139,140,141, 143,144,145,146,147,148,149,150,151,152,153,154,155, 158, 159, 161,162,163,164,165,166,167,168,169,170,171,172,173,174, 177, 179,180,181,182,183,184] containing 20,922 hematologic malignancy patients were eligible for quantitative assessment of seroconversion rates. Among vaccine platforms, mRNA vaccines were administered in 117 studies, while mRNA vaccines and adenoviral vector vaccines, adenoviral vector vaccines and inactivated vaccines were administered in 29, 2 and 1 studies, respectively. The timing of serology tests after vaccination was reported in 94.7% of the studies. Most studies performed the test between 7 and 60 days after complete vaccination. The pooled seroconversion rate following complete SARS-CoV-2 vaccination was 67.7% (95% confidence interval [CI], 64.8–70.4%; I2 = 94%) (Fig. 1 and Supplementary Fig. S3).
There were 12 studies [16, 21, 29, 30, 59, 67, 89, 92, 96, 101, 110, 140] including 1479 patients with solid cancers and 20 studies [20, 23, 25, 28, 39, 42, 43, 45, 46, 49, 54, 56, 59, 73, 78, 92, 93, 141, 144, 175] including 1121 healthy controls for comparison. The pooled seroconversion rates of solid cancer patients and healthy controls were 89.2% (95% CI, 87.2–90.9%, I2 = 83%) and 98.7% (95% CI, 97.7–99.3%, I2 = 0%), respectively. Hematologic malignancy patients attained significantly lower seroconversion rates compared to solid cancer patients and healthy controls (both P < 0.0001). The pooled RR for seroconversion in hematologic malignancy patients compared to solid cancer patients and healthy participants were 0.72 (95% CI, 0.65–0.80, I2 = 87%) and 0.67 (95% CI, 0.61–0.75, I2 = 91%), respectively.
Due to high heterogeneity in seroconversion rates among hematologic malignancy patients, subgroup analyses were performed to explore the impact of disease subtypes and various treatment modalities on serological responses.
Seroconversion rate and association with hematologic malignancy subtypes
There were 64 studies containing 9,482 patients (34 multiple myeloma [MM], 27 chronic lymphocytic leukemia [CLL], 23 non-Hodgkin lymphoma [NHL], 19 myeloproliferative neoplasms [MPN], 12 Hodgkin lymphoma [HL], 8 acute leukemia and 6 myelodysplastic syndrome [MDS]) [18, 20, 22,23,24,25,26, 28, 30, 31, 34, 35, 37,38,39, 43,44,45, 47,48,49,50,51, 53, 55,56,57,58, 62, 66, 71,72,73,74, 76, 78, 80, 83, 86, 87, 95,96,97, 101, 104, 107, 110,111,112,113,114, 121, 123, 128, 134, 143, 145, 148, 153, 159, 164, 167, 168, 179, 182] providing sufficient data for estimating seroconversion rates among disease subtypes. Subgroup analysis demonstrated significantly different seroconversion rates among hematologic malignancies subtypes (P < 0.001), of which the seroconversion rate was lowest in CLL (54.1%; 95% CI, 52.2–56.0%, I2 = 74%), followed by NHL (58.0%; 95% CI, 56.0–60.0%, I2 = 93%), MM (78.0%; 95% CI, 76.3–79.6%, I2 = 84%), HL (80.1%; 95% CI, 71.9–86.4%, I2 = 55%), MDS (83.7%; 95% CI, 73.8–90.4%, I2 = 0%), MPN (86.8%; 95% CI, 84.1–89.2%, I2 = 63%) and acute leukemia (88.5%; 95% CI, 82.3–92.7%, I2 = 0%) (Fig. 2 and Supplementary Fig. S4).
Meta-regression analysis showed that patients with hematologic malignancies had inferior humoral immune responses to those with solid cancers (R2 = 0.52, P < 0.0001). Patients with lymphoid malignancies (CLL [P < 0.0001], NHL [P < 0.0001], MM [P < 0.0001], and HL [P = 0.0123]), but not myeloid malignancies (MPN [P = 0.0624], MDS [P = 0.0828] and acute leukemia [P = 0.2253]), were associated with lower seroconversion rates than those with solid cancers.
Seroconversion rate and association with treatment modalities
There were 48 studies containing 7418 patients [16,17,18, 20, 22,23,24, 26, 27, 32, 35, 38, 41,42,43,44,45,46, 58, 62, 63, 67, 70, 73,74,75, 78, 83, 86, 95, 96, 100, 109,110,111,112, 114, 121, 128, 134, 137, 139, 141, 154, 158, 164, 168, 169] available for subgroup analysis to assess the impact of treatment modalities on seroconversion rates. Hematologic malignancy patients who received treatments had significantly lower seroconversion rates (59.2%; 95% CI, 54.2–63.9%, I2 = 90%) compared to those without treatments (80.4%; 95% CI, 73.7–85.8%, I2 = 79%), (P < 0.001) (Fig. 1). Treatment subgroups were classified into non-treatment, chemotherapy, immunomodulatory agents (IMiD), proteasome inhibitors (PI), B-cell lymphoma 2 inhibitors (BCL2i), B-cell targeted kinase inhibitors (BKI), including Bruton tyrosine kinase inhibitors and phosphatidylinositol-3 kinase inhibitors, Janus kinase inhibitors (JAKi), tyrosine kinase inhibitors (TKI) for therapy of chronic myeloid leukemia, monoclonal antibody to CD20 (Mab-CD20), monoclonal antibody to CD38 (Mab-CD38), chimeric antigen receptor T-cell therapy (CART) and hematopoietic stem cell transplantation (HSCT), including both autologous and allogeneic HSCT. Subgroup analysis demonstrated significantly different seroconversion rates among treatment modalities (P < 0.001), of which the seroconversion rate was lowest in CART (18.6%; 95% CI, 11.5–28.6%, I2 = 0%), followed by Mab-CD20 (35.8%; 95% CI, 27.6–44.9%, I2 = 92%), BKI (36.6%; 95% CI, 28.4–45.6%, I2 = 77%), BCL2i (39.5%; 95% CI, 27.7–52.7%, I2 = 52%), JAKi (63.3%; 95% CI, 48.9–75.6%, I2 = 60%), chemotherapy (75.1%; 95% CI, 63.6–83.9%, I2 = 76%), no treatment (80.4%; 95% CI, 73.7–85.8%, I2 = 79%), IMiD (80.6%; 95% CI, 67.6–89.2%, I2 = 81%), Mab-CD38 (81.4%; 95% CI, 63.2–91.7%, I2 = 90%), HSCT (81.6%; 95% CI, 77.1–85.3%, I2 = 70%), PI (83.1%; 95% CI, 59.8–94.2%, I2 = 91%) and TKI (93.9%; 95% CI, 80.2–98.3%, I2 = 14%) (Supplementary Fig. S5 and Table S4).
We performed a subgroup analysis to determine the impact of the interval between the last Mab-CD20 treatment and vaccination [17, 22, 41, 58, 86, 109, 110, 114, 139, 141, 145, 164]. Patients recently exposed to Mab-CD20 had significantly lower seroconversion rates (23.4%; 95% CI, 16.2–32.5%, I2 = 76%) than those who were treated with Mab-CD20 over 6–12 months (63.0%; 95% CI, 40.7–80.8%, I2 = 94%), (P = 0.001).
Among patients receiving hematopoietic stem cell transplantation (HSCT) [23, 24, 27, 38, 41, 43, 46, 58, 62, 63, 70, 75, 95, 109, 121, 134, 137, 154, 168], subgroup analysis showed significantly lower seroconversion rates in patients receiving allogeneic HSCT (76.7%; 95% CI, 71.6–81.1%, I2 = 58%) compared to those receiving autologous HSCT (86.3%; 95% CI, 80.5–90.6%, I2 = 43%), (P = 0.011).
Among MPN patients [26, 66, 83, 111, 128], patients currently exposed to JAKi had significantly lower seroconversion rates (64.2%; 95% CI, 53.1–74.0%, I2 = 0%) than those unexposed to JAKi (90.4%; 95% CI, 84.9–94.1%, I2 = 0%), (P < 0.001).
Meta-regression analysis demonstrated an association between treatment modalities and seroconversion rates (R2 = 0.39, P < 0.0001). Hematologic malignancy patients who received treatment with CART (P < 0.0001), Mab-CD20 (P < 0.0001), BKI (P < 0.0001), BCL2i (P < 0.0001), and JAKi (P = 0.0238) were associated with lower seroconversion rates compared to untreated patients, while those who received chemotherapy, Mab-CD38, IMiD, PI, HSCT, and TKI had no significant response rates compared to the untreated group.
Effects of a booster dose on seroconversion
A total of 21 studies containing 1518 hematologic malignancy patients [48, 69, 72, 74, 81, 86, 96, 105, 112, 115, 120, 156, 157, 160, 164, 175, 176, 182,183,184,185] were available to assess seroconversion rates after a booster dose, mainly mRNA vaccines, among patients who remained seronegative for anti-S antibodies following primary SARS-CoV-2 vaccination. Most studies explored the effect of booster vaccination in patients with lymphoid malignancies, including CLL and NHL. The pooled seroconversion rate after booster vaccination was 40.5% (95% CI, 33.0–48.4%; I2 = 87%) (Fig. 3). Subgroup analysis did not show statistical significance in seroconversion rates following booster vaccination between studies containing only patients with lymphoid malignancies (36.8%, 95% CI; 24.9–50.5%, I2 = 84%) and those with all disease subtypes (43.1%, 95% CI; 34.0–52.6%, I2 = 87%), (P = 0.448).
Development of neutralizing antibodies
A total of 21 studies including 2011 hematologic malignancy patients [19, 25, 28, 29, 32, 33, 41, 60, 61, 68, 77, 82, 99, 109, 138,139,140, 142, 144, 166, 178] assessed the development of neutralizing antibodies after complete SARS-CoV-2 vaccination. The pooled proportion of neutralizing antibody development was 52.8% (95% CI; 45.8–59.7%, I2 = 87%) (Fig. 4). Of 21 included studies, 9 studies required antibody levels with at least 30% inhibitory activities against SARS-CoV-2, while 7 studies required at least 50% inhibitory activities as a positive result. Subgroup analysis did not show significant differences between the pooled proportion of neutralizing antibody development between studies using cutoff levels of 30% (56.0%, 95% CI; 46.4–65.3%) and 50% (47.6%, 95% CI; 34.5–61.0%), (P = 0.321). There were 10 studies containing 532 healthy participants for comparison. The pooled proportion of neutralizing antibody development in healthy controls was 94.6% (95% CI; 90.5–97.0%, I2 = 26%). Compared to healthy controls, the pooled RR of neutralizing antibody development in hematologic malignancy patients was 0.52 (95% CI, 0.42–0.66, I2 = 92%).
Assessment of cellular immune response
A total of 17 studies including 872 hematologic malignancy patients [28, 41, 54, 59, 65, 78, 91, 111, 112, 130, 140, 142, 144, 145, 153, 159, 174] evaluated cellular immune responses against SARS-CoV-2 after vaccination. All studies evaluated cell-mediated immune responses using interferon production or release from T-lymphocytes exposed to SARS-CoV-2 antigens. The pooled proportion of cellular immune responses was 66.6% (95% CI, 57.1–74.9%; I2 = 86%) (Fig. 5). Patients with seroconversion attained higher cellular immune responses (67.8%, 95% CI; 52.1–80.4%; I2 = 78%) compared to those with serological failure (46.1%, 95% CI; 28.6–64.5%; I2 = 82%). However, there was no statistical significance between the subgroups (P = 0.078), probably due to inadequate statistical power. There were 9 studies containing 224 healthy participants for comparison. The pooled proportion of cellular immune responses in healthy subjects was 93.8% (95% CI; 86.6–97.2%, I2 = 24%). Compared to healthy controls, the pooled RR of mounting cellular immune response in hematologic malignancy patients was 0.67 (95% CI, 0.57–0.80, I2 = 82%).
Notably, the pooled proportion of hematologic malignancy patients who failed to elicit humoral and cellular immunity was 20.9% (95% CI, 11.4–35.1%, I2 = 90%).
Discussion
This systematic review and meta-analysis of 170 studies involving over 20,000 hematologic malignancy patients demonstrates impaired immunogenicity following SARS-CoV-2 vaccination. Despite approaching 100% seroconversion achieved in healthy subjects, only two-thirds of hematologic malignancy patients were able to mount an immune response after complete primary SARS-CoV-2 vaccination. This meta-analysis confirmed the lower seroconversion rates of patients with hematologic malignancies, especially those with lymphoid malignancies, compared to those with solid cancers [9, 10]. However, hematologic malignancies contain various subtypes, which have varied immunosuppressed status. Furthermore, various treatment modalities for hematologic malignancies could diversely affect immune function. Since the pooled seroconversion rate showed high heterogeneity, we performed a subgroup analysis to determine which disease subtypes or treatments were associated with poor humoral immune responses following SARS-CoV-2 vaccination in hematologic malignancies.
Patients with lymphoid malignancies, including CLL, NHL, MM, and HL, showed lower seroconversion rates than those with solid cancers. Seroconversion rates were remarkably low in patients with CLL and NHL, of which only approximately half of these patients attained seroconversion. In contrast, patients with myeloid malignancies, including MPNs, MDS and acute leukemia, exhibited serological responses over 80% comparable to response rates in solid cancer patients. Patients with CLL and NHL appear at the highest risk of immunologic failure following primary vaccination. Strategies to enhance immune responses or preexposure prophylaxis with monoclonal antibodies are needed in these severely immunosuppressed patients. Furthermore, although post-vaccination serology tests are not routinely indicated in the general population, such tests may be helpful in evaluating immune responses and infection risks in this population.
B-cell depletion therapy or B-cell-directed therapy contributed to poor immunogenicity in hematologic malignancy patients. Approximately 20–40% of patients receiving CART, Mab-CD20, BKI and BCL2i attained seroconversion following primary SARS-CoV-2 vaccination. Among patients treated with Mab-CD20, those who were recently administered Mab-CD20 less than 6–12 months prior to vaccination had a poorer immune response. Several studies demonstrated that rituximab exposure, especially within 6–12 months, substantially impaired humoral immune responses to various vaccines, including Streptococcus pneumoniae polysaccharide, Haemophilus influenzae type b, influenza, and hepatitis B virus vaccines, in patients with immune thrombocytopenia, rheumatoid arthritis and hematologic malignancies [186,187,188]. This underscores the crucial role of B-lymphocytes in antibody development after immunization.
JAKi, which has initially been investigated for the treatment of myelofibrosis, was the only non-B-cell-directed therapy associated with lower seroconversion rates compared to the untreated subgroup. Furthermore, MPN patients currently treated with JAKi showed lower seroconversion rates compared to those who did not receive JAKi. Notably, there was no heterogeneity in this subgroup analysis. In addition, one study showed a non-significant lower cellular immune response in MPN patients treated with JAKi [111]. The first approved JAKi ruxolitinib inhibits the JAK-STAT pathway, which is required not only for myeloid signaling but also for T-effector cell responses and NK cell functions. Subsequently, ruxolitinib was approved for the treatment of steroid-refractory-acute-graft-versus-host disease [189,190,191]. A study demonstrated a negative correlation with low CD4+ T-cell counts and an antibody response, particularly in MPN patients treated with ruxolitinib [128]. Thus, JAKi may impair immunogenicity following SARS-CoV-2 vaccination by suppressing T-cell response.
Surprisingly, patients receiving chemotherapy, Mab-CD38, IMiD, PI, HSCT, and TKI had estimated seroconversion rates between 75 and 90%, which were comparable to untreated patients. Although Mab-CD38 was associated with impaired serological responses (40–60%) in MM patients in several studies [18, 20, 45, 168], many studies showed approximately 90% seroconversion rates in MM patients treated with Mab-CD38 [27, 58, 100, 109, 154]. Patients undergoing HSCT had a pooled seroconversion rate of 81.2%, which was more slightly impaired in patients with allogeneic HSCT. However, most patients received HSCT over 6–12 months before vaccination. Therefore, immunogenicity following SARS-CoV-2 vaccination after 4–6 months posttransplant could not be adequately determined. Untreated patients, mainly composed of CLL or indolent NHL patients, had a pooled seroconversion rate of 80.4% (95% CI, 73.7–85.8%) suggesting intrinsic impairment of immunogenicity. Patients with untreated CLL are at risk for encapsulated microorganisms due to hypogomaglobulinemia. Untreated CLL patients also have functional T-cell and NK-cell defects as well as complement deficiencies [192]. These may indicate an intrinsic immunosuppressed status underlying poor immunogenicity in untreated CLL and NHL patients.
To overcome poor immunogenicity, booster vaccination has been investigated to elicit immune responses in hematologic malignancy patients. The mRNA vaccines were mainly administered as booster vaccination. Among patients who were seronegative after primary vaccination, a booster dose yielded a modest additional benefit, with only 40% seroconversion after booster. Thus, approximately 20–40% of hematologic malignancy patients remained seronegative despite booster vaccination. Strategies to elicit immune responses, such as a heterologous boosted vaccine, a double-dose booster or a fourth dose, should be explored. Alternatively, long-acting antibody administration, such as a combination of tixagevimab and cilgavimab, may be helpful for patients unable to mount immune responses after multiple doses of vaccination [193].
Although two-thirds of hematologic malignancy patients could attain seroconversion following SARS-CoV-2 vaccination, antibody levels were found lower than those of healthy controls. Due to different methods used to detect antibodies, we were unable to perform a quantitative assessment of antibody levels with hematologic malignancy patients and healthy controls. Among seroconverted patients, it remains uncertain whether their antibody levels are sufficient for prevention of SARS-CoV-2 infection, especially for emerging immune escape variants such as Beta and Omicron. Neutralizing antibody levels are associated with immune protection against symptomatic SARS-CoV-2 infection as well as hospitalization. The 50% in vitro neutralization level for SARS-CoV-2 is approximately 20% of the mean convalescent titer required for 50% protection against symptomatic infection. In contrast, only 3% of the mean convalescent level is required for protection against severe infection [194]. In this meta-analysis, approximately 50% of hematologic malignancy patients attained adequate levels of neutralizing antibodies in vitro. This implies that a significant proportion of seroconverted patients did not have adequate protection from symptomatic SARS-CoV-2 infection. Since the neutralization level required for protection against severe infection is substantially lower, protection against severe disease should be largely retained in seroconverted patients. Neutralizing antibody levels are also predictive of protection against SARS-CoV-2 variants, which escape serum neutralization elicited by primary vaccination series [194, 195]. Booster vaccination demonstrates significantly increased neutralizing titers, which is predicted to provide protection against severe SARS-CoV-2 infection with the current variants of concern, including Omicron [195,196,197]. Therefore, booster vaccination should be offered to hematologic malignancy patients, especially for patients who are seronegative or attain low neutralization levels [82, 167].
Cellular immunity provides protection against severe SARS-CoV-2 infection and death even in hematologic malignancy patients with impaired humoral immunity, including those treated with B-cell depletion therapy [11]. Therefore, cellular immune responses may compensate for deficient humoral immunity in hematologic malignancy patients following SARS-CoV-2 vaccination. This meta-analysis showed that approximately two-thirds of hematologic malignancy patients elicited SARS-CoV-2-specific T-cell responses. However, most studies did not assess cellular immune responses in the entire study population. This may partially explain the high heterogeneity of the estimated cellular immune response following SARS-CoV-2 vaccination. Approximately 20% of hematologic malignancy patients failed to attain humoral and cellular immunity. Booster vaccination demonstrated enhancement of cellular immune responses in hematologic malignancy patients [144, 160, 167]. Thus, booster vaccination should be recommended for hematologic malignancy patients who are at risk for immunological failure after primary vaccination series.
Most studies excluded hematologic malignancy patients with previous SARS-CoV-2 infection or contained a small proportion of patients with previous infection (<5%) during the primary vaccination scheme or booster vaccination. Therefore, we could not perform quantitative analysis to determine the effect of the previous infection on immunogenicity after SARS-CoV-2 vaccination. Bagacean et al. analyzed the additional cohort of 40 CLL patients infected with SARS-CoV-2 prior to vaccination and found that all CLL patients with prior COVID-19 attained seroconversion after a single dose of the mRNA vaccine. Furthermore, the anti-S IgG titers were significantly higher after the first dose of the mRNA vaccine in CLL patients with prior COVID-19 compared with the titers of COVID-19-naive CLL patients who seroconverted after the second dose [74]. In addition, Kohn et al. [86] and Thompson et al. [184] demonstrated that previous SARS-CoV-2 infection was associated with increased seroconversion after booster vaccination in hematologic malignancy patients. These findings suggest a greater boosting effect of vaccination after natural SARS-CoV-2 infection.
This study has been the largest systematic review and meta-analysis evaluating immunogenicity following SARS-CoV-2 vaccination in patients with hematologic malignancies. This meta-analysis contained 170 studies and aggregated over 20,000 patients, including most disease subtypes and treatment modalities for hematologic malignancies. The size of the study provided sufficient power for quantitative assessment of humoral and cellular immunogenicity following primary vaccination scheme and following booster vaccination. In addition, it allowed us to assess the risks associated with impaired immunogenicity due to the disease itself and the therapy used in hematologic malignancy patients. Of note, no publication bias was identified.
This study has some limitations. Considerable heterogeneity was detected in this meta-analysis, suggesting the inherent effects of disease subtypes and the influence of treatment modalities evidenced by our meta-regression analysis. Additionally, patients with lymphoid neoplasms, including MM, CLL, and NHL, are disproportionately included in the studies and may be overrepresented in the entire hematologic malignancy patients. Although subgroup analysis was performed to explore diverse effects of diseases and treatments, noticeable heterogeneity remained detectable in most analyses. This may be partially explained by heterogeneous patient selection in most studies. For example, some studies included patients with different disease states, such as untreated, ongoing therapy, recent and remote discontinuation of treatments. The intervals between prior treatments, such as Mab-CD20 and HSCT, and vaccination were also inconsistently reported and varied greatly. Another limitation was the lack of standard criteria for techniques and cutoff levels to determine both humoral and cellular immune responses following SARS-CoV-2 vaccination. Furthermore, the correlation between detectable immune responses and the efficacy of vaccines in the prevention of symptomatic and severe SARS-CoV-2 infection in hematologic malignancy patients remains undetermined, especially for SARS-CoV-2 variants. There were insufficient data to evaluate the efficacy of SARS-CoV-2 vaccination in this population. Other factors that may affect seroconversion, such as age, comorbidities, and previous SARS-CoV-2 infection, were not evaluated in this analysis due to inadequately disaggregated results from primary studies. Subgroup analysis was not performed on different vaccine platforms due to the preponderance of mRNA vaccines.
Conclusions
This meta-analysis of 170 studies and over 20,000 hematologic malignancy patients demonstrate both impaired humoral and cellular immune responses following primary SARS-CoV-2 vaccination. Booster vaccination enhances immune responses in hematologic malignancy patients and should be offered to patients at high risk of immunological failure, especially those with lymphoid malignancies or those receiving CART, B-cell targeted therapy, or JAKi. Further studies focusing on improving immune responses following SARS-CoV-2 vaccination and immunization for other infectious diseases in hematologic malignancy patients are warranted.
Availability of data and materials
The authors confirm that data supporting the findings of this study are available within the article and its supplementary materials.
References
Worldometer. COVID-19 coronavirus pandemic. 2020. https://www.worldometers.info/coronavirus/ (accessed September 1, 2022).
Pagano L, Salmanton-García J, Marchesi F, Busca A, Corradini P, Hoenigl M, et al. COVID-19 infection in adult patients with hematological malignancies: a European Hematology Association Survey (EPICOVIDEHA). J Hematol Oncol. 2021;14:168.
Krem MM, Nutalapati S, Latta HL, Thomas CZ, Haddad HE, Vilchez GA, et al. Hematologic malignancy patients suffer higher mortality and morbidity from COVID-19 than solid tumor patients. J Clin Oncol. 2021;39:e19048.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–15.
Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384:403–16.
Sadoff J, Gray G, Vandebosch A, Cardenas V, Shukarev G, Grinsztejn B, et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med. 2021;384:2187–201.
Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021;397:99–111.
Maneikis K, Šablauskas K, Ringelevičiũtẽ U, Vaitekẽnaitẽ V, Čekauskienẽ R, Kryžauskaitẽ L, et al. Immunogenicity of the BNT162b2 COVID-19 mRNA vaccine and early clinical outcomes in patients with haematological malignancies in Lithuania: a national prospective cohort study. Lancet Haematol. 2021;8:e583–92.
Becerril-Gaitan A, Vaca-Cartagena BF, Ferrigno AS, Mesa-Chavez F, Barrientos-Gutiérrez T, Tagliamento M, et al. Immunogenicity and risk of severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) infection after Coronavirus Disease 2019 (COVID-19) vaccination in patients with cancer: a systematic review and meta-analysis. Eur J Cancer. 2022;160:243–60.
Corti C, Antonarelli G, Scotté F, Spano JP, Barrière J, Michot JM, et al. Seroconversion rate after vaccination against COVID-19 in patients with cancer-a systematic review. Ann Oncol. 2022;33:158–68.
Bange EM, Han NA, Wileyto P, Kim JY, Gouma S, Robinson J, et al. CD8+ T cells contribute to survival in patients with COVID-19 and hematologic cancer. Nat Med. 2021;27:1280–9.
Kamar N, Abravanel F, Marion O, Couat C, Izopet J, Del Bello A. Three doses of an mRNA Covid-19 vaccine in solid-organ transplant recipients. N. Engl J Med. 2021;385:661–2.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
GA Wells, B Shea, D O’Connell, J Peterson, V Welch, M Losos, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Accessed September 8, 2022. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring in consistency in meta-analyses. BMJ 2003;327:557–60.
Addeo A, Shah PK, Bordry N, Hudson RD, Albracht B, Di Marco M, et al. Immunogenicity of SARS-CoV-2 messenger RNA vaccines in patients with cancer. Cancer Cell. 2021;39:1091–8.
Agha ME, Blake M, Chilleo C, Wells A, Haidar G. Suboptimal response to Coronavirus disease 2019 messenger RNA vaccines in patients with hematologic malignancies: A need for vigilance in the postmasking era. Open Forum Infect Dis. 2021;8:ofab353.
Aleman A, Upadhyaya B, Tuballes K, Kappes K, Gleason CR, Beach K, et al. Variable cellular responses to SARS-CoV-2 in fully vaccinated patients with multiple myeloma. Cancer Cell. 2021;39:1442–4.
Ariamanesh M, Porouhan P, PeyroShabany B, Fazilat-Panah D, Dehghani M, Nabavifard M, et al. Immunogenicity and safety of the inactivated SARS-CoV-2 vaccine (BBIBP-CorV) in patients with malignancy. Cancer Invest. 2022;40:26–34.
Avivi I, Balaban R, Shragai T, Sheffer G, Morales M, Aharon A, et al. Humoral response rate and predictors of response to BNT162b2 mRNA COVID19 vaccine in patients with multiple myeloma. Br J Haematol. 2021;195:186–93.
Benda M, Mutschlechner B, Ulmer H, Grabher C, Severgnini L, Volgger A, et al. Serological SARS-CoV-2 antibody response, potential predictive markers and safety of BNT162b2 mRNA COVID-19 vaccine in haematological and oncological patients. Br J Haematol. 2021;195:523–31.
Benjamini O, Rokach L, Itchaki G, Braester A, Shvidel L, Goldschmidt N, et al. Safety and efficacy of the BNT162b mRNA COVID-19 vaccine in patients with chronic lymphocytic leukemia. Haematologica 2022;107:625–34.
Bergman P, Blennow O, Hansson L, Mielke S, Nowak P, Chen P, et al. Safety and efficacy of the mRNA BNT162b2 vaccine against SARS-CoV-2 in five groups of immunocompromised patients and healthy controls in a prospective open-label clinical trial. EBioMedicine 2021;74:103705.
Bird S, Panopoulou A, Shea R, Tsui M, Saso R, Sud A, et al. Response to SARS-CoV-2 vaccination in patients with Multiple Myeloma using a 12-week spaced dosing strategy. Clin Lymphoma Myeloma Leuk. 2021;21:S114.
Bitoun S, Henry J, Vauloup-Fellous C, Dib N, Belkhir R, Mouna L, et al. Response to COVID-19 mRNA vaccination in multiple myeloma is conserved but impaired compared to controls. J Hematol Oncol. 2021;14:166.
Cattaneo D, Bucelli C, Cavallaro F, Consonni D, Iurlo A. Impact of diagnosis and treatment on response to COVID-19 vaccine in patients with BCR-ABL1-negative myeloproliferative neoplasms. A single-center experience. Blood Cancer J. 2021;11:185.
Chan WY, Howells L, Wilson W, Sanchez E, Ainley L, Chavda SJ, et al. Serological response to the BNT162b2 mRNA or ChAdOx1 nCoV-19 COVID-19 vaccine after first and second doses in patients with plasma cell disorders: influence of host and disease factors. Br J Haematol. 2022;196:e21–6.
Chung DJ, Shah GL, Devlin SM, Ramanathan LV, Doddi S, Pessin MS, et al. Disease- and therapy-specific impact on humoral immune responses to COVID-19 vaccination in hematologic malignancies. Blood Cancer Disco. 2021;2:568–76.
Fendler A, Shepherd STC, Au L, Wilkinson KA, Wu M, Byrne F, et al. Adaptive immunity and neutralizing antibodies against SARS-CoV-2 variants of concern following vaccination in patients with cancer: the CAPTURE study. Nat Cancer. 2021;2:1305–20.
Figueiredo JC, Merin NM, Hamid O, Choi SY, Lemos T, Cozen W, et al. Longitudinal SARS-CoV-2 mRNA vaccine-induced humoral immune responses in patients with cancer. Cancer Res. 2021;81:6273–80.
Fiorino F, Sicuranza A, Ciabattini A, Santoni A, Pastore G, Simoncelli M, et al. The slower antibody response in myelofibrosis patients after two doses of mRNA SARS-CoV-2 vaccine calls for a third dose. Biomedicines 2021;9:1480.
Fox TA, Kirkwood AA, Enfield L, O’Reilly M, Arulogun S, D’Sa S, et al. Low seropositivity and suboptimal neutralisation rates in patients fully vaccinated against COVID-19 with B-cell malignancies. Br J Haematol. 2021;195:706–9.
Gavriatopoulou M, Terpos E, Ntanasis-Stathopoulos I, Briasoulis A, Gumeni S, Malandrakis P, et al. Poor neutralizing antibody responses in 106 patients with WM after vaccination against SARS-CoV-2: a prospective study. Blood Adv. 2021;5:4398–405.
Ghione P, Gu JJ, Attwood K, Torka P, Goel S, Sundaram S, et al. Impaired humoral responses to COVID-19 vaccination in patients with lymphoma receiving B-cell-directed therapies. Blood 2021;138:811–4.
Greenberger LM, Saltzman LA, Senefeld JW, Johnson PW, DeGennaro LJ, Nichols GL. Antibody response to SARS-CoV-2 vaccines in patients with hematologic malignancies. Cancer Cell. 2021;39:1031–3.
Gurion R, Rozovski U, Itchaki G, Gafter-Gvili A, Leibovitch C, Raanani P, et al. Humoral serological response to the BNT162b2 vaccine is abrogated in lymphoma patients within the first 12 months following treatment with anti-CD2O antibodies. Haematologica 2022;107:715–20.
Henriquez S, Zerbit J, Bruel T, Ouedrani A, Planas D, Deschamps P, et al. Anti-CD38 therapy impairs SARS-CoV-2 vaccine response against alpha and delta variants in patients with multiple myeloma. Blood 2022;139:942–6.
Herzog Tzarfati K, Gutwein O, Apel A, Rahimi-Levene N, Sadovnik M, Harel L, et al. BNT162b2 COVID-19 vaccine is significantly less effective in patients with hematologic malignancies. Am J Hematol. 2021;96:1195–203.
Jurgens EM, Ketas TJ, Zhao Z, Joseph Satlin M, Small CB, Sukhu A, et al. Serologic response to mRNA COVID-19 vaccination in lymphoma patients. Am J Hematol. 2021;96:E410–3.
Kozak KE, Ouyang L, Derkach A, Sherman A, McCall SJ, Famulare C, et al. Serum antibody response in patients with philadelphia-chromosome positive or negative myeloproliferative neoplasms following vaccination with SARS-CoV-2 spike protein messenger RNA (mRNA) vaccines. Leukemia 2021;35:3578–80.
Liebers N, Speer C, Benning L, Bruch PM, Kraemer I, Meissner J, et al. Humoral and cellular responses after COVID-19 vaccination in anti-CD20-treated lymphoma patients. Blood 2022;139:142–7.
Lim SH, Campbell N, Johnson M, Joseph-Pietras D, Collins GP, O’Callaghan A, et al. Antibody responses after SARS-CoV-2 vaccination in patients with lymphoma. Lancet Haematol. 2021;8:e542–4.
Schulz E, Hodl I, Forstner P, Hatzl S, Sareban N, Moritz M, et al. CD19+IgD+CD27- naive B cells as predictors of humoral response to COVID 19 mRNA vaccination in immunocompromised patients. Front Immunol. 2021;12:803742.
Re D, Barrière J, Chamorey E, Delforge M, Gastaud L, Petit E, et al. Low rate of seroconversion after mRNA anti-SARS-CoV-2 vaccination in patients with hematological malignancies. Leuk Lymphoma. 2021;62:3308–10.
Pimpinelli F, Marchesi F, Piaggio G, Giannarelli D, Papa E, Falcucci P, et al. Fifth-week immunogenicity and safety of anti-SARS-CoV-2 BNT162b2 vaccine in patients with multiple myeloma and myeloproliferative malignancies on active treatment: preliminary data from a single institution. J Hematol Oncol. 2021;14:81.
Lindemann M, Klisanin V, Thümmler L, Fisenkci N, Tsachakis-Mück N, Ditschkowski M, et al. Humoral and cellular vaccination responses against SARS-CoV-2 in hematopoietic stem cell transplant recipients. Vaccines (Basel). 2021;9:1075.
Tadmor T, Benjamini O, Braester A, Rahav G, Rokach L. Antibody persistence 100 days following the second dose of BNT162b mRNA Covid19 vaccine in patients with chronic lymphocytic leukemia. Leukemia 2021;35:2727–30.
Marlet J, Gatault P, Maakaroun Z, Longuet H, Stefic K, Handala L, et al. Antibody responses after a third dose of COVID-19 vaccine in kidney transplant recipients and patients treated for chronic lymphocytic leukemia. Vaccines (Basel). 2021;9:1055.
Parry H, McIlroy G, Bruton R, Ali M, Stephens C, Damery S, et al. Antibody responses after first and second Covid-19 vaccination in patients with chronic lymphocytic leukaemia. Blood Cancer J. 2021;11:136.
Lockmer S, Uttervall K, Kashif M, Svärd C, Malmsten K, Fletcher-Torres E, et al. Antibody response to COVID-19 mRNA vaccine (Comirnaty) in myeloma patients treated with high-dose melphalan and/or immunotherapy. Am J Hematol. 2021;96:E443–6.
Ollila TA, Lu S, Masel R, Zayac A, Paiva K, Rogers RD, et al. Antibody response to COVID-19 vaccination in adults with hematologic malignant disease. JAMA Oncol. 2021;7:1714–6.
Greenberger LM, Saltzman LA, Senefeld JW, Johnson PW, DeGennaro LJ, Nichols GL. Anti-spike antibody response to SARS-CoV-2 booster vaccination in patients with B cell-derived hematologic malignancies. Cancer Cell. 2021;39:1297–9.
Schiller Salton N, Szwarcwort M, Tzoran I, Horowitz NA, Zuckerman T, Shachor-Meyouhas Y, et al. Attenuated humoral immune response following anti-SARS-CoV-2 vaccine in heavily pretreated patients with multiple myeloma and AL amyloidosis. Am J Hematol. 2021;96:E475–8.
Ramanathan M, Murugesan K, Yang LM, Costales C, Bulterys PL, Schroers-Martin J, et al. Cell-mediated and humoral immune response to 2-dose SARS-CoV2 mRNA vaccination in Immunocompromised patient population. medRxiv 2021.07.21.21260921; https://doi.org/10.1101/2021.07.21.21260921.
Roeker LE, Knorr DA, Thompson MC, Nivar M, Lebowitz S, Peters N, et al. COVID-19 vaccine efficacy in patients with chronic lymphocytic leukemia. Leukemia 2021;35:2703–5.
Perry C, Luttwak E, Balaban R, Shefer G, Morales MM, Aharon A, et al. Efficacy of the BNT162b2 mRNA COVID-19 vaccine in patients with B-cell non-Hodgkin lymphoma. Blood Adv. 2021;5:3053–61.
Van Oekelen O, Gleason CR, Agte S, Srivastava K, Beach KF, Aleman A, et al. Highly variable SARS-CoV-2 spike antibody responses to two doses of COVID-19 RNA vaccination in patients with multiple myeloma. Cancer Cell. 2021;39:1028–30.
Shapiro LC, Thakkar A, Gali R, Gonzalez-Lugo JD, Bazarbachi AH, Rahman S, et al. High seroconversion rates amongst black and Hispanics with hematologic malignancies after SARS-CoV-2 vaccination. Leuk Lymphoma. 2022 May;1-5 [Epub ahead of print].
McKenzie DR, Muñoz-Ruiz M, Monin L, Alaguthurai T, Lechmere T, Abdul-Jawad S, et al. Humoral and cellular immunity to delayed second dose of SARS-CoV-2 BNT162b2 mRNA vaccination in patients with cancer. Cancer Cell. 2021;39:1445–7.
Zeng C, Evans JP, Reisinger S, Woyach J, Liscynesky C, Boghdadly ZE, et al. Impaired neutralizing antibody response to COVID-19 mRNA vaccines in cancer patients. Cell Biosci. 2021;11:197.
Peeters M, Verbruggen L, Teuwen L, Vanhoutte G, Vande Kerckhove S, Peeters B, et al. Reduced humoral immune response after BNT162b2 coronavirus disease 2019 messenger RNA vaccination in cancer patients under antineoplastic treatment. ESMO Open. 2021;6:100274.
Salvini M, Maggi F, Damonte C, Mortara L, Bruno A, Mora B, et al. Immunogenicity of anti-SARS-CoV-2 Comirnaty vaccine in patients with lymphomas and myeloma who underwent autologous stem cell transplantation. Bone Marrow Transpl. 2022;57:137–9.
Piñana JL, López-Corral L, Martino R, Montoro J, Vazquez L, Pérez A, et al. SARS-CoV-2-reactive antibody detection after SARS-CoV-2 vaccination in hematopoietic stem cell transplant recipients: prospective survey from the Spanish Hematopoietic Stem Cell Transplantation and Cell Therapy Group. Am J Hematol. 2022;97:30–42.
Verina D, Van Oekelen O, Gleason C, Agte S, Srivastava K, Beach K, et al. Lesson Learned: Management of patients with Multiple Myeloma (MM) and their response to two doses of COVID-19 RNA vaccine. Clin lymphoma myeloma Leuk. 2021;21:S171.
Malard F, Gaugler B, Gozlan J, Bouquet L, Fofana D, Siblany L, et al. Weak immunogenicity of SARS-CoV-2 vaccine in patients with hematologic malignancies. Blood. Cancer J. 2021;11:142.
Pimpinelli F, Marchesi F, Piaggio G, Giannarelli D, Papa E, Falcucci P, et al. Lower response to BNT162b2 vaccine in patients with myelofibrosis compared to polycythemia vera and essential thrombocythemia. J Hematol Oncol. 2021;14:119.
Thakkar A, Gonzalez-Lugo JD, Goradia N, Gali R, Shapiro LC, Pradhan K, et al. Seroconversion rates following COVID-19 vaccination among patients with cancer. Cancer Cell. 2021;39:1081–90.
Abdallah AO, Mahmoudjafari Z, Atieh T, Ahmed N, Cui W, Shune L, et al. Neutralizing antibody responses against SARS-CoV-2 in patients with plasma cell disorders who are on active treatment after two doses of mRNA vaccination. Eur J Haematol. 2022;109:458–64.
Abid MB, Rubin M, Ledeboer N, Szabo A, Longo W, Mohan M, et al. Efficacy of a third SARS-CoV-2 mRNA vaccine dose among hematopoietic cell transplantation, CAR T cell, and BiTE recipients. Cancer Cell. 2022;40:340–2.
Attolico I, Tarantini F, Carluccio P, Schifone CP, Delia M, Gagliardi VP, et al. Serological response following BNT162b2 anti-SARS-CoV-2 mRNA vaccination in haematopoietic stem cell transplantation patients. Br J Haematol. 2022;196:928–31.
Auteri G, Bartoletti D, Di Pietro C, Sutto E, Mazzoni C, Romagnoli AD, et al. Longer-term response to SARS-CoV-2 vaccine in MPN patients: Role of ruxolitinib and disease severity. Leuk Res. 2022;116:106819.
Avivi I, Luttwak E, Saiag E, Halperin T, Haberman S, Sarig A, et al. BNT162b2 mRNA COVID-19 vaccine booster induces seroconversion in patients with B-cell non-Hodgkin lymphoma who failed to respond to two prior vaccine doses. Br J Haematol. 2022;196:1329–33.
Bacova B, Kohutova Z, Zubata I, Gaherova L, Kucera P, Heizer T, et al. Cellular and humoral immune response to SARS-CoV-2 mRNA vaccines in patients treated with either Ibrutinib or Rituximab. Clin Exp Med. 2022:1–9.
Bagacean C, Letestu R, Al-Nawakil C, Brichler S, Lévy V, Sritharan N, et al. Humoral response to mRNA anti-COVID-19 vaccines BNT162b2 and mRNA-1273 in patients with chronic lymphocytic leukemia. Blood Adv. 2022;6:207–11.
Baker M, Cortes M, Ahn J, Donato ML, Kaur S, Suh HC, et al. Assessment of serology after Sars-Cov-2 vaccine in allogeneic HCT recipients. Blood 2021;138:2900.
Beerlage A, Leuzinger K, Valore L, Mathew R, Junker T, Drexler B, et al. Antibody response to mRNA SARS-CoV-2 vaccination in 182 patients after allogeneic hematopoietic cell transplantation. Transpl Infect Dis. 2022;24:e13828.
Bellesi S, Sali M, Maiolo E, Pereyra Boza MDC, Alma E, Palucci I, et al. Anti CD20-based immunochemotherapy abolishes antibody response to Covid-19 mRNA vaccine in lymphoma patients vaccinated during active first line treatment. Leuk Lymphoma. 2022;63:1474–8.
Blixt L, Wullimann D, Aleman S, Lundin J, Chen P, Gao Y, et al. T-cell immune responses following vaccination with mRNA BNT162b2 against SARS-CoV-2 in patients with chronic lymphocytic leukemia: results from a prospective open-label clinical trial. Haematologica 2022;107:1000–3.
Bordry N, Addeo A, Jaksic C, Dutoit V, Roux-Lombard P, Shah DP, et al. Humoral and cellular immunogenicity two months after SARS-CoV-2 messenger RNA vaccines in patients with cancer. iScience. 2021;25:103699.
Branagan AR, Lei MM, Maron JS, Yee AJ, O’Donnell E, Castillo JJ, et al. COVID-19 vaccine responsiveness in patients with multiple myeloma and Waldenström macroglobulinemia. Blood 2021;138:3801.
Candon S, Lemee V, Leveque E, Etancelin P, Paquin C, Carette M, et al. Dissociated humoral and cellular immune responses after a three-dose schema of BNT162b2 vaccine in patients receiving anti-CD20 monoclonal antibody maintenance treatment for B-cell lymphomas. Haematologica 2022;107:755–8.
Canti L, Ariën KK, Desombere I, Humblet-Baron S, Pannus P, Heyndrickx L, et al. Antibody response against SARS-CoV-2 Delta and Omicron variants after third-dose BNT162b2 vaccination in allo-HCT recipients. Cancer Cell. 2022;40:335–7.
Caocci G, Mulas O, Mantovani D, Costa A, Galizia A, Barabino L, et al. Should be a third dose of BNT162b2 mRNA COVID-19-vaccine administered in patients with myelofibrosis under ruxolitinib? Blood 2021;138:2573.
Cavanna L, Proietto M, Citterio C, Anselmi E, Zaffignani E, Stroppa EM, et al. COVID-19 vaccination in cancer patients older than 70 years undergoing active treatment. Seroconversion rate and safety. Vaccines (Basel). 2022;10:164.
Chang A, Akhtar A, Linderman SL, Lai L, Orellana-Noia VM, Valanparambil R, et al. Humoral responses against SARS-CoV-2 and variants of concern after mRNA vaccines in patients with non-Hodgkin lymphoma and chronic lymphocytic leukemia. J Clin Oncol. 2022;40:3020–31.
Kohn M, Delord M, Chbat M, Guemriche A, Merabet F, Roupie AL, et al. A third anti-SARS-CoV-2 mRNA dose does not overcome the pejorative impact of anti-CD20 therapy and/or low immunoglobulin levels in patients with lymphoma or chronic lymphocytic leukemia. Haematologica 2022;107:1454–59.
Chelysheva EY, Petrova A, Shukhov OA, Gurianova M, Bykova A, Nemchenko I, et al. Humoral immunity and adverse events after vaccination against COVID-19 by a vector based vaccine Sputnik V in patients with chronic myeloid leukemia. Blood 2021;138:4599.
Chopra M, Jain A, Chhabra S, Kaundal S, Singh C, Jandial A, et al. Short research communication anti-spike antibody response to COVISHIELD™ (SII-ChAdOx1 nCoV-19) vaccine in patients with B-cell and plasma cell malignancies and hematopoietic cell transplantation recipients. Indian J Hematol Blood Transfus. 2022;38:745–9.
Chumsri S, Advani PP, Pai TS, Li Z, Mummareddy A, Acampora M, et al. Humoral responses after SARS-CoV-2 mRNA vaccination and breakthrough infection in cancer patients. Mayo Clin Proc Innov Qual Outcomes. 2022;6:120–5.
Claudiani S, Apperley JF, Parker EL, Marchesin F, Katsanovskaja K, Palanicawandar R, et al. Durable humoral responses after the second anti-SARS-CoV-2 vaccine dose in chronic myeloid leukaemia patients on tyrosine kinase inhibitors. Br J Haematol. 2022;197:e1–e4.
Clémenceau B, Guillaume T, Coste-Burel M, Peterlin P, Garnier A, Le Bourgeois A, et al. SARS-CoV-2 T-cell responses in allogeneic hematopoietic stem cell recipients following two doses of BNT162b2 mRNA vaccine. Vaccines (Basel). 2022;10:448.
Corradini P, Agrati C, Apolone G, Mantovani A, Giannarelli D, Marasco V, et al. Humoral and T-cell immune response after three doses of mRNA SARS-CoV-2 vaccines in fragile patients: the Italian VAX4FRAIL study. Clin Infect Dis. 2022 May:ciac404. https://doi.org/10.1093/cid/ciac404. [Epub ahead of print].
da Cunha-Bang C, Kirkby NS, Friis-Hansen L, Niemann CU. Serological response following vaccination with BNT162b2 mRNA in patients with chronic lymphocytic leukemia. Leuk Lymphoma. 2022;63:503–5.
Del Poeta G, Bomben R, Polesel J, Rossi FM, Pozzo F, Zaina E, et al. COVID-19 vaccination: evaluation of risk for protection failure in chronic lymphocytic leukemia patients. Hematol Oncol. 2021;39:712–4.
Dong N, Jain AG, Tan ES, Ball S, Whiting J, Gaballa S, et al. Immunogenicity of Sars-Cov-2 mRNA 1273 vaccine in patients with lymphoid malignancies. Blood 2021;138:2504.
Ehmsen S, Asmussen A, Jeppesen SS, Nilsson AC, Østerlev S, Kragh A, et al. Antibody responses following third mRNA COVID-19 vaccination in patients with cancer and potential timing of a fourth vaccination. Cancer Cell. 2022;40:338–9.
Enßle JC, Campe J, Schwenger A, Wiercinska E, Hellstern H, Dürrwald R, et al. Severe impairment of T-cell responses to BNT162b2 immunization in patients with multiple myeloma. Blood 2022;139:137–42.
Gastinne T, Le Bourgeois A, Coste-Burel M, Guillaume T, Peterlin P, Garnier A, et al. Safety and antibody response after one and/or two doses of BNT162b2 Anti-SARS-CoV-2 mRNA vaccine in patients treated by CAR T cells therapy. Br J Haematol. 2022;196:360–2.
Gavriatopoulou M, Terpos E, Malandrakis P, Ntanasis-Stathopoulos I, Briasoulis A, Gumeni S, et al. Myeloma patients with COVID-19 have superior antibody responses compared to patients fully vaccinated with the BNT162b2 vaccine. Br J Haematol. 2022;196:356–9.
Ghandili S, Schönlein M, Wiessner C, Becher H, Lütgehetmann M, Brehm TT, et al. Lymphocytopenia and anti-CD38 directed treatment impact the serological SARS-CoV-2 response after prime boost vaccination in patients with multiple myeloma. J Clin Med. 2021;10:5499.
Giuliano AR, Lancet JE, Pilon-Thomas S, Dong N, Jain AG, Tan E, et al. Evaluation of antibody response to SARS-CoV-2 mRNA-1273 vaccination in patients with cancer in Florida. JAMA Oncol. 2022;8:748–54.
Goel S, Gu JJ, Torka P, Mavis C, Sundaram S, Neiders M, et al. Determinants of COVID-19 vaccine response in patients with lymphoma on B cell directed therapy. Blood 2021;138:1340.
Goessi S, Bacher U, Haslebacher C, Nagler M, Staehelin C, Novak U, et al. Poor humoral responses to mRNA vaccines against SARS-CoV-2 in patients after CAR-T-cell therapy. Swiss Med Wkly. 2021;151:6S.
Goksu SY, Rolwes J, Premnath N, Patel P, Ikpefan R, Kaur G, et al. COVID vaccine antibody responses in patients with hematologic malignancies in a myeloid enriched cohort: a better antibody response in patients with myeloid malignancies than B-cell malignancies. Blood 2021;138:4134.
Greenberger LM, Saltzman LA, Senefeld JW, Johnson PW, DeGennaro LJ, Nichols GL. Sars-Cov-2 antibody levels in blood cancer patients after a third Sars-Cov-2 “Booster” vaccination - observational data from the LLS National Registry. Blood 2021;138:185.
Mencoboni M, Fontana V, Damiani A, Spitaleri A, Raso A, Bottaro LC, et al. Antibody response to COVID-19 mRNA vaccines in oncologic and hematologic patients undergoing chemotherapy. Curr Oncol. 2022;29:3364–74.
Gressens SB, Fourati S, Le Bouter A, Le Bras F, Dupuis J, Hammoud M, et al. Anti-SARS-CoV-2 antibody response after 2 and 3 doses of BNT162b2 mRNA vaccine in patients with lymphoid malignancies. Clin Microbiol Infect. 2022;28:885.e7–885.e11.
Guerra VA, Ocampo M, Cusnir M. Sars-CoV2 antibody responses in patients with hematological malignancies following anti-CD20 therapy. Blood 2021;138:3554.
Haggenburg S, Lissenberg-Witte BI, van Binnendijk RS, den Hartog G, Bhoekhan MS, Haverkate NJE, et al. Quantitative analysis of mRNA-1273 COVID-19 vaccination response in immunocompromised adult hematology patients. Blood Adv. 2022;6:1537–46.
Haidar G, Agha M, Bilderback A, Lukanski A, Linstrum K, Troyan R, et al. Prospective Evaluation of Coronavirus Disease 2019 (COVID-19) vaccine responses across a broad spectrum of immunocompromising conditions: the COVID-19 vaccination in the immunocompromised study (COVICS). Clin Infect Dis. 2022;75:e630–e644.
Harrington P, Doores KJ, Saunders J, de Lord M, Saha C, Lechmere T, et al. Impaired humoral and T cell response to vaccination against SARS-CoV-2 in chronic myeloproliferative neoplasm patients treated with ruxolitinib. Blood Cancer J. 2022;12:73.
Haydu JE, Maron JS, Redd RA, Gallagher KME, Fischinger S, Barnes JA, et al. Humoral and cellular immunogenicity of SARS-CoV-2 vaccines in chronic lymphocytic leukemia: a prospective cohort study. Blood Adv. 2022;6:1671–83.
Helfgott DC, Racine-Brzostek S, Short KJ, Zhao Z, Christos P, Nino I, et al. Immunogenicity of COVID-19 mRNA Vaccines in Patients with Acute Myeloid Leukemia and Myelodysplastic Syndrome. medRxiv 2022.01.26.22269932; https://doi.org/10.1101/2022.01.26.22269932.
Herishanu Y, Avivi I, Aharon A, Shefer G, Levi S, Bronstein Y, et al. Efficacy of the BNT162b2 mRNA COVID-19 vaccine in patients with chronic lymphocytic leukemia. Blood 2021;137:3165–73.
Herishanu Y, Rahav G, Levi S, Braester A, Itchaki G, Bairey O, et al. Efficacy of a third BNT162b2 mRNA COVID-19 vaccine dose in patients with CLL who failed standard 2-dose vaccination. Blood 2022;139:678–85.
Molica S, Giannarelli D, Lentini M, Zappala D, Loiacono D, Gianfelici V, et al. A clue to better select chronic lymphocytic leukemia patients with optimal response to BNT162b2 mRNA COVID-19 vaccine. Blood 2021;138:3740.
Wu AHB, Wang CC, Ong CM, Lynch KL. Adequate antibody response to COVID-19 vaccine in patients with monoclonal gammopathies and light chain amyloidosis. Lab Med. 2022;53:314–9.
How J, Gallagher KME, Liu Y, Katsis K, Elder EL, Larson RC, et al. Antibody and T-cell responses to SARS-CoV-2 vaccination in myeloproliferative neoplasm patients. Leukemia 2022;36:1176–9.
Schena M, Alliod V, Cucchi M, Alvaro MR, Mozzicafreddo A, Trogu A, et al. Antibody immunoresponse to antiSars-COV2 vaccine in cancer patients. Tumori 2021;107:169.
Maillard A, Redjoul R, Klemencie M, Labussière Wallet H, Le Bourgeois A, et al. Antibody response after 2 and 3 doses of SARS-CoV-2 mRNA vaccine in allogeneic hematopoietic cell transplant recipients. Blood 2022;139:134–7.
Narita K, Nakaji S, Tabata R, Terao T, Kuzume A, Tsushima T, et al. Antibody response to COVID-19 vaccination in patients with lymphoma. Int J Hematol. 2022;115:728–36.
Huang A, Cicin-Sain C, Pasin C, Epp S, Audigé A, Müller NJ, et al. Antibody response to SARS-CoV-2 vaccination in patients following allogeneic hematopoietic cell transplantation. Transpl Cell Ther. 2022;28:214.e1–214.e11.
Rotterdam J, Thiaucourt M, Weiss C, Schwaab J, Reiter A, Kreil S, et al. Definition of factors associated with negative antibody response after COVID-19 vaccination in patients with hematological diseases. Ann Hematol. 2022;101:1825–34.
Molina JG. Anti-spike (S) antibody production post Covid-19 vaccination after B cell depleting therapy (BCDT) for Non-Hodgkin Lymphoma (NHL). Blood 2021;138:2486.
Tvito A, Ronson A, Ghosheh R, Kharit M, Ashkenazi J, Magen S, et al. Anti-CD20 monoclonal antibodies inhibit seropositive response to Covid-19 vaccination in non-Hodgkin lymphoma patients within 6 months after treatment. Exp Hematol. 2022;107:20–3.
Jullien M, Le Bourgeois A, Coste-Burel M, Peterlin P, Garnier A, Rimbert M, et al. B cell aplasia is the most powerful predictive marker for poor humoral response after BNT162b2 mRNA SARS-CoV-2 vaccination in recipients of allogeneic hematopoietic stem cell transplantation. Transpl Cell Ther. 2022;28:279.e1–279.e4.
Tanguay M, Boutin M, Laumaea A, Salaciak M, Mendoza A, Cassis C, et al. B-cell cytopenia and time to last B-cell-depleting therapy predict response to SARS-COV-2 vaccines in patients with lymphoproliferative disorders. Vaccine 2022;40:1203–7.
Ikeda D, Terao T, Miura D, Narita K, Fukumoto A, Kuzume A, et al. Impaired antibody response following the second dose of the BNT162b2 vaccine in patients with myeloproliferative neoplasms receiving ruxolitinib. Front Med (Lausanne). 2022;9:826537.
Infante MS, Marín IGG, Muñoz C, Foncillas MA, Landete E, Churruca J, et al. Impaired antibody response after mRNA COVID-19 vaccination in patients with chronic lymphocytic leukemia. Leuk Lymphoma. 2021;62:S122–S123.
Itchaki G, Rokach L, Benjamini O, Bairey O, Sabag A, Vernitsky H, et al. Cellular immune responses to BNT162b2 mRNA COVID-19 vaccine in patients with chronic lymphocytic leukemia. Blood 2021;138:638.
Izaguirre NE, Sherman AC, Crombie J, Desjardins M, Cheng C, Gilboa T, et al. Immunogenicity of COVID-19 mRNA vaccines in patients with lymphoid malignancies. Open Forum Infect Dis. 2021;8:S395–S396.
Jain AG, Dong NC, Ball S, Tan ES, Whiting J, Komrokji RS, et al. Responses to Sars-Cov-2 vaccines in patients with myelodysplastic syndrome and acute myeloid leukemia. Blood 2021;138:217.
Jenner MW, Hall A, Faustini SE, Pitchford A, de Tute RM, Roberts S, et al. Response to COVID-19 vaccines in patients receiving intensified post-ASCT Therapy with Daratumumab, Lenalidomide, Bortezomib (Dara-VR) due to ultra-high risk (UHiR) newly diagnosed myeloma (NDMM) or primary plasma cell leukemia (pPCL): exploratory analysis of the UK optimum/muknine trial. Blood 2021;138:2699.
Jiménez M, Roldán E, Fernández-Naval C, Villacampa G, Martinez-Gallo M, Medina-Gil D, et al. Cellular and humoral immunogenicity of the mRNA-1273 SARS-CoV-2 vaccine in patients with hematologic malignancies. Blood Adv. 2022;6:774–84.
Lim SH, Campbell N, Stuart B, Johnson M, Joseph-Pietras D, Kelly A, et al. Humoral and cellular responses to SARS-CoV-2 vaccination in patients with lymphoid malignancies. medRxiv 2021.12.08.21266760; https://doi.org/10.1101/2021.12.08.21266760.
Khan QJ, Bivona CR, Liu B, Nelson M, Martin GA, Mushtaq MU, et al. Prospective longitudinal study of kinetics of humoral response to one, two, or three doses of SARS-CoV-2 vaccine in hematopoietic cell transplant recipients. Bone Marrow Transpl. 2022;57:1013–6.
Majcherek M, Matkowska-Kocjan A, Szymczak D, Karasek M, Szeremet A, Kiraga A, et al. Two Doses of BNT162b2 mRNA vaccine in patients after hematopoietic stem cell transplantation: humoral response and serological conversion predictors. Cancers (Basel). 2022;14:325.
Terpos E, Gavriatopoulou M, Ntanasis-Stathopoulos I, Briasoulis A, Gumeni S, Malandrakis P, et al. Booster BNT162b2 optimizes SARS-CoV-2 humoral response in patients with myeloma: the negative effect of anti-BCMA therapy. Blood 2022;139:1409–12.
Shree T, Shankar V, Lohmeyer JJK, Czerwinski DK, Schroers-Martin JG, Rodriguez GM, et al. CD20-targeted therapy ablates De Novo antibody response to vaccination but spares preestablished immunity. Blood Cancer Disco. 2022;3:95–102.
Yang LM, Costales C, Ramanathan M, Bulterys PL, Murugesan K, Schroers-Martin J, et al. Cellular and humoral immune response to SARS-CoV-2 vaccination and booster dose in immunosuppressed patients: an observational cohort study. J Clin Virol. 2022;153:105217.
Mehta-Shah N, Bartlett NL, Kahl B, Watkins MP, Dubois A, Schmelzle G, et al. COVID-19 booster vaccines generate seroconversion in subset of patients with lymphoma/CLL: single institution experience. Leuk Lymphoma. 2022;63:1723–7.
Malard F, Gaugier B, Gozlan J, Bouquet L, Fofana D, Van De Wyngaert Z, et al. Immunogenicity of SARS-CoV-2 vaccine in patients with multiple myeloma. Clin Lymphoma Myeloma Leuk. 2021;21:S117.
Mancuso K, Zamagni E, Solli V, Gabrielli L, Pantani L, Rocchi S, et al. High humoral response after anti-Sars-Cov-2 mRNA-based vaccines in patients with active multiple myeloma (MM) and relationship with disease status/line of therapy. Blood 2021;138:4732.
Mellinghoff SC, Mayer L, Robrecht S, Weskamm LM, Dahlke C, Gruell H, et al. SARS-CoV-2-specific cellular response following third COVID-19 vaccination in patients with chronic lymphocytic leukemia. Haematologica 2022;107:2480–4.
Marasco V, Carniti C, Guidetti A, Farina L, Magni M, Miceli R, et al. T-cell immune response after mRNA SARS-CoV-2 vaccines is frequently detected also in the absence of seroconversion in patients with lymphoid malignancies. Br J Haematol. 2022;196:548–58.
Marchesi F, Pimpinelli F, Giannarelli D, Ronchetti L, Papa E, Falcucci P, et al. Impact of anti-CD20 monoclonal antibodies on serologic response to BNT162b2 vaccine in B-cell Non-Hodgkin’s lymphomas. Leukemia 2022;36:588–90.
Morsink LM, van Doesum J, Choi G, Hazenberg CLE, Biswana A, Meppelink F, et al. Robust COVID-19 vaccination response after allogeneic stem cell transplantation using post transplantation cyclophosphamide conditioning. Blood Cancer J. 2022;12:6.
Marchesi F, Pimpinelli F, Sperandio E, Papa E, Falcucci P, Pontone M, et al. The 12-week kinetics of anti-SARS-CoV-2 antibodies in different haematological cancers after vaccination with BNT162b2. Br J Haematol. 2022;196:362–7.
Nooka AK, Shanmugasundaram U, Cheedarla N, Verkerke H, Edara VV, Valanparambil R, et al. Determinants of neutralizing antibody response after SARS CoV-2 vaccination in patients with myeloma. J Clin Oncol. 2022;40:3057–64.
Obeid M, Suffiotti M, Pellaton C, Bouchaab H, Cairoli A, Salvadé V, et al. Humoral responses against variants of concern by COVID-19 mRNA vaccines in immunocompromised patients. JAMA Oncol. 2022;8:e220446.
Minehart JC, Catania C, Perry L, Martin ME, Smith J, McCurdy SR, et al. Incidence and predictors of Sars-Cov-2 antibody responses following COVID-19 vaccination in allogeneic stem cell transplant recipients. Blood 2021;138:2888.
Pagano L, Salmanton-García J, Marchesi F, López-García A, Lamure S, Itri F, et al. COVID-19 in vaccinated adult patients with hematological malignancies: preliminary results from EPICOVIDEHA. Blood 2022;139:1588–92.
Shen Y, Freeman JA, Holland J, Solterbeck A, Naidu K, Soosapilla A, et al. COVID-19 vaccine failure in chronic lymphocytic leukaemia and monoclonal B-lymphocytosis; humoural and cellular immunity. Br J Haematol. 2022;197:41–51.
Shah MR, Gabel A, Beers S, Salaru G, Lin Y, Cooper DL. COVID-19 vaccine responses in patients with plasma cell dyscrasias after complete vaccination. Clin Lymphoma Myeloma Leuk. 2022;22:e321–e326.
Wagner A, Garner-Spitzer E, Schötta A, Orola M, Wessely A, Zwazl I, et al. Humoral and cellular immune responses and their kinetics vary in dependence of diagnosis and treatment in immunocompromised patients upon COVID-19 mRNA vaccination. medRxiv 2021.12.13.21267603; https://doi.org/10.1101/2021.12.13.21267603.
Shapiro LC, Thakkar A, Campbell ST, Forest SK, Pradhan K, Gonzalez-Lugo JD, et al. Efficacy of booster doses in augmenting waning immune responses to COVID-19 vaccine in patients with cancer. Cancer Cell. 2022;40:3–5.
Reimann P, Ulmer H, Mutschlechner B, Benda M, Severgnini L, Volgger A, et al. Efficacy and safety of heterologous booster vaccination with Ad26.COV2.S after BNT162b2 mRNA COVID-19 vaccine in haemato-oncological patients with no antibody response. Br J Haematol. 2022;196:577–84.
Singal M, Kashinath SK, Mustafa SS, Walsh E, Vadamalai K, Jamshed S, et al. Evaluation of antibody response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) immunizations in patients with B-cell malignancies. Blood 2021;138:4681.
Ramasamy K, Sadler R, Jeans S, Weeden P, Varghese S, Turner A, et al. Immune response to COVID-19 vaccination is attenuated by poor disease control and antimyeloma therapy with vaccine driven divergent T-cell response. Br J Haematol. 2022;197:293–301.
Re D, Seitz-Polski B, Brglez V, Carles M, Graça D, Benzaken S, et al. Humoral and cellular responses after a third dose of SARS-CoV-2 BNT162b2 vaccine in patients with lymphoid malignancies. Nat Commun. 2022;13:864.
Yeshurun M, Pasvolsky O, Shargian L, Yahav D, Ben-Zvi H, Rubinstein M, et al. Humoral serological response to the BNT162b2 vaccine after allogeneic haematopoietic cell transplantation. Clin Microbiol Infect. 2022;28:303.e1–303.e4.
Parry H, McIlroy G, Bruton R, Damery S, Tyson G, Logan N, et al. Impaired neutralisation of SARS-CoV-2 delta variant in vaccinated patients with B cell chronic lymphocytic leukaemia. J Hematol Oncol. 2022;15:3.
Petzer V, Steiner N, Angelova-Unterberger O, Hetzenauer G, Philipp-Abbrederis K, Willenbacher E, et al. Serologic responses to COVID-19 vaccines in hematological patients are predominantly impaired in lymphoid but not in myeloid malignancies hemasphere. 2022;6:e686.
Pia AD, Kim GY, Ip A, Ahn J, Liu Y, Kats S, et al. Production of anti-spike antibodies in response to COVID vaccine in lymphoma patients. medRxiv 2022.03.24.22272883; https://doi.org/10.1101/2022.03.24.22272883.
Robinson A, Mazurek A, Xu M, Gong Y. Quantitative analysis of SARS-CoV-2 antibody status between patients with cancer and healthy individuals with extended vaccination dosing intervals in Canada. Curr Oncol. 2021;29:68–76.
Tamari R, Politikos I, Knorr D, Vardhana S, Young J, Marcello L, et al. Timing and Immune Status after Cellular Therapies Predict Response to COVID-19 Vaccines. Blood 2021;138:3891.
Storti P, Marchica V, Vescovini R, Franceschi V, Russo L, Notarfranchi L, et al. Immune response to SARS-CoV-2 mRNA vaccination and booster dose in patients with multiple myeloma and monoclonal gammopathies: impact of Omicron variant on the humoral response. Oncoimmunology 2022;11:2120275.
Tamariz-Amador LE, Battaglia AM, Maia C, Zherniakova A, Guerrero C, Zabaleta A, et al. Immune biomarkers to predict SARS-CoV-2 vaccine effectiveness in patients with hematological malignancies. Blood Cancer J. 2021;11:202.
Tomowiak C, Leblond V, Laribi K, Baron M, Puppinck C, Gérard P, et al. Response to vaccination against SARS-CoV-2 in 168 patients with Waldenström macroglobulinaemia: a French Innovative Leukaemia Organization study. Br J Haematol. 2022;197:424–7.
Sertić Z, Lucijanic M, Bašić-Kinda S, Seiwerth RS, Periša V, Sertić D, et al. Serologic responses following Sars-Cov-2 vaccination and factors influencing it in patients with hematological malignant and non-malignant diseases: a prospective multicentric study. Blood 2021;138:47.
Ujjani C, Shadman M, Lynch RC, Tu B, Stevenson PA, Grainger C, et al. The impact of B-cell-directed therapy on SARS-CoV-2 vaccine efficacy in chronic lymphocytic leukaemia. Br J Haematol. 2022;197:306–9.
Shields AM, Venkatachalam S, Shafeek S, Paneesha S, Ford M, Sheeran T, et al. SARS-CoV-2 vaccine responses following CD20-depletion treatment in patients with haematological and rheumatological disease: a West Midlands Research Consortium study. Clin Exp Immunol. 2022;207:3–10.
Schönlein M, Wrage V, Ghandili S, Mellinghoff SC, Brehm TT, Leypoldt LB, et al. Risk factors for poor humoral response to primary and booster SARS-CoV-2 vaccination in hematologic and oncological outpatients-COVIDOUT study. Cancer Cell. 2022;40:581–3.
Schubert L, Koblischke M, Schneider L, Porpaczy E, Winkler F, Jaeger U, et al. Immunogenicity of COVID-19 vaccinations in hematological patients: 6-month follow-up and evaluation of a 3rd vaccination. Cancers (Basel). 2022;14:1962.
Saiag E, Grupper A, Avivi I, Elkayam O, Ram R, Herishanu Y, et al. The effect of a third-dose BNT162b2 vaccine on anti-SARS-CoV-2 antibody levels in immunosuppressed patients. Clin Microbiol Infect. 2022;28:735.e5–735.
Sesques P, Bachy E, Ferrant E, Safar V, Gossez M, Morfin-Sherpa F, et al. Immune response to three doses of mRNA SARS-CoV-2 vaccines in CD19-targeted chimeric antigen receptor T cell immunotherapy recipients. Cancer Cell. 2022;40:236–7.
Riise J, Meyer S, Blaas I, Chopra A, Tran TT, Delic-Sarac M, et al. Rituximab-treated patients with lymphoma develop strong CD8 T-cell responses following COVID-19 vaccination. Br J Haematol. 2022;197:697–708.
Terpos E, Gavriatopoulou M, Fotiou D, Giatra C, Asimakopoulos I, Dimou M, et al. Poor neutralizing antibody responses in 132 patients with CLL, NHL and HL after vaccination against SARS-CoV-2: a prospective study. Cancers (Basel). 2021;13:4480.
Stampfer SD, Goldwater MS, Regidor B, Jew SK, Bujarski SE, Chen H, et al. Sars-Cov-2 antibody decay monitoring in mRNA vaccinated multiple myeloma patients. Blood 2021;138:2712.
Ram R, Hagin D, Kikozashvilli N, Freund T, Amit O, Bar-On Y, et al. Safety and immunogenicity of the BNT162b2 mRNA COVID-19 vaccine in patients after allogeneic HCT or CD19-based CART therapy-a single-center prospective cohort study. Transpl Cell Ther. 2021;27:788–94.
Terao T, Yamashita T, Fukumoto A, Kamura Y, Ikeda D, Kuzume A, et al. Low clinical protective response to SARS-CoV-2 mRNA COVID-19 vaccine in patients with multiple myeloma. Int J Hematol. 2022;115:737–47.
Šušol O, Hájková B, Zelená H, Hájek R. Third dose of COVID-19 vaccine restores immune response in patients with haematological malignancies after loss of protective antibody titres. Br J Haematol. 2022;197:302–5.
Ollila TA, Masel RH, Reagan JL, Lu S, Rogers RD, Paiva KJ, et al. Seroconversion and outcomes after initial and booster COVID-19 vaccination in adults with hematologic malignancies. Cancer 2022;128:3319–29.
Thompson MA, Hallmeyer S, Fitzpatrick VE, Liao Y, Mullane MP, Medlin SC, et al. Real-world third COVID-19 vaccine dosing and antibody response in patients with hematologic malignancies. J Patient Cent Res Rev. 2022;9:149–57.
Haggenburg S, Hofsink Q, Lissenberg-Witte BI, Broers AEC, van Doesum JA, van Binnendijk RS, et al. Antibody response in immunocompromised patients with hematologic cancers who received a 3-dose mRNA-1273 vaccination schedule for COVID-19. JAMA Oncol. 2022;8:1477–83.
van Assen S, Holvast A, Benne CA, Posthumus MD, van Leeuwen MA, Voskuyl AE, et al. Humoral responses after influenza vaccination are severely reduced in patients with rheumatoid arthritis treated with rituximab. Arthritis Rheum. 2010;62:75–81.
Nazi I, Kelton JG, Larché M, Snider DP, Heddle NM, Crowther MA, et al. The effect of rituximab on vaccine responses in patients with immune thrombocytopenia. Blood 2013;122:1946–53.
Araujo-Neto JM, Guimarães GS, Fernandes FF, Soares MA, Hepatitis B. Surface antibody (Anti-HBs) kinetics during rituximab chemotherapy and performance of hepatitis B vaccine before immunosuppression: two prospective studies. Viruses 2022;14:1780.
Spoerl S, Mathew NR, Bscheider M, Schmitt-Graeff A, Chen S, Mueller T, et al. Activity of therapeutic JAK 1/2 blockade in graft-versus-host disease. Blood 2014;123:3832–42.
Schönberg K, Rudolph J, Vonnahme M, Parampalli Yajnanarayana S, Cornez I, Hejazi M, et al. JAK inhibition impairs NK cell function in myeloproliferative neoplasms. Cancer Res. 2015;75:2187–99.
Zeiser R, von Bubnoff N, Butler J, Mohty M, Niederwieser D, Or R, et al. Ruxolitinib for glucocorticoid-refractory acute graft-versus-host disease. N. Engl J Med. 2020;382:1800–10.
Tsiodras S, Samonis G, Keating MJ, Kontoyiannis DP. Infection and immunity in chronic lymphocytic leukemia. Mayo Clin Proc. 2000;75:1039–54.
Levin MJ, Ustianowski A, De Wit S, Launay O, Avila M, Templeton A, et al. Intramuscular AZD7442 (Tixagevimab–Cilgavimab) for prevention of Covid-19. N. Engl J Med. 2022;386:2188–200.
Khoury DS, Cromer D, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat Med. 2021;27:1205–11.
Cromer D, Steain M, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, et al. Neutralising antibody titres as predictors of protection against SARS-CoV-2 variants and the impact of boosting: a meta-analysis. Lancet Microbe. 2022;3:e52–e61.
Cele S, Jackson L, Khoury DS, Khan K, Moyo-Gwete T, Tegally H, et al. Omicron extensively but incompletely escapes Pfizer BNT162b2 neutralization. Nature 2022;602:654–6.
Gruell H, Vanshylla K, Tober-Lau P, Hillus D, Schommers P, Lehmann C, et al. mRNA booster immunization elicits potent neutralizing serum activity against the SARS-CoV-2 Omicron variant. Nat Med. 2022;28:477–80.
Author information
Authors and Affiliations
Contributions
N.U. was involved in conceptualization, database search, screening of abstracts and full texts, data extraction and analysis, quality appraisal, and writing the original manuscript; P.P. was involved in database search, screening of abstracts and full texts, data extraction, quality appraisal and writing of the manuscript; N.T. was involved in adjudication, data analysis, appraisal and editing of the manuscript; T.C. was involved in data analysis, appraisal and editing of the manuscript; and P.R. was involved in appraisal and editing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Uaprasert, N., Pitakkitnukun, P., Tangcheewinsirikul, N. et al. Immunogenicity and risks associated with impaired immune responses following SARS-CoV-2 vaccination and booster in hematologic malignancy patients: an updated meta-analysis. Blood Cancer J. 12, 173 (2022). https://doi.org/10.1038/s41408-022-00776-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41408-022-00776-5