Abstract
Nonalcoholic fatty liver disease is a growing public health crisis, with phenotypes from nonalcoholic fatty liver to nonalcoholic steatohepatitis, currently known as NASH, which can progress to liver fibrosis and end stage cirrhosis. NASH is associated with an increased risk of cardiovascular disease and Type 2 diabetes mellitus. There are still no U.S. FDA approved drugs or biological treatments for NASH or related liver diseases. Despite official agency guidance, the regulatory pathway to ultimate product approval is unclear, due to both the extra-hepatic factors that contribute to NASH, as well as the organizational structure of FDA, with its traditional separation of therapeutic indications within discrete review divisions. There is hope that continued evolution of the regulatory process will lead to the ability for clinical trial endpoints supporting NASH treatment approval to include both liver-based and traditional metabolic measures, independent of specific FDA division review.
Similar content being viewed by others
Introduction
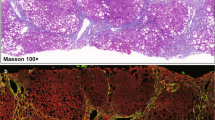
Nonalcoholic fatty liver disease (NAFLD) is the most common cause of chronic liver disease in the industrialized world [1]. The phenotypes of the disease range from nonalcoholic fatty liver (NAFL) to nonalcoholic steatohepatitis (NASH), which can progress to liver fibrosis and end stage cirrhosis [2]. NASH is also associated with an increased risk of cardiovascular (CV) morbidity and mortality [3], as well as Type 2 diabetes mellitus (DM) [4]. Cirrhosis associated with NASH increases the risk of hepatocellular carcinoma [5]. Currently, liver biopsy is currently the most generally acceptable procedure for the diagnosis of NASH and to accurately assess progression to cirrhosis. Although less invasive methods are in development, these imaging tests and serum biomarkers have not yet reached adequate levels of clinical validation needed for regulatory utility [6]. There are still no U.S. FDA approved drugs or biological treatments for NASH or related liver diseases [7].
Regulatory history of NASH at FDA
With the FDA reorganization of the Office of New Drugs (OND) in the Center for Drug Evaluation and Research (CDER) in 2005, the new Gastroenterology Products Division for the first time regulated both drugs and biologic products in therapeutic areas, including hepatology. The general advice to sponsors of NASH products at that time included the suggestion to consider studying related hepatic conditions where the natural history and progression to end-stage disease were better understood, such as primary biliary cholangitis (PBC). The epidemiology of NASH was then in its infancy. It was unclear in patients with fatty liver, how quickly they progressed to NASH, fibrosis, then end stage cirrhosis and death, and also what percentage of patients progressed versus had continued asymptomatic disease. Sponsors were advised in parallel to study the natural history of NASH patients under standard of care, as well as to develop non-invasive measures of liver fat, hepatic stiffness and stage of fibrosis, which could then be correlated with liver biopsy-derived data and thus validated in clinical trials across multiple development programs.
During this same timeframe, the importance of monitoring patients in clinical trials for drug-induced liver injury (DILI) was raised for drug development in general and especially when treating patients with underlying liver disease. These concepts for monitoring patients were captured in a draft document by FDA’s Gastroenterology Product Division Team Leader Ruyi He, MD, which then served as the basis of the FDA guidance document “Drug-Induced Liver Injury: Premarketing Clinical Evaluation” published in July 2009 [8]. This important guidance is still in effect today and serves as the template for monitoring for drug-induced liver injury in the NASH population, who already have liver compromise due to their underlying disease. Note that this is the same as Dr. Ruyi He, who after his distinguished career at U.S. FDA, went onto serving as Chief Scientist at the Center For Drug Evaluation (CFDA) in China. His work in both China and the U.S. serves as a model for the goals of mutual cooperation and partnership which will be needed for large multi-regional clinical trials to support NASH drug approval.
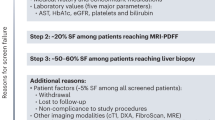
With the academic input from the National Institutes of Health (NIH) and the consensus achieved at the 2009 research workshop of the American Association for Study of Liver Diseases (AASLD) on the key endpoints and specific trial design issues for development of diagnostic biomarkers and treatment trials for NASH [9], FDA staff developed advice for each specific sponsor advice meeting provided on a case-by-case basis. It was not until December 2018 that the first FDA guidance—Noncirrhotic Nonalcoholic Steatohepatitis With Liver Fibrosis: Developing Drugs for Treatment Guidance for Industry—regarding regulatory issues around NASH drug development was published [10]. As described by FDA staff in this document, the following regulatory paradigm was outlined:
“Of the histologic features of NASH, fibrosis is considered the strongest predictor of adverse clinical outcomes, including liver-related death. Because of the significant prognostic differences between NAFL and NASH with fibrosis and the absence of clear clinical, biochemical, or histological criteria that can identify patients with NAFL who are at risk for progression to NASH, the FDA encourages sponsors to focus drug development on the area of greatest need and potential effect on health (i.e., noncirrhotic NASH with liver fibrosis)” [10].
Therefore, based upon this first FDA guidance, noncirrhotic NASH with liver fibrosis should be the focus of drug sponsors. FDA described specific patient inclusion criteria in Table 1.
This guidance also outlined what elements should be included in NASH clinical development, such as evaluation of drugs for the treatment of NASH in double-blind, placebo controlled clinical trials of sufficient duration and size. In addition, any NASH treatment should “slow the progress of, halt, or reverse disease progression and improve clinical outcomes (i.e., prevent progression to cirrhosis and cirrhosis complications, reduce the need for liver transplantation, and improve survival)” [10].
It was not until the second guidance published in June 2019—Nonalcoholic Steatohepatitis with Compensated Cirrhosis—that FDA addressed advanced disease and described recommended clinical trial design and efficacy endpoints as outlined in Table 2 [11].
It was also clear from this second guidance that the accelerated approval pathway for this advanced stage of the disease was not a regulatory option from the perspective of the FDA staff:
“The FDA strongly recommends clinical outcome trials to support a marketing application… at present the relationship between histological changes in cirrhosis and clinical outcomes has not been characterized…there is insufficient evidence to support the use of histological improvements as a surrogate endpoint that is reasonably likely to predict clinical benefit to support accelerated approval”[11].
Specific NASH sponsors appeared to be following agency guidance and conducted patient trials, as documented in https://clinicaltrials.gov. A notable example of a sponsor following this FDA advice is Intercept Pharmaceuticals in its development programs for NASH entitled “Randomized Global Phase 3 Study to Evaluate the Impact on NASH With Fibrosis of Obeticholic Acid Treatment (REGENERATE)” [12]. The data from this Phase 3 clinical trial were published in the peer-reviewed literature and was optimistic regarding its regulatory future since the study met its “18 Month Interim Analysis Endpoint” on liver histology, defined as “improvement of fibrosis by ≥1 stage with no worsening of NASH” [13].
“REGENERATE is designed in conjunction with regulatory authorities to support regulatory approvals in NASH. This robust phase 3 study assesses the effect of OCA on liver histology as a surrogate for transplant-free survival and liver-related outcomes, including progression to cirrhosis and mortality, and will ultimately assess clinical benefit through specific evaluation of these outcomes”[13].
However, with submission of its New Drug Application (NDA) to FDA, at the end of the FDA review cycle the sponsor provided the following press release:
“Intercept Pharmaceuticals, Inc. (Nasdaq: ICPT), a biopharmaceutical company focused on the development and commercialization of novel therapeutics to treat progressive non-viral liver diseases, today announced that the U.S. Food and Drug Administration (FDA) has issued a Complete Response Letter (CRL) regarding the New Drug Application (NDA) for obeticholic acid (OCA) for the treatment of fibrosis due to nonalcoholic steatohepatitis (NASH).
The CRL indicated that, based on the data the FDA has reviewed to date, the Agency has determined that the predicted benefit of OCA based on a surrogate histopathologic endpoint remains uncertain and does not sufficiently outweigh the potential risks to support accelerated approval for the treatment of patients with liver fibrosis due to NASH. The FDA recommends that Intercept submit additional post-interim analysis efficacy and safety data from the ongoing REGENERATE study in support of potential accelerated approval and that the long-term outcomes phase of the study should continue” [14].
This non-approval action, called Complete Response Letter (CRL) by FDA created uncertainty among NASH drug development sponsors, academic hepatologists and the liver patient advocacy community. Subsequent communications by FDA Hepatology Review Division staff, both in print [15] and on the web [16], emphasized that agency advice has not deviated from the previous published guidance documents of 2018 and 2019, despite the recent agency NASH drug application CRL.
Unanswered regulatory questions
Since the mechanisms underlying NASH include accumulation of fat in the liver, hepatocyte inflammation, fibrosis and progression to liver cirrhosis, it is unclear how treatments will be judged if they only treat one aspect of this disease, such as fat accumulation or NASH resolution. It remains to be seen how well any one mechanism will be likely to predict ultimate clinical benefit in NASH patients, the regulatory standard for FDA accelerated approval, or what the level of evidence necessary will be to support the use of biomarkers and move beyond the current clinical trial primary endpoints of changes in histology from liver biopsy samples, looking at both NAS and degree of liver fibrosis currently supported by FDA. It is likely that multiple mechanisms will need to be targeted using combination drug therapy to reduce fat in the liver, decrease hepatic inflammation and prevent/reverse liver fibrosis. None of the current proposed biomarkers have adequate supporting data across drug sponsors to support FDA validation of qualification in the near future.
Since NASH is associated with an increased risk of cardiovascular (CV) morbidity and mortality [3], as well as Type 2 diabetes mellitus (DM) [4], it would be of interest to see if FDA will consider clinical trial endpoints in these related therapeutic areas and thus outside of traditional hepatology review. FDA was able to incorporate CV measures in Type 2 DM drug approvals when faced with questions from health experts outside the agency, and incorporated the following into FDA diabetes guidance:
“Glycemic control in these studies has been based on changes in HbA1c. This endpoint reflects a beneficial effect on the immediate clinical consequences of diabetes (hyperglycemia and its associated symptoms) and lowering of HbA1c is reasonably expected to reduce the long-term risk of microvascular complications. Therefore, reliance on HbA1c remains an acceptable primary efficacy endpoint for approval of drugs seeking an indication to treat hyperglycemia secondary to diabetes mellitus. However, diabetes mellitus is associated with an elevated risk of cardiovascular disease, which is the leading cause of morbidity and mortality in this patient population”[17].
Subsequent agency documents stress the relationship between CV and diabetes diseases and described “rigorous methods for the collection of adverse CV events and assess them by adjudication” [18]. Similarly, allowing NASH studies to have clinical endpoints to include lowering HbA1c or reduction of CV risk using traditional analysis of major adverse cardiovascular events (MACE) would be useful. In addition, since according to FDA, “low-density lipoprotein cholesterol (LDL-C) causes atherosclerotic disease” that “has been repeatedly demonstrated in experimental studies, epidemiological cohorts, randomised clinical trials of LDL-C lowering drugs,” and an “individual’s risk of atherosclerotic disease is strongly determined by their cumulative lifelong exposure to LDL-C” [19], then LDL-C lowering should also have consideration for NASH clinical trial endpoints.
Regulatory optimism for the future?
In 2017, FDA’s CDER embarked on an initiative to modernize the New Drugs Regulatory Program. This reorganization of the Office of New Drugs is now complete. In addition to “enabling greater efficiency,” these envisioned changes will help FDA to “better understand the diseases intended to be treated by the drugs evaluated for approval” [20]. The new “Division of Hepatology and Nutrition (DHN) regulates and reviews Investigational New Drug (IND) applications and marketing applications for drug and biologic products intended for the prevention, treatment or diagnosis of conditions including: Nonalcoholic fatty liver disease (NAFLD) including nonalcoholic steatohepatitis (NASH)” [21]. A recent example of cooperation between the new review divisions is of the FDA approval of the supplement indication for reduction of CV death in the general heart failure patient population by the Division of Cardiology and Nephrology [22], for a previously approved diabetes drug regulated by the Division of Diabetes, Lipid Disorders, and Obesity [23]. JARDIANCE is now indicated for the following:
-
Lower blood sugar along with diet and exercise in adults with type 2 diabetes;
-
Reduce the risk of cardiovascular death in adults with type 2 diabetes who also have known cardiovascular disease;
-
Reduce the risk of cardiovascular death and hospitalization for heart failure in adults with heart failure. [24]
Specifically, this diabetes drug was approved for “a new indication to reduce the risk of cardiovascular death and hospitalization for heart failure in adults with heart failure and reduced ejection fraction” [25], with no mention of any diabetes population, based upon the data provided by the sponsor to FDA. A similar regulatory path forward could be considered for NASH patients, both with and without Type 2 diabetes. The newly created Division of Hepatology and Nutrition [21], Division of Cardiology and Nephrology [22] and Division of Diabetes, Lipid Disorders, and Obesity [23], should be able to work together and cover all aspects of NASH disease and agree upon clinical trial designs that include endpoints traditionally from all three divisions.
Further regulatory optimism is derived from FDA publicly expressing interest in the agency staff finding what is important to patients, including those with NASH, in a program called “patient-focused drug development (PFDD)”, which is
“a systematic approach to help ensure that patients’ experiences, perspectives, needs, and priorities are captured and meaningfully incorporated into drug development and evaluation. As experts in what it is likely to live with their condition, patients are uniquely positioned to inform the understanding of the therapeutic context for drug development and evaluation” [26].
The primary goal of patient-focused drug development is to better incorporate the patient’s voice in drug development and evaluation, including advancing use of systematic approaches to collecting meaningful patient and caregiver input to more consistently inform both drug development and regulatory decision-making [26].
What is important to NASH patients is likely to be improved quality of their life, reduction in fatigue, improved exercise tolerance, weight loss, reduction in cardiac events and in general, a long healthy life [26]. Patient Focused Drug Development efforts will inform the creation and validation of Patient Reported Outcome (PRO) measures that can serve as endpoints in clinical trials. Drugs that ultimately receive FDA approval using these PRO endpoints, will then be based upon data which directly support patient benefit and not indirectly or theoretically such as improvement in one stage fibrosis on liver biopsy histology.
If FDA drug approval for NASH does not occur for many years, then perhaps efforts should be directed toward NASH disease prevention through public health measures
The U.S. Preventive Services Task Force is an independent volunteer panel of national experts in disease prevention and evidence-based medicine. The Task Force works “to improve the health of people nationwide by making evidence-based recommendations about clinical preventive services” [27]. They recently made the following statement:
“Diabetes is …associated with increased risks of cardiovascular disease, nonalcoholic fatty liver disease, and nonalcoholic steatohepatitis and was estimated to be the seventh leading cause of death in the US in 2017. Screening asymptomatic adults for prediabetes and type 2 diabetes may allow earlier detection, diagnosis, and treatment, with the ultimate goal of improving health outcomes” [28].
Specifically, the Task Force has now expanded discussions to include “nonalcoholic fatty liver disease” [28], as well as expanding the ages of screening for “prediabetes” and “type 2 diabetes” to adults ages 35 to 70 years old [29]. Of note, FDA has not yet recognized “prediabetes” as eligible for inclusion in an Indications for Use statement in a drug label.
Patient advocacy is key in this expanding recognition of fatty liver related disease and need for increased screening programs. Playing a leading role in these efforts is the Global Liver Institute, a 501(c) [3] non-profit organization based in Washington, DC [30], with the mission to “improve the lives of individuals and families impacted by liver disease through promoting innovation, encouraging collaboration, and scaling optimal approaches to help eradicate liver diseases” [30].
Early in 2021 and well prior to the Task Force expanding their recommendations:
“Global Liver Institute (GLI) and many of the leaders of the liver, diabetes and obesity advocacy community have submitted a formal letter and comments to the U.S. Preventive Services Task Force (USPSTF) urging the task force to mention the direct connection between diabetes and liver diseases, such as nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH), in their recommendations for type 2 diabetes (T2D) and prediabetes screening. The current Draft Recommendation Statement from USPSTF recommends screening adults ages 35 to 70 years who are overweight or obese for prediabetes and T2D but does not mention the strong link between T2D and chronic liver disease”[31, 32].
In parallel with these efforts, GLI has initiated an “U.S. NASH Action Plan”, with recommendations for medical societies and related groups involved in “NASH prevention and treatment, including patients and caregivers, clinicians, patient advocacy organizations, medical societies, industry, policymakers, regulators, health systems, and health insurance payers” [33]. These recommendations include:
-
Education: Develop and offer NASH-related medical school curricula.
-
Diagnosis: Convene a consensus conference to drive the acceleration of the adoption of noninvasive diagnostics and the simplification/streamlined version for integration into primary care and diverse (high-low resource) clinical settings.
-
Patient management/treatment: Collaborate with health systems on the development of meaningful quality measures for the diagnosis and management of NAFLD and NASH appropriate to each stage of disease.
-
Policy effort/legislation: Advocate for coverage/reimbursement coding changes and raise awareness of recent NASH coding changes that have occurred (International Classification of Diseases, Tenth Revision, Clinical Modification [ICD-10-CM] and Current Procedural Terminology [CPT]) [33].
If NASH specific drugs are not approved by FDA for years, then prevention efforts should be focused upon diet and exercise since these interventions in the placebo groups of certain NASH trials produced a response rate approaching 20%. Risk factor reduction such as weight loss, glucose control, LDL cholesterol lowering, as well as overall Cardiovascular (CV) risk reduction including tight blood pressure control, should be front and center on the public health agenda. These and related public health efforts that contribute to regulatory optimism for the future are outlined in Table 3.
Conclusions
Nonalcoholic fatty liver disease is a growing public health crisis, with phenotypes including NASH, which can progress to liver fibrosis and end stage cirrhosis and associated with an increased risk of cardiovascular disease and type 2 diabetes mellitus. There are still no U.S. FDA approved drugs or biological treatments for NASH or related liver diseases. Despite official agency guidance, the regulatory pathway to ultimate product approval remains unclear due to both the extrahepatic factors that contribute to NASH as well as the organizational structure of FDA, with its traditional separation of therapeutic indications within discrete review divisions. There is hope that continued evolution of the regulatory process will lead to the ability for clinical trial endpoints supporting NASH treatment approval to include both liver-based and traditional metabolic measures, independent of specific FDA division review. Meanwhile, public health efforts are moving forward which may improve the underlying causes of fatty liver disease and may prevent future causes of NASH and their resulting morbidity and mortality.
References
Ratziua V, Bellentanib S, Cortez-Pintoc H, Dayd C, Marchesinie G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J Hepatol. 2010;53:372–84. http://www.journal-of-hepatology.eu/article/S0168-8278(10)00414-9/fulltext.
Ekstedt M, Franzen LE, Mathiesen UL, Thorelius L, Holmqvist M, Bodemar G, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44:865–73. https://doi.org/10.1002/hep.21327/abstract;jsessionid=05BED8DE29EA91ADB17E9A321FEB71FC.f04t01.
Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363:1341–50. https://www.ncbi.nlm.nih.gov/pubmed/20879883.
Tomah S, Alkhouri N, Hamdy O. Nonalcoholic fatty liver disease and type 2 diabetes: where do Diabetologists stand? Clin Diabetes Endocrinol. 2020;6:9 https://doi.org/10.1186/s40842-020-00097-1.
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–57. https://doi.org/10.1002/hep.29367
Diehl AM, Day C. Cause, pathogenesis, and treatment of nonalcoholic steatohepatitis. N Engl J Med. 2017;377:2063–72. http://www.nejm.org/doi/abstract/10.1056/NEJMra1503519
U.S. Food & Drug Administration: News & Events. http://www.fda.gov/news-events/.
FDA Guidance Drug-Induced Liver Injury: Premarketing Clinical Evaluation July 2009. https://www.fda.gov/media/116737/download.
Sanyal A, Brunt EM, Kleiner DE, Kowdley K, Chalasani N, Lavine J, et al. Endpoints and clinical trial design for nonalcoholic steatohepatitis. Hepatology. 2011;54:344–53. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4014460/.
Noncirrhotic Nonalcoholic Steatohepatitis With Liver Fibrosis: Developing Drugs for Treatment Guidance for Industry (December 2018) Draft Guidance. https://www.fda.gov/media/119044/download.
Nonalcoholic Steatohepatitis with Compensated Cirrhosis: Developing Drugs for Treatment Guidance for Industry (June 2019) Draft Guidance https://www.fda.gov/media/127738/download.
Randomized Global Phase 3 Study to Evaluate the Impact on NASH With Fibrosis of Obeticholic Acid Treatment (REGENERATE) NCT02548351. https://clinicaltrials.gov/ct2/show/NCT02548351.
Ratziu V, Sanyal AJ, Loomba R, Rinella M, Harrison S, Anstee QM, et al. REGENERATE: Design of a pivotal, randomised, phase 3 study evaluating the safety and efficacy of obeticholic acid in patients with fibrosis due to nonalcoholic steatohepatitis. Contemp Clin Trials. 2019;84:105803 https://doi.org/10.1016/j.cct.2019.06.017.
Intercept Pharmaceuticals, Inc. Press Release June 29, 2020. https://ir.interceptpharma.com/news-releases/news-release-details/intercept-receives-complete-response-letter-fda-obeticholic-acid
Anania FA, Dimick-Santos L, Mehta R, Toerner J, Beitz J. Nonalcoholic steatohepatitis: current thinking from the division of hepatology and nutrition at the food and drug administration. Hepatology. 2020;73:2023–7. https://doi.org/10.1002/hep.31687.
Regulatory Perspectives for Development of Drugs for Treatment of NASH - 01/29/2021 - 01/29/2021 | FDA. www.fda.gov/drugs/news.
Guidance for Industry Diabetes Mellitus — Evaluating Cardiovascular Risk in New Antidiabetic Therapies to Treat Type 2 Diabetes (December 2008). https://www.fda.gov/media/71297/download
Type 2 Diabetes Mellitus: Evaluating the Safety of New Drugs for Improving Glycemic Control Guidance for Industry (March 2020). (https://www.fda.gov/media/135936/download.
Penson PE, Pirro M, Banach M. LDL-C: lower is better for longer—even at low risk. BMC Med. 2020;18:320–5. https://doi.org/10.1186/s12916-020-01792-7.
Reorganization of the Office of New Drugs with Corresponding Changes to the Office of Translational Sciences and the Office of Pharmaceutical Quality https://www.fda.gov/drugs/regulatory-science-research-and-education/reorganization-office-new-drugs-corresponding-changes-office-translational-sciences-and-office.
Office of Immunology and Inflammation - Division of Hepatology and Nutrition (DHN). https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/office-immunology-and-inflammation-division-hepatology-and-nutrition-dhn.
Division of Cardiology and Nephrology. https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/office-cardiology-hematology-endocrinology-and-nephrology-ochen-division-cardiology-and-nephrology.
Division of Diabetes, Lipid Disorders, and Obesity. https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/office-cardiology-hematology-endocrinology-and-nephrology-division-diabetes-lipid-disorders-and.
JARDIANCE® (empagliflozin tablets) Label Revision August 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/204629s026lbl.org.
FDA Jardiance Supplement Approval Letter (August 18, 2021) Norman Stockbridge. https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2021/204629Orig1s026ltr.pdf.
Patient-focused drug development (PFDD). https://www.fda.gov/drugs/development-approval-process-drugs/cder-patient-focused-drug-development.
U.S. Preventive Services Task Force https://www.uspreventiveservicestaskforce.org/uspstf/.
Screening for Prediabetes and Type 2 Diabetes US Preventive Services Task Force Recommendation Statement. JAMA. 2021;326:736–43. https://jamanetwork.com/journals/jama/fullarticle/2783414.
Screening for Prediabetes and Type 2 Diabetes August 24, 2021. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/screening-for-prediabetes-and-type-2-diabetes.
Global Liver Institute. https://www.globalliver.org/about.
USPSTF Must Include Link to Liver Disease in Recommendation on Screening for Diabetes. https://www.globalliver.org/news/2021/04/uspstf-must-include-link-to-liver-disease-in-recommendation-on-screening-for-diabetes.
Letter To USPSTF April 9, 2021. https://static1.squarespace.com/static/53bafd3ce4b0ae714af7153f/t/60759994a5a7834044a70c8b/1618319765042/Response+to+USPSTF+RE_+Diabetes+and+Prediabetes+Screening.pdf.
Patient-Driven Transformation is Key to NASH Clinical Trials August 25, 2021. https://www.globalliver.org/news/2021/nash-news-august.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Rights and permissions
About this article
Cite this article
Harvey, B.E. NASH: regulatory considerations for clinical drug development and U.S. FDA approval. Acta Pharmacol Sin 43, 1210–1214 (2022). https://doi.org/10.1038/s41401-021-00832-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-021-00832-z
Keywords
This article is cited by
-
Rotundic acid improves nonalcoholic steatohepatitis in mice by regulating glycolysis and the TLR4/AP1 signaling pathway
Lipids in Health and Disease (2023)
-
iTRAQ-based quantitative proteomics analysis of the effect of ACT001 on non-alcoholic steatohepatitis in mice
Scientific Reports (2023)
-
Age-related liver endothelial zonation triggers steatohepatitis by inactivating pericentral endothelium-derived C-kit
Nature Aging (2022)
-
All about NASH: disease biology, targets, and opportunities on the road to NASH drugs
Acta Pharmacologica Sinica (2022)