Abstract
Ghrelin is a circulating orexigenic hormone that promotes feeding behavior and regulates metabolism in humans and rodents. We previously reported that local infusion of ghrelin into the basolateral amygdala (BLA) blocked memory acquisition for conditioned taste aversion (CTA) by activating growth hormone secretagogue receptor 1a. In this study, we further explored the underlying mechanism and signaling pathways mediating ghrelin modulation of CTA memory in rats. Pharmacological agents targeting distinct signaling pathways were infused into the BLA during conditioning. We showed that preadministration of the PI3K inhibitor LY294002 abolished the repressive effect of ghrelin on CTA memory. Moreover, LY294002 pretreatment prevented ghrelin from inhibiting Arc and zif268 mRNA expression in the BLA triggered by CTA memory retrieval. Preadministration of rapamycin eliminated the repressive effect of ghrelin, while Gsk3 inhibitors failed to mimic ghrelin’s effect. In addition, PLC and PKC inhibitors microinfused in the BLA blocked ghrelin’s repression of CTA acquisition. These results demonstrate that ghrelin signaling in the BLA shapes CTA memory via the PI3K/Akt/mTOR and PLC/PKC pathways. We conducted in vivo multichannel recordings from mouse BLA neurons and found that microinjection of ghrelin (20 µM) suppressed intrinsic excitability. By means of whole-cell recordings from rat brain slices, we showed that bath application of ghrelin (200 nM) had no effect on basal synaptic transmission or synaptic plasticity of BLA pyramidal neurons. Together, this study reveals the mechanism underlying ghrelin-induced interference with CTA memory acquisition in rats, i.e., suppression of intrinsic excitability of BLA principal neurons via the PI3K/Akt/mTOR and PLC/PKC pathways.
Similar content being viewed by others
Introduction
Ghrelin is a 28-amino-acid peptide hormone predominantly secreted by mammalian stomach cells and is critical for feeding, glucose metabolism and energy homeostasis [1]. There are two forms of ghrelin circulating in blood plasma, acylated and nonacylated ghrelin, both of which are capable of crossing the blood–brain barrier. However, only acylated ghrelin is capable of binding to its receptor, GHS-R1a, in the brain [2]. It is assumed that acetylation by ghrelin-O-acyltransferase occurs immediately before ghrelin binds to GHS-R1a in selected brain areas [3, 4]. Interestingly, recent studies reported that, instead of just being a precursor or a metabolic product of acylated ghrelin, nonacylated ghrelin might play roles opposite those of acylated ghrelin in regulating food intake, metabolism and memory [5,6,7]. Nevertheless, the receptor for nonacylated ghrelin, the most stable and abundant form in circulation (up to 60%-90%), has yet to be identified [8, 9].
Studies have highlighted intriguing and contradictory roles that the ghrelin/GHS-R1a system plays in regulating multiple brain functions beyond feeding and energy homeostasis, such as learning and memory [10, 11]. In particular, ghrelin was previously reported to facilitate learning and memory by activating GHS-R1a in the hippocampus [10, 12, 13]. In contrast, other studies stated that ghrelin had no substantial effect on memory processes [14, 15]. In fact, we found in previous studies that ghrelin impaired both hippocampus-dependent spatial memory and amygdala-sensitive emotional memory by activating GHS-R1a [16,17,18]. To date, the reason for these conflicting findings remains unclear, and the molecular and cellular mechanism mediating ghrelin’s effect on memory processes has not been well explored.
Ghrelin-activated GHS-R1a primarily engages excitatory Gα11/q-dependent molecular cascades, leading to hydrolysis of phosphatidylinositol diphosphate (PIP2) by phospholipase C (PLC) and production of inositol-3-phosphate (IP3) and diacylglycerol (DAG) [8]. However, other G proteins, such as Gi/o and G12/13, as well as G protein-independent pathways, can also mediate ghrelin/GHS-R1a activity under different experimental conditions [19, 20]. Indeed, ghrelin-dependent GHS-R1a activation has been reported to participate in a variety of intracellular signaling pathways, including phosphatidylinositol 3 kinase (PI3K), extracellular signal-regulated protein kinases 1 and 2 (Erk1/2), and protein kinase A (PKA) [13, 21,22,23]. In particular, activation of PI3K was suggested to play a key role in hippocampal ghrelin/GHS-R1a signaling [22, 24]. In addition, GHS-R1a was assumed to be able to form heterodimers with various other receptors, such as dopamine receptors, to affect downstream signaling and receptor trafficking, which increases the complexity of its function [25, 26].
We previously reported that a single low dose of ghrelin (12 ng, 0.5 µL/side) locally administered in the rat BLA during CTA training selectively impaired the acquisition of CTA memory but had no effect on the consolidation or retrieval phase in a GHS-R1a-dependent manner. In this study, we proposed manipulating the activity of targeting signaling cascades during conditioning by a pharmacological approach to determine the key downstream molecules involved in ghrelin/GHS-R1a-dependent modulation of CTA memory acquisition. We also investigated the influence of acute administration of ghrelin on neuronal excitability and synaptic activity of BLA pyramidal neurons in both rats and mice to determine whether the effect of ghrelin was general or species-specific. The aim of our study was to uncover the molecular and cellular mechanism underlying ghrelin-induced repression of CTA memory encoding.
Materials and methods
Animals
Adult male Wistar rats (300–350 g body weight, 10-12 weeks old) were purchased from the Experimental Animal Center at Lukang Pharmaceutical Co (Jining, China). Adult male C57BL/6 J mice (10-12 weeks old) for in vivo multichannel recordings were purchased from the Vital River Laboratory Animal Technology Co. (Beijing, China). Both rats and mice were group-housed in an environment with constant humidity (50% ± 10%), temperature (21 ± 2 °C), 12 h:12 h light/dark cycle, and free access to food and water except for experiment required. Animals were acclimated to colony environment for two weeks before the start of any experiments. Specially, rats for behavioral assays were single-housed right after surgery until behavioral experiments were complete, in order to protect cannulation and to measure liquid intake easily during CTA training and test. We handled rats daily starting immediately after surgery for 1 week to reduce stress induced by single housing. Behavioral experiments were carried out during light cycle from 9:00 am to 6:00 pm. The Chancellor’s Animal Research Committee at Qingdao University approved all animal protocols used in this study, in accordance with National Institutes of Health guidelines.
Surgical procedures and microinfusion in LA
Rats were anesthetized with 1.5%–2.0% isoflurane in oxygen and head-fixed on a stereotaxic apparatus (RWD Life Science, Guangdong, China). Stainless steel guide cannulas (22-gauge) were bilaterally implanted in the BLA according to the following coordinates (relative to bregma): − 2.8 mm anteroposterior, ±5.2 mm mediolateral and −7.5 mm dorsoventral, according to Paxinos and Watson (1998). The cannulas were secured to the skull with stainless steel screws and dental cement. A 28-gauge dummy cannula was inserted into each cannula to prevent clogging. Rats were allowed to recover for 7 days before initiating behavioral study. Drugs were then delivered to the BLA through a 28-gauge infusion cannula preconnected via a PE20 tubing (RWD Life Science, Guangdong, China) to a Hamilton microsyringe driven by a microinfusion pump (Stoelting, IL, USA). The infusion cannula was 0.8 mm longer than the guide cannula. Bilateral delivery of drug or vehicle (0.5 µL/side) was done 20 min before conditioning with an infusion rate of 0.1 μL/min. Rats were awake and able to move freely during drug delivery. The infusion cannula was then left in position for an additional 5 min before withdrawal.
All chemicals were purchased from Tocris Bioscience (MN, USA), prepared in stock solution, and freshly diluted to final concentration right before use. Specifically, ghrelin and dopamine D1 receptor (D1R) antagonist SCH23390 was first dissolved in ddH2O and then diluted with normal saline. Other drugs were first dissolved in DMSO and then freshly diluted at least 1000 times before use with normal saline, to ensure less than 0.1% DMSO in the final solution. All drug dosages were chosen based on pilot studies and previous reports [16, 18, 27].
CTA training and memory test
Rats were deprived of water for 24 h and habituated for 4 days to get the daily water supply within 20 min from 2 serological tubes each containing 10 mL of tap water. On the last day of habituation, rats were assigned to groups with balanced total water intake and body weight. On conditioning (training) day, the two tubes were filled with 0.2% saccharin (w/v, the conditioned taste) instead of water, and rats were allowed to consume it for 10 min followed by intraperitoneal injection of the malaise-inducing agent LiCl (0.1 M, 2% of body weight, intraperitoneal) 20 min later. Drug/vehicle was microinfused in the BLA 20 min before conditioning with an inter-drug-interval (IDI) of 15 min. Testing for aversion to saccharin occurred 24 h later. Two tubes (one containing water and the other containing saccharin) were presented for 20 min. The intake of each fluid was measured and the aversion index (AI) was defined as (milliliters of water consumed)/(milliliters of water + milliliters of saccharin consumed) × 100%. The 50% AI is the equal preference level, and the higher the aversion index, the more the rats preferred water to saccharin. That is to say, the higher AI means the better CTA memory.
Histology
The cannula tip location was confirmed by methylene blue staining shortly after behavioral studies were done. The rats were killed by an overdose of isoflurane, and their brains were isolated and fixed with 4% paraformaldehyde for 6 h, then dehydrated with 30% sucrose in 0.1 M phosphate buffer for 48 h. The frozen brain was sectioned into 40 μm coronal slices with a cryostat (Leica, IL, USA). Only the animals with bilateral cannula placement in the BLA were included in further analyses.
In vivo electrophysiology
Mice were anesthetized with urethane (1.2 g/kg, i.p.) and maintained under isoflurane (0.5%-1%). A small craniotomy (about 1 mm in diameter) was performed (Bregma -1.4 mm; lateral 3.2 mm). Hard dura was broken in warm ACSF. A 16-channel electrode (A1x16-5 mm-50-177, NeuroNexus, MI, USA) was inserted perpendicularly until the deepest channel reached 4.8 mm relative to brain surface. Local field potentials (LFPs) were high-pass filtered at 230 Hz and recorded with a Plexon amplifier (TX, USA). Microinjection of 20 µM ghrelin was puffed with a glass pipette electrode (5–10 µm tip) by a microinjection pump at a speed of 0.3 µL/min. The glass pipette was inserted just above the amygdala before advancing the recording electrode. Recording electrode tip was dyed with DiI (Sigma-Aldrich, MO, USA). After recordings, the mice were perfused with 4% PFA and the brains were sectioned to locate the electrode according to the brain atlas.
Ex vivo slice electrophysiology
Rats coronal brain slices containing amygdala were freshly prepared with a VT-1000 vibratome (Leica, IL, USA) in ice-cold cutting solution containing (in mM): 7 MgSO4, 1 CaCl2, 2.5 KCl, 26 NaHCO3, 1 NaH2PO4, 30 glucose, 1.3 sodium L-ascorbate, 1 kynurenic acid, 3 sodium pyruvate, and 119 choline chloride. Slices (350 µm in thickness) were recovered in a submerged chamber containing a recovery solution consisting of (in mM): 85 NaCl, 2.5 KCl, 4 MgCl2, 0.5 CaCl2, 1.25 NaH2PO4, 24 NaHCO3, 25 glucose, and 50 sucrose for at least 1 h at room temperature. Slices were then transferred to a recording chamber and were continuously perfused with 32 °C artificial cerebrospinal fluid (ACSF) at a rate of about 2 mL/min. ACSF contains (in mM): 120 NaCl, 3.5 KCl, 1.3 MgCl2, 2.5 CaCl2, 1.25 NaH2PO4, 26 NaHCO3, 10 D-glucose. All solutions (pH 7.2–7.4, Osmo 290–310) were bubbled with 95% O2 / 5% CO2.
Neurons were visualized through an upright microscope equipped with an infrared differential interference contrast (IR/DIC) technique (Olympus, Shinjuku, Japan). Whole-cell patch clamp recording in LA pyramidal neurons was performed as previously described [16, 28]. Glass electrodes (3–5 MΩ) for whole-cell current-clamp recording were filled with an internal solution containing (in mM): 120 KMeSO4, 10 KCl, 2 MgCl2, 0.2 EGTA, 10 Hepes, 0.3 Na3GTP, 4 Na2ATP, 5 phosphocreatine. A series of depolarizing currents (1 s in duration) were injected in LA pyramidal neurons. The number of action potentials, resting membrane potential (RMP), and action potential threshold were analyzed with the Matlab program (R2018b). Only neurons that had RMP smaller than −55 mV without spontaneous firing were included in data analysis. Electrodes (4–6 MΩ) for whole-cell voltage-clamp recording were filled with an internal solution containing (in mM): 125 CsCl2, 5 NaCl, 2 MgCl2, 0.2 EGTA, 4 Hepes, 0.2 Na3GTP, 2 MgATP, 7 phosphocreatine and 4 QX-314. Postsynaptic currents were detected at a holding potential of −60 mV, with 50 µM AP-5 and 50 µM picrotoxin in ACSF to isolate spontaneous excitatory postsynaptic currents (sEPSCs), or with 3 mM kynuric acid in ACSF for spontaneous inhibitory postsynaptic currents (sIPSCs). Miniature excitatory and inhibitory postsynaptic currents (mEPSCs and mIPSCs) were recorded separately with 1 µM TTX in ACSF. The amplitude and frequency of PSCs were analyzed with the Mini Analysis Program. To induce evoked EPSC (eEPSC), the thalamo-lateral amygdala pathway was stimulated with a bipolar platinum electrode. The distance between the recording and stimulating sites was between 150 and 450 µm. We delivered 100 µs stimuli at 10 s intervals. Peak EPSC was measured as the peak inward current. For PPF studies, the peak amplitude for individual response was measured as the difference between the current level before the stimulus artifact and the peak of the EPSC. Stimulation position and intensity were set to evoke an EPSC of ~50–200 pA.
Data were acquired with a MultiClamp 700B amplifier, digidata 1440 A interface, and pCLAMP 10.0 software (Axon Instruments, CA, USA). Sampling was filtered at 2 kHz and digitized at 10 kHz. The concentration of ghrelin used in slice recording was 200 nM.
Quantitative reverse transcription PCR (RT-qPCR) and Western Blot (WB)
Total RNA was extracted from microdissected basolateral amygdala tissue with the PureLinkTM RNA Mini Kit (Invitrogen, CA, USA). RNA quantity and quality were measured using a NanoDrop 2000 Spectrophotometer (Thermo Fisher Scientific, MA, USA). Complementary DNA was synthesized from 1 µg of total RNA with SuperScriptTM III Reverse Transcriptase (Invitrogen, CA, USA). PCR-based quantification of Arc and Zif268 expression was performed using a MasterCycler® ep realplex PCR system (Eppendorf, Hamburg, Germany) and a QuantiFast SYBR Green PCR Kit (Qiagen, Hilden, Germany). The PCR cycling parameters were as follows: 95 °C for 5 min, 40 cycles of PCR reaction at 95 °C for 5 s, 60 °C for 30 s, and 72 °C for 30 s, respectively. The 2-ΔΔCT method was used first to normalize CT values against the housekeeping gene Actb, and then to quantify relative expression of Arc and Zif268 mRNA in each treatment group. Triplicates were done for each sample. PCR primer sequences (Thermo Fisher Scientific, MA, USA) used were as follows: Arc-F 5′-GGGAGGTCTTCTACCGTCTG-3′, Arc-R 5′- CTTCACCGAGCCCTGTTT-3′; Zif268-F 5′-GAACAACCCTACGAGCACCTG-3′, Zif268-R 5′-GCCACAAAGTGTTGCCACTG-3′; Actb-F 5′-CCCATCTATGAGGGTTACGC-3′, Actb-R 5′-TTTAATGTCACGCACGATTTC-3′.
WB was done according to previous description [28]. In brief, the BLA tissue were rapidly microdissected and homogenized in ice-cold lysis buffer containing (in mM): 1% Triton X-100, 0.1% SDS, 150 NaCl, 2 EDTA, 50 NaF, 10 sodium pyrophosphate, 1.0 Na3VO4, 1.0 PMSF, and complete protease inhibitor cocktail (Roche, Basel, Switzerland). The same amount of protein samples was separated by electrophoresis on a 7% SDS-PAGE gel (Invitrogen, CA, USA) and then transferred to nitrocellulose membranes (Bio-Rad, CA, USA). After blocked with 5 % (w/v) nonfat dry milk in TBS-T (Tris-buffer saline containing 0.1% Tween-20) for 1 h at room temperature, membranes were first hybridized with a primary antibody of interest overnight at 4 °C, then with a secondary antibody in TBS-T containing 5% nonfat milk for 1 h at room temperature. Signals were visualized with ECL (Thermo Fisher Scientific, MA, USA). Exposure time was adjusted so that the signals measured were in a linear range. Primary antibodies used were anti-Akt (1:1000, #9271, CST, MA, USA), anti-p-Akt at Ser473 (1:1000, #S9272, CST, MA, USA), anti-S6 (1:1000, #2217S, CST, MA, USA), anti-p-S6 at Ser 235/236 (1:1000, #2211S, CST, MA, USA), anti-Gsk3β (1:1000, #9832S, CST, MA, USA), anti-p-Gsk3β at Ser9 (1:1000, #9323S, CST, MA, USA), anti-Erk1/2 (1:1000, #9102 S, CST, MA, USA), anti-p-Erk1/2 at Thr202/Tyr204 (1:1000, #9101S, CST, MA, USA), anti-PKCα (1:1000, #ab32376, abcam, MA, USA), anti-p-PKCα at Ser657 (1:1000, #ab180848, abcam, MA, USA) and anti-β-actin (1:1000, Sigma, MO, USA). β-actin was used as controls for protein loading. The phosphorylated protein/total protein ratio in each treatment group was normalized by that in the home cage control group before comparison.
Statistical analysis
Results were expressed as means ± SEMs. Data were analyzed using paired or unpaired t-test, one-way ANOVA with Tukey’s multiple comparisons test, or two-way ANOVA with Sidak’s multiple comparisons test. P < 0.05 indicates a significant difference. Statistical analysis was performed with GraphPad Prism 6.0 (GraphPad Software).
Result
Local infusion of ghrelin in the BLA blocks CTA memory acquisition via PI3K activation
We previously reported that microinfusion of a single, low dose of ghrelin (12 ng, 0.5 µL/side) in the BLA during conditioning impairs acquisition of long-term CTA memory in rats through activation of GHS-R1a [16]. To build on this finding, we further explored intracellular signaling cascades that mediate the blocking effect of ghrelin and GHS-R1a activation on CTA memory. Since activation of PI3K was suggested to play a key role in ghrelin/GHS-R1a signaling, we first preadministered a PI3k inhibitor to the BLA during CTA training to test its effect on ghrelin-induced memory impairment. Specifically, LY294002 and ghrelin (LY294002 + ghrelin, n = 8) were microinfused in the BLA in sequence with a 15-min interval between substances (Fig. 1a). We also tested the effect of LY303511, a negative control compound for LY 294002 PI3K inhibitory activity, on ghrelin-induced memory impairment (LY303511 + ghrelin, n = 7). Meanwhile, the effect of LY294002 or ghrelin alone on the acquisition of CTA memory was also examined. Our results consistently showed that a single low dose of ghrelin (12 ng, 0.5 µL/side) microinfused in the BLA during CTA training blocked memory acquisition (Fig. 1b left; one-way ANOVA with Tukey’s multiple comparisons test, F(4,33) = 12.93, ghrelin vs. vehicle, P < 0.001, n = 8 per group). Microinfusion of LY294002 (1.0 ng, 0.5 µL/side) alone during conditioning had no effect on the CTA memory process (LY294002 vs. vehicle, P > 0.05, n = 7, 8); however, it completely blocked the adverse effect of ghrelin (Fig. 1b left; LY294002 + ghrelin vs. ghrelin, P < 0.01, n = 8 per group). In contrast, LY303511 (1.0 ng, 0.5 µL/side) pretreatment failed to block the repressive effect of ghrelin on CTA memory acquisition (Fig. 1b left; LY303511 + ghrelin vs. ghrelin, P > 0.05, n = 7, 8). Rats treated with vehicle (VEH), LY294002, or LY294002 + ghrelin showed a higher CTA memory index than random 50% (Fig. 1b left; one sample t test, P < 0.001), and the other groups did not (P > 0.05). Importantly, there were no differences among groups regarding total liquid intake either during conditioning or during the 24-h CTA memory test (Fig. 1b middle and right; one-way ANOVA with Tukey’s multiple comparisons test, middle F(4,33) = 0.59, right F(4,33) = 0.34, P > 0.05). Our findings thus indicate that ghrelin/GHS-R1a signaling blocks CTA memory acquisition via activation of the PI3K pathway.
a Diagram illustrating experimental procedure. Microinfusion in the BLA was done 20 min before CTA conditioning. b LY294002 pretreatment abolished ghrelin’s blocking effect on CTA memory. Left, aversion index representing CTA memory. Middle, liquid intakes during conditioning. Right, total liquid intakes during CTA memory test. n = 7-8 rats per group. c Quantitative RT-PCR assays showing Arc and Zif268 mRNA expression triggered by CTA memory retrieval in the BLA. mRNA expression was normalized by home cage control before comparing. n = 7-8 per group. d Representative histology image illustrating location of cannula tip in the BLA. Bar indicates 1 mm. All data are shown as means ± SEM. One-way ANOVA with Tukey’s multiple comparisons test, ***P < 0.001, **P < 0.01 or *P < 0.05 means a significant difference, n.s. means no significance.
Immediate early genes (IEG) Arc and zif268 have been implicated in synaptic plasticity supporting multiple forms of learning and memory, including CTA [29,30,31]. We then examined ghrelin’s effect on Arc and Zif268 expression in the BLA and tested whether LY294002 administration was able to abolish the effect of ghrelin on Arc and Zif268 expression. We found that ghrelin that was microinfused during conditioning repressed both Arc and Zif268 mRNA expression in the BLA triggered by CTA memory retrieval (Fig. 1c; one-way ANOVA with Tukey’s multiple comparisons test, Arc F(2,18) = 5.311, Zif268 F(2,21) = 5.188, ghrelin vs. VEH, P < 0.05, Arc: n = 7 per group; Zif268: n = 8 per group). As expected, LY294002 pretreatment prevented ghrelin’s repression of Arc and Zif268 expression (Fig. 1c; LY294002 + ghrelin vs. ghrelin, P < 0.05, n = 7–8 per group), a similar effect as it had on ghrelin-induced CTA memory impairment. Altogether, our findings demonstrate that intra-BLA injection of a single, low dose of ghrelin blocks CTA memory acquisition via the PI3K signaling pathway.
Local infusion of ghrelin in the BLA blocks CTA memory acquisition via PI3K/Akt/mTOR signaling cascades
Next, to determine downstream signaling cascades engaged in ghrelin/GHS-R1a-dependent inhibition of CTA memory acquisition, we checked the phosphorylation level of key molecules in the PI3K and Erk1/2 pathways shortly after the memory test. As shown in Fig. 2a, rats received an identical CTA procedure as above, with ghrelin or vehicle microinfusion during conditioning. BLA tissues were microdissected shortly after memory retrieval. We found that among the four targeting molecules (p-Akt-Ser473, p-Gsk3β-Ser9, p-S6-Ser235/236, p-Erk1/2-Thr202/Tyr204), only Akt and S6 phosphorylation was increased after ghrelin treatment compared to vehicle treatment (Fig. 2b–e; unpaired t test, t = 2.75 for Akt, t = 2.52 for S6, ghrelin vs. vehicle, P < 0.05, n = 5 per group), not Gsk3β or Erk1/2 (t = 1.84, P > 0.05). Our results thus suggest that PI3K/Akt/mTOR signaling cascades may mediate the blocking effect of ghrelin on CTA memory acquisition.
a Diagram illustrating experimental procedure. b–e Representative immunoblots (top) and the quantification (bottom) of protein phosphorylation. The vehicle (VEH) group and ghrelin group were normalized by the home cage control (HC-CON) group before comparing. n = 5 per group. All data are shown as means ± SEM. Unpaired t test, *P < 0.05 means a significant difference.
To confirm these findings, we further tested whether the mammalian target of rapamycin (mTOR) inhibitor rapamycin was able to abolish ghrelin’s inhibition of CTA memory acquisition (Fig. 3a). As shown in Fig. 3b left, we found that rapamycin (15 ng, 0.5 µL/side) preinfused in the BLA during conditioning removed ghrelin’s blocking effect on CTA memory (one-way ANOVA with Tukey’s multiple comparisons test, F(3,26) = 10.82, rapamycin+ghrelin vs. VEH + ghrelin, P < 0.01, n = 8 per group). Rapamycin alone did not affect CTA memory acquisition (rapamycin vs. VEH, P > 0.05, n = 7 per group). There were no differences among groups in total liquid intake either during conditioning or during the 24-h CTA memory test (Fig. 3b middle and right; one-way ANOVA with Tukey’s multiple comparisons test, middle F(3,26) = 0.40, right F(3,26) = 0.55, P > 0.05). We also investigated whether intra-BLA infusion of the selective glycogen synthase kinase-3 (Gsk3) inhibitor SB216763 (1.0 ng, 0.5 µL/side) or CHIR99021 (0.5 ng, 0.5 µL/side) could mimic ghrelin’s effect on CTA memory acquisition. Our results showed that none of them did, and both groups showed a memory index similar to that of the vehicle control group (Fig. 3c; one-way ANOVA with Tukey’s multiple comparisons test, F(2, 21) = 1.02, P > 0.05, n = 8 per group). In addition, neither SB216763 nor CHIR99021 affected total liquid intake during either CTA training or the memory test. Our findings thus indicate that ghrelin and subsequent GHS-R1a activation block CTA memory acquisition via the PI3K/Akt/mTOR signaling pathway.
a Diagram illustrating experimental procedure. b Rapamycin prevented ghrelin’s blocking effect on CTA memory. Left, aversion index representing CTA memory. Middle, liquid intakes during conditioning. Right, total liquid intakes during CTA memory test. n = 7–8 per group. c intra-BLA infusion of Gsk3 inhibitor during conditioning did not block CTA memory. Left, aversion index representing CTA memory. Middle, liquid intakes during conditioning. Right, total liquid intakes during CTA memory test. n = 8 per group. All data are shown as means ± SEM. One-way ANOVA with Tukey’s multiple comparisons test, ***P < 0.001, or **P < 0.01 means a significant difference, n.s. means no significance.
The PLC/PKC signaling pathway in the BLA also engages in ghrelin’s effect on CTA memory acquisition
Since ghrelin/GHS-R1a is well known to activate Gq-dependent molecular cascades, leading to hydrolysis of PIP2 by PLC and production of IP3 and DAG [8], we also pharmacologically inhibited local activities of PLC or its downstream molecules IP3 and PKC to test whether the PLC/PKC pathway contributed to ghrelin-induced impairment in CTA memory acquisition (Fig. 4a). Indeed, we found that intra-BLA infusion of either the PLC inhibitor U73122 (20 ng, 0.5 µL/side), PKC inhibitor GF109203X (0.2 ng, 0.5 µL/side) (Fig. 4b), or IP3 receptor antagonist 2-APB (4 ng, 0.5 µL/side) (Fig. 4c) during conditioning abolished ghrelin’s blocking effect on CTA memory, while none of them administered alone affected CTA memory processes (Fig. 4b, c). The U73122 + ghrelin group, the GF109203X + ghrelin group and the 2-APB + ghrelin group all exhibited a higher aversion index than the VEH + ghrelin group (one-way ANOVA with Tukey’s multiple comparisons test, F(4,35) = 6.22 in b, F(3,28) = 7.40 in c, P < 0.01, n = 8 per group). There were no differences among groups in total liquid intake either during CTA conditioning or during the memory test (P > 0.05). Supportively, our WB analyses showed that PKC phosphorylation was increased after ghrelin treatment compared to vehicle treatment (Supplemental Fig. 1; unpaired t test, t = 2.99, ghrelin vs. vehicle, P < 0.05, n = 6 per group), suggesting that the PLC/PKC signaling pathway in the BLA may also contribute to ghrelin’s suppressive effect on CTA memory acquisition.
a Diagram illustrating experimental procedure. b Selective PLC or PKC inhibitors prevented ghrelin’s blocking effect on CTA memory. Left, aversion index. Middle, liquid intakes during conditioning. Right, total liquid intakes during CTA memory test. n = 8 per group. c Intra-BLA infusion of IP3R antagonist 2-APB during conditioning blocked ghrelin’s effect on CTA memory. Left, aversion index. Middle, liquid intakes during conditioning. Right, total liquid intakes during CTA memory test. n = 8 per group. d The effect of MEK inhibitor PD98059, PKA inhibitor H-89, D1R antagonist SCH23390, and D2R antagonist haloperidol on ghrelin-induced impairment in CTA memory. Left, aversion index. Middle, liquid intakes during conditioning. Right, total liquid intakes during CTA memory test. n = 8 per group. All data are shown as means ± SEM. One-way ANOVA with Tukey’s multiple comparisons test, **P < 0.01 means significant a difference, n.s. means no significance.
The ghrelin/GHS-R1a system has been reported to participate in signaling pathways other than PI3K and PLC, including Erk1/2 and PKA, under different experimental conditions. In addition, GHS-R1a was reported to form heterodimers with dopamine receptors to affect downstream signaling. Therefore, we further examined the effect of the MEK inhibitor PD98059 (20 ng, 0.5 µL/side), PKA inhibitor H-89 (2 ng, 0.5 µL/side), D1R inhibitor SCH23390 (1.0 ng, 0.5 µL/side), and D2R inhibitor haloperidol (2.5 ng, 0.5 µL/side) on ghrelin-induced CTA memory impairment. Our results showed that none of those inhibitors preadministered in the BLA could block the effect of ghrelin on CTA memory acquisition (Fig. 4d; one-way ANOVA with Tukey’s multiple comparisons test, F(6,49) = 4.52, P > 0.05, in comparison to the VEH + ghrelin group, n = 8 per group). Hence, we concluded here that ghrelin/GHS-R1a signaling in the BLA suppresses CTA memory formation via both the PI3K/Akt/mTOR and PLC/PKC pathways.
Ghrelin administration in the BLA represses pyramidal neuron excitability both in vivo and ex vivo
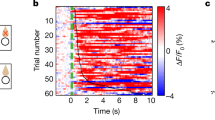
Our extracellular single-unit recordings previously showed that ghrelin regulated the firing of rat BLA neurons in a GHS-R1a-dependent manner. In this study, we further investigated ghrelin’s effect on neuronal firing of mouse BLA neurons with in vivo 16-channel electrodes (Fig. 5a). LFPs of a total of 96 recording sites were collected, and multiunit spikes were sorted (Fig. 5b). Of all 96 recordings in the BLA, 62 (65%) showed a decrease in spontaneous firing after ghrelin (20 µM) puff (Fig. 5c, d; 0.7 ± 0.2 Hz vs. baseline 2.1 ± 0.3 Hz, paired t test, t = 6.35, P < 0.0001, n = 62), while the remaining 34 (35%) showed an increase in firing (Fig. 5c, d; 1.9 ± 0.4 Hz vs. baseline 0.6 ± 0.2, paired t test, t = 3.56, P < 0.01, n = 34). The basal firing rate of the ghrelin-increased cells (0.6 ± 0.2 Hz) was lower than that of the ghrelin-decreased cells (2.1 ± 0.3 Hz) (Fig. 5e; unpaired t test, t = 3.34, P < 0.01).
a Extracelluar multichannel single-unit recording in mice. Left, diagram illustrating extracellular 16-channel electrode and microinfusion needle implanted in the BLA. Right, representative histology image illustrating location of electrode tip in the BLA. Electrode tip was dyed with DiI. Bar indicates 1 mm. b Sample multiunit firings recorded in the BLA with a 16-channel electrode. Channel 1 (Ch 1) was the deepest at 4800 µm. Vertical broken line was the onset of 20 µM ghrelin puffed at the speed of 0.3 µL/min. In this recording, ghrelin started to take effect after 1.5 µL was applied. Channels 4, 5, 8 and 9 displayed slight increase in firings after ghrelin application while all other channels showed obvious decrease. Vertical scale of 9 Hz applies to channel 1 and 8, and 3 Hz applies to the other channels. c A pie chart showing the proportion of BLA neurons with spontaneous firing rate decreased (Firing decrease) or increased (Firing increase) after ghrelin application. d Summarization of firing rate alteration of those two groups of BLA neurons after ghrelin application. e Basal firing rate comparison between those two groups of BLA neurons. n = 96 recordings in 6 animals. f Ex vivo recordings showing that ghrelin represses excitability of BLA pyramidal neurons. Left, representative whole-cell patch clamp recordings showing firings of BLA pyramidal neurons in response to a 240 pA (1000 ms in duration) current injection. Right, summary data showing the effect of bath application of ghrelin on firings of BLA pyramidal neurons. g–i Effects of ghrelin on membrane properties of BLA pyramidal neurons. g AP threshold and RMP. h Current injection to induce minimum (Min) and Maximum (Max) firings of BLA pyramidal neurons. i Input resistance. ACSF group, n = 19 cells; ghrelin group, n = 20 cells, 5 rats per group. All data are shown as means ± SEM. Two-way ANOVA with Sidak’s multiple comparisons test for f, paired t test for d, and unpaired t test for e, g–i. ****P < 0.0001, ***P < 0.001, **P < 0.01 or *P < 0.05 means a significant difference.
To explore the cellular and synaptic mechanism mediating the inhibitory effect of ghrelin on CTA memory acquisition, we further measured the effect of bath application of ghrelin on neuronal excitability, synaptic transmission and plasticity of rat BLA pyramidal neurons in ex vivo slices. Ghrelin (200 nM) was applied during slice recovery for 1 h and continuously during electrophysiological recording. We found that bath application of ghrelin caused a decrease in neuronal excitability of BLA pyramidal neurons. As shown in Fig. 5f, the number of APs triggered by depolarizing current (1 s duration) injection was lower during ghrelin administration (n = 20 cells) than with ACSF (n = 19 cells) (Fig. 5f; two-way ANOVA with Sidak’s multiple comparisons test, current F(5,119) = 84.69, treatment F(1,119) = 26.02, current x treatment interaction F(5,119) = 2.25, P < 0.05 to P < 0.01 along different depolarizing currents, 5 animals per group). Further analyses revealed that bath application of ghrelin elevated the threshold for AP (Fig. 5g; unpaired t test, t = 3.32, ghrelin vs. ACSF, P < 0.01), and it had no effect on RMP (P > 0.05). Consistently, the current injected to trigger the minimum number of firings was increased by ghrelin treatment (Fig. 5h; unpaired t test, t = 2.20, ghrelin vs. ACSF, P < 0.05). Our results thus indicated that acute application of ghrelin suppresses the excitability of BLA pyramidal neurons, which may contribute to ghrelin-induced impairment in CTA memory acquisition.
In addition, bath application of ghrelin ex vivo did not change excitatory or inhibitory miniature postsynaptic currents (mEPSCs or mIPSCs) (Fig. 6a, b; ghrelin vs. ACSF, unpaired t test, mEPSC comparison t = 1.47, mIPSC comparison t = 0.21, P > 0.05, n = 15–19 cells, 7 rats per group). We also checked ghrelin’s effect on evoked EPSCs (eEPSCs) of BLA pyramidal neurons and found no change in eEPSC amplitude after bath application of ghrelin (Fig. 6c; paired t test, t = 0.80, ghrelin vs. ACSF baseline, P > 0.05, n = 6 cells from 6 rats). Neither did ghrelin treatment change the paired pulse ratio (Fig. 6d; paired t test, t = 0.57, ghrelin vs. ACSF baseline, P > 0.05, n = 6 cells from 6 rats). Altogether, our findings demonstrated that while ghrelin inhibited intrinsic excitability, it had no substantial effect on synaptic transmission or plasticity of BLA pyramidal neurons.
Ghrelin’s effect on miniature excitatory (a) and inhibitory (b) postsynaptic currents. n = 15–19 neurons from 7 rats. c Ghrelin had no effect on eEPSCs of BLA pyramidal neurons. Left, sample sweeps showing the amplitude of eEPSCs before and during ghrelin application. Right, time course of eEPSCs during ghrelin application. d Ghrelin did not change PPR of BLA pyramidal neurons. Left, sample traces showing no change of PPR during ghrelin application. Right, group data of PPF for ACSF and ghrelin application. n = 6 neurons from 6 rats. All data are shown as means ± SEM. Unpaired t test for a and b, and paired t test for c and d.
Discussion
We have reported previously that local infusion of a single low dose of ghrelin in the BLA activates GHS-R1a and impairs acquisition rather than consolidation or retrieval of aversive memory for conditioned taste [16]. In this study, we further demonstrated that ghrelin microinfusion in the BLA blocks CTA memory acquisition through the PI3K/Akt/mTOR and PLC/PKC signaling pathways. Since a single, low dose of ghrelin delivered in the BLA did not affect total liquid intake during the conditioning or CTA memory test, we predict that the blocking effect of ghrelin on CTA memory acquisition is specific and more likely attributes to the interruption of initial encoding for taste-aversion information. These results, along with our previous finding that local infusion of a similar amount of ghrelin in the dorsal hippocampus impairs spatial memory formation without changing swimming speed or motor coordination [17], suggest that a low dose of ghrelin may disrupt memory encoding in general.
Our findings are incongruous with previous studies demonstrating that ghrelin and GHS-R1a agonists facilitate learning and memory by activating GHS-R1a signaling [10, 12, 13, 24, 32]. The reason for this discrepancy may result from different doses and durations of treatment that may induce distinct receptor kinetics. A previous study has shown that transient and intensive GHS-R1a stimulation leads to rapid desensitization and internalization of the receptor that is slow to recover [33], while chronic administration of a GHS-R1a agonist may not [34]. Indeed, many previous studies delivered large amounts of ghrelin (100 ng100 µg) locally or systemically [12, 32, 35, 36], which may be out of physiological range. Instead, we delivered a low dose of ghrelin in specific brain regions (12 ng in BLA or 8 ng in dCA1) and obtained consistent results showing that ghrelin acts as a memory inhibitor in the acquisition or early encoding phase. Although GHS-R1a is relatively rich in the central nervous system, ghrelin-producing cells are undetectable, with perhaps the exception of a tiny amount in the hypothalamus [37]. In addition, it was reported that only trace amounts of circulating ghrelin are accessible to the brain [26]. Therefore, we consider our findings to show more of the physiological than the pharmacological role of ghrelin in learning and memory. Our findings are consistent with limited human data showing that serum ghrelin is inversely associated with cognitive function in both healthy individuals and patients with mild cognitive impairment (MCI) [38,39,40,41].
Ghrelin was reported to promote spine density and facilitate LTP induction in acute slices [12], to trigger synaptic incorporation of AMPA receptors in hippocampal cultures [13] and to prolong LTP expression in the dentate gyrus in vivo [24]. All these previous findings provide synaptic mechanisms underlying ghrelin modulation of long-term memory consolidation or retention, especially in the hippocampus [12, 24, 32, 35, 42]. However, the synaptic mechanism mediating ghrelin’s effect on memory acquisition has not yet been explored. In this study, we found no acute effect of ghrelin administration on synaptic transmission or short-term plasticity (PPR) of BLA pyramidal neurons. In addition, our preliminary data showed that ghrelin has no effect on 100 Hz tetanus-induced 1-h LTP (data not shown), which depends primarily on short-term kinase activity and is thought to be critical for memory acquisition [43]. Altogether, our current findings suggest that mechanisms other than synaptic changes may contribute to ghrelin’s inhibition of CTA memory acquisition.
In addition to learning-induced modulation of synaptic strength, neuronal intrinsic excitability changes are also assumed to serve as a critical cellular mechanism underlying learning and memory [44,45,46,47,48,49]. Moreover, CTA conditioning has been reported to result in long-term excitability changes in both BLA and insular cortex neurons [50, 51]. Parameters associated with APs, such as afterhyperpolarization (AHP), AP half-width and frequency, AP threshold, and input resistance, have been used to quantify changes in intrinsic excitability. Alterations in these firing properties usually reflect changes in the overall expression, distribution, and function of voltage-gated ion channels [52]. It is important that our in vivo and ex vivo studies consistently showed that a low dose of ghrelin (≤20 µM in vivo and 200 nM ex vivo) suppresses the firing of a large portion of BLA neurons in both rats and mice. Moreover, we discovered in this study that ghrelin increased the action potential threshold and thus contributed to decreased firing of BLA pyramidal neurons. Similarly, the intrinsic excitability of dCA1 pyramidal neurons was also reduced by bath application of ghrelin [53]. We thus suggest that ghrelin/GHS-R1a-induced impairment in memory acquisition is common for different brain regions essential for memory encoding, and modulation of intrinsic excitability plays a key role in this process. Protein kinases such as PKA, PKC, and calmodulin-dependent protein kinase II (CaMKII) have been reported to alter ion channel expression and modulate intrinsic excitability [52]. Moreover, we found that pretreatment with the PI3K inhibitor LY294002 completely abolished ghrelin’s inhibition of both the excitability of dCA1 pyramidal neurons and hippocampus-dependent memory [53]. Therefore, it is reasonable to assume that repressing the intrinsic excitability of BLA pyramidal neurons via PI3K/Akt/mTOR and/or PLC/PKC signaling cascades contributes to ghrelin/GHS-R1a-induced acquisition dysfunction of CTA memory.
Neuronal intrinsic excitability is primarily determined by the distribution and function of voltage-gated ion channels. The specific channels that are modified by ghrelin-activated GHS-R1a signaling and contribute to intrinsic excitability changes in BLA pyramidal neurons are currently undefined. Previous studies have demonstrated that ghrelin inhibits Kv7/KCNQ/M-channels in dopaminergic neurons by activating Gα11/q and causing hydrolysis of PIP2 by PLC [54]. In addition to M-channels, PIP2 also regulates the function of other channels playing important roles in regulating cellular excitability, such as Na+ channels and inwardly rectifying potassium channels [55]. Additionally, ghrelin was also reported to impair CaV2.1 and CaV2.2 currents in hypothalamic neurons [56]. Future studies are needed to identify specific channels modified by ghrelin/GHS-R1a and downstream signaling cascades in the BLA, leading to consequent CTA memory impairment.
In conclusion, we report here that microinfusion of a single low dose of ghrelin in the BLA impairs CTA memory acquisition by activating GHS-R1a and downstream PI3K/Akt/mTOR and PLC/PKC signaling pathways, causing an increase in the AP threshold and a resultant decrease in neuronal intrinsic excitability. Our findings suggest that GHS-R1a may be a promising target to modify memory processes and to treat related cognitive decline.
References
Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 1999;402:656–60.
Perello M, Cabral A, Cornejo MP, De Francesco PN, Fernandez G, Uriarte M. Brain accessibility delineates the central effects of circulating ghrelin. J Neuroendocrinol. 2019;31:e12677.
Murtuza MI, Isokawa M. Endogenous ghrelin-O-acyltransferase (GOAT) acylates local ghrelin in the hippocampus. J Neurochem. 2018;144:58–67.
Abizaid A, Hougland JL. Ghrelin Signaling: GOAT and GHS-R1a take a LEAP in complexity. Trends Endocrinol Metab. 2020;31:107–17.
Stevanovic DM, Grefhorst A, Themmen AP, Popovic V, Holstege J, Haasdijk E, et al. Unacylated ghrelin suppresses ghrelin-induced neuronal activity in the hypothalamus and brainstem of male rats [corrected]. PLoS One. 2014;9:e98180.
Hornsby AKE, Buntwal L, Carisi MC, Santos VV, Johnston F, Roberts LD, et al. Unacylated-ghrelin impairs hippocampal neurogenesis and memory in mice and is altered in Parkinson’s dementia in humans. Cell Rep Med. 2020;1:100120.
Agosti E, De Feudis M, Angelino E, Belli R, Alves Teixeira M, Zaggia I, et al. Both ghrelin deletion and unacylated ghrelin overexpression preserve muscles in aging mice. Aging. 2020;12:13939–57.
Howard AD, Feighner SD, Cully DF, Arena JP, Liberator PA, Rosenblum CI, et al. A receptor in pituitary and hypothalamus that functions in growth hormone release. Science. 1996;273:974–7.
Shiimura Y, Horita S, Hamamoto A, Asada H, Hirata K, Tanaka M, et al. Structure of an antagonist-bound ghrelin receptor reveals possible ghrelin recognition mode. Nat Commun. 2020;11:4160.
Andrews ZB. The extra-hypothalamic actions of ghrelin on neuronal function. Trends Neurosci. 2011;34:31–40.
Spencer SJ, Emmerzaal TL, Kozicz T, Andrews ZB. Ghrelin’s role in the hypothalamic-pituitary-adrenal axis stress response: implications for mood disorders. Biol Psychiatry. 2015;78:19–27.
Diano S, Farr SA, Benoit SC, McNay EC, da Silva I, Horvath B, et al. Ghrelin controls hippocampal spine synapse density and memory performance. Nat Neurosci. 2006;9:381–8.
Ribeiro LF, Catarino T, Santos SD, Benoist M, van Leeuwen JF, et al. Ghrelin triggers the synaptic incorporation of AMPA receptors in the hippocampus. Proc Natl Acad Sci USA. 2014;111:E149–58.
Dresler M, Kluge M, Genzel L, Schussler P, Steiger A. Nocturnal administration of ghrelin does not promote memory consolidation. Pharmacopsychiatry. 2010;43:277–8.
Albarran-Zeckler RG, Brantley AF, Smith RG. Growth hormone secretagogue receptor (GHS-R1a) knockout mice exhibit improved spatial memory and deficits in contextual memory. Behav Brain Res. 2012;232:13–9.
Song L, Zhu Q, Liu T, Yu M, Xiao K, Kong Q, et al. Ghrelin modulates lateral amygdala neuronal firing and blocks acquisition for conditioned taste aversion. PLoS One. 2013;8:e65422.
Zhu Q, Xiao K, Yu M, Niu M, Li C, Gao Y, et al. Ghrelin but not nesfatin-1 affects certain forms of learning and memory in both rats and mice. Brain Res. 2013;1541:42–51.
Song G, Zhu Q, Han F, Liu S, Zhao C, Zhou Y. Local infusion of ghrelin into the lateral amygdala blocks extinction of conditioned taste aversion in rats. Neurosci Lett. 2018;662:71–6.
Bennett KA, Langmead CJ, Wise A, Milligan G. Growth hormone secretagogues and growth hormone releasing peptides act as orthosteric super-agonists but not allosteric regulators for activation of the G protein Galpha(o1) by the ghrelin receptor. Mol Pharmacol. 2009;76:802–11.
Evron T, Peterson SM, Urs NM, Bai Y, Rochelle LK, Caron MG, et al. G Protein and beta-arrestin signaling bias at the ghrelin receptor. J Biol Chem. 2014;289:33442–55.
Chung H, Li E, Kim Y, Kim S, Park S. Multiple signaling pathways mediate ghrelin-induced proliferation of hippocampal neural stem cells. J Endocrinol. 2013;218:49–59.
Kanoski SE, Fortin SM, Ricks KM, Grill HJ. Ghrelin signaling in the ventral hippocampus stimulates learned and motivational aspects of feeding via PI3K-Akt signaling. Biol Psychiatry. 2013;73:915–23.
Cavalier M, Crouzin N, Ben Sedrine A, de Jesus Ferreira MC, Guiramand J, Cohen-Solal C, et al. Involvement of PKA and ERK pathways in ghrelin-induced long-lasting potentiation of excitatory synaptic transmission in the CA1 area of rat hippocampus. Eur J Neurosci. 2015;42:2568–76.
Chen L, Xing T, Wang M, Miao Y, Tang M, Chen J, et al. Local infusion of ghrelin enhanced hippocampal synaptic plasticity and spatial memory through activation of phosphoinositide 3-kinase in the dentate gyrus of adult rats. Eur J Neurosci. 2011;33:266–75.
Schellekens H, van Oeffelen WE, Dinan TG, Cryan JF. Promiscuous dimerization of the growth hormone secretagogue receptor (GHS-R1a) attenuates ghrelin-mediated signaling. J Biol Chem. 2013;288:181–91.
Kern A, Mavrikaki M, Ullrich C, Albarran-Zeckler R, Brantley AF, Smith RG. Hippocampal dopamine/DRD1 signaling dependent on the ghrelin receptor. Cell. 2015;163:1176–90.
Li N, Song G, Wang Y, Zhu Q, Han F, Zhang C, et al. Blocking constitutive activity of GHSR1a in the lateral amygdala facilitates acquisition of conditioned taste aversion. Neuropeptides. 2018;68:22–7.
Cui L, Sun W, Yu M, Li N, Guo L, Gu H, et al. Disrupted-in-schizophrenia1 (DISC1) L100P mutation alters synaptic transmission and plasticity in the hippocampus and causes recognition memory deficits. Mol Brain. 2016;9:89.
Jones MW, Errington ML, French PJ, Fine A, Bliss TV, Garel S, et al. A requirement for the immediate early gene Zif268 in the expression of late LTP and long-term memories. Nat Neurosci. 2001;4:289–96.
Plath N, Ohana O, Dammermann B, Errington ML, Schmitz D, Gross C, et al. Arc/Arg3.1 is essential for the consolidation of synaptic plasticity and memories. Neuron. 2006;52:437–44.
Lonergan ME, Gafford GM, Jarome TJ, Helmstetter FJ. Time-dependent expression of Arc and zif268 after acquisition of fear conditioning. Neural Plast. 2010;2010:139891.
Carlini VP, Varas MM, Cragnolini AB, Schioth HB, Scimonelli TN, de Barioglio SR. Differential role of the hippocampus, amygdala, and dorsal raphe nucleus in regulating feeding, memory, and anxiety-like behavioral responses to ghrelin. Biochem Biophys Res Commun. 2004;313:635–41.
Camina JP, Carreira MC, El Messari S, Llorens-Cortes C, Smith RG, Casanueva FF. Desensitization and endocytosis mechanisms of ghrelin-activated growth hormone secretagogue receptor 1a. Endocrinology. 2004;145:930–40.
Meyer RM, Burgos-Robles A, Liu E, Correia SS, Goosens KA. A ghrelin-growth hormone axis drives stress-induced vulnerability to enhanced fear. Mol Psychiatry. 2014;19:1284–94.
Carlini VP, Monzon ME, Varas MM, Cragnolini AB, Schioth HB, Scimonelli TN, et al. Ghrelin increases anxiety-like behavior and memory retention in rats. Biochem Biophys Res Commun. 2002;299:739–43.
Goshadrou F, Ronaghi A. Attenuating the effect of Ghrelin on memory storage via bilateral reversible inactivation of the basolateral amygdale. Behav Brain Res. 2012;232:391–4.
Cabral A, Lopez Soto EJ, Epelbaum J, Perello M. Is ghrelin synthesized in the central nervous system? Int J Mol Sci. 2017;18:638.
Spitznagel MB, Benitez A, Updegraff J, Potter V, Alexander T, Glickman E, et al. Serum ghrelin is inversely associated with cognitive function in a sample of non-demented elderly. Psychiatry Clin Neurosci. 2010;64:608–11.
Bellar D, Glickman EL, Judge LW, Gunstad J. Serum ghrelin is associated with verbal learning and adiposity in a sample of healthy, fit older adults. Biomed Res Int. 2013;2013:202757.
Yoshino Y, Funahashi Y, Nakata S, Ozaki Y, Yamazaki K, Yoshida T, et al. Ghrelin cascade changes in the peripheral blood of Japanese patients with Alzheimer’s disease. J Psychiatr Res. 2018;107:79–85.
Cao X, Zhu M, He Y, Chu W, Du Y, Du H. Increased serum acylated ghrelin levels in patients with mild cognitive impairment. J Alzheimers Dis. 2018;61:545–52.
Ghersi MS, Gabach LA, Buteler F, Vilcaes AA, Schioth HB, Perez MF, et al. Ghrelin increases memory consolidation through hippocampal mechanisms dependent on glutamate release and NR2B-subunits of the NMDA receptor. Psychopharmacology. 2015;232:1843–57.
Lynch MA. Long-term potentiation and memory. Physiol Rev. 2004;84:87–136.
Daoudal G, Debanne D. Long-term plasticity of intrinsic excitability. learning rules and mechanisms. Learn Mem. 2003;10:456–65.
Zhang W, Linden DJ. The other side of the engram. experience-driven changes in neuronal intrinsic excitability. Nat Rev Neurosci. 2003;4:885–900.
Disterhoft JF, Oh MM. Learning, aging and intrinsic neuronal plasticity. Trends Neurosci. 2006;29:587–99.
Matthews EA, Linardakis JM, Disterhoft JF. The fast and slow afterhyperpolarizations are differentially modulated in hippocampal neurons by aging and learning. J Neurosci. 2009;29:4750–5.
Oh MM, Oliveira FA, Disterhoft JF. Learning and aging related changes in intrinsic neuronal excitability. Front Aging Neurosci. 2010;2:2.
Oh MM, Disterhoft JF. Increased excitability of both principal neurons and interneurons during associative learning. Neuroscientist. 2015;21:372–84.
Yasoshima Y, Yamamoto T. Short-term and long-term excitability changes of the insular cortical neurons after the acquisition of taste aversion learning in behaving rats. Neuroscience. 1998;84:1–5.
Kim MJ, Mizumori SJ, Bernstein IL. Neuronal representation of conditioned taste in the basolateral amygdala of rats. Neurobiol Learn Mem. 2010;93:406–14.
Chen L, Cummings K, Mau W, Zaki Y, Dong Z, Rabinowitz S, et al. The role of intrinsic excitability in the evolution of memory: significance in memory allocation, consolidation, and updating. Neurobiol Learn Mem. 2020;173:107266.
Li N, Xiao K, Mi X, Li N, Guo L, Wang X, et al. Ghrelin signaling in dCA1 suppresses neuronal excitability and impairs memory acquisition via PI3K/Akt/GSK-3β cascades. Neuropharmacology. 2021;203:108871.
Shi L, Bian X, Qu Z, Ma Z, Zhou Y, Wang K, et al. Peptide hormone ghrelin enhances neuronal excitability by inhibition of Kv7/KCNQ channels. Nat Commun. 2013;4:1435.
Soom M, Schonherr R, Kubo Y, Kirsch C, Klinger R, Heinemann SH. Multiple PIP2 binding sites in Kir2.1 inwardly rectifying potassium channels. FEBS Lett. 2001;490:49–53.
Lopez Soto EJ, Agosti F, Cabral A, Mustafa ER, Damonte VM, Gandini MA, et al. Constitutive and ghrelin-dependent GHSR1a activation impairs CaV2.1 and CaV2.2 currents in hypothalamic neurons. J Gen Physiol. 2015;146:205–19.
Acknowledgements
This work was supported by NNSFC (Grant no. 32071141 and 91732110 to YZ, 31900854 to MY), China Postdoctoral Science Foundation (Grant no. 2019M662292 to MY), and NSFC of SD province (Grant no. ZR2019ZD34 and 2019GGX101045 to YZ, ZR201911120651 to NL). We thank Ms. Jennifer Li for native language editing.
Author information
Authors and Affiliations
Contributions
YZ designed and supervised the experiments. MY, QQZ and MLN performed behavioral experiments. ZSZ and JDG designed and performed electrophysiological experiment, NL and BQR helped with data analysis. YZ and TBY wrote the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary information
Rights and permissions
About this article
Cite this article
Yu, M., Zhu, Qq., Niu, Ml. et al. Ghrelin infusion into the basolateral amygdala suppresses CTA memory formation in rats via the PI3K/Akt/mTOR and PLC/PKC signaling pathways. Acta Pharmacol Sin 43, 2242–2252 (2022). https://doi.org/10.1038/s41401-022-00859-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-022-00859-w