Abstract
Calcineurin inhibitors (CNIs), such as cyclosporine A and tacrolimus, are widely used immunosuppressive agents for the prevention of post-transplantation rejection and have improved 1-year graft survival rates by up to 90%. However, CNIs can induce severe reactions, such as acute or chronic allograft nephropathy, hypertension, and neurotoxicity. Because CNIs have varied bioavailabilities, narrow therapeutic ranges, and individual propensities for toxic effects, therapeutic drug monitoring is necessary for all CNIs. Identifying the genetic polymorphisms in drug-metabolizing enzymes will help to determine personalized dosage regimens for CNIs, as CNIs are substrates for CYP3A5 and P-glycoprotein (P-gp, MDR1). CNIs are often concomitantly administered with voriconazole or proton pump inhibitors (PPIs), giving rise to drug interaction problems. Voriconazole and PPIs can increase the blood concentrations of CNIs, and both are primarily metabolized by CYP2C19. Thus, it is expected that interactions between CNIs and voriconazole or PPI would be affected by CYP2C19 and CYP3A5 polymorphisms. CNI-induced acute kidney injury (AKI) is a serious complication of transplantations. Neutrophil gelatinase-associated lipocalin (NGAL) and kidney injury molecule 1 (KIM-1) are noninvasive urinary biomarkers that are believed to be highly sensitive to CNI-induced AKI. In this article, we review the adverse events and pharmacokinetics of CNIs and the biomarkers related to CNIs, including CYP3A5, CYP2C19, MDR1, NGAL, and KIM-1. We hope that these data will help to identify the optimal biomarkers for monitoring CNI-based immunosuppressive therapy after organ transplantation.
Similar content being viewed by others
Introduction
An organ transplantation is the best method for curing end-stage organ disease, especially in conjunction with the strong immunosuppressive abilities of calcineurin inhibitors (CNIs), such as cyclosporine A (CsA), which was discovered in the 1970s [1]. Subsequently, the more effective and less toxic CNI tacrolimus (TAC) was identified in the 1980s [2, 3], resulting in lower rejection rates and improving the short-term allograft survival rates. Current 1-year graft survival rates are ~90%, and acute rejection rates are below 20% [4,5,6].
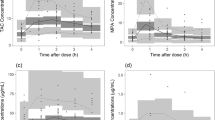
Due to the narrow therapeutic range and large inter-individual and intraindividual variability in the pharmacokinetics of CNIs, the therapeutic drug monitoring of CNIs is considered to be essential for patient management and determining individualized dosage adjustments for the prevention of post-transplant rejection. Despite the large variation in TAC pharmacokinetics, the area under the concentration-time curve (AUC) has a nearly linear relationship with the trough blood concentration among organ transplant patients [7, 8]. CNIs are substrates of P-glycoprotein (P-gp), CYP3A4, and CYP3A5, and therefore, these proteins represent potential pharmacokinetic factors that may help to determine the personalized dosage regimens for these drugs. The effects of single-nucleotide polymorphisms (SNPs) in the genes MDR1 (also known as ABCB1) and CYP3A5 on the pharmacokinetics of immunosuppressive drugs have been widely examined. CNIs can induce severe reactions, such as nephrotoxicity that can lead to renal dysfunction and the eventual need for a kidney transplant. Patients with TAC trough concentrations higher than 6 ng/mL have a significantly increased risk of developing adverse events following pediatric liver transplantations [9]. Therefore, genetic polymorphisms may affect CNI pharmacokinetics and affect the risks of experiencing adverse drug reactions. Because of these severe reactions, the long-term use of CNIs is not compatible with good survival. After 10 years, the graft survival rate remains at 50% after a deceased donation in the US and Europe, with approximately 30% of patients returning to dialysis, and 1 in 4 patients dying with a functional graft [10].
Although there are currently no biomarkers that can predict CNI-induced nephrotoxicity early, accurately, and noninvasively, some pharmacokinetic biomarkers, such as CYP3A5 and CYP2C19, and kidney damage markers, such as neutrophil gelatinase-associated lipocalin (NGAL) and kidney injury molecule 1 (KIM-1), can still be used to predict CNI-induced nephrotoxicity.
In this article, we review the adverse events and pharmacokinetics of CNIs and the biomarkers related to adverse drug reactions to CNI, including CYP3A5, CYP2C19, MDR1, NGAL, and KIM-1. We hope that this information will lead to the identification of the optimal biomarkers for monitoring CNI-based immunosuppressive therapy.
The immunosuppressive mechanism
CsA acts by binding to molecules of the cyclophilin family, with a high affinity for calcineurin, which is the key protein phosphatase for the activation of T cells. Calcineurin is a serine/threonine phosphatase that is widely distributed in mammalian tissues and is able to sense Ca2+ through its activation by calmodulin. TAC is a macrolide, containing a 23-membered lactone ring, whose mechanism of action is similar to that of CsA. TAC becomes biologically active only after forming a complex with the cytosolic FK-binding protein (FKBP). Several FKBP family members, such as FKBP12, FKBP12.6, and FKBP51, are expressed in T cells. However, no pharmacological effect of TAC was observed in T cells derived from FKBP12-deficient mice [11]. CNIs prevent the dephosphorylation of nuclear factor of activated T cells (NFAT) proteins by binding to cytosolic immunophilins (cyclophilin A and FKBP12), which, in turn, bind to and inhibit calcineurin, which inhibits NFAT activity [12, 13]. An NFAT has two subunits, one of which is confined to the cytoplasm, while the other has a predominantly nuclear localization. In resting T cells, NFAT proteins are hyperphosphorylated and are retained in the cytosol. The activation of T-cell receptors activates calcineurin, which dephosphorylates NFAT, allowing for its translocation to the nucleus, where it activates the expression of a range of genes [14]. The calcineurin–NFAT pathway was initially described in T cells, where NFAT acts as a master regulator of lymphocyte development and the expression of pro-inflammatory cytokines, such as interleukin (IL)-2, IL-3, IL-4, IFN-γ, and TNF-α. The classic calcineurin-NFAT signaling pathway can be described as follows. When receptors accept an antigen, phospholipase C-γ is activated and hydrolyzes phosphatidylinositol-4,5-bisphosphate into inositol-1,4,5-trisphosphate (IP3) and diacylglycerol. Next, IP3 binds to specific receptors on the endoplasmic reticulum and drives Ca2+ release from the endoplasmic reticulum into the cytoplasm, which triggers the opening of Ca2+ release-activated Ca2+ channels. As a result of the increased intracellular Ca2+ levels, the calcineurin enzyme becomes active and dephosphorylates NFAT, allowing for the translocation of NFAT into the nucleus and the subsequent regulation of gene expression [15]. NFAT signaling was later identified in other immune cells, including B cells, dendritic cells, and megakaryocytes [16, 17]. CNIs have therefore been regarded as inhibitors of immune-cell functions. TAC and CsA limit the immune response through the inhibition of calcineurin activity, using similar but slightly different mechanisms. In vitro, the pharmacological effect of TAC was approximately 100-fold greater than that of CsA [18]. According to the maximum effect model, the population mean estimates of the blood concentrations that yield a half-maximal effect (EC50) for TAC and CsA were 26.4 and 200 ng/mL, respectively [19]. Although FKBP12 is the only known drug target in T cells that mediates the pharmacological actions of TAC [11], the results of Xu et al. suggest that TAC may have one or more unknown molecular mechanism(s) that reduce immunological activity, which are distinct from the classical calcineurin inhibitory pathway.
Adverse effects
All adverse events and adverse drug reactions were coded using the coding system described in the Medical Dictionary for Regulatory Activities (MedDRA 21.0, March 2018).
Acute kidney injury
The characteristic feature of acute CNI nephrotoxicity is reversible tubular dysfunction [20]. Several studies have indicated that vascular dysfunction results from the upregulation of vasoconstrictor factors, including endothelin and thromboxane, the activation of the renin-angiotensin system (RAS), and the downregulation of vasodilating factors, such as prostacyclin, prostaglandin E2, and nitric oxide [21, 22]. CNIs can activate the RAS through both direct effects on juxtaglomerular cells [23] and indirect effects related to hemodynamic changes in the renal vasculature (arteriolar vasoconstriction), leading to the downregulation of vasodilating factors and the upregulation of endothelin [24]. Moreover, CNIs also augment the vasoconstricting effects of angiotensin II in smooth muscle cells by influencing intracellular calcium stores and smooth-muscle cell phenotypic maintenance and contractility [25]. In addition, CsA induces imbalances in the vasodilator/vasoconstrictor ratio of arachidonic acid metabolites (eicosanoids), which ultimately promotes renal vasoconstriction. In addition, the inhibition of calcineurin–NFAT signaling by CNIs inhibits COX-2, which promotes renal vasoconstriction and reduces the glomerular filtration rate [26, 27]. Because this vasoconstriction is dose-dependent and reversible, the withdrawal of CNIs is sufficient to cure this nephrotoxicity [28, 29].
Chronic allograft nephropathy
Chronic CNI nephrotoxicity is a more serious problem. In 1984, Myers et al. were the first to demonstrate chronic CNI nephrotoxicity after the long-term use of CsA. In heart transplant recipients, this nephrotoxicity was associated not only with a reversible decrease in the glomerular filtration rate but also with irreversible renal functional deterioration as a result of irreparable and progressive tubulointerstitial injury and glomerulosclerosis [30].
The initial phase (year 1) of the development of chronic allograft nephropathy is characterized by early tubulointerstitial damage from ischemic injury, prior to severe rejection, and subclinical rejection. These findings are present in 94.2% of patients [31].
Chronic CNI use not only contributes to late allograft loss but may also be the major cause of chronic renal allograft damage, which is characterized by the progressive and irreversible deterioration of renal function, in conjunction with interstitial fibrosis, tubular atrophy, arteriolar hyalinosis, and glomerulosclerosis [32].
The exact mechanism of nephrotoxicity induced by CNIs remains unknown. Tolou-Ghamari et al. [33] suggest that it may result from alterations in the production of vasoactive substances by mesangial and endothelial cells, which are contributing factors to decreased renal blood flow and glomerular thrombosis.
Hypertension
Given that CNIs can lead to vasoconstriction by many mechanisms, as mentioned above, hypertension is a common reaction to CNIs. The de novo development or aggravation of hypertension is common and can pose a significant hazard, both early and late, after all types of solid-organ transplantations. Hypertension can promote or aggravate cardiovascular risk factors, which are associated with poor long-term outcomes in patients [34, 35]. Opelz et al. [36] showed that a lower systolic blood pressure is associated with improved patient and graft survival.
Research has shown that TAC is associated with a slower reduction in cardiac output, lower systemic vascular resistance, and less rapid increases in arterial pressure and that hypertension significantly decreases when CsA is replaced with TAC [37,38,39,40].
Neurotoxicity
Neurotoxicity is a well-recognized adverse effect of CNIs, although the mechanism remains obscure. Although this reaction is uncommon and is often resolved after withdrawal, Chohan et al. [41] reported that CNI-induced neurotoxicity is frequently associated with a poor prognosis. Some studies have shown that mTOR treatment can recover neurological functions and can be combined with low doses of CNIs to prevent rejection [42, 43].
Efforts to achieve the maximal CNI dose reduction and the careful monitoring of CNI serum levels are important for the prevention of these irreversible changes. However, the administration of CNIs is complicated by variable pharmacokinetics, narrow therapeutic ranges, and individual sensitivities to toxic effects [44]. To help strike a balance between the immunosuppressive and toxic effects, identifying a good biomarker is key.
Biomarkers
SNPs and pharmacokinetics
CYP3A5
In general, drug–drug interactions involving CNIs occur most frequently when potent CYP3A4/5 inhibitors, such as macrolide antibiotics, azole antifungals, and calcium channel blockers, are combined with CYP3A4/5-metabolized CNIs. Because CYP3A5 is an important intestinal and hepatic enzyme for CNI metabolism, CYP3A5 polymorphisms are believed to be the primary cause for the interindividual variability in CNI pharmacokinetics and affect the risk of experiencing adverse drug reactions.
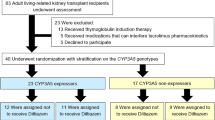
The presence of an SNP in intron 3 of CYP3A5, 6986A>G, results in the absence of a functional CYP3A5 protein in homozygous carriers (poor metabolizer phenotype). CYP3A5 has 2 alleles (*1 and *3), and patients can therefore be subdivided into three groups: CYP3A5*1/*1 (expressers), CYP3A5*1/*3 (expressers) and CYP3A5*3/*3 (nonexpressers). Nonexpressers are believed to have a higher bioavailability of (and exposure to) CNIs, in part due to increased intestinal absorption, and thus require lower doses to achieve the target concentration in comparison to expressers. Some studies have shown that expressers require approximately double the starting dose of CNIs, indicating that nonexpressers have an almost 2-fold higher trough level of CNIs than expressers [45,46,47]. However, the CYP3A5 polymorphism only appears to have a measurable effect on TAC therapy, and many studies have revealed that there is no relation between the CYP3A5 polymorphism and CsA activity [48,49,50].
In addition, many reports suggest that CYP3A5 is related to the mean concentration/dose ratio (C/D) of CNIs. Some researchers have reported that nonexpressers exhibit greater renal CNI metabolism; thus, even though nonexpressers require a lower initial dose, they have higher CNI blood concentrations and C/D values [51,52,53,54,55]. These results suggest that expressers experience the increased metabolic clearance of TAC and low trough concentrations, which results in a high incidence of acute rejection. Therefore, the *1 genotype may increase the risk of acute cellular rejection [54].
These findings are summarized in Table 1 [56, 57]. One hypothesis is that the polymorphism in the CYP3A5 gene affects the nephrotoxicity of TAC and acute rejection; however, because the mechanism of TAC-induced chronic allograft nephropathy is still unknown, and the definition of chronic allograft nephropathy varies across the world, studies in this area have not been consistent.
Kuypers et al. [58] found that CYP3A5*1 genotypes are significantly more frequently associated with the development of biopsy-proven TAC-related nephrotoxicity than are CYP3A5*3 genotypes. However, this result contradicts the findings of Chen et al. [51] and de Denus et al. [59], who found that nephrotoxicity was the greatest in the CYP3A5*3/*3 group. Queineh et al. [60] found that the CYP3A5 genetic polymorphism was not associated with TAC nephrotoxicity. Further research is required to elucidate these conflicting results.
CYP2C19
Because immunosuppressive agents reduce the activity of the immune system, transplant recipients have increased risks of infections. CNIs are often combined with an antifungal agent, such as voriconazole, to prevent fungal infections early after transplantation, thus introducing drug interaction problems. Many researchers have demonstrated that when a CNI is combined with voriconazole, the blood concentration of the CNI increases [61,62,63,64,65].
Voriconazole is a strong inhibitor of CYP3A4/5 [66] and is primarily metabolized by CYP2C19. Thus, it is expected that the interaction between CNIs and voriconazole may be affected by CYP2C19 polymorphisms, as the magnitude of CNI inhibition due to metabolism by CYP3A4/5 has been found to be dependent on the concentration of voriconazole, within a specific range, in human liver microsomes in vitro [62].
The gene CYP2C19 is located in chromosomal region 10q24.2 and consists of nine exons. CYP2C19 contains many SNPs, and its variants can be categorized into three groups, based on the ability to metabolize voriconazole: poor metabolizers (CYP2C19*2/*2, CYP2C19*3/*3, and CYP2C19*2/*3, PMs), intermediate metabolizers (CYP2C19*1/*2 and CYP2C19*1/*3, IMs) and extreme metabolizers (CYP2C19*1/*1, EMs). PMs and IMs experience 4- and 2-fold higher voriconazole exposure (AUC), respectively, than EMs; therefore, when a CNI is combined with voriconazole, CYP2C19 polymorphisms should be considered [66]. A few studies have indicated that the AUC0-24 of a CNI (primarily TAC) in IMs and PMs was significantly higher than that in EMs when the CNI is combined with voriconazole [66, 67].
Similar to voriconazole, proton pump inhibitors (PPIs) can affect the blood concentrations of CNIs through CYP2C19. In contrast to voriconazole, PPIs inhibit the metabolism of CNIs only in patients who carry variant alleles of CYP2C19 (EMs have the wild-type allele) because PPIs are metabolized by both CYP3A4/5 and CYP2C19. Therefore, CYP2C19 polymorphisms can also increase the blood concentrations of a CNI [68, 69]. The interactions between CNIs and voriconazole/PPIs is illustrated in Fig. 1.
Because the contribution of CYP2C19 to the metabolism of omeprazole is greater than that to lansoprazole and rabeprazole [70], some researchers have reported that the C/D ratios of CNIs co-administered with lansoprazole or rabeprazole were less strongly associated with CYP2C19 polymorphisms, although lansoprazole can increase the Cmax of TAC [71,72,73]. Overall, the blood concentration of CNIs that are co-administered with PPIs is higher in EMs and IMs than in PMs, especially for the co-administration of omeprazole [68, 74]. In addition, Chiu et al. [75] have reported that CYP2C19 polymorphisms do not affect the expression of CYP3A4*18, CYP3A5*3, or MDR1-3435 variants and, therefore, are independent factors.
MDR1/ABCB1
P-gp, the product of the ATP-binding cassette transporter gene (ABCB1; also known as MDR1), acts as an efflux transporter and decreases the blood concentration of CNIs [76]. The contributions of intestinal P-gp and/or CYP3A4 to CNI therapy are presented in Fig. 2. There are three factors that are believed to affect P-gp expression, which influences the blood concentration of CNIs: (1) the expression level of MDR1 mRNA; (2) MDR1 polymorphisms; and (3) MDR1 haplotype. In this article, we focus on the influence of MDR1 polymorphisms and the expression level of MDR1 mRNA on CNI effects.
The role of P-glycoprotein (P-gp; also known as MDR1 or ABCB1) and CYP3A4/5 in the enterohepatic processing of tacrolimus and cyclosporine A. Blue and green symbols represent the unchanged form and metabolite, respectively. (Adapted from the article by Masuda S. and Inui K. [2006], with permission from Elsevier.)
MDR1 has multiple polymorphisms; 1236C>T, 2677G>T/A, and 3435C>T were identified as better predictors of the blood concentration of CNIs than 1236C>T and 2677G>T/A [77, 78]. It has been reported that the 3435C>T polymorphism is associated with higher CNI concentrations [79,80,81,82], but many studies suggest that MDR1 polymorphisms (even 3435C>T) do not influence the CNI concentrations in Asian patients [47, 83,84,85,86,87]. Consequently, ethnicity may be a stronger factor affecting the association between the MDR1 polymorphisms and CNI concentrations in blood. Similarly, a meta-analysis of studies showed no significant effect of the 3435C>T polymorphism on the pharmacokinetics of digoxin [88]. The literature data are summarized in Tables 2–4 [89,90,91,92,93].
In contrast, studies have shown that the expression level of P-gp is strongly related to the trough levels of CNIs [47, 94, 95], and because the expression level of P-gp may depend on the expression level of MDR1 mRNA, the latter could be a useful biomarker for monitoring CNI therapy. Studies have shown that high expression levels of MDR1 mRNA are associated with a higher target concentration of TAC, a high risk of acute rejection, a lower C/D ratio of CNIs, and reduced survival rates [96,97,98]. All these data suggest that MDR1 mRNA is a good molecular marker for determining the oral dosage regimen of TAC. However, because studies on MDR1 mRNA in Caucasians are limited and there are no studies on MDR1 mRNA in relation to CsA, more research is required in this field.
Urinary biomarkers and nephrotoxicity
Kidney Disease Improving Global Outcomes defines acute kidney injury (AKI) as any of the following: (1) an increase in serum creatinine concentration of 0.3 mg/dL within 48 h; (2) an increase in the serum creatinine level of up to 1.5 times the baseline, which is known or presumed to have occurred within the previous 7 days; and (3) a urine volume of 0.5 mL/(kg·h) for 6 h. However, serum creatinine fails to be a sensitive and specific marker of renal injury [99]. In most cases, the signal is delayed and manifests when 70–80% of renal epithelial mass is already lost [100]. In addition, serum creatinine levels are affected by nonrenal factors, such as age, sex, body weight, muscle mass, total body volume, and protein intake [101].
Therefore, biomarkers that are more sensitive and specific for the prediction of renal function are required. There are many biomarkers used to predict renal function, including albumin, α-GST, α1-microglobulin, β2-microglobulin, clusterin, cysteine-rich protein, cystatin-C, exosomal fetuin-A, heart-type fatty acid-binding protein, hepatocyte growth factor, interleukin-18, liver-type fatty acid-binding protein, N-acetyl-β-glucosaminidase, netrin-1, osteopontin, retinol-binding protein, sodium/hydrogen exchanger isoform 3, NGAL, and KIM-1 [102]. Here, we will discuss two of these factors: NGAL and KIM-1.
CNIs cause structural damage to the straight segment of the proximal tubule and renal vasoconstriction, which is mediated by the renal sympathetic nervous system [20]. Therefore, biomarkers synthesized both in the proximal and distal tubules, such as NGAL and KIM-1, may be well associated with renal vasoconstriction and the interstitial fibrosis caused by CNI-induced nephrotoxicity. A summary of the available literature data on NGAL and KIM-1 is provided in Table 5 [103,104,105,106,107].
NGAL
NGAL is a small protein belonging to the lipocalin family [108,109,110]. This ubiquitous 25 kDa protein is secreted by various human tissues, including those of the gastrointestinal tract, respiratory tract, and kidneys, and because of its small molecular size, NGAL easily passes filtration and can be readily detected in urine [111]. When kidney function is essentially normal, the concentration of NGAL should be undetectable in the urine and serum; however, NGAL is rapidly induced in kidney tubule cells in response to ischemic injury [112]. The early appearance of NGAL in urine and serum is independent of the glomerular filtration rate but is highly predictive of a drop in this rate, which may happen up to several days later [109]. NGAL levels in urine and plasma may undergo a 100- to 10,000-fold concentration increase compared to normal levels in cases of renal injury [113]. Furthermore, NGAL was expressed during renal failure caused by ischemia-reperfusion injury in a mouse model [114]. A clinical study showed that NGAL staining contributed to the characterization of renal damage after kidney transplantation [115] and that NGAL could predict the development of AKI approximately 2 days before a rise in serum creatinine was observed [116].
One research group studied TAC-induced AKI in liver transplant patients and identified seven biomarkers, including monocyte chemotactic protein 1, liver-type fatty acid-binding protein, interleukin-18, osteopontin, cystatin-C, clusterin, and NGAL. This group showed that NGAL was superior to the other six urinary biomarkers, as high urinary levels of NGAL correlated with the probability of AKI [101].
Many studies have confirmed the sensitivity and specificity of urinary NGAL for the early diagnosis of AKI [109, 111, 112, 117], and NGAL not only has the potential to predict AKI but may also be a biomarker of chronic kidney disease, with high sensitivity and specificity, suggesting that NGAL is an early and accurate biomarker of renal function [112, 118].
KIM-1
KIM-1 is a type 1 transmembrane protein expressed in the proximal tubules that is cleaved from the surface of activated tubular cells and released into urine by a metalloproteinase. KIM-1 staining is detectable in proximal tubule epithelial cells and is sensitive to drugs and their metabolites [102, 113, 119]. The KIM-1 gene is located in human chromosomal region 5q33.2, and the KIM-1 protein is undetectable in healthy kidneys or in normal urine but is released into urine after proximal tubular kidney injury [120, 121]. A clinical study showed that urinary KIM-1 could predict the development of graft loss after kidney transplantation [122]. Therefore, KIM-1 has been consistently demonstrated to be an early indicator of kidney injury and is considered a highly sensitive and specific urinary biomarker for monitoring drug-induced kidney injury [123,124,125,126].
Studies have revealed that urinary KIM-1 protein concentrations are significantly higher in patients with AKI [123, 124], but increased KIM-1 expression can also be an early marker for identifying renal tubular damage. Nogare et al. [125] have reported that KIM-1 protein expression is increased in biopsies with interstitial fibrosis and tubular atrophy, implying that KIM-1 can serve as a biomarker of chronic kidney injury (CKI) induced by CNIs. Thus, KIM-1 expression is significantly related to kidney function, which makes KIM-1 a sensitive and specific marker of both AKI and CKI.
Conclusion
In summary, although CYP3A5, CYP2C19, and MDR1 can affect the CNI concentration, more information is available regarding CYP3A5 and CYP2C19 polymorphisms in relation to TAC, in the absence of differences in patient ethnicity. In contrast, MDR1 has a stronger relationship with ethnicity than CYP3A5 polymorphisms. NGAL and KIM-1 are sensitive and specific biomarkers of CNI toxicity, but other immunosuppressive drugs (e.g., everolimus) do not have similar biomarkers and will also induce toxicity; therefore, the identification of a more effective biomarker is required.
References
Borel JF, Feurer C, Gubler HU, Stahelin H. Biological effects of cyclosporin A: a new antilymphocytic agent. Agents Actions. 1976;6:468–75.
Kino T, Hatanaka H, Miyata S, Inamura N, Nishiyama M, Yajima T, et al. FK-506, a novel immunosuppressant isolated from a Streptomyces. II. Immunosuppressive effect of FK-506 in vitro. J Antibiot. 1987;40:1256–65.
Hatanaka H, Iwami M, Kino T, Goto T, Okuhara M. FR-900520 and FR-900523, novel immunosuppressants isolated from a Streptomyces. I. Taxonomy of the producing strain. J Antibiot. 1988;41:1586–91.
Shihab F, Christians U, Smith L, Wellen JR, Kaplan B. Focus on mTOR inhibitors and tacrolimus in renal transplantation: pharmacokinetics, exposure-response relationships, and clinical outcomes. Transpl Immunol. 2014;31:22–32.
Jia JJ, Lin BY, He JJ, Geng L, Kadel D, Wang L, et al. “Minimizing tacrolimus” strategy and long-term survival after liver transplantation. World J Gastroenterol. 2014;20:11363–9.
Helmschrott M, Beckendorf J, Akyol C, Ruhparwar A, Schmack B, Erbel C, et al. Superior rejection profile during the first 24 months after heart transplantation under tacrolimus as baseline immunosuppressive regimen. Drug Des Devel Ther. 2014;8:1307–14.
Venkataramanan R, Swaminathan A, Prasad T, Jain A, Zuckerman S, Warty V, et al. Clinical pharmacokinetics of tacrolimus. Clin Pharmacokinet. 1995;29:404–30.
Jusko WJ, Piekoszewski W, Klintmalm GB, Shaefer MS, Hebert MF, Piergies AA, et al. Pharmacokinetics of tacrolimus in liver transplant patients. Clin Pharmacol Ther. 1995;57:281–90.
Staatz CE, Taylor PJ, Lynch SV, Tett SE. A pharmacodynamic investigation of tacrolimus in pediatric liver transplantation. Liver Transpl. 2004;10:506–12.
Sommerer C, Suwelack B, Dragun D, Schenker P, Hauser IA, Nashan B, et al. Design and rationale of the ATHENA study - A 12-month, multicentre, prospective study evaluating the outcomes of a de novo everolimus-based regimen in combination with reduced cyclosporine or tacrolimus versus a standard regimen in kidney transplant patients: study protocol for a randomised controlled trial. Trials. 2016;17:92.
Xu X, Su B, Barndt RJ, Chen H, Xin H, Yan G, et al. FKBP12 is the only FK506 binding protein mediating T-cell inhibition by the immunosuppressant FK506. Transplantation. 2002;73:1835–8.
Liu J, Farmer JD Jr, Lane WS, Friedman J, Weissman I, Schreiber SL. Calcineurin is a common target of cyclophilin-cyclosporin A and FKBP-FK506 complexes. Cell. 1991;66:807–15.
Liu J, Albers MW, Wandless TJ, Luan S, Alberg DG, Belshaw PJ, et al. Inhibition of T cell signaling by immunophilin-ligand complexes correlates with loss of calcineurin phosphatase activity. Biochemistry. 1992;31:3896–901.
Schreiber SL, Crabtree GR. The mechanism of action of cyclosporin A and FK506. Immunol Today. 1992;13:136–42.
Hogan PG, Chen L, Nardone J, Rao A. Transcriptional regulation by calcium, calcineurin, and NFAT. Genes Dev. 2003;17:2205–32.
Macian F. NFAT proteins: key regulators of T-cell development and function. Nat Rev Immunol. 2005;5:472–84.
Muller MR, Rao A. NFAT, immunity and cancer: a transcription factor comes of age. Nat Rev Immunol. 2010;10:645–56.
Wasik M, Stepien-Sopniewska B, Lagodzinski Z, Gorski A. Effect of FK-506 and cyclosporine on human T and B lymphoproliferative responses. Immunopharmacology. 1990;20:57–61.
Fukudo M, Yano I, Masuda S, Fukatsu S, Katsura T, Ogura Y, et al. Pharmacodynamic analysis of tacrolimus and cyclosporine in living-donor liver transplant patients. Clin Pharmacol Ther. 2005;78:168–81.
Naesens M, Kuypers DR, Sarwal M. Calcineurin inhibitor nephrotoxicity. Clin J Am Soc Nephrol. 2009;4:481–508.
Bobadilla NA, Gamba G. New insights into the pathophysiology of cyclosporine nephrotoxicity: a role of aldosterone. Am J Physiol Ren Physiol. 2007;293:F2–9.
Burdmann EA, Andoh TF, Yu L, Bennett WM. Cyclosporine nephrotoxicity. Semin Nephrol. 2003;23:465–76.
Kurtz A, Della Bruna R, Kuhn K. Cyclosporine A enhances renin secretion and production in isolated juxtaglomerular cells. Kidney Int. 1988;33:947–53.
Ruster C, Wolf G. Renin-angiotensin-aldosterone system and progression of renal disease. J Am Soc Nephrol. 2006;17:2985–91.
Lassila M. Interaction of cyclosporine A and the renin-angiotensin system; new perspectives. Curr Drug Metab. 2002;3:61–71.
Hocherl K, Dreher F, Vitzthum H, Kohler J, Kurtz A. Cyclosporine A suppresses cyclooxygenase-2 expression in the rat kidney. J Am Soc Nephrol. 2002;13:2427–36.
Hocherl K, Kees F, Kramer BK, Kurtz A. Cyclosporine A attenuates the natriuretic action of loop diuretics by inhibition of renal COX-2 expression. Kidney Int. 2004;65:2071–80.
Andoh TF, Bennett WM. Chronic cyclosporine nephrotoxicity. Curr Opin Nephrol Hypertens. 1998;7:265–70.
Mihatsch MJ, Kyo M, Morozumi K, Yamaguchi Y, Nickeleit V, Ryffel B. The side-effects of ciclosporine-A and tacrolimus. Clin Nephrol. 1998;49:356–63.
Myers BD, Ross J, Newton L, Luetscher J, Perlroth M. Cyclosporine-associated chronic nephropathy. N Engl J Med. 1984;311:699–705.
Mathis AS, Egloff G, Ghin HL. Calcineurin inhibitor sparing strategies in renal transplantation, part one: late sparing strategies. World J Transplant. 2014;4:57–80.
Issa N, Kukla A, Ibrahim HN. Calcineurin inhibitor nephrotoxicity: a review and perspective of the evidence. Am J Nephrol. 2013;37:602–12.
Tolou-Ghamari Z. Nephro and neurotoxicity of calcineurin inhibitors and mechanisms of rejections: a review on tacrolimus and cyclosporin in organ transplantation. J Nephropathol. 2012;1:23–30.
Kim BR, Shin HS, Jung YS, Rim H. A case of tacrolimus-induced supraventricular arrhythmia after kidney transplantation. Sao Paulo Med J. 2013;131:205–7.
Dehghani SM, Haghighat M, Imanieh MH, Zahmatkeshan M, Borzooei M, Amoozegar H, et al. Tacrolimus related hypertrophic cardiomyopathy in liver transplant recipients. Arch Iran Med. 2010;13:116–9.
Opelz G, Dohler B. Improved long-term outcomes after renal transplantation associated with blood pressure control. Am J Transplant. 2005;5:2725–31.
Canzanello VJ, Textor SC, Taler SJ, Schwartz LL, Porayko MK, Wiesner RH, et al. Late hypertension after liver transplantation: a comparison of cyclosporine and tacrolimus (FK 506). Liver Transpl Surg. 1998;4:328–34.
Shihab FS, Waid TH, Conti DJ, Yang H, Holman MJ, Mulloy LC, et al. Conversion from cyclosporine to tacrolimus in patients at risk for chronic renal allograft failure: 60-month results of the CRAF Study. Transplantation. 2008;85:1261–9.
Textor SC, Wiesner R, Wilson DJ, Porayko M, Romero JC, Burnett JC Jr, et al. Systemic and renal hemodynamic differences between FK506 and cyclosporine in liver transplant recipients. Transplantation. 1993;55:1332–9.
Xue W, Zhang Q, Xu Y, Wang W, Zhang X, Hu X. Effects of tacrolimus and cyclosporine treatment on metabolic syndrome and cardiovascular risk factors after renal transplantation: a meta-analysis. Chin Med J. 2014;127:2376–81.
Chohan R, Vij R, Adkins D, Blum W, Brown R, Tomasson M, et al. Long-term outcomes of allogeneic stem cell transplant recipients after calcineurin inhibitor-induced neurotoxicity. Br J Haematol. 2003;123:110–3.
Bilbao I, Dopazo C, Castells L, Lazaro J, Caralt M, Sapisochin G, et al. Immunosuppression based on everolimus in liver transplant recipients with severe early post-transplantation neurotoxicity. Transplant Proc. 2014;46:3104–7.
Forgacs B, Merhav HJ, Lappin J, Mieles L. Successful conversion to rapamycin for calcineurin inhibitor-related neurotoxicity following liver transplantation. Transplant Proc. 2005;37:1912–4.
Krejci K, Tichy T, Hruby M, Horak P, Ciferska H, Horcicka V, et al. Subclinical toxicity of calcineurin inhibitors in repeated protocol biopsies: an independent risk factor for chronic kidney allograft damage. Transpl Int. 2010;23:364–73.
Nair SS, Sarasamma S, Gracious N, George J, Anish TS, Radhakrishnan R. Polymorphism of the CYP3A5 gene and its effect on tacrolimus blood level. Exp Clin Transplant. 2015;13:197–200.
Eng HS, Mohamed Z, Calne R, Lang CC, Mohd MA, Seet WT, et al. The influence of CYP3A gene polymorphisms on cyclosporine dose requirement in renal allograft recipients. Kidney Int. 2006;69:1858–64.
Goto M, Masuda S, Kiuchi T, Ogura Y, Oike F, Okuda M, et al. CYP3A5*1-carrying graft liver reduces the concentration/oral dose ratio of tacrolimus in recipients of living-donor liver transplantation. Pharmacogenetics. 2004;14:471–8.
Bouamar R, Hesselink DA, van Schaik RH, Weimar W, Macphee IA, de Fijter JW, et al. Polymorphisms in CYP3A5, CYP3A4, and ABCB1 are not associated with cyclosporine pharmacokinetics nor with cyclosporine clinical end points after renal transplantation. Ther Drug Monit. 2011;33:178–84.
Xin HW, Liu HM, Li YQ, Huang H, Zhang L, Yu AR, et al. Association of CYP3A4*18B and CYP3A5*3 polymorphism with cyclosporine-related liver injury in Chinese renal transplant recipients. Int J Clin Pharmacol Ther. 2014;52:497–503.
Jordan de Luna C, Herrero Cervera MJ, Sanchez Lazaro I, Almenar Bonet L, Poveda Andres JL, Alino Pellicer SF. Pharmacogenetic study of ABCB1 and CYP3A5 genes during the first year following heart transplantation regarding tacrolimus or cyclosporine levels. Transplant Proc. 2011;43:2241–3.
Chen JS, Li LS, Cheng DR, Ji SM, Sun QQ, Cheng Z, et al. Effect of CYP3A5 genotype on renal allograft recipients treated with tacrolimus. Transplant Proc. 2009;41:1557–61.
Wu S, Sun C, Tian D, Li Y, Gao X, He S, et al. Expression and clinical significances of Beclin1, LC3 and mTOR in colorectal cancer. Int J Clin Exp Pathol. 2015;8:3882–91.
Deininger KM, Vu A, Page RL 2nd, Ambardekar AV, Lindenfeld J, Aquilante CL. CYP3A pharmacogenetics and tacrolimus disposition in adult heart transplant recipients. Clin Transplant. 2016;30:1074–81.
Uesugi M, Kikuchi M, Shinke H, Omura T, Yonezawa A, Matsubara K, et al. Impact of cytochrome P450 3A5 polymorphism in graft livers on the frequency of acute cellular rejection in living-donor liver transplantation. Pharm Genom. 2014;24:356–66.
Uesugi M, Masuda S, Katsura T, Oike F, Takada Y, Inui K. Effect of intestinal CYP3A5 on postoperative tacrolimus trough levels in living-donor liver transplant recipients. Pharm Genom. 2006;16:119–27.
Lesche D, Sigurdardottir V, Setoud R, Oberhansli M, Carrel T, Fiedler GM, et al. CYP3A5*3 and POR*28 genetic variants influence the required dose of tacrolimus in heart transplant recipients. Ther Drug Monit. 2014;36:710–5.
Zheng H, Zeevi A, Schuetz E, Lamba J, McCurry K, Griffith BP, et al. Tacrolimus dosing in adult lung transplant patients is related to cytochrome P4503A5 gene polymorphism. J Clin Pharmacol. 2004;44:135–40.
Kuypers DR, de Jonge H, Naesens M, Lerut E, Verbeke K, Vanrenterghem Y. CYP3A5 and CYP3A4 but not MDR1 single-nucleotide polymorphisms determine long-term tacrolimus disposition and drug-related nephrotoxicity in renal recipients. Clin Pharmacol Ther. 2007;82:711–25.
de Denus S, Zakrzewski M, Barhdadi A, Leblanc MH, Racine N, Belanger F, et al. Association between renal function and CYP3A5 genotype in heart transplant recipients treated with calcineurin inhibitors. J Heart Lung Transplant. 2011;30:326–31.
Quteineh L, Verstuyft C, Furlan V, Durrbach A, Letierce A, Ferlicot S, et al. Influence of CYP3A5 genetic polymorphism on tacrolimus daily dose requirements and acute rejection in renal graft recipients. Basic Clin Pharmacol Toxicol. 2008;103:546–52.
Romero AJ, Le Pogamp P, Nilsson LG, Wood N. Effect of voriconazole on the pharmacokinetics of cyclosporine in renal transplant patients. Clin Pharmacol Ther. 2002;71:226–34.
Venkataramanan R, Zang S, Gayowski T, Singh N. Voriconazole inhibition of the metabolism of tacrolimus in a liver transplant recipient and in human liver microsomes. Antimicrob Agents Chemother. 2002;46:3091–3.
Zhang S, Pillai VC, Mada SR, Strom S, Venkataramanan R. Effect of voriconazole and other azole antifungal agents on CYP3A activity and metabolism of tacrolimus in human liver microsomes. Xenobiotica. 2012;42:409–16.
Kramer MR, Amital A, Fuks L, Shitrit D. Voriconazole and itraconazole in lung transplant recipients receiving tacrolimus (FK 506): efficacy and drug interaction. Clin Transplant. 2011;25:E163–7.
Chang HH, Lee NY, Ko WC, Lee HC, Yang YH, Wu CJ, et al. Voriconazole inhibition of tacrolimus metabolism in a kidney transplant recipient with fluconazole-resistant cryptococcal meningitis. Int J Infect Dis. 2010;14:e348–50.
Imamura CK, Furihata K, Okamoto S, Tanigawara Y. Impact of cytochrome P450 2C19 polymorphisms on the pharmacokinetics of tacrolimus when coadministered with voriconazole. J Clin Pharmacol. 2016;56:408–13.
Iwamoto T, Monma F, Fujieda A, Nakatani K, Gayle AA, Nobori T, et al. Effect of genetic polymorphism of CYP3A5 and CYP2C19 and concomitant use of voriconazole on blood tacrolimus concentration in patients receiving hematopoietic stem cell transplantation. Ther Drug Monit. 2015;37:581–8.
Hosohata K, Masuda S, Katsura T, Takada Y, Kaido T, Ogura Y, et al. Impact of intestinal CYP2C19 genotypes on the interaction between tacrolimus and omeprazole, but not lansoprazole, in adult living-donor liver transplant patients. Drug Metab Dispos. 2009;37:821–6.
Andersson T. Pharmacokinetics, metabolism and interactions of acid pump inhibitors. Focus on omeprazole, lansoprazole and pantoprazole. Clin Pharmacokinet. 1996;31:9–28.
Ishizaki T, Horai Y. Review article: cytochrome P450 and the metabolism of proton pump inhibitors--emphasis on rabeprazole. Aliment Pharmacol Ther. 1999;13:27–36.
Hosohata K, Masuda S, Yonezawa A, Sugimoto M, Takada Y, Kaido T, et al. Absence of influence of concomitant administration of rabeprazole on the pharmacokinetics of tacrolimus in adult living-donor liver transplant patients: a case-control study. Drug Metab Pharmacokinet. 2009;24:458–63.
Itagaki F, Homma M, Yuzawa K, Nishimura M, Naito S, Ueda N, et al. Effect of lansoprazole and rabeprazole on tacrolimus pharmacokinetics in healthy volunteers with CYP2C19 mutations. J Pharm Pharmacol. 2004;56:1055–9.
Miura M, Kagaya H, Tada H, Sagae Y, Satoh S, Habuchi T, et al. Comparison of enantioselective disposition of rabeprazole versus lansoprazole in renal-transplant recipients who are CYP2C19 extensive metabolizers. Xenobiotica. 2005;35:479–86.
Boso V, Herrero MJ, Bea S, Galiana M, Marrero P, Marques MR, et al. Increased hospital stay and allograft dysfunction in renal transplant recipients with Cyp2c19 AA variant in SNP rs4244285. Drug Metab Dispos. 2013;41:480–7.
Chiu KW, Hu TH, Nakano T, Chen KD, Lai CY, Hsu LW, et al. Biological interactions of CYP2C19 genotypes with CYP3A4*18, CYP3A5*3, and MDR1-3435 in living donor liver transplantation recipients. Transplant Res. 2013;2:6.
Stefanovic NZ, Cvetkovic TP, Jevtovic-Stoimenov TM, Ignjatovic AM, Paunovic GJ, Velickovic RM. Investigation of CYP 3A5 and ABCB1 gene polymorphisms in the long-term following renal transplantation: effects on tacrolimus exposure and kidney function. Exp Ther Med. 2015;10:1149–56.
Fathy M, Kamal M, Mohy A, Nabil A. Impact of CYP3A5 and MDR-1 gene polymorphisms on the dose and level of tacrolimus among living-donor liver transplanted patients: single center experience. Biomarkers. 2016;21:335–41.
Kravljaca M, Perovic V, Pravica V, Brkovic V, Milinkovic M, Lausevic M, et al. The importance of MDR1 gene polymorphisms for tacrolimus dosage. Eur J Pharm Sci. 2016;83:109–13.
Foote CJ, Greer W, Kiberd B, Fraser A, Lawen J, Nashan B, et al. Polymorphisms of multidrug resistance gene (MDR1) and cyclosporine absorption in de novo renal transplant patients. Transplantation. 2007;83:1380–4.
Isla Tejera B, Aumente Rubio MD, Martinez-Moreno J, Reyes Malia M, Arizon JM, Suarez Garcia A. Pharmacogenetic analysis of the absorption kinetics of cyclosporine in a population of Spanish cardiac transplant patients. Farm Hosp. 2009;33:324–9.
Yates CR, Zhang W, Song P, Li S, Gaber AO, Kotb M, et al. The effect of CYP3A5 and MDR1 polymorphic expression on cyclosporine oral disposition in renal transplant patients. J Clin Pharmacol. 2003;43:555–64.
Lopez-Montenegro Soria MA, Kanter Berga J, Beltran Catalan S, Milara Paya J, Pallardo Mateu LM, Jimenez Torres NV. Genetic polymorphisms and individualized tacrolimus dosing. Transplant Proc. 2010;42:3031–3.
Chowbay B, Cumaraswamy S, Cheung YB, Zhou Q, Lee EJ. Genetic polymorphisms in MDR1 and CYP3A4 genes in Asians and the influence of MDR1 haplotypes on cyclosporin disposition in heart transplant recipients. Pharmacogenetics. 2003;13:89–95.
Sun JY, Wang XG, Zou YG, Wang YP, Liang DR, Liang MZ, et al. Association of CYP3A5 and MDR1 genetic polymorphisms with the blood concentration of tacrolimus in Chinese liver and renal transplant recipients. Sichuan Da Xue Xue Bao Yi Xue Ban. 2013;44:573–7.
Kuzuya T, Kobayashi T, Moriyama N, Nagasaka T, Yokoyama I, Uchida K, et al. Amlodipine, but not MDR1 polymorphisms, alters the pharmacokinetics of cyclosporine A in Japanese kidney transplant recipients. Transplantation. 2003;76:865–8.
Hu YF, Qiu W, Liu ZQ, Zhu LJ, Tu JH, Wang D, et al. Effects of genetic polymorphisms of CYP3A4, CYP3A5 and MDR1 on cyclosporine pharmacokinetics after renal transplantation. Clin Exp Pharmacol Physiol. 2006;33:1093–8.
Goto M, Masuda S, Saito H, Uemoto S, Kiuchi T, Tanaka K, et al. C3435T polymorphism in the MDR1 gene affects the enterocyte expression level of CYP3A4 rather than Pgp in recipients of living-donor liver transplantation. Pharmacogenetics. 2002;12:451–7.
Chowbay B, Li H, David M, Cheung YB, Lee EJ. Meta-analysis of the influence of MDR1 C3435T polymorphism on digoxin pharmacokinetics and MDR1 gene expression. Br J Clin Pharmacol. 2005;60:159–71.
Anglicheau D, Thervet E, Etienne I, Hurault De Ligny B, Le Meur Y, Touchard G, et al. CYP3A5 and MDR1 genetic polymorphisms and cyclosporine pharmacokinetics after renal transplantation. Clin Pharmacol Ther. 2004;75:422–33.
Saracino A, Muscaridola N, Cifarelli RA, Stallone G, Grandaliano G, Santarsia G. Multidrug-resistance 1 gene single-nucleotide polymorphisms do not influence long-term graft survival after kidney transplantation. Transplant Proc. 2014;46:2214–9.
Mendes J, Martinho A, Simoes O, Mota A, Breitenfeld L, Pais L. Genetic polymorphisms in CYP3A5 and MDR1 genes and their correlations with plasma levels of tacrolimus and cyclosporine in renal transplant recipients. Transplant Proc. 2009;41:840–2.
Sharaki O, Zeid M, Moez P, Zakaria NH, Nassar E. Impact of CYP3A4 and MDR1 gene (G2677T) polymorphisms on dose requirement of the cyclosporine in renal transplant Egyptian recipients. Mol Biol Rep. 2015;42:105–17.
Mostafa-Hedeab G, Saber-Ayad MM, Latif IA, Elkashab SO, Elshaboney TH, Mostafa MI, et al. Functional G1199A ABCB1 polymorphism may have an effect on cyclosporine blood concentration in renal transplanted patients. J Clin Pharmacol. 2013;53:827–33.
Jin M, Shimada T, Shintani M, Yokogawa K, Nomura M, Miyamoto K. Long-term levothyroxine treatment decreases the oral bioavailability of cyclosporin A by inducing P-glycoprotein in small intestine. Drug Metab Pharmacokinet. 2005;20:324–30.
Masuda S, Uemoto S, Hashida T, Inomata Y, Tanaka K, Inui K. Effect of intestinal P-glycoprotein on daily tacrolimus trough level in a living-donor small bowel recipient. Clin Pharmacol Ther. 2000;68:98–103.
Goto M, Masuda S, Kiuchi T, Ogura Y, Oike F, Tanaka K, et al. Relation between mRNA expression level of multidrug resistance 1/ABCB1 in blood cells and required level of tacrolimus in pediatric living-donor liver transplantation. J Pharmacol Exp Ther. 2008;325:610–6.
Masuda S, Goto M, Fukatsu S, Uesugi M, Ogura Y, Oike F, et al. Intestinal MDR1/ABCB1 level at surgery as a risk factor of acute cellular rejection in living-donor liver transplant patients. Clin Pharmacol Ther. 2006;79:90–102.
Hashida T, Masuda S, Uemoto S, Saito H, Tanaka K, Inui K. Pharmacokinetic and prognostic significance of intestinal MDR1 expression in recipients of living-donor liver transplantation. Clin Pharmacol Ther. 2001;69:308–16.
Vaidya VS, Waikar SS, Ferguson MA, Collings FB, Sunderland K, Gioules C, et al. Urinary biomarkers for sensitive and specific detection of acute kidney injury in humans. Clin Transl Sci. 2008;1:200–8.
Sieber M, Hoffmann D, Adler M, Vaidya VS, Clement M, Bonventre JV, et al. Comparative analysis of novel noninvasive renal biomarkers and metabonomic changes in a rat model of gentamicin nephrotoxicity. Toxicol Sci. 2009;109:336–49.
Tsuchimoto A, Shinke H, Uesugi M, Kikuchi M, Hashimoto E, Sato T, et al. Urinary neutrophil gelatinase-associated lipocalin: a useful biomarker for tacrolimus-induced acute kidney injury in liver transplant patients. PLoS ONE. 2014;9:e110527.
Bonventre JV, Vaidya VS, Schmouder R, Feig P, Dieterle F. Next-generation biomarkers for detecting kidney toxicity. Nat Biotechnol. 2010;28:436–40.
Gustafsson F, Gude E, Sigurdardottir V, Aukrust P, Solbu D, Goetze JP, et al. Plasma NGAL and glomerular filtration rate in cardiac transplant recipients treated with standard or reduced calcineurin inhibitor levels. Biomark Med. 2014;8:239–45.
Field M, Lowe D, Cobbold M, Higgins R, Briggs D, Inston N, et al. The use of NGAL and IP-10 in the prediction of early acute rejection in highly sensitized patients following HLA-incompatible renal transplantation. Transpl Int. 2014;27:362–70.
Dedeoglu B, de Geus HR, Fortrie G, Betjes MG. Novel biomarkers for the prediction of acute kidney injury in patients undergoing liver transplantation. Biomark Med. 2013;7:947–57.
Jin ZK, Tian PX, Wang XZ, Xue WJ, Ding XM, Zheng J, et al. Kidney injury molecule-1 and osteopontin: new markers for prediction of early kidney transplant rejection. Mol Immunol. 2013;54:457–64.
Yadav B, Prasad N, Agrawal V, Jaiswal A, Rai M, Sharma R, et al. Urinary Kidney injury molecule-1 can predict delayed graft function in living donor renal allograft recipients. Nephrology. 2015;20:801–6.
Bolignano D, Lacquaniti A, Coppolino G, Donato V, Fazio MR, Nicocia G, et al. Neutrophil gelatinase-associated lipocalin as an early biomarker of nephropathy in diabetic patients. Kidney Blood Press Res. 2009;32:91–8.
Mishra J, Dent C, Tarabishi R, Mitsnefes MM, Ma Q, Kelly C, et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005;365:1231–8.
Mishra J, Ma Q, Prada A, Mitsnefes M, Zahedi K, Yang J, et al. Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J Am Soc Nephrol. 2003;14:2534–43.
Wasilewska A, Zoch-Zwierz W, Taranta-Janusz K, Michaluk-Skutnik J. Neutrophil gelatinase-associated lipocalin (NGAL): a new marker of cyclosporine nephrotoxicity? Pediatr Nephrol. 2010;25:889–97.
Cantaluppi V, Dellepiane S, Tamagnone M, Medica D, Figliolini F, Messina M, et al. Neutrophil gelatinase associated lipocalin is an early and accurate biomarker of graft function and tissue regeneration in kidney transplantation from extended criteria donors. PLoS ONE. 2015;10:e0129279.
Sereno J, Vala H, Nunes S, Rocha-Pereira P, Carvalho E, Alves R, et al. Cyclosporine A-induced nephrotoxicity is ameliorated by dose reduction and conversion to sirolimus in the rat. J Physiol Pharmacol. 2015;66:285–99.
Mori K, Lee HT, Rapoport D, Drexler IR, Foster K, Yang J, et al. Endocytic delivery of lipocalin-siderophore-iron complex rescues the kidney from ischemia-reperfusion injury. J Clin Invest. 2005;115:610–21.
Mishra J, Ma Q, Kelly C, Mitsnefes M, Mori K, Barasch J, et al. Kidney NGAL is a novel early marker of acute injury following transplantation. Pediatr Nephrol. 2006;21:856–63.
Zappitelli M, Washburn KK, Arikan AA, Loftis L, Ma Q, Devarajan P, et al. Urine neutrophil gelatinase-associated lipocalin is an early marker of acute kidney injury in critically ill children: a prospective cohort study. Crit Care. 2007;11:R84.
Nickolas TL, O’Rourke MJ, Yang J, Sise ME, Canetta PA, Barasch N, et al. Sensitivity and specificity of a single emergency department measurement of urinary neutrophil gelatinase–associated lipocalin for diagnosing acute kidney injury. Ann Intern Med. 2008;148:810–9.
Malyszko J, Malyszko JS, Bachorzewska-Gajewska H, Poniatowski B, Dobrzycki S, Mysliwiec M. Neutrophil gelatinase-associated lipocalin is a new and sensitive marker of kidney function in chronic kidney disease patients and renal allograft recipients. Transplant Proc. 2009;41:158–61.
Ichimura T, Bonventre JV, Bailly V, Wei H, Hession CA, Cate RL, et al. Kidney injury molecule-1 (KIM-1), a putative epithelial cell adhesion molecule containing a novel immunoglobulin domain, is up-regulated in renal cells after injury. J Biol Chem. 1998;273:4135–42.
Carlos CP, Sonehara NM, Oliani SM, Burdmann EA. Predictive usefulness of urinary biomarkers for the identification of cyclosporine A-induced nephrotoxicity in a rat model. PLoS ONE. 2014;9:e103660.
Monney L, Sabatos CA, Gaglia JL, Ryu A, Waldner H, Chernova T, et al. Th1-specific cell surface protein Tim-3 regulates macrophage activation and severity of an autoimmune disease. Nature. 2002;415:536–41.
van Timmeren MM, Vaidya VS, van Ree RM, Oterdoom LH, de Vries AP, Gans RO, et al. High urinary excretion of kidney injury molecule-1 is an independent predictor of graft loss in renal transplant recipients. Transplantation. 2007;84:1625–30.
Malyszko J, Koc-Zorawska E, Malyszko JS, Mysliwiec M. Kidney injury molecule-1 correlates with kidney function in renal allograft recipients. Transplant Proc. 2010;42:3957–9.
Cosner D, Zeng X, Zhang PL. Proximal tubular injury in medullary rays is an early sign of acute tacrolimus nephrotoxicity. J Transplant. 2015;2015:142521.
Nogare AL, Veronese FV, Carpio VN, Montenegro RM, Pedroso JA, Pegas KL, et al. Kidney injury molecule-1 expression in human kidney transplants with interstitial fibrosis and tubular atrophy. BMC Nephrol. 2015;16:19.
Shinke H, Masuda S, Togashi Y, Ikemi Y, Ozawa A, Sato T, et al. Urinary kidney injury molecule-1 and monocyte chemotactic protein-1 are noninvasive biomarkers of cisplatin-induced nephrotoxicity in lung cancer patients. Cancer Chemother Pharmacol. 2015;76:989–96.
Acknowledgements
This work was supported in part by a Grant-in-Aid for Scientific Research (KAKENHI) from the Ministry of Education, Science, Culture, Sports, and Technology of Japan (MEXT) (grant numbers: 15H04666 and 18H02588 to Satohiro Masuda, 16K08404 to Hiroyuki Watanabe, 17K08953 to Nobuaki Egashira, and 18K06786 to Soichiro Tajima).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fu, R., Tajima, S., Suetsugu, K. et al. Biomarkers for individualized dosage adjustments in immunosuppressive therapy using calcineurin inhibitors after organ transplantation. Acta Pharmacol Sin 40, 151–159 (2019). https://doi.org/10.1038/s41401-018-0070-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-018-0070-2
Keywords
This article is cited by
-
Cyclosporine A-related neurotoxicity after haploidentical hematopoietic stem cell transplantation in children with hematopathy
Italian Journal of Pediatrics (2021)