Abstract
Alcoholic liver disease (ALD) is one of the pathogenic factors of chronic liver disease with the highest clinical morbidity worldwide. Ursolic acid (UA), a pentacyclic terpenoid carboxylic acid, has shown many health benefits including antioxidative, anti-inflammatory, anticancer, and hepatoprotective activities. We previously found that UA was metabolized in vivo into epoxy-modified UA containing an epoxy electrophilic group and had the potential to react with nucleophilic groups. In this study we prepared an alkynyl-modified UA (AM-UA) probe for tracing and capturing the target protein of UA from liver in mice, then investigated the mode by which UA bound to its target in vivo. By conducting proteome identification and bioinformatics analysis, we identified caspase-3 (CASP3) as the primary target protein of UA associated with liver protection. Molecule docking analysis showed that the epoxy group of the UA metabolite reacted with Cys-163 of CASP3, forming a covalent bond with CASP3. The binding mode of the UA metabolites (UA, CM-UA, and EM-UA) was verified by biochemical evaluation, demonstrating that the epoxy group produced by metabolism played an important role in the inhibition of CASP3. In alcohol-treated HepG2 cells, pretreatment with the UA metabolite (10 μM) irreversibly inhibited CASP3 activities, and subsequently decreased the cleavage of PARP and cell apoptosis. Finally, pre-administration of UA (20–80 mg· kg−1 per day, ig, for 1 week) dose-dependently alleviated alcohol-induced liver injury in mice mainly via the inhibition of CASP3. In conclusion, this study demonstrates that UA is a valuable lead compound for the treatment of ALD.
Similar content being viewed by others
Introduction
Alcoholic liver disease (ALD) remains one of the most common causes of chronic liver disease worldwide [1]. Chronic excessive alcohol consumption induces a broad spectrum of hepatic injuries, the most characteristic of which is fatty liver. With continued alcohol consumption, ALD can lead to liver inflammation, fibrosis, cirrhosis, and even liver cancer [2]. The detailed mechanism of alcohol-induced liver injury is complicated. Emerging evidence suggests that alcohol metabolites and reactive oxygen species (ROS), which are generated by alcohol metabolism, play a key role in alcohol-induced liver injury. Alcohol metabolites and ROS trigger the apoptotic process in the liver through the induction of inflammatory cytokines and proapoptotic molecules [3, 4]. Clinical evidence suggests that hepatocellular apoptosis is an important pathological feature of ALD [5], and relieving dysregulated apoptosis in the liver represents a critical approach for the prevention and alleviation of ALD [6].
There is growing interest in the health benefits associated with the consumption of phytochemicals in fruits, vegetables, and herbs. Botanical preparations not only serve as nutrient supplements but are also used to prevent diseases [7]. Ursolic acid (UA) is a pentacyclic terpenoid carboxylic acid that is widely found in leaves, flowers, vegetables, and fruits [8]. In recent years, UA has become the subject of many publications because of its various activities and low toxicity. Many beneficial effects of UA, such as antioxidative, anti-inflammatory [9], anticancer, hepatoprotective, and cardiovascular protective effects, have been reported [10].
UA can be used alone or in combination with other hepatoprotective compounds, such as α-hederin, oleanolic acid, and uvaol, as an oral medication [11]. UA alleviates multiple factors that induce liver injury by acting against the hepatitis B and C viruses, exerting anti-inflammatory activity, inhibiting cytokine production, activating nuclear receptors, and scavenging free radicals [12, 13]. Binduja et al. demonstrated that UA has a significant protective effect in vitro against alcohol-induced toxicity in isolated rat hepatocytes [14]. Compared with silymarin, UA has better potency in rats with chronic ethanol-mediated liver injury [15]. The well-investigated effects of UA indicate that it has the potential to be developed as a therapeutic agent to prevent and alleviate ALD [16]. However, few studies have revealed the specific targets and molecular mechanisms by which UA protects the liver.
In this study, an alkynyl-modified UA (AM-UA) probe was prepared for tracing and capturing the target protein of UA in the liver in vivo. Subsequently, proteome identification, bioinformatics analysis, molecular docking, and biochemical evaluation were applied to verify the binding mode of the UA metabolite. The mechanisms by which UA targets CASP3 to alleviate alcohol-induced liver injury in vivo and in vitro were revealed.
Materials and methods
Reagents
UA (purity >98.5%, determined by HPLC), GSH and N,N-diisopropyl ethylamine (DIPEA, CAS: 7087-68-5) were purchased from Aladdin (Beijing, China). Sodium 1-((3-((4-azidophenyl) disulfanyl) propanoyl) oxy)-2,5-dioxopyrrolidine-3-sulfonate (Sulfo-SADP) was obtained from Bioworld (Tulare, MN, USA). Fe3O4 amino magnetic microspheres (MMs) were purchased from Tianjin Baseline Chromtech Research Center (Tianjin, China). Primary antibodies against CASP3 and PARP and secondary antibodies were obtained from Cell Signaling Technology (Beverly, MA, USA). Fluorescently labeled anti-rabbit IgG secondary antibodies were purchased from Abcam (Cambridge, UK). Chemiluminescent HRP substrates were obtained from Millipore Corporation (Billerica, MA, USA). All the reagents used for cell culture were purchased from Gibco BRL Life Technologies (Grand Island, NY, USA).
Cell culture
The HepG2 cell line, which is derived from human hepatoma cells, was cultured in Dulbecco’s modified Eagle’s medium supplemented with 10% fetal bovine serum. The cells were obtained from the American Type Culture Collection (Manassas, VA, USA) and incubated at 37 °C in a 5% CO2 atmosphere in a humidified incubator.
Animal experiments and sample preparation
Male Kunming mice (18–22 g) were purchased from the Experimental Animal Center of the National Institute for the Control of Pharmaceutical and Biological Products (Beijing, China, lot no. 0006407). The animals were housed in a suitable environment with ad libitum access to food and water. The mice were allowed to adjust to the housing environment for 3 days. Then, the mice were randomly divided into two groups (n = 6). The UA group (UA, 80 mg/kg daily) and the AM-UA group (the AM-UA probe was prepared as reported in our previous study [17], 80 mg/kg daily) were treated via gavage for 7 days. The animal experiments were approved by the Animal Ethics Committee, Guangxi University of Chinese Medicine (Nanning, China) and were performed in accordance with the guidelines of the national legislation of China. The protocols for mouse use and care described herein were approved (2019-DW20190930-11). Plasma sample collection, pretreatment, and detection protocols were performed as reported in our previous study [18].
Click chemistry reaction in the liver
The liver tissues of the UA- and AM-UA-treated mice were collected and fixed with 10% formalin. After fixation, the liver tissue sections were dehydrated, embedded in paraffin, and sectioned. The sections were dewaxed and rehydrated; then, the endogenous enzymes were inactivated, and antigen retrieval and blocking were performed according to the instructions of the Immunostain SP Kit (Tianjin Jiage, Tianjin, China). Then, the sections were incubated with click reaction solution (10 μM TMR azide fluorophore, 1 mM CuSO4, 1 mM TCEP, and 0.1 mM TBTA in distilled water) at 37 °C for 30 min. After washing the sections three times with PBST, fluorescence images were obtained with a confocal microscope (Carl Zeiss, Oberkochen, Germany). The excitation and emission wavelengths were 365 and 470 nm, respectively.
In-gel fluorescence imaging
Liver lysates from the UA- and AM-UA-treated mice were prepared according to the method described above. Subsequently, click reaction solution was added to the lysates and incubated for 30 min at 37 °C. The solution was centrifuged, and the unbound TMR azide fluorophore tracer was washed away with MeOH. Then, 0.2% SDS in PBS was added for 5 min at 65 °C to dissolve the pelleted protein, and the supernatants were collected for SDS-PAGE. For in-gel fluorescence imaging, the gels were scanned with a PXi9 multifunction imager (Syngene, MD, USA). The gels were stained with Coomassie blue to image total protein as a control.
Target fishing
The minced livers of the UA- and AM-UA-treated mice were homogenized with precooled RIPA lysis buffer (China COSCO, Beijing, China) at 4 °C. The lysates were centrifuged, and the protein contents of the supernatants were quantified with a BCA protein assay kit (Thermo Scientific, Waltham, MA, USA). Azide-modified functionalized MMs [17] and click reaction catalyst (1 mM CuSO4, 1 mM TCEP, and 0.1 mM TBTA in distilled water) were added to the lysates and incubated for 2 h at 37 °C. Then, the MMs were collected by magnetic separation and washed three times with precooled PBST. The bound proteins were released with 200 µL DTT (100 mM) at 4 °C for 30 min, and the supernatants were collected for SDS-PAGE. Enriched proteins on the SDS-PAGE gels were identified by Huada Gene Co., Ltd (Beijing, China).
Western blot analysis
Briefly, proteins were diluted with loading buffer, boiled, and loaded onto a gel for SDS-PAGE and Coomassie blue staining. The proteins were transferred from SDS-PAGE gels to PVDF membranes for Western blot analysis. After transfer, the membranes were blocked with 5% skim milk for 1 h and then incubated with CASP3 or PARP primary antibodies (1:1000) overnight at 4 °C to assess enriched protein and cleaved PARP levels. The membranes were washed with PBST three times and then incubated with secondary antibody (1:1000) at room temperature for 1 h. The membranes were washed, incubated with chemiluminescent HRP substrates, and exposed with a FluorChem E imager (ProteinSimple, Santa Clara, CA, USA).
Colocalization of the AM-UA probe with the target protein in the liver
The liver tissues of the mice treated with the AM-UA probe were sectioned and then incubated with the TMR azide fluorophore as described in section of “Click chemistry reaction in the liver”. Subsequently, the tissue sections were incubated with a CASP3 antibody (1:500) in 5% serum albumin at 4 °C overnight and washed three times with PBST. According to the instructions, the tissue sections were incubated with Alexa Fluor® 594-conjugated goat anti-rabbit antibody (1:1000) for 30 min and then washed three times with PBST. Fluorescence images were captured with a spectral-type LSM 700 confocal laser scanning microscope. The excitation and emission wavelengths for detecting the click reaction were 365 and 488 nm, respectively, while those for detecting immunofluorescence staining of the target protein were 490 and 617 nm, respectively.
Covalent binding of EM-UA with CASP3
The purified CASP3 protein (prepared as described in the Supplementary material, Supplementary Fig. S1) was incubated with or without EM-UA for 4 h at 37 °C, concentrated to 0.27 mg/mL and detected by UPLC-HDMS. The separated peptides were detected via MS with a full scan range of m/z 400−4000 in positive mode followed by ten data-dependent collision-induced dissociation MS/MS scans. An electrospray ionization voltage of 3.0 kV was applied directly to the LC buffer distal to the chromatography column using an ACQUITY UPLCr Protein BEH C4 column. The ion transfer tube temperature on the LTQ Velos ion trap was set to 300 °C.
Molecular docking
Three-dimensional structures of the CASP3 protein (PDB: 5IC4) were obtained from the Protein Data Bank (http://www.rcsb.org/pdb). The structure of the molecule and target protein were constructed and minimized using SYBYL software (Chemical Computing Group, Inc.). Then, Schrödinge_2018 software (Schrödinge, Inc.) was applied to evaluate covalent docking. The nucleophilic receptor was set to interact with all cysteines in the protein, and the reaction type was set as an epoxide opening reaction. The binding mode and reaction site were analyzed by PyMOL software (Schrödinge, Inc).
CASP3 enzyme activity assays
The purified CASP3 protein was incubated with different UA derivatives (10 μM), including UA, CM-UA and EM-UA, for 4 h. Then, the enzyme activity of CASP3 was measured by commercial CASP3 activity kits (Beyotime, Shanghai, China) according to the manufacturer’s instructions. The absorbance values were determined at 405 nm using a BioTek ELx800 microplate reader (BioTek Instruments, Inc. USA). CASP3 activity is expressed as the fold change compared to the control group.
Alcohol-induced HepG2 cell apoptosis
HepG2 cells were cultured in 6-well or 96-well plates. When the cells reached ~60% confluence, they were treated with UA, CM-UA, or EM-UA with or without varying concentrations of alcohol for 24 h. The viability of the cells in the 96-well plates were evaluated by the MTT assay (Shanghai Yuanye, Shanghai, China), and the cells in the 6-well plates were cultured with 0.5 mL RIPA lysis buffer for 30 min at 4 °C and collected with a cell scraper. The lysates were centrifuged, and the protein contents of the supernatants were quantified with a BCA protein assay kit. CASP3 activity and the fraction of cleaved PARP in the lysates were detected following a previously described method [17]. Apoptosis of these cells was measured using an Annexin V-FITC/PI Detection Kit (BD Biosciences, San Diego, CA, USA) and detected according to the manufacturer’s instructions.
Alcohol-induced liver injury in mice
The animals were randomly divided into six groups consisting of six mice each. The mice were administered 20, 40, or 80 mg/kg UA intragastrically (i.g.) once daily for 1 week. The mice in the control and model groups were administered the appropriate vehicle. One hour after UA administration on the 7th day, the animals were administered 25% (w/v) ethanol at a total accumulative dose of 6 g/kg body weight via four equal gavages at 20-min intervals. The control group received the same volume of water. Twelve hours after ethanol administration, all the mice were anesthetized with pentobarbital sodium (5 μg/g body weight), and serum and liver tissues were harvested for H&E staining, biochemical measurements, Western blot analysis, and enzymatic detection.
Statistical analysis
The results are expressed as the mean values ± SDs. Differences between two groups were analyzed by t-tests, and differences between multiple groups were analyzed by analysis of variance followed by Bonferroni’s test. A P value <0.05 was considered statistically significant.
Results
Molecular imaging and in-gel fluorescence imaging of UA in the liver
To explore the function of UA in relieving ALD, fluorescence imaging analysis of liver sections was carried out with an AM-UA probe. A schematic diagram of the experiment is shown in Fig. 1a. TMR azide, a fluorophore tracer, was click reacted with the AM-UA probe bound to liver tissue (Fig. 1b). Unlike the UA group, the AM-UA group exhibited clear pseudo-green fluorescence. This result suggested that the AM-UA probe can be used for in vivo tracing. Next, the liver lysates were pretreated with the TMR azide probe and visually detected by in-gel fluorescence imaging (Fig. 1c). Coomassie brilliant blue staining showed that the two test groups contained the same proteins. The in-gel fluorescence image suggested that some proteins in the liver were labeled with the AM-UA probe. The above results indicated that the AM-UA probe could be utilized for target fishing.
a The procedures used for fluorescence localization and target fishing of UA in the liver. b Fluorescence imaging analysis of liver sections. c Coomassie blue staining and in-gel fluorescence scanning were used to analyze proteins labeled with AM-UA. d Silver staining was used to detect the proteins enriched by AM-UA in the liver. e Functional analysis of the enriched proteins and the identified proteins related to liver injury. f Western blot analysis was used to detect CASP3 among the enriched proteins. The potential CASP3 bands in in-gel fluorescence images and silver staining images are labeled with red triangles. g The colocalization of CASP3 (pseudo-red) and the AM-UA probe (pseudo-green) in liver sections.
CASP3 was identified as a potential target of UA
To analyze the main targets of UA, AM-UA functionalized MMs were used to capture the potential targets in liver homogenates. The captured proteins were released by DDT reduction and subsequently analyzed via SDS-PAGE with sliver staining (Fig. 1d). The results of activity-based protein profiling showed that the enriched proteins in lane 3 of the AM-UA group were the main targets. Nevertheless, the intensity of the bands in the UA group (lane 2, negative control group) was low. To identify the potential target of UA, the captured proteins were then identified by Q-Exactive HF X. A scatter diagram was constructed from the ratio of the mass scores of the captured proteins in the AM-UA group to those of the captured proteins in the UA group (lane 3/lane 2). As shown in Fig. 1e, there were 201 eligible proteins in the AM-UA group and 16 significantly differentially expressed proteins (log2 > 2) in the AM-UA group compared to the UA group. The significantly differentially expressed proteins are shown in the supplemental material. Functional analysis of the differential proteins was performed by KEGG analysis. Subsequently, the CASP3 protein, which is associated with liver injury, was identified [19]. To further verify these results, Western blotting was performed to determine the most likely target of CASP3 enrichment. As expected, the approximately 32-kDa CASP3 protein band was enriched in the AM-UA group compared to that in the UA group (Fig. 1f), which is consistent with the target screening result, suggesting that AM-UA might label CASP3 in vivo.
To verify the results of our fishing strategy, the colocalization of CASP3 and AM-UA was investigated in liver sections. As shown in Fig. 1g, the pseudo-green fluorescence of the AM-UA probe was observed only in the AM-UA group, and unlabeled UA showed little fluorescence in the UA group. The distribution of CASP3 (stained pseudo-red with a Cy3 antibody) was observed in hepatocytes. After amplification, chemical imaging showed that AM-UA appeared to partially colocalize with the CASP3 protein in hepatocytes (pseudo-yellow). The above results indicated that CASP3 was the primary target protein of UA.
Epoxide metabolite of UA covalently bound with Cys-163 of CASP3
In our previous study, UA could be metabolized into epoxy-modified UA (EM-UA) in vivo, which contains electrophilic epoxy groups. EM-UA has the potential to react with nucleophilic groups, such as GSH and thiols (Fig. 2a) [17]. To test our hypothesis, we detected the secondary metabolite of EM-UA conjugated with GSH in the mouse serum after oral administration of UA. In the extracted ion chromatogram (Fig. 2b), EM-UA-GSH was eluted at 20.45 min and gave the parent ion at m/z = 779.4391, suggesting that the UA metabolite reacted with GSH.
a The metabolism of UA and its binding mode with its potential targets. b UPLC-Q-Tof was used to detect the reaction product of the UA metabolite and GSH in the mouse serum after the oral administration of UA. c UPLC-HDMS was used to detect the CASP3 protein. d UPLC-HDMS was used to detect the CASP3 protein after pretreatment with EM-UA. The mass information of the peptides labeled or unlabeled with EM-UA are displayed in red and blue, respectively.
To further analyze the binding mode of the UA metabolite with CASP3, EM-UA was incubated with purified CASP3 protein, and the reaction products were identified by UPLC-HDMS. The base peak intensity chromatograms (Fig. 2c) showed that several ions appeared after EM-UA was added, and among these peaks, the peak at 7.30 min was more evident than those in the control group. The mass spectral information of the peak indicated that two peptides containing Cys-163, 157LFIIQACEM-UAR164 (m/z = 962.5749) and 162ACEM-UARGTELDC170 (m/z = 967.4254), which were labeled with EM-UA, were detected with a mass increase of +474.37 Da (Fig. 2d). The results suggest that the epoxy group of the UA metabolite reacted with Cys-163 of CASP3 and formed a covalent bond with CASP3.
Epoxide metabolites of UA irreversibly inhibited the activity of CASP3
The active site of CASP3 is composed of four conserved loops, namely, loops 1–4, and the peptide sequence of loop 2 that covalently bonded with EM-UA is the same in both humans and mice (Fig. 3a). The above mass information indicated that the epoxy group of EM-UA formed a covalent bond with Cys-163, which is the catalytic cysteine residue of CASP3 [20]. To provide additional insights into the interaction between EM-UA and CASP3, we docked EM-UA to CASP3 (PDB: 5IC4) using Schrodinger_2018 software. The docking settings imitated the potential covalent binding poses of EM-UA with the Cys-163 residue of CASP3. In all cases, the top-scoring pose of EM-UA was displayed as a 3D map (Fig. 3b). The carboxyl group of EM-UA established hydrogen bonds with the active domain amino acids Arg-207 and Arg-64 of the S1 subsite [21]. In addition, EM-UA may also interact with His-121; the side chain of His-121 approached Cys-163 to participate in a catalytic reaction via a previously proposed Cys-His catalytic dyad hydrolysis mechanism [22]. The four residues that interact with EM-UA, Arg-64, His-121, Cys-163, and Arg-207, are conserved in humans and mice. UA may also interact with Cys-163, Arg-207, and His-121 in a noncovalent manner via carboxyl and hydroxyl groups [23]. However, the above results indicated that the covalent binding mode of the UA metabolite (EM-UA) to Cys-163 was more stable and suitable than that of UA to Cys-163.
a Sequence alignment of CASP3 in humans and mice. b Molecular modeling of CASP3 and EM-UA. PyMOL software was used to construct 3D maps of the covalent interaction between CASP3 (PDB: 5IC4) an EM-UA. EM-UA, and Cys-163 are displayed as sticks and colored according to atom type, with carbon atoms in gray and sulfur atoms in yellow; c the structures of UA, CM-UA, and EM-UA. d Effects of UA, CM-UA, and EM-UA on CASP3 activity. e Inhibition of CASP3 activity at 10 min from three independent experiments. Drugs were added at a concentration of 10 μM. Different superscripted letters indicate statistically significant differences among the groups (***P < 0.001 compared to the control group; +++P < 0.001 compared to UA group or CM-UA group).
To evaluate the effect of the epoxy group, we prepared EM-UA and carbonyl-modified UA (CM-UA), which is a derivative of EM-UA in which the epoxy group has been removed (Fig. 3c). As shown in Fig. 3d, e, the activity of CASP3 was decreased following the addition of UA, CM-UA, or EM-UA. However, the irreversible inhibitory effects of EM-UA through its covalent binding were much stronger than those of UA and CM-UA at the same dose. This result suggests that the epoxy group generated by UA metabolism plays an important role in the inhibitory effect of UA on CASP3.
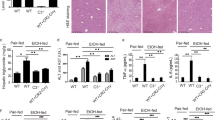
UA metabolite reduced alcohol-induced hepatocyte apoptosis
Hepatocellular apoptosis is an essential pathological feature of ALD. To verify the protective effect of UA against alcohol-induced injury via the inhibition of CASP3, we detected the effects of UA and its derivatives on HepG2 cells treated with alcohol for 24 h. As shown in Fig. 4a, alcohol decreased cell viability in a dose-dependent manner. However, cell viability was increased by UA, CM-UA, or EM-UA treatment. Next, the activation of CASP3 in HepG2 cells was measured. As shown in Fig. 4b, the activity of CASP3 significantly increased upon alcohol stimulation and decreased following the addition of UA, CM-UA, or EM-UA. PARP is a nuclear transcription protein that serves as the substrate of CASP3, and activation of CASP3 leads to cleavage of PARP. The cleavage of PARP was measured by Western blotting. As shown in Fig. 4c, the fraction of cleaved PARP in the cells was significantly increased in the alcohol-induced liver injury model group compared to the control group (P < 0.01). After treatment with UA derivatives, the fraction of cleaved PARP was considerably reduced (P < 0.01). Furthermore, EM-UA had a better inhibitory effect than UA or CM-UA (P < 0.05).
a HepG2 cells were stimulated with various concentrations of alcohol for 24 h and pretreated with or without 10 mM UA, CM-UA, or EM-UA for 6 h. Cell viability was measured by the MTT assay. b The activity of CASP3 was measured by an enzyme activity kit (n = 3). c Cleaved PARP was detected by Western blotting, and the relative intensity of cleaved PARP to that of total PARP is presented as the mean ± SD of three experiments. d Apoptotic cells were measured by flow cytometry, and the rate of apoptosis is presented as the mean ± SD of three experiments (##P < 0.01, ###P < 0.001 compared to the control group; **P < 0.01, ***P < 0.001 compared to the model group; +P < 0.05, ++P < 0.01 compared to the UA group or CM-UA group).
It is known that PARP plays an essential role in the regulation of apoptosis. The cleavage of PARP leads to DNA degradation and apoptosis. In our research, apoptotic cells were detected by flow cytometry following Annexin V-FITC and propidium iodide double labeling. As shown in Fig. 4d, the number of apoptotic cells was significantly increased upon alcohol stimulation and decreased upon UA, CM-UA, or EM-UA treatment. Treatment with EM-UA caused a more dramatic decrease in alcohol-induced death, CASP3 activation, PARP cleavage, and apoptosis of HepG2 cells than UA or CM-UA.
UA alleviated alcohol-induced liver injury in mice by targeting CASP3
To confirm the inhibitory effect of UA on CASP3 in vivo, a mouse model of alcohol-induced liver injury was examined. First, histopathological changes in the liver were analyzed (Fig. 5a). Liver samples from animals administered alcohol showed that the structure of the liver lobule was deformed, the arrangement of hepatocyte cords was disordered, and hepatocytes underwent edema and necrosis. Treatment with 20, 40, or 80 mg/kg UA or 120 mg/kg GSH reduced the degree of pathological liver changes, and the groups treated with these agents showed normal liver histology. Subsequently, ALT, AST, GGT, and SOD levels, which are indicators of liver injury, were also measured. As shown in Fig. 5b–d, compared with GSH treatment, alcohol stimulation increased the contents of ALT, AST, and GGT in the serum, but the contents of ALT, AST, and GGT in the serum were significantly decreased by treatment with UA in a dose-dependent manner. In addition, the content of SOD in liver lysates was decreased in the alcohol-induced liver injury model group compared to the control group and significantly increased in the UA and GSH treatment groups (Fig. 5e). These results indicated that UA could effectively alleviate alcohol-induced liver injury in mice. Then, the activation of CASP3 and cleavage of PARP in the liver lysates were measured. As shown in Fig. 5g, h, the activation of CASP3 and cleavage of PARP were increased in mice administered alcohol. However, the activation of CASP3 and cleavage of PARP were significantly decreased following treatment with UA or GSH. Treatment with UA was more effective in inhibiting the activation of CASP3 and cleavage of PARP at moderate and high doses than GSH (P < 0.05). The above results suggest that the hepatoprotective mechanisms of UA and GSH are different; UA alleviates alcohol-induced liver injury mainly via the inhibition of CASP3, which is consistent with the cell assay results presented above.
a Mice were administered alcohol and pretreated with or without GSH or UA. Histopathological changes in the liver were observed by H&E staining. The contents of ALT (b), AST (c), and GGT (d) in the serum and the content of SOD (e) in the liver were analyzed by ELISA kits (n = 6). f The activity of CASP3 in the liver was measured by an enzyme activity kit (n = 3). g The expression of cleaved PARP in the liver was measured by Western blotting, and the relative intensity of cleaved PARP to that of total PARP is presented as the mean ± SD of three experiments (##P < 0.01, ###P < 0.001 compared to the control group; *P < 0.01, **P < 0.01, ***P < 0.001 compared to the model group).
Discussion
The ability of alcohol consumption to induce apoptosis in a variety of tissues, especially the liver, has been widely recognized in rats, mice, and humans [24]. Hepatocyte apoptosis is an important pathogenesis of ALD and exacerbates inflammation, fibrosis, and cancer in the liver [2]. Alcohol administration can disturb the delicate balance between the pro- and antioxidant systems of organisms, leading to oxidative stress and ROS release [25]. ROS induce FasL expression and the release of cytochrome c from mitochondria, which associates in the cytosol with adenosine triphosphate, apoptosis-associated factor-1, and pro-CASP9 to form the apoptosome [26]. Apoptosome formation leads to the autocatalytic activation of CASP9, which then cleaves pro-CASP3 to generate active CASP3. Active CASP3 cleaves its enzyme substrate, PARP, and the cleavage of PARP leads to DNA degradation and apoptosis [27, 28]. Studies have found that the CASP3 inhibitors Ac-DEVD-FMK and zinc can decrease hepatocyte apoptosis and alleviate ALI via inhibition of CASP3 in mice [4].
Caspases are related cysteinyl proteinases that mediate critical steps in the apoptotic process. These enzymes are exquisitely specific molecular proteases that employ cysteinyl thiol groups as nucleophiles to catalyze the cleavage of peptide bonds containing an aspartic acid [22]. CASP3 is an effector caspase and leads to the fragmentation of nuclear DNA in cells during the apoptotic process [24]. CASP3 also participates in the MAPK signaling pathway and in the inflammatory response [29]. Excessive activation of CASP3 is closely associated with many disorders, such as myocardial infarction, alcoholic hepatitis, hepatitis B, Parkinson’s disease, and Alzheimer’s disease [30]. Our study demonstrates that the epoxide metabolite of UA acts as a ligand that targets and reacts with Cys-163 in the active domain of CASP3. Cys-163 is the catalytic cysteine of CASP3 and plays a key role in the catalysis of downstream molecules [20]. It was previously shown that the epoxide metabolite of UA irreversibly inhibits CASP3 via covalent binding with Cys-163 and subsequently decreases the cleavage of PARP, reduces death and apoptosis of hepatocytes, and alleviates the progression of alcohol-induced liver injury.
There are numerous natural electrophilic products that contain epoxide groups [31]. For example, fosfomycin intervenes at an early step in bacterial cell wall synthesis by inhibiting peptidoglycan synthesis. This inhibition takes place once the epoxide group of fosfomycin attacks Cys-115, the active site, to form a covalent linkage [32]. Fumagillin selectively inhibits angiogenesis through covalent binding of its epoxide group to a histidine residue near the active site of MetAP2 [33]. Our evidence shows that the epoxide group of the UA metabolite is electrophilic and plays a crucial role in the interaction of the metabolite with GSH and the thiol group of Cys-163 of CASP3 in vitro.
There are many nucleophilic residues in CASP3, and the key residue, Cys-163, contains a nucleophile group [20]. However, inhibitors of CASP3 mainly include peptides, quinolones, isatin sulfonamides, and metal ion inhibitors [34], which are all reversible. These inhibitors are efficacious in animal models of various human diseases, such as liver diseases, traumatic brain injury, myocardial infarction, and stroke [35,36,37]. In contrast, irreversible inhibitors have potential advantages in potency and selectivity. Wang et al. designed novel β-strand peptidomimetic irreversible inhibitors of CASP3, but because the enzyme substrates of CASP family proteins are similar, the inhibitors also act on CASP8 [38]. In our target fishing study, only the CASP3 subtype was enriched by AM-UA. We chose three analogs with the same skeleton, namely, UA, CM-UA, and EM-UA, and compared their protective effects. CASP3 activity analysis revealed that the irreversible inhibitory effects of EM-UA through covalent binding were significantly stronger than those of UA and CM-UA at the same dose. EM-UA also exerted a better hepatoprotective effect against alcohol-induced cell death than UA or CM-UA. These results indicate that a UA metabolite is a potential selective and irreversible CASP3 inhibitor for ALD treatment in vivo.
In our animal study, UA increased the serum content of SOD, which was oxidized by ROS in the mouse model of alcohol-induced liver injury. This result suggests that the antioxidative activity of UA is the mechanism by which it protects hepatocytes. Triterpenoid is an effective inducer of metallothionein, which is a small cysteine-rich protein that functions like glutathione to defend against toxic insults to the human body [39]. However, this phenomenon requires further verification.
In addition to protecting hepatocytes against alcohol-induced injury, UA also alleviates injuries caused by multiple factors. For example, UA regulates high glucose-induced apoptosis in U937 cells [40] and UV–VIS broad band radiation-induced apoptosis in retinal pigment epithelial cells [41]. Furthermore, UA enhanced the survival of cells and decreased the content of ROS and activity of CASP3 in our study. In animal studies, UA has been shown to reduce CASP3 activity and alleviate DNA damage and myocardial apoptosis in isoproterenol-induced myocardial infarction [42]. Yang et al. illustrated that UA decreases heat stress-induced apoptosis and the activities of cytochrome c and CASP3 in mouse cardiomyocytes and enhances the survival of mice [43]. There are many different mechanisms through which the release of ROS can be stimulated and the apoptotic pathway can be activated. The protective mechanism of UA described above may be consistent with the results of our study.
Currently, there is a concern surrounding the use of natural compounds or products as daily dietary supplements to prevent diseases. The brine shrimp test showed that UA has a low toxicity with an LC50 of 0.95 mg/mL, and 60 mg/kg UA is not toxic to rats based on the hippocratic test. Therefore, a daily administration of UA is safe and can lead to a reduced risk of diseases [44].
In summary, our findings suggest that UA reduced the cleavage of PARP, decreased death and apoptosis of hepatocytes, and alleviated alcohol-induced liver injury via irreversible inhibition of CASP3 in vivo. These results provide an enhanced understanding of UA, particularly its molecular mechanism of hepatoprotection, and demonstrate the potential of UA as a novel therapeutic for the treatment of ALD.
References
Louvetand A, Mathurin P. Alcoholic liver disease: mechanisms of injury and targeted treatment. Nat Rev Gastroenterol Hepatol. 2015;12:231–42.
Osna NA, Donohue TM, Kharbanda KK. Alcoholic liver disease: pathogenesis and current management. Alcohol Res. 2017;38:147–61.
An L, Wang X, Cederbaum A. Cytokines in alcoholic liver disease. Arch Toxicol. 2012;86:1337–48.
Zhou Z, Sun X, Kang YJ. Ethanol-induced apoptosis in mouse liver: Fas- and cytochrome c-mediated caspase-3 activation pathway. Am J Pathol. 2001;159:329–38.
Natori S, Rust C, Stadheim LM, Srinivasan A, Burgart LJ, Gores GJ. Hepatocyte apoptosis is a pathologic feature of human alcoholic hepatitis. J Hepatol. 2001;34:248–53.
Purohit V, Gao B, Song BJ. Molecular mechanisms of alcoholic fatty liver. Alcohol Clin Exp Res. 2018;33:191–205.
Liu RH. Health-promoting components of fruits and vegetables in the diet. Adv Nutr. 2013;4:384S–92S.
Shanmugam MK, Dai X, Kumar AP, Tan BK, Sethi G, Bishayee A. Ursolic acid in cancer prevention and treatment: molecular targets, pharmacokinetics and clinical studies. Biochem Pharm. 2013;85:1579–87.
Baek S, Lee J, Lee D, Park MK, Lee J, Kwok SK, et al. Ursolic acid ameliorates autoimmune arthritis via suppression of Th17 and B cell differentiation. Acta Pharmacol Sin. 2014;35:1177–87.
Cargninand ST, Gnoatto SB. Ursolic acid from apple pomace and traditional plants: a valuable triterpenoid with functional properties. Food Chem. 2017;220:477–89.
Liu J. Oleanolic acid and ursolic acid: research perspectives. J Ethnopharmacol. 2015;100:92–4.
Chen SR, Chen XP, Lu JJ, Wang Y, Wang YT. Potent natural products and herbal medicines for treating liver fibrosis. Chin Med. 2005;10:7.
Seo DY, Lee SR, Heo JW, No MH, Han J. Ursolic acid in health and disease. Korean J Physiol Pharmacol. 2018;22:235–48.
Saraswat B, Visen PKS, Agarwal DP. Ursolic acid isolated from Eucalyptus tereticornis protects against ethanol toxicity in isolated rat hepatocytes. Phytother Res. 2000;14:163–6.
Saravanan R, Viswanathan P, Pugalendi KV. Protective effect of ursolic acid on ethanol-mediated experimental liver damage in rats. Life Sci. 2006;78:713–8.
López Hortas L, Pérez Larrán P, González Muñoz MJ, Falqué E, Domínguez H. Recent developments on the extraction and application of ursolic acid: a review. Food Res Int. 2017;103:130–49.
Ma XY, Zhang Y, Wang ZY, Shen YB, Zhang M, Nie QD, et al. Ursolic acid, a natural nutraceutical agent, targets caspase3 and alleviates inflammation-associated downstream signal transduction. Mol Nutr Food Res. 2017;61:1700332.
Hu XY, Shen YB, Yang SN, Lei W, Cheng L, Hou YY, et al. Metabolite identification of ursolic acid in mouse plasma and urine after oral administration by ultra-high performance liquid chromatography/quadrupole time-of-flight mass spectrometry. RSC Adv. 2018;8:6532–9.
Xiang YW, Johnson EA, Zhang C, Huang GL, Hayes RL, Wang KKW, et al. Generation of aberrant forms of DFF40 concurrent with caspase-3 activation during acute and chronic liver injury in rats. Biochem Biophys Res Commun. 2006;350:457–62.
Fang B, Boross PI, Tozser J, Weber IT. Structural and kinetic analysis of caspase-3 reveals role for s5 binding site in substrate recognition. J Mol Biol. 2006;360:654–66.
Aşula MF, Onur IU, Yigit FU. Efficacy of fumagillin bicyclohexylamine on experimental corneal neovascularization in rat model. Int Ophthalmol. 2019;39:1553–8.
Becker J, Jennifer R, Soisson SM, Renee A, Christopher B, Sébastien F, et al. Reducing the peptidyl features of caspase-3 inhibitors: a structural analysis. J Med Chem. 2004;47:2466–74.
Feeney B, Pop C, Swartz P, Mattos C, Clark AC. Role of loop bundle hydrogen bonds in the maturation and activity of (Pro)caspase-3. Biochemistry. 2006;45:13249–63.
Nanji A. Apoptosis and alcoholic liver disease. Semin Liver Dis. 1998;18:187–90.
Castaneda F, Rosin-Steiner S. Low concentration of ethanol induce apoptosis in HepG2 cells: role of various signal transduction pathways. Int J Med Sci. 2006;3:160–7.
Tait SW, Green DR. Mitochondria and cell death: outer membrane permeabilization and beyond. Nat Rev Mol Cell Biol. 2010;11:621–32.
Decker P, Muller S. Modulating poly (ADP-ribose) polymerase activity: potential for the prevention and therapy of pathogenic situations involving DNA damage and oxidative stress. Curr Pharm Biotechnol. 2002;3:275–83.
Hengartner MO. The biochemistry of apoptosis. Nature. 2000;407:770–76.
Feoktistova M, Leverkus M. Programmed necrosis and necroptosis signalling. FEBS J. 2015;282:19–31.
Dassé E, Bridoux L, Baranek T, Lambert E, Salesse S, Sowa ML, et al. Tissue inhibitor of metalloproteinase-1 promotes hematopoietic differentiation via caspase-3 upstream the MEKK1/MEK6/p38α pathway. Leukemia. 2007;21:116–9.
Shafaghati L, Razaghi-Moghadam Z, Mohammadnejad J. A systems biology approach to understanding alcoholic liver disease molecular mechanism: the development of static and dynamic models. Bull Math Biol. 2017;79:2450–73.
Nomuraand DK, Maimone TJ. Target identification of bioactive covalently acting natural products. Curr Top Microbiol Immunol. 2019;420:351–74.
Lee H, Shin EA, Lee JH, Ahn D, Kim CG, Kim JH, et al. Caspase inhibitors: a review of recently patented compounds (2013-2015). Expert Opin Ther Pat. 2018;28:47–59.
Silver LL. Fosfomycin: Mechanism and resistance. Cold Spring Harb Perspect Med. 2017;7:a025262.
Baskin Bey ES, Washburn K, Feng S, Oltersdorf T, Shapiro D, Huyghe M, et al. Clinical trial of the pan-caspase inhibitor, IDN-6556, in human liver preservation injury. Am J Transpl. 2007;7:218–25.
Castro MM, Fuah J, Ali M, Sung M, Schulz J, Kondo MY, et al. Inhibitory effects of caspase inhibitors on the activity of matrix metalloproteinase-2. Biochem Pharmacol. 2013;86:469–75.
Han W, Sun YY, Wang XY, Zhu CL, Blomgren K. Delayed, long-term administration of the caspase inhibitor Q-VD-OPh reduced brain injury induced by neonatal hypoxia-ischemia. Dev Neurosci. 2014;36:64–72.
Wang ZG, Watt W, Brooks NA, Harris MS, Urban J, Boatman D, et al. Kinetic and structural characterization of caspase-3 and caspase-8 inhibition by a novel class of irreversible inhibitors. Biochim Biophys Acta. 2010;1804:1817–31.
Jeong HG, Kim HG, Hwang YP. Involvement of cytokines in the hepatic expression of metallothionein by ursolic acid. Toxicol Lett. 2005;155:369–76.
Chang JO, Kil IS, Park CI, Yang CH, Park JW. Ursolic acid regulates high glucose-induced apoptosis. Free Radic Res. 2007;41:638–44.
Lee YH, Wang E, Kumar N, Glickman RD. Ursolic acid differentially modulates apoptosis in skin melanoma and retinal pigment epithelial cells exposed to UV–VIS broadband radiation. Apoptosis. 2014;19:816–28.
Radhiga T, Rajamanickam C, Sundaresan A, Ezhumalai M, Pugalendi KV. Effect of ursolic acid treatment on apoptosis and DNA damage in isoproterenol-induced myocardial infarction. Biochimie. 2012;94:1135–42.
Yang Y, Li CW, Xiang X, Dai ZL, Chang JY, Zhang M, et al. Ursolic acid prevents endoplasmic reticulum stress-mediated apoptosis induced by heat stress in mouse cardiac myocytes. J Mol Cell Cardiol. 2014;67:103–11.
Somova LO, Nadar A, Rammanan P, Shode FO. Cardiovascular, antihyperlipidemic and antioxidant effects of oleanolic and ursolic acids in experimental hypertension. Phytomedicine. 2003;10:115–21.
Acknowledgements
This research was funded by a grant from the National Key R&D Program of China (No. 2018YFC1704500), Guangxi Innovation-driven Development 20 Special Foundation Project (Guike No. AA18118049), and Guangxi Collaborative Innovation Center for Functional Ingredients Study of Agricultural Residues (No. CICAR 2019-Z3).
Author information
Authors and Affiliations
Contributions
GB and YYH designed the study and drafted and edited the manuscript; XYM performed the experiments and acquired and analyzed the data; MZ and GF performed CASP3 protein purification; CJC analyzed the mass spectrum data; MKW performed the molecular dynamic simulation and docking experiments. MZ and YMH assisted with the experiments. XTH and EWH contributed to the data discussion and review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary information
Rights and permissions
About this article
Cite this article
Ma, Xy., Zhang, M., Fang, G. et al. Ursolic acid reduces hepatocellular apoptosis and alleviates alcohol-induced liver injury via irreversible inhibition of CASP3 in vivo. Acta Pharmacol Sin 42, 1101–1110 (2021). https://doi.org/10.1038/s41401-020-00534-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-020-00534-y