Abstract
The efficacy of SARS-CoV-2 vaccination in patients with hematological malignancies (HM) appears limited due to disease and treatment-associated immune impairment. We conducted a systematic review of prospective studies published from 10/12/2021 onwards in medical databases to assess clinical efficacy parameters, humoral and cellular immunogenicity and adverse events (AE) following two doses of COVID-19 approved vaccines. In 57 eligible studies reporting 7393 patients, clinical outcomes were rarely reported and rates of SARS-CoV-2 infection (range 0–11.9%), symptomatic disease (0–2.7%), hospital admission (0–2.8%), or death (0–0.5%) were low. Seroconversion rates ranged from 38.1–99.1% across studies with the highest response rate in myeloproliferative diseases and the lowest in patients with chronic lymphocytic leukemia. Patients with B-cell depleting treatment had lower seroconversion rates as compared to other targeted treatments or chemotherapy. The vaccine-induced T-cell response was rarely and heterogeneously reported (26.5–85.9%). Similarly, AEs were rarely reported (0–50.9% ≥1 AE, 0–7.5% ≥1 serious AE). In conclusion, HM patients present impaired humoral and cellular immune response to COVID-19 vaccination with disease and treatment specific response patterns. In light of the ongoing pandemic with the easing of mitigation strategies, new approaches to avert severe infection are urgently needed for this vulnerable patient population that responds poorly to current COVID-19 vaccine regimens.
Similar content being viewed by others
Introduction
The ongoing coronavirus disease 2019 (COVID-19) pandemic causes immense mortality and morbidity [1]. Patients with hematological malignancies (HM) have a higher risk of infection after exposure, a worse prognosis after infection, and a higher risk of severe or critical disease and COVID-19-related complications due to disease and/or treatment associated with complex immune dysfunction [2,3,4,5].
Vaccines were shown to be a key element to prevent severe diseases resulting in hospitalization and death in most patients [6]. Current evidence proves impaired vaccine-induced immune response in immunocompromised individuals with HM [7, 8]. At the same time, data regarding vaccination to mitigate sequelae by SARS-CoV-2 variants of concern (VOC) is indicative of reduced neutralizing activity and protective efficacy of vaccination, compared to the wild type or less pathogenic variants [9, 10]. Ongoing studies evaluating booster vaccinations and the aim to develop adjusted vaccines addressing VOCs are of utmost importance—especially when considering their impact on vulnerable patient groups, such as immunocompromised individuals [11].
COVID-19 vaccine immunity is mediated by the interplay of humoral and cellular components [12]. In many HM patients a disease-induced dysfunction of the innate and adaptive immune system, as well as a treatment-related immune deficiency, severely impacts the immune response following COVID-19 vaccination. Mechanisms underlying protection against COVID-19 are not yet fully understood. There is already strong evidence that the humoral response is required to prevent infection, while the cellular response seems to be critical for the prevention of severe disease. Yet, the humoral response may not always correlate with T-cell-mediated immunity in immunocompromised patients [13,14,15]. Data evaluating the vaccine-induced immune response is generally scarce for HM patients since most clinical trials initially excluded such patients. In the past months, several studies have investigated vaccine-induced immunogenicity in patients with cancer and indicated a decreased immune response to COVID-19 vaccines. A better understanding of the immune response to SARS-CoV-2 vaccination in these individuals is critical for optimizing vaccination programs, identifying particularly vulnerable patient groups and areas of unmet need, and thereby reducing severe disease and mortality.
As people with HM are at high risk of severe disease after infection with SARS-CoV-2 [16], and research on vaccine effectiveness in this population is generally scarce, there is an urgent ongoing need to evaluate the effectiveness, immunogenicity, and safety of COVID-19 vaccines for these individuals. There are several studies reporting on the effects of COVID-19 vaccines in hematological and oncological patients [17,18,19,20,21]. However, a comprehensive synthesis of the available evidence and evaluation of patient-relevant outcomes is needed to support disease prevention and the identification of optimized vaccination schedules. Thus, the objective of this systematic review is to assess the effectiveness, immunogenicity, and safety of COVID-19 vaccines for individuals with HM.
Methods
The protocol for this review was registered with PROSPERO (CRD42021281412) and is provided at Open Science Framework under https://osf.io/2nbev/.
Literature search
On December 10, 2021, the Web of Science Core collection, the WHO COVID-19 Global literature on Coronavirus disease, and Cochrane COVID-19 Study Register (CCSR)were searched. The search strategies can be found in the supplement. In addition, reference lists of included publications were hand searched.
Study selection criteria
We included randomized controlled trials and prospective cohort studies, examining adult participants with a diagnosis of a HM who completed vaccination schedules with one or more of the COVID-19 vaccines that have been authorized for use in the European Union or approved, authorized, licensed or granted an emergency use authorization in at least ten countries worldwide; as of September 1, 2021; those were:
-
mRNA-based vaccines: BNT162 (Comirnaty®) from Pfizer/BiontechmRNA-1273 (Spikevax®) from Moderna;
-
Vector-based vaccines: AZD1222 (Vaxzevria®) from Astrazeneca, JNJ-78436735 (COVID-19 Vaccine Janssen®) from Janssen Pharmaceuticals, rAd26 (Sputnik Light®) from Gamaleya, rAd5 (Sputnik V®, Gam-COVID-Vac®) from Gamaleya;
-
Inactivated vaccines: BBIBP-CorV (Covilo®) from Sinopharm, CoronaVac (Sinovac®) from Sinovac Biotech [22].
Complete vaccination (=full primary immunization) schedules were defined as per marketing authorization at the time of study conduct and included two doses for full primary immunization (except COVID-19 Vaccine Janssen®). An additional dose at ≥3 months after completion of full primary immunization was considered as a booster dose. An additional dose <3 months after completion of full primary immunization was considered as optimization of the full primary immunization schedule.
We did not exclude studies based on publication format, as long as sufficient information was available, and the abstract could be retrieved in English. Study selection was performed in duplicate using a web-based online platform (Rayyan; www.rayyan.ai) by VP, CH, AB, CI, and/or NK. Disagreements were resolved by discussion or by consulting a third author [23].
Data extraction and synthesis of the evidence
Data were extracted by one reviewer and verified by another (VP, CH, CI, AB, NK, SM, and/or PJB). Predefined outcomes were clinical parameters (COVID-19 related mortality, COVID-19-related admission to intensive care unit (ICU), COVID-19 related hospitalization, symptomatic COVID-19, SARS-CoV-2 infection, time to infection, and transmissibility); immunity parameters describing the seroconversion and binding immunoglobulin G titers, seroconversion described by neutralization assays, and T-cell parameters; and adverse events, serious adverse events, and events of special interest (i.e., allergic reactions, thrombotic events, heart muscle inflammation, the progress of underlying malignancy).
We collected outcome data (event frequencies and sample size) for the overall cohort and relevant subgroups and recalculated confidence intervals where necessary. Data on healthy controls of the same studies were extracted, but not directly compared to the HM cohorts, as most of these controls were not well-matched in age and clinical condition. Due to the large clinical, geographical, and temporal heterogeneity of studies, outcome rates were not pooled but depicted in form of forest plots without a combined effect estimate using R (version 4.1.2) as well as presented in a table format, both according to overall identified studies and subgroups (type of disease, type of therapy, age, the biological sex of participants).
Risk of bias assessment and GRADEing of the evidence
For risk of bias assessments, we used a tool that is currently being developed for overall prognosis studies (RoB-OPS; https://osf.io/dfk2r) and which is based on previous items in prognosis and risk of bias research but tailored to studies without a control arm. Based on the four domains of participants, outcomes, analysis, and reporting bias, an overall judgement of each outcome set was made per study. The complete list of items and the rating options in their current form can be found in the supplement.
For prioritized outcomes, we used the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach to assess the certainty in the evidence, starting at a high level of evidence according to guidelines for overall prognosis studies [24, 25].
Results
Results of the search
The search flow is summarized in Fig. 1. We initially identified 2575 potentially relevant records. After removing 326 duplicates and 1970 records through title and abstract screening, 279 full-text manuscripts were evaluated for eligibility. Further, 128 records were excluded for specific reasons (see Supplementary Table 1). Finally, 156 studies (151 records) that met the inclusion criteria were included. Of those, 58 studies were still ongoing or completed, but without published data (see Supplementary Table 2). After all, 57 studies were included in our outcome synthesis.
Description of studies
Of the 57 identified studies, all were conducted between December 2020 and October 2021. Most studies were conducted in Europe (29 of 57 studies), followed by 14 studies from the US, and 12 from Israel. We did not identify any information on study location for the two studies. The majority of studies received funding from academic organizations, charities or foundations, or governmental institutions (29 of 57 studies). Eight studies received no dedicated funding, one study was funded by the pharmaceutical industry and the remaining did not disclose funding sources.
Ten studies included only individuals with plasma cell neoplasms (primarily multiple myeloma, MM), four only individuals with chronic lymphocytic leukemia (CLL), and one only individual with Waldenström macroglobulinemia. The remaining studies included participants with different malignancies or did not specify the underlying type of HM. In total, 39 studies had a control group, with 15 of those consisting of healthy volunteers, 12 healthy health care workers (HCW), 3 age-matched or -compatible cohorts, and 2 age- and sex-matched HCW. In two studies the control group consisted of a solid tumour cohort and a non-vaccinated COVID-19-positive MM patient cohort, respectively.
Overall, we identified studies on five different vaccines, which were examined in various combinations: Comirnaty®, Spikevax®, Vaxzevria®, COVID-19 Vaccine Janssen®, and BBIBP-CorV, with Comirnaty® used as a single vaccine in 31/57 studies. Most studies evaluated the effectiveness of a defined full primary immunization schedule (i.e., one dose for COVID-19 Vaccine Janssen®, and two doses for all other vaccines). Two studies evaluating the effect of a third vaccine dose were identified. None of the studies had a prospectively planned interventional comparison. However, five studies enrolled participants receiving different vaccines and provided subgroup outcome data.
All of the included studies reported on at least one immunity parameter of interest. Clinical outcomes evaluating the effectiveness of the vaccines were reported in 22 of 57 studies, and safety outcomes, including data on reactogenicity, were reported in 20 of the studies. Supplementary Table 3 summarizes details regarding the study and participant characteristics.
Risk of bias
Effectiveness outcomes
From the 22 studies reporting clinical outcomes, one study was separately rated for three different clinical outcomes. Among these 24 judgments, the overall risk of bias was rated to be low in three studies, to be moderate in ten studies and to be high in 11 studies. For nine studies no information was available to assess selective reporting bias. The separate judgements for each domain are illustrated in Supplementary Fig. 1, and supporting judgements are available from the authors upon request.
Immunogenicity outcomes
From the 57 studies reporting immunogenicity outcomes, three studies were separately rated for two different immunogenicity outcomes. Among these 60 judgements, the overall risk of bias was rated to be low in ten studies, to be moderate in 36 studies and to be high in 14 studies. For nine studies no information was available to assess selective reporting bias. The separate judgements for each domain are illustrated in Supplementary Fig. 2.
Safety outcomes
From the 20 studies reporting safety outcomes, one study was separately rated for two different safety outcomes. Among these 21 judgements, the overall risk of bias was rated to be low in none of the studies, to be moderate in nine studies and to be high in 12 studies. For seven studies no information was available to assess selective reporting bias. The separate judgements for each domain are illustrated in supplementary fig. 3.
Effectiveness, immunogenicity, and safety of vaccination
A summary of findings with the GRADE-certainty assessments, for outcomes prioritized as most patient-relevant at the protocol stage, is available in Table 1. Further, an overview of all reported outcomes, including the ranges of reported effect rates, and the number of participants and studies is available in Supplementary Table 6.
SARS-CoV-2 infection and severity
We identified 19 studies (3277 participants with HM) reporting on SARS-CoV-2 infections following full primary immunization. The event rate ranged across studies from 0 to 11.9% (⊕⊖⊖⊖ very-low certainty of the evidence) (see Fig. 2A). The time of follow-up (FU) was not reported in six studies [26,27,28,29,30,31], and ranged from 11 days to 6 months after the second vaccination in the remaining studies. One study (72 participants with HM) reported the time to occurrence of SARS-CoV-2 infections after full primary immunization. The study reported two cases that occurred after a median 19.5 days (range 16–23) following the second vaccination. It was not reported whether both individuals achieved an immune response after vaccination.
We identified 13 studies (1484 participants with HM) reporting on symptomatic COVID-19. The event rate ranged across studies from 0 to 2.7% (⊕⊖⊖⊖ very-low certainty of the evidence) (see Fig. 2B). FU time was not reported in six studies [26,27,28,29,30,31] and ranged from 19 days to 6 months after the second vaccination in the remaining studies.
Six studies (382 participants with HM) reporting on COVID-19 related hospitalization (Mona 2021) were identified. The event rate ranged studies from 0 to 2.8% across studies (⊕⊖⊖⊖ very-low certainty of the evidence) (see Fig. 2C). FU time was not reported in three studies [28, 32, 33] one had a follow-up of 2 months, and two studies of 3 months [34, 35] after the second vaccination. One study (72 participants with HM) reported on COVID-19 related admission to ICU. After a follow-up of 3 months after the second vaccination, no cases were observed [35].
In total, we identified six studies (1228 participants with HM) reporting on COVID-19-related mortality in vaccinated individuals. The event rate ranged across studies from 0 to 0.5% (⊕⊖⊖⊖ very-low certainty of the evidence) (see Fig. 2D). We did not identify any studies reporting on transmissibility (e.g., secondary attack rates) or quality of life after SARS-CoV-2 vaccination.
Immunogenicity
Humoral response
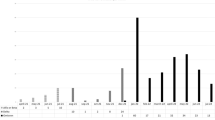
Forty-eight studies reported on antibody response after full primary vaccination. Of those, 18 compared their results to a healthy control group and described significant between-group differences in antibody response. Positive humoral immune response was defined in the primary studies according to cutoffs defined for the respective assays used (see Supplementary Table 6). Across studies (including 7393 individuals), response rates ranged from 38.1 to 99.1% after the first measurement at least 14 days after the second vaccine (⊕⊕⊖⊖ low certainty of the evidence) (see Fig. 2E). We stratified the results along underlying disease and treatment received (see Table 2). Detailed results with the number of patients and events are depicted in the corresponding forest plots Supplementary Figs. 4 and 5, respectively. The highest response rate was seen for patients with myeloproliferative diseases and the lowest in patients with CLL. Patients with lymphoma showed very diverse responses irrespective of whether indolent or aggressive lymphoma was reported. Regarding treatment, patients with B-cell depleting or -directed treatment had lower seroconversion rates as compared to those receiving chemotherapy or other targeted treatments. Patients who underwent either allogeneic or autologous stem cell transplantation (SCT) showed higher seroconversion rates than those after CAR T-cell therapy. Available data differed in quantity and detail with regard to different underlying diseases (Fig. 3A). Most data were available for patients with indolent lymphoma, especially MM, and CLL, while data for patients with acute leukaemia and myeloproliferative diseases are sparse. Due to different assays applied in the various studies including heterogeneity in target measurement throughout the studies, the direct comparison of IgG titers was unfeasible and is not reported.
We identified five studies reporting on FU after the second vaccine dose. During the initial measurement, 573 participants with HM were evaluated while at the extended FU measurement 373 participants were evaluated. Response rate at the initial measurement ranged from 58 to 82% and after the extended FU from 45 to 76%, with four studies suggesting a waning IgG antibody response over time (Supplementary Fig. 6). Measurements were performed ~2–3.5 months apart.
Two studies reported IgG response after a third (i.e., “booster”) vaccine dose for a total of 78 participants with HM. The response rate ranged from 31 to 65%. For one study, IgG measurements after the second dose were also available, however for a larger cohort. In comparison, the response rate for the full cohort was 75% after completing full primary immunization and 65% for the patients receiving a booster dose (Supplementary Fig. 7) [36].
Five studies (429 participants with HM) compared IgG antibody responses for different vaccine types. Four studies compared BNT162b2 with mRNA-123 [30, 37,38,39] and one study BNT162b2 with ChAdox-nCoV-19 [40]. Confidence intervals were widely overlapping for all but one study that compared BNT162b2 with mRNA-123 (27% (95% CI 15–40) vs. 62% (95% CI 49–76)). Further, the one study comparing BNT162b2 with ChAdox-nCoV-19 suggests no difference in response (supplementary fig. 8).
Eighteen studies provided data on healthy controls. As described above, no direct comparisons to the HM cohorts were made, as most of these controls were not well-matched in age and clinical condition. Seroconversion in healthy controls ranged from 96 to 100% (supplementary fig. 9).
Of all studies searched, 14 reported the development of neutralizing antibodies against SARS-CoV-2 (1174 participants with HM). Response rate ranged across studies from 21.8 to 96.2% after the first measurement at least 14 days after the second vaccine (see supplementary table 7).
Cellular response
There were 11 studies reporting vaccine-induced T-cell responses in patients with HM. To evaluate such response, different assays were used across the studies and T-cell immunity was analyzed by intracellular cytokine staining and flow cytometry, measurement of secreted interferon-gamma (IFN-γ) by the ELISpot technique, or a whole-blood platform, and by measurement of secreted IFN-γ/Interleukin (IL)-2 by the FluoroSpot technique. T-cell response rates ranged from 26.5 to 85.9% in all studies (⊕⊕⊖⊖ low certainty of the evidence) (see Fig. 2F). Two studies providing data for HSCT patients only, reported the lowest response rates of 27% and 29%, respectively [41, 42]. Five studies did not further specify subgroups of hematological patients, three studies reported on multiple myeloma patients only [43,44,45], and the remaining study included various types of lymphoma [46]. The timepoint of T-cell measurement ranged between 14 days and 6 weeks after full primary immunization (two vaccines). Four studies further specified their results on the type of treatment with very small sample sizes in consequence. Yet, patients with anti-CD20 therapy within 6 months from vaccination were shown to have robust T-cell responses in 2/2 studies (100% response [n = 4] [47] and 75% [n = 33] [48]). In contrast, treatment with corticosteroids was associated with poor T-cell response [46].
A majority of studies (6/11) reported discordant immune responses with positive T-cell responses in patients lacking serological responses ranging from 19.7 to 74%. Aleman and colleagues performed in-depth analyses of such discordant responses and reported those T cells to be monofunctional and lower in their extent compared to T-cell responses in seropositive patients [43].
Safety
We identified six studies (853 participants with HM) reporting on adverse events (AEs). Across studies 0–50.9% of participants experienced at least one event (⊕⊕⊖⊖ low certainty of the evidence) (see Fig. 2G). Three studies did not report the observation period [28, 49, 50]. In addition, 17 studies reported local and/or systemic reactions or AEs of special interest for their study; an overview of reported events can be found in Supplementary Table 8. We identified three studies (208 participants with HM) reporting on vaccine-induced immune thrombotic thrombocytopenia (VITT). Across studies, 0–2.5% of participants experienced at least one event. One study did not report the observation period [37], one study observed participants for 49 days from the first dose[27], and one study for 2 weeks after the second dose [31]. Three studies (761 participants with HM) reported anaphylactic or systemic allergic reactions, 0–1.3% of participants experienced at least one event. Two studies (226 participants with HM) reporting the progress of the underlying HM were identified and 2.5–5.5% of participants reported experiencing progression of their underlying disease. Participants were followed for up to 1 month after the second vaccine dose; however, we did not identify any information on whether the disease progression was likely related or unrelated to the vaccination. We did not identify any studies reporting any events of myocarditis or termination of anti-cancer treatment due to vaccination.
Four studies (901 participants with HM) reported serious adverse events (SAEs). Across studies, 0–7.5% of participants experienced at least one event (⊕⊕⊖⊖ low certainty of the evidence) (see Fig. 2G). SAEs were assessed for at least 7 and up to 49 days following vaccination.
Discussion
We here report the results of a systematic review assessing the effectiveness, immunogenicity, and safety of COVID-19 vaccines in patients with HM. Clinical outcomes assessing vaccine effectiveness were generally only occasionally and not systematically reported and further limited by short observational periods. Thus, a firm appraisal of the protective effect of COVID-19 vaccines on these highly patient-relevant outcomes is to date not possible. With regard to immunogenicity, we found heterogeneous vaccine-induced seroconversion rates and cellular immunity in HM patients, which was lower than reported for healthy participants in all studies. The highest humoral response rates were reported for myeloproliferative diseases and the lowest in CLL. Poor immunogenicity by COVID-19 vaccines in patients with an impaired B-cell axis is in line with other vaccines showing reduced efficacy in this population [51,52,53,54,55].
The detrimental effect of B-cell depleting treatment, especially when administered within 12 months from vaccine application, is concerning beyond the population of HM patients studied herein since these drugs are widely used beyond HM [56, 57]. Interestingly, initiating B-cell depleting treatment shortly after vaccination does not seem to relevantly impair humoral vaccine response [58]. The relatively low humoral response to vaccination in patients undergoing CAR-T-cell treatment compared to HSCT recipients could be attributable to the lymphodepleting chemotherapy and B-cell targeting constructs. Additionally, a historic effect, with HSCT recipients potentially recovered from treatment effects, appears plausible [59]. Due to different assays used and lacking international standards, a pooled outcome analysis of antibody titres was infeasible. However, it is generally questionable whether the serologic response can serve as reliable CoP in a population with an impaired B-cell axis.
In contrast to the serologic response to COVID-19 vaccines, insights into cellular vaccine response are still scarce. In the light of impaired serologic response in HM, SARS-CoV-2 specific T cells may be crucial in this population. Of 57 studies included, only 11 reported vaccine-induced T-cell response. Except for patients after allogeneic HSCT, robust T-cell responses were reported in HM patients across the studies included. Especially those receiving anti-CD20 treatment responded well on the T-cell level highlighting the protective capacities of vaccination also in patients with treatment-associated B cells [60]. Studies reporting on discordant immune responses show that at least 20% of patients show a T-cell response in the absence of seroconversion. These results are reassuring for those patients failing serologic response but question the role of antibodies as the sole correlate of protection. Caution is warranted; however, since most studies used different assays, different thresholds and usually lacked control groups. Further, the kinetics of T cells after COVID-19 vaccination in the immunocompromised remain sparsely investigated, and therefore, the ideal timepoint for T-cell measurement is yet to be determined.
With regard to safety, AE assessment and reporting were not performed systematically in most studies. However, reported events herein are largely consistent with the safety profile observed in clinical trials and real-world evidence of the general population [61,62,63]. AEs of special interest as identified and prioritized in the conducted patient workshop were rarely or never reported.
Given the rapid changes in the epidemiological situation and turnover of research output in the SARS-CoV-2 / COVID-19 field, it is nearly impossible to stay up to date with a methodologically sound and systematic approach. The problem of waning immunity was identified only in the last months and optimization schedules are widely investigated and partially already applied through an additional booster dose. A recent systematic review with meta-regression provides evidence of a decrease in vaccine effectiveness after full primary immunization against pre-omicron SARS-CoV-2 variant infection by 21% (95% CI 13.9–29.8) in the general population [64]. By the time of our search, we only identified a small number of studies investigating a third vaccine dose in HM patients. Interestingly, a more recent study reported successfully seroconversion after a third mRNA vaccine dose in 59% of 75 patients that had received cellular therapies or bispecific antibodies and failed the primary two-dose vaccine scheme [65]. This and other emerging studies highlight the potential of booster vaccinations and several international committees on immunization already recommend a fourth vaccine dose for immunologically vulnerable patient groups [66, 67].
None of the identified studies investigated vaccine effectiveness against the omicron VOC (BA.1, BA.2). First studies investigating neutralizing effectiveness against omicron in cancer patients suggest a higher immune evasive capacity; in individuals with HM also after receiving the third dose [68]. Even though the evidence synthesized here does not assess evidence on variant-specific vaccine effectiveness or effectiveness of (repeated) boosters, it provides a thorough summary of the capacity to develop a humoral and/or cellular response following vaccination for individuals with different HM stratified by disease entity and treatments received. Taken together, we identified growing evidence for humoral COVID-19 vaccine-induced humoral response, but scarce data for a cellular response, and even less evidence for clinical vaccine effectiveness and safety in HM patients. To date, patients with MM or CLL and those receiving B-cell depleting therapies are the best-described patient groups with regard to humoral response. In contrast, data for patients with other diseases such as acute leukemias or aggressive lymphoma are still largely lacking. As highlighted by the evidence-gap maps (Fig. 3) a large evidence gap remains for most HM patients and underlying treatment and/or disease status, while data on the cellular immune response is particularly scarce.
Overall, our systematic review highlights the generally poor immune response of people with HM to COVID-19. In light of easing or ending strategies aimed to reduce virus transmission for the general population, the flux in prevalent SARS-CoV-2 variants and entailing high incidence rates pose major risks to this vulnerable group. For high-risk individuals who respond poorly to current COVID-19 vaccination regimens, new approaches to prevent infections and severe or prolonged disease courses are urgently needed.
Further research should therefore evaluate improved booster immunization strategies including heterologous vaccinations for immunocompromised individuals, such as the herein reported group of HM patients. By defining standards for reporting vaccine efficacy on the humoral and cellular level and enforcing the adequate reporting of clinical outcomes, international boards of experts could guide future research to enhance cross-study comparability and maximize the evidence and benefit generated.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard: World Health Organisation. 2020b. https://covid19.who.int/. Accessed 14 March 2022.
Bertuzzi AF, Ciccarelli M, Marrari A, Gennaro N, Dipasquale A, Giordano L, et al. Impact of active cancer on COVID-19 survival: a matched-analysis on 557 consecutive patients at an Academic Hospital in Lombardy, Italy. Br J Cancer. 2021;125:358–65.
ElGohary GM, Hashmi S, Styczynski J, Kharfan-Dabaja MA, Alblooshi RM, de la Cámara R, et al. The risk and prognosis of COVID-19 infection in cancer patients: a systematic review and meta-analysis. Hematol Oncol Stem Cell Ther. 2020.
Piñana JL, Martino R, García-García I, Parody R, Morales MD, Benzo G, et al. Risk factors and outcome of COVID-19 in patients with hematological malignancies. Exp Hematol Oncol. 2020;9:21.
Pagano L, Salmanton-García J, Marchesi F, Busca A, Corradini P, Hoenigl M, et al. COVID-19 infection in adult patients with hematological malignancies: a European Hematology Association Survey (EPICOVIDEHA). J Hematol Oncol [Internet]. 2021. http://europepmc.org/abstract/MED/34649563.
Ontario Agency for Health Protection and Promotion. COVID-19 real-world vaccine effectiveness—what we know so far. Toronto: Queen’s Printer for Ontario; 2021.
Agha ME, Blake M, Chilleo C, Wells A, Haidar G. Suboptimal response to Coronavirus disease 2019 messenger RNA vaccines in patients with hematologic malignancies: a need for vigilance in the postmasking era. Open Forum Infect Dis. 2021;8:ofab353. https://doi.org/10.1093/ofid/ofab353.
Terpos E, Gavriatopoulou M, Ntanasis-Stathopoulos I, Briasoulis A, Gumeni S, Malandrakis P, et al. The neutralizing antibody response post COVID-19 vaccination in patients with myeloma is highly dependent on the type of anti-myeloma treatment. Blood Cancer J. 2021;11:138-.
Lopez Bernal J, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, et al. Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant. N Engl J Med. 2021;385:585–94.
Planas D, Veyer D, Baidaliuk A, Staropoli I, Guivel-Benhassine F, Rajah MM, et al. Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization. Nature. 2021;596:276–80.
Passalacqua R, Ratti M, Pan A, Testa S, Molteni A, Tonoli S, et al. Efficacy of SARS-CoV-2 vaccination in cancer patients during treatment: A prospective observational study (ANTICOV trial). Ann Oncol. 2021;32:S1161–S.
Koch TA-O, Mellinghoff SC, Shamsrizi PA-O, Addo MA-O, Dahlke CA-O. Correlates of vaccine-induced protection against SARS-CoV-2. LID. https://doi.org/10.3390/vaccines9030238.
Ravandi F, O’Brien S. Immune defects in patients with chronic lymphocytic leukemia. Cancer Immunol Immunother. 2006;55:197–209.
Bitterman R, Eliakim-Raz N, Vinograd I, Zalmanovici Trestioreanu A, Leibovici L, Paul M. Influenza vaccines in immunosuppressed adults with cancer. Cochr Database Syst Rev. 2018;2:CD008983.
Bedognetti D, Ansaldi F, Zanardi E, Durando P, Sertoli MR, Massucco C, et al. Seasonal and pandemic (A/H1N1 2009) MF-59–adjuvanted influenza vaccines in complete remission non-Hodgkin lymphoma patients previously treated with rituximab containing regimens. Blood. 2012;120:1954–7.
Rubinstein SM, Bhutani D, Lynch RC, Hsu C-Y, Shyr Y, Advani S, et al. Patients recently treated for B-lymphoid malignancies show increased risk of severe COVID-19. Blood Cancer Discov. 2022;3:181–93.
Addeo A, Shah PK, Bordry N, Hudson RD, Albracht B, Di Marco M, et al. Immunogenicity of SARS-CoV-2 messenger RNA vaccines in patients with cancer. Cancer Cell. 2021;39:1091–8.
Greenberger LM, Saltzman LA, Senefeld JW, Johnson PW, DeGennaro LJ, Nichols GL. Antibody response to SARS-CoV-2 vaccines in patients with hematologic malignancies. Cancer Cell. 2021;39:1031–3.
Malard FA-O, Gaugler B, Gozlan J, Bouquet L, Fofana D, Siblany L, et al. Weak immunogenicity of SARS-CoV-2 vaccine in patients with hematologic malignancies. Blood Cancer J. 2021;11:142.
Maneikis K, Šablauskas K, Ringeleviičiūtė U, Vaitekėnaitė V, Čekauskienė R, Kryžauskaitė L, et al. Immunogenicity of the BNT162b2 COVID-19 mRNA vaccine and early clinical outcomes in patients with haematological malignancies in Lithuania: a national prospective cohort study. Lancet Haematol. 2021;8:e583–92.
Monin L, Laing AG, Muñoz-Ruiz M, McKenzie DR, Del Molino Del Barrio I, Alaguthurai T. et al. Safety and immunogenicity of one versus two doses of the COVID-19 vaccine BNT162b2 for patients with cancer: interim analysis of a prospective observational study. Lancet Oncol. 2021;22:765–78.
McGill COVID19 Vaccine Tracker Team. COVID-19 vaccine tracker. 2021. https://covid19.trackvaccines.org/vaccines/.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
Guyatt G, Oxman Ad Fau, Akl EA, Akl Ea Fau, Kunz R, Kunz R, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–94.
Iorio A, Spencer FA, Falavigna M, Alba C, Lang E, Burnand B, et al. Use of GRADE for assessment of evidence about prognosis: rating confidence in estimates of event rates in broad categories of patients. BMJ. 2015;350:h870.
Peter B, Ola B, Lotta H, Stephan M, Piotr N, Puran C, et al. Safety and efficacy of the mRNA BNT162b2 vaccine against SARS-CoV-2 in five groups of immunocompromised patients and healthy controls in a prospective open-label clinical trial. EBioMedicine. 2021;74:103705.
Canti L, Humblet-Baron S, Desombere I, Neumann J, Pannus P, Heyndrickx L, et al. Predictors of neutralizing antibody response to BNT162b2 vaccination in allogeneic hematopoietic stem cell transplant recipients. J Hematol Oncol. 2021;14:174.
Figueiredo J, Merin NM, Hamid O, Choi SY, Lemos T, Cozen W, et al. Longitudinal SARS-CoV-2 mRNA vaccine-induced humoral immune responses in cancer patients. Cancer Res. 2021;81:6273–80.
Sherman AC, Desjardins M, Cheng CA, Bausk B, Izaguirre N, Zhou G, et al. SARS-CoV-2 mRNA vaccines in allogeneic hematopoietic stem cell transplant recipients: immunogenicity and reactogenicity. Clin Infect Dis. 2021;30:ciab930.
Stampfer SD, Goldwater MS, Jew S, Bujarski S, Regidor B, Daniely D, et al. Response to mRNA vaccination for COVID-19 among patients with multiple myeloma. Leukemia. 2021;35:3534–41.
Yeshurun M, Pasvolsky O, Shargian L, Yahav D, Ben-Zvi H, Rubinstein M, et al. Humoral serologic response to the BNT162b2 vaccine after allogeneic haematopoietic cell transplantation. Clin Microbiol Infect. 2022;28:303.e1–303.e4.
Gavriatopoulou M, Ntanasis-Stathopoulos I, Korompoki E, Terpos E, Dimopoulos MA. SARS-CoV-2 vaccines in patients with multiple myeloma. Hemasphere. 2021;5:e547.
Salvini M, Maggi F, Damonte C, Mortara L, Bruno A, Mora B, et al. Immunogenicity of anti-SARS-CoV-2 Comirnaty vaccine in patients with lymphomas and myeloma who underwent autologous stem cell transplantation. Bone Marrow Transplant. 2022;57:137–9.
Peeters M, Verbruggen L, Teuwen L, Vanhoutte G, Vande Kerckhove S, Peeters B, et al. Reduced humoral immune response after BNT162b2 coronavirus disease 2019 messenger RNA vaccination in cancer patients under antineoplastic treatment. ESMO Open. 2021;6:100274.
Soledad H, Jeremie Z, Timothee B, Amani O, Delphine P, Paul D, et al. Anti-CD38 therapy impairs SARS-CoV-2 vaccine response in multiple myeloma patients. Blood. 2022;139:942–6.
Greenberger LM, Saltzman LA, Senefeld JW, Johnson PW, DeGennaro LJ, Nichols GL. Anti-spike antibody response to SARS-CoV-2 booster vaccination in patients with B cell-derived hematologic malignancies. Cancer Cell. 2021;39:1297–9.
Cattaneo D, Bucelli C, Cavallaro F, Consonni D, Iurlo A. Impact of diagnosis and treatment on response to COVID-19 vaccine in patients with BCR-ABL1-negative myeloproliferative neoplasms. A single-center experience. Blood Cancer J. 2021;11:185
Mairhofer M, Kausche L, Kaltenbrunner S, Ghanem R, Stegemann M, Klein K. et al. Humoral and cellular immune responses in SARS-CoV-2 mRNA-vaccinated patients with cancer. Cancer Cell. 2021;39:1171–2.
Tamari R, Politikos I, Knorr DA, Vardhana SA, Young JC, Marcello LT, et al. Predictors of humoral response to SARS-CoV-2 vaccination after hematopoietic cell transplantation and CAR T-cell therapy. Blood Cancer Discov. 2021;2:577–85.
Chan WY, Howells L, Wilson W, Sanchez E, Ainley L, Chavda SJ, et al. Serological response to the BNT162b2 mRNA or ChAdOx1 nCoV-19 COVID-19 vaccine after first and second doses in patients with plasma cell disorders: influence of host and disease factors. Br J Haematol. 2022;196:e21–6.
Ram R, Hagin D, Kikozashvilli N, Freund T, Amit O, Bar-On Y, et al. Safety and immunogenicity of the BNT162b2 mRNA COVID-19 vaccine in patients after allogeneic HCT or CD19-based CART therapy—a single-center prospective cohort study. Transpl Cell Ther. 2021;27:788–94.
Lindemann M, Klisanin V, Thümmler L, Fisenkci N, Tsachakis-Mück N, Ditschkowski M, et al. Humoral and Cellular Vaccination Responses against SARS-CoV-2 in Hematopoietic Stem Cell Transplant Recipients. Vaccines. 2021;9:1075.
Aleman A, Upadhyaya B, Tuballes K, Kappes K, Gleason CR, Beach K, et al. Variable cellular responses to SARS-CoV-2 in fully vaccinated patients with multiple myeloma. Cancer Cell. 2021;39:1442–4.
McKenzie DR, Muñoz-Ruiz M, Monin L, Alaguthurai T, Lechmere T, Abdul-Jawad S, et al. Humoral and cellular immunity to delayed second dose of SARS-CoV-2 BNT162b2 mRNA vaccination in patients with cancer. Cancer Cell. 2021;39:1445–7.
Karthik R, Ross S, Sally J, Paul W, Sherin V, Alison T, et al. Immune response to COVID-19 vaccination is attenuated by poor disease control and antimyeloma therapy with vaccine driven divergent T cell response. Br J Haematol. 2022;197:293–301.
Ehmsen S, Asmussen A, Jeppesen SS, Nilsson AC, Østerlev S, Vestergaard H, et al. Antibody and T cell immune responses following mRNA COVID-19 vaccination in patients with cancer. Cancer Cell. 2021;39:1034–6.
Fendler A, Shepherd STC, Au L, Wilkinson KA, Wu M, Byrne F, et al. Adaptive immunity and neutralizing antibodies against SARS-CoV-2 variants of concern following vaccination in patients with cancer: the CAPTURE study. Nat Cancer. 2021;2:1305–20.
Marasco V, Carniti C, Guidetti A, Farina L, Magni M, Miceli R, et al. T-cell immune response after mRNA SARS-CoV-2 vaccines is frequently detected also in the absence of seroconversion in patients with lymphoid malignancies. Br J Haematol. 2022;196:548–58.
Cattaneo C, Cancelli V, Pagani C, Ogna A, Tucci A, Rossi G, et al. Impaired humoral response in lymphoma patients surviving the acute phase of COVID-19. Hematol Oncol. 2021;39(Suppl 2).
Piñana JL, López-Corral L, Martino R, Montoro J, Vazquez L, Pérez A, et al. Infectious Complications Subcommittee of the Spanish Hematopoietic Stem Cell Transplantation and Cell Therapy Group (GETH-TC). SARS-CoV-2-reactive antibody detection after SARS-CoV-2 vaccination in hematopoietic stem cell transplant recipients: Prospective survey from the Spanish Hematopoietic Stem Cell Transplantation and Cell Therapy Group. Am J Hematol. 2022;97:30–42.
Hartkamp A, Mulder AH, Rijkers GT, van Velzen-Blad H, Biesma DH. Antibody responses to pneumococcal and haemophilus vaccinations in patients with B-cell chronic lymphocytic leukaemia. Vaccine. 2001;19:1671–7.
Whitaker JA, Parikh SA, Shanafelt TD, Kay NE, Kennedy RB, Grill DE, et al. The humoral immune response to high-dose influenza vaccine in persons with monoclonal B-cell lymphocytosis (MBL) and chronic lymphocytic leukemia (CLL). Vaccine. 2021;39:1122–30.
Mauro FR, Giannarelli D, Galluzzo CM, Vitale C, Visentin A, Riemma C, et al. Response to the conjugate pneumococcal vaccine (PCV13) in patients with chronic lymphocytic leukemia (CLL). Leukemia. 2021;35:737–46.
Svensson T, Kättström M, Hammarlund Y, Roth D, Andersson PO, Svensson M, et al. Pneumococcal conjugate vaccine triggers a better immune response than pneumococcal polysaccharide vaccine in patients with chronic lymphocytic leukemia A randomized study by the Swedish CLL group. Vaccine. 2018;36:3701–7.
Pasiarski M, Rolinski J, Grywalska E, Stelmach-Goldys A, Korona-Glowniak I, Gozdz S, et al. Antibody and plasmablast response to 13-valent pneumococcal conjugate vaccine in chronic lymphocytic leukemia patients–preliminary report. PLoS ONE. 2014;9:e114966.
Bange EM, Han NA, Wileyto P, Kim JY, Gouma S, Robinson J, et al. CD8 + T cells contribute to survival in patients with COVID-19 and hematologic cancer. Nat Med. 2021;27:1280–9.
Apostolidis SA, Kakara M, Painter MM, Goel RR, Mathew D, Lenzi K, et al. Cellular and humoral immune responses following SARS-CoV-2 mRNA vaccination in patients with multiple sclerosis on anti-CD20 therapy. Nat Med. 2021;27:1990–2001.
Shree TA-O, Shankar V, Lohmeyer JA-O, Czerwinski DK, Schroers-Martin JA-O, Rodriguez GM, et al. CD20-targeted therapy ablates de novo antibody response to vaccination but spares preestablished immunity. Blood Cancer Discov. 2022;3:95–102.
Logue JM, Zucchetti E, Bachmeier CA, Krivenko GS, Larson V, Ninh D, et al. Immune reconstitution and associated infections following axicabtagene ciloleucel in relapsed or refractory large B-cell lymphoma. Haematologica. 2021;106:978–86.
Apostolidis SA, Kakara M, Painter MM, Goel RR, Mathew D, Lenzi K, et al. Cellular and humoral immune responses following SARS-CoV-2 mRNA vaccination in patients with multiple sclerosis on anti-CD20 therapy. Nat Med. 2021;27:1990–2001.
Thomas SJ, Moreira ED, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine through 6 months. N Engl J Med. 2021;385:1761–73.
Barda N, Dagan N, Ben-Shlomo Y, Kepten E, Waxman J, Ohana R, et al. Safety of the BNT162b2 mRNA Covid-19 vaccine in a nationwide setting. N Engl J Med. 2021;385:1078–90.
Klein NP, Lewis N, Goddard K, Fireman B, Zerbo O, Hanson KE, et al. Surveillance for adverse events after COVID-19 mRNA vaccination. JAMA. 2021;326:1390–9.
Feikin DR, Higdon MM, Abu-Raddad LJ, Andrews N, Araos R, Goldberg Y, et al. Duration of effectiveness of vaccines against SARS-CoV-2 infection and COVID-19 disease: results of a systematic review and meta-regression. Lancet. 2022;399:924–44.
Abid MB, Rubin M, Ledeboer N, Szabo A, Longo W, Mohan M, et al. Efficacy of a third SARS-CoV-2 mRNA vaccine dose among hematopoietic cell transplantation, CAR T cell, and BiTE recipients. Cancer Cell. 2022;40:340–2.
Koch J, Vygen-Bonnet S, Bogdan C, Burchard G, Garbe E, Heininger U, et al. STIKO-Empfehlung zur 2. COVID-19-Auffrischimpfung mit einem mRNAImpfstoff für besonders gesundheitlich gefährdete bzw. exponierte Personengruppen und die dazugehörige wissenschaftliche Begründung. Epid Bull. 2022;7:41–57.
Burki TK. Fourth dose of COVID-19 vaccines in Israel. Lancet Respir Med. 2022;10:e19.
Fendler A, Shepherd STC, Au L, Wu M, Harvey R, Schmitt AM, et al. Omicron neutralising antibodies after third COVID-19 vaccine dose in patients with cancer. Lancet. 2022;399:905–7.
Funding
This systematic review was funded by the Federal Ministry of Education and Research in Germany (Grant no: 01KG2104). PJB is supported by Deutsche Krebshilfe through a Mildred Scheel Nachwuchszentrum Grant (no. 70113307). Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
VP: study selection, data extraction, data synthesis, conception, and writing of the manuscript. SCM: data verification, data synthesis, conception, and writing of the manuscript. AB: study selection and data extraction. CH: study selection and data extraction. CI: study selection, data extraction, and writing of the manuscript. AA: data synthesis. IM: literature search. NK: study selection, data extraction, and writing of the manuscript. JS: review and proofreading of the manuscript. OC: review and proofreading of the manuscript. PJB: clinical supervision, data verification, conception, and writing of the manuscript. NS: methodological supervision, conception, and proofreading of the manuscript.
Corresponding author
Ethics declarations
Competing interests
VP, AB, CH, CI, AA, IM, NK, JS, PJB, and NS declare no financial conflicts of interest with regard to the present study. SCM reports grants from DZIF. OAC reports grants or contracts from Amplyx, Basilea, BMBF, Cidara, DZIF, EU-DG RTD (101037867), F2G, Gilead, Matinas, MedPace, MSD, Mundipharma, Octapharma, Pfizer, Scynexis; Consulting fees from Amplyx, Biocon, Biosys, Cidara, Da Volterra, Gilead, Matinas, MedPace, Menarini, Molecular Partners, MSG-ERC, Noxxon, Octapharma, PSI, Scynexis, Seres; Honoraria for lectures from Abbott, Al-Jazeera Pharmaceuticals, Astellas, Grupo Biotoscana/United Medical/Knight, Hikma, MedScape, MedUpdate, Merck/MSD, Mylan, Pfizer; Payment for expert testimony from Cidara; Participation on a Data Safety Monitoring Board or Advisory Board from Actelion, Allecra, Cidara, Entasis, IQVIA, Jannsen, MedPace, Paratek, PSI, Shionogi; A patent at the German Patent and Trade Mark Office (DE 10 2021 113 007.7); Other interests from DGHO, DGI, ECMM, ISHAM, MSG-ERC, Wiley.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Piechotta, V., Mellinghoff, S.C., Hirsch, C. et al. Effectiveness, immunogenicity, and safety of COVID-19 vaccines for individuals with hematological malignancies: a systematic review. Blood Cancer J. 12, 86 (2022). https://doi.org/10.1038/s41408-022-00684-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41408-022-00684-8
This article is cited by
-
Rezidivierende SARS-CoV-2-Infektionen bei Immundefizienz
Die Innere Medizin (2023)
-
A multinational, phase 2, randomised, adaptive protocol to evaluate immunogenicity and reactogenicity of different COVID-19 vaccines in adults ≥75 already vaccinated against SARS-CoV-2 (EU-COVAT-1-AGED): a trial conducted within the VACCELERATE network
Trials (2022)