Abstract
There is increasing interest in individualizing treatment selection for more than 25 regulatory approved treatments for major depressive disorder (MDD). Despite an inconclusive efficacy evidence base, antidepressants (ADs) are prescribed for the depressive phase of bipolar disorder (BD) with oftentimes, an inadequate treatment response and or clinical concern for mood destabilization. This study explored the relationship between antidepressant response in MDD and antidepressant-associated treatment emergent mania (TEM) in BD. We conducted a genome-wide association study (GWAS) and polygenic score analysis of TEM and tested its association in a subset of BD-type I patients treated with SSRIs or SNRIs. Our results did not identify any genome-wide significant variants although, we found that a higher polygenic score (PGS) for antidepressant response in MDD was associated with higher odds of TEM in BD. Future studies with larger transdiagnostic depressed cohorts treated with antidepressants are encouraged to identify a neurobiological mechanism associated with a spectrum of depression improvement from response to emergent mania.
Similar content being viewed by others
Introduction
While there is a substantial evidence base for antidepressants (ADs) in major depressive disorder (MDD), the therapeutic benefit in bipolar disorder (BD) is far from conclusive [1]. The use of ADs, particularly in BD type I, remains controversial mainly due to a lack of consistent evidence for efficacy and potential concern for mood destabilization [2]. Data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) showed that up to 40% of participants self-reported manic or hypomanic symptoms with ADs [3]. As recent data has suggested an increase in prescription rates of AD monotherapy in BD [4], there is an urgent need to identify clinical correlates or biomarkers of treatment non-response and/or adverse drug-related events, especially AD associated treatment-emergent mania (TEM) [5].
Genome-wide association studies (GWAS) have identified many genetic variants associated with BD [6] and a potential overlap in the biological pathways with MDD [7]; however, in many cases sample sizes may still remain too small to be able to detect significant variants associated with disease or treatment response. Additionally, there has been increasing evidence that would suggest a genetic overlap between MDD, BD and schizophrenia symptoms [8]. Polygenic scores (PGS) have become frequently used to examine how an individual’s genetic loading, computed from a combination of genetic variants, could predict risk to disease or clinical outcomes [9]. Specifically, a PGS is a weighted sum of a person’s alleles, creating a metric score used for risk quantification [10], diagnosis [11], or treatment response prediction [12, 13]. For example, studies focusing on treatment response have shown that a high genetic loading for schizophrenia or MDD in people with BD will decrease their response to lithium [14, 15].
In this study, our aim was to identify genetic factors associated with AD associated TEM in BD individuals and to explore a potential genetic overlap of AD response in MDD and TEM in BD.
Methods
Study population
Clinical and genomic data of adult patients with a BD diagnosis, prior AD treatment, and assessment of history of TEM were extracted from the Mayo Clinic Bipolar Biobank. The Biobank was established with the aim of building a repository that would facilitate studies on disease risk and pharmacogenomic treatment outcomes [16]. Enrollment sites included: Mayo Clinic (Rochester, Minnesota), Lindner Center of HOPE/University of Cincinnati College of Medicine (Cincinnati, Ohio), University of Minnesota (Minneapolis, Minnesota), Universidad des Los Andres (Santiago, Chile) and Universidad Autonoma de Nuevo Leon (Monterrey, Mexico). Each of the study sites received approval by their institutional review boards and every participant provided written informed consent at the time of inclusion into the study. Details of the primary study are described elsewhere [16]. A TEM case was defined by fulfilling DSM-IV criteria for a manic or hypomanic episode within 8 weeks of starting an AD or increasing its dose, while similar exposure to an AD with no TEM was considered as a control. ADs were grouped into selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), serotonin antagonist and reuptake inhibitors (SARIs – nefazodone trazadone), monoamine oxidase inhibitors (MAOIs), norepinephrine–dopamine reuptake inhibitor (NDRIs – bupropion), and tricyclic antidepressants (TCAs). For exploratory analyses, we restricted the cases to those who had history of TEM on specific AD classes. For these class-specific definitions, controls were considered those with adequate (≥8 weeks) exposure to the specific AD class and no history of TEM. A participant meeting criterion for TEM may have had multiple AD exposures and thus TEM history was documented for specific ADs.
Genotyping and imputation for overall sample
Genotyping of the biobank sample was performed in three batches using different genomic platforms: (1) HumanOmniExpress-12v1-1; (2) GSA-24v2 and (3) Genotyping-by-Sequencing (GxS) performed by the Regeneron Genetics Center. Each batch was processed through the Mayo Clinic genotype quality control (QC) pipeline. In this QC pipeline, single nucleotide polymorphisms (SNPs) were excluded using filters for call rate (<95%), minor allele frequency (<0.5%), and Hardy-Weinberg Equilibrium (p < 1e-6). SNPs with a minor allele frequency less than 0.01 were also excluded Individuals were excluded for excessive missing genotypes (>5%), sex discrepancies, or abnormal heterozygosity (< 70% on multiple chromosomes). Each batch was then imputed using the TOPMed Imputation Server [17] and finally all three batches were merged. Relatedness within and across batches was estimated using KING-Robust [18]. For each pair with an estimated 2nd degree or higher relatedness, we preferentially kept those from the first batch, then those from the second batch and finally, those from the third batch. An individual was removed at random for related pairs within the same batch. Ancestry was estimated using ADMIXTURE [19]. Principal components (PCs) of ancestry were estimated using FlashPCA2 [20].
Polygenic score for antidepressant response
The PGS for response to ADs was estimated using summary statistics from the largest GWAS of AD response in MDD (N = 5218) [21] with LDpred2 with auto-selection of tuning parameters [22]. The PGS was standardized to have standard deviation equal to one and a mean of zero. The GWAS of AD response in MDD included only individuals of European ancestries. Thus, because PGS can be biased if estimated in a target sample of different ancestry from the training ancestry, we restricted our analysis to include only samples of European ancestry. We excluded samples with a predicted probability of European ancestry of less than 80%. We also excluded subjects from Mexico and Chile due to the known admixed populations in those countries [23]. In total, this accounted for N = 101 patients being removed from the analysis leaving N = 861 patients of European ancestry with an assessment of TEM included in the analyses.
Data analysis
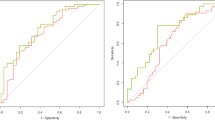
We first conducted a GWAS of TEM in BD using logistic regression to test for associations between each SNP with TEM while adjusting for the first PC and the GWAS batch. For the PGS analysis, logistic regression was used to examine the association between the AD response PGS and TEM in the BD sample adjusting for the first PC, GWAS batch, and BD type because BD-I has been associated with higher risk of TEM [24]. Given the higher risk of TEM within BD- I, we further explored how this PGS predicted TEM in a subset of patients with BD-I. Finally, within this subset, we restricted our definition of TEM to ADs with different mechanisms of action (SSRI or SNRI) to examine how this affected the association between genetically predicted AD response and TEM.
Results
A total of N = 313 (36%) patients had a history of TEM, while N = 548 (64%) patients had no history of TEM. When grouped by AD type, N = 221 (34%) and N = 139 (28%) had a history of TEM on SSRIs or SNRIs, respectively. Compared to patients without a history of TEM, patients with TEM were more likely to be female (69% vs. 60%; p = 0.011), have BD-I (78% vs. 69%; p = 0.0085) and, have a higher rate of history of serious suicide attempts (40% vs. 31%; p = 0.013). In addition, at study entry, patients with a history of TEM were less likely to be taking ADs (46% vs. 60%; p = 0.00013) and more likely to be currently using lamotrigine (39% vs. 25%; p = 0.00001). Table 1 summarizes participants’ demographic and clinical variables with or without a history of AD-associated TEM.
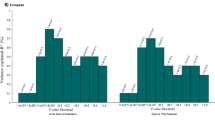
The GWAS of TEM did not identify any genome-wide significant variants. The top locus was (rs12929564 G/A; OR = 1.67; p = 2e-6) in an intronic region of RBFOX1. In the PGS analysis, a higher PGS for antidepressant response in MDD was associated with higher odds of TEM in BD (OR = 1.16 per SD increase in the PGS; p = 0.047). The PGS was more strongly associated with TEM in the BD-I sample (N = 622; OR = 1.27; p = 0.011) and was similar in BD-I individuals treated with SSRIs (N = 462; OR = 1.31; p = 0.016) or SNRIs (N = 352; OR = 1.32; p = 0.044). Conversely, the PGS association was not significant for the subset of BD-type II participants (N = 69; OR = 1.03; p = 0.811).
Discussion
This study extends previous work examining clinical and genetic factors of antidepressant-associated TEM in BD. Our PGS analysis revealed a genetically predicted better AD response in MDD associated with higher odds of TEM in BD, particularly for BD-I.
Importantly, this study is the first to suggest that biological mechanisms underpinning AD response in MDD directly overlaps with those conferring the adverse event of TEM in BD or that depression improvement may represent a spectrum from response, remission, to emergent mania. Similarly, recent studies have underscored the value in the utilization of PGS in examining treatment resistance in MDD, and its overlap association with other psychiatric disorders such as schizophrenia [25] and therapeutic response to medications such as lithium [26]. Our PGS results did not identify a significant association with BD-II disorder, which mirrors clinical practice where ADs monotherapy has suggested relative efficacy and safety [24, 27]. Our PGS BD-I signal aligns with controlled clinical studies and current meta-analyses suggesting that the BD-I subtype has greater clinical and now also, genomic risk of TEM, despite higher rates of antimanic mood stabilization.
Similar to recent publications [27, 28], our GWAS did not identify any genome-wide significant variants. The top locus in our GWAS was an intronic variant in RNA binding fox-1 homolog 1 (RBFOX1), a gene highly expressed in the brain. RBFOX1 regulates the expression of large genetic networks during neurodevelopment and was one of the top genes identified in the largest GWAS of mood disorders [29]. Importantly, RBFOX1 has been shown to critically regulate the expression of TrkB neurotrophin receptors to impact molecular signaling cascades conferring synaptic plasticity [30], and well-established to underpin mechanisms of AD response [31, 32].
Numerous hypotheses have highlighted the complexity surrounding ADs response and the emergence of side effects. Mechanistically, the monoaminergic hypothesis of AD response fails to fully address biological adaptations such as the AD-associated delayed therapeutic onset and neuroplasticity. Neurotrophic mechanisms dependent on brain-derived neurotrophic factor (BDNF) and mammalian target of rapamycin (mTOR) signaling promoting synaptic plasticity and activation of Wnt/ β-catenin signaling pathway have been proposed as an overlapping biological mechanism of action of ADs [31, 33,34,35,36]. Furthermore, the importance of mitochondrial energetics in the pathophysiology of BD is increasingly recognized [37, 38]. Interestingly, mitochondrial energetics may also play a role in AD associated TEM as recent data reported a significant increase in TEM rates in patients who were exposed to ADs that increase mitochondrial energetics [39], which would exert a downstream effect in the mTOR and Wnt/ β-catenin signaling pathways [35]. Importantly, the mTOR/Wnt/β-catenin signaling/pathway and mitochondrial energetics are mechanisms to further investigate in the spectrum of depression improvement from response to emergent mania aligning with the available genetic data.
We should consider several limitations of our study, most notably a negative GWAS result, likely because our study was underpowered due to the small sample size. This can be addressed by expanding to larger sample sizes in future GWAS and PGS analyses [40]. However, AD associated TEM studies will likely always have this limitation due to the complexities of collecting information on this phenotype. Our second limitation is the retrospective study design as to define the TEM phenotype. In addition, we did not analyze data from patients on AD monotherapy separately, and we should be aware of the possibility of a natural switch due to course of illness [5]. Considering our first limitation regarding a small sample size, we only included patients on specific classes of ADs such as SSRIs (N = 689) and SNRIs (N = 293) in our analysis. Finally, our PRS analysis was restricted to patients of European ancestry, which may limit the generalizability of our findings to other populations.
Nevertheless, our study has several strengths such as the inclusion of a TEM cohort confirmed by a thorough clinician review, not limiting only to self-report symptoms, with a narrow “window” of AD exposure. This study replicates previously established clinical risk factors for TEM (i.e., BD-I) [41] and would also be in accordance with previous registry data highlighting greatest risk within first three months of AD exposure [42].
In summary, our study extends previous literature on the clinical features and associations with AD associated TEM and supports the trans-diagnostic examination of the genetic overlap of treatment response across affective disorders (MDD and BD). Our findings suggest similar underlying genetic mechanisms between AD response in MDD and AD associated TEM in BD. Future work should focus on building larger samples examining AD mechanism of action and specific genetic variants which may provide a better understanding about the relationship between AD usage and TEM in BD.
Data availability
Data supporting the findings of this study are available from the corresponding author.
References
Pacchiarotti I, Bond DJ, Baldessarini RJ, Nolen WA, Grunze H, Licht RW, et al. The International Society for Bipolar Disorders (ISBD) task force report on antidepressant use in bipolar disorders. Am J Psychiatry. 2013;170:1249–62.
Frye MA, Helleman G, McElroy SL, Altshuler LL, Black DO, Keck PE, et al. Correlates of treatment-emergent mania associated with antidepressant treatment in bipolar depression. Am J Psychiatry. 2009;166:164–72.
Truman CJ, Goldberg JF, Ghaemi SN, Baldassano CF, Wisniewski SR, Dennehy EB, et al. Self-reported history of manic/hypomanic switch associated with antidepressant use: data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD).(CME). J Clin Psychiatry. 2007;68:1472–9.
Rhee TG, Olfson M, Nierenberg AA, Wilkinson ST. 20-year trends in the pharmacologic treatment of bipolar disorder by psychiatrists in outpatient care settings. Am J Psychiatry. 2020;177:706–15.
Blumberg HP. Euthymia, depression, and mania: what do we know about the switch? Biol psychiatry. 2012;71:570–1.
Stahl EA, Breen G, Forstner AJ, McQuillin A, Ripke S, Trubetskoy V, et al. Genome-wide association study identifies 30 loci associated with bipolar disorder. Nat Genet. 2019;51:793–803.
Cross-Disorder Group of the Psychiatric Genomics Consortium. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. 2013;381:1371–9.
Prata DP, Costa-Neves B, Cosme G, Vassos E. Unravelling the genetic basis of schizophrenia and bipolar disorder with GWAS: a systematic review. J Psychiatr Res. 2019;114:178–207.
Torkamani A, Wineinger NE, Topol EJ. The personal and clinical utility of polygenic risk scores. Nat Rev Genet. 2018;19:581–90.
Ruiz JAS, Commbes BJ, Pendegraft RS, Ozerdem A, McElroy SL, Cuellar-Barboza AB, et al. Pharmacotherapy exposure as a marker of disease complexity in bipolar disorder: associations with clinical & genetic risk factors. Psychiatry Res. 2023;323:115174.
Lewis CM, Vassos E. Polygenic risk scores: from research tools to clinical instruments. Genome Med. 2020;12:1–11.
Cearns M, Amare AT, Schubert KO, Thalamuthu A, Frank Joseph, Streit F, et al. Using polygenic scores and clinical data for bipolar disorder patient stratification and lithium response prediction: machine learning approach. Br J Psychiatry. 2022;220:219–28.
Coombes BJ, Markota M, Mann JJ, Colby C, Stahl E, Talati A, et al. Dissecting clinical heterogeneity of bipolar disorder using multiple polygenic risk scores. Transl Psychiatry. 2020;10:314.
Amare AT, Schubert KO, Hou L, Clark SR, Papiol S, Cearns M, et al. Association of polygenic score for major depression with response to lithium in patients with bipolar disorder. Mol Psychiatry. 2021;26:2457–70.
Amare AT, Schubert KO, Hou L, Clark SR, Papiol S, International Consortium on Lithium Genetics (ConLi+Gen) et al. Association of polygenic score for schizophrenia and HLA antigen and inflammation genes with response to lithium in bipolar affective disorder: a genome-wide association study. JAMA psychiatry. 2018;75:65–74.
Frye MA, McElroy SL, Fuentes M, Sutor B, Schak KM, Galardy CW, et al. Development of a bipolar disorder biobank: differential phenotyping for subsequent biomarker analyses. Int J Bipolar Disord. 2015;3:1–7.
Das S, Forer L, Schonherr S, Sidore C, Locke AE, Kwong A, et al. Next-generation genotype imputation service and methods. Nat Genet. 2016;48:1284–7.
Manichaikul A, Mychaleckyi JC, Rich SS, Daly K, Sale M, Chen WM. Robust relationship inference in genome-wide association studies. Bioinformatics. 2010;26:2867–73.
Alexander DH, Novembre J, Lange K. Fast model-based estimation of ancestry in unrelated individuals. Genome Res. 2009;19:1655–64.
Abraham G, Qiu Y, Inouye M. FlashPCA2: principal component analysis of Biobank-scale genotype datasets. Bioinformatics. 2017;33:2776–8.
Pain O, Hodgson K, Trubetskoy V, Ripke S, Marshe VS, Adams MJ, et al. Antidepressant response in major depressive disorder: a genome-wide association study. medRxiv, 2020.2012. 2011.20245035 (2020).
Privé F, Arbel J, Vilhjálmsson BJ. LDpred2: better, faster, stronger. Bioinformatics. 2020;36:5424–31.
Silva-Zolezzi I, Hidalgo-Miranda A, Estrada-Gil J, Fernandez-Lopez J, Uribe-Figueroa L, Contreras A, et al. Analysis of genomic diversity in Mexican Mestizo populations to develop genomic medicine in Mexico. Proc Natl Acad Sci. 2009;106:8611–6.
Altshuler LL, Suppes T, Black DO, Nolen WA, Leverich G, Keck PE, et al. Lower switch rate in depressed patients with bipolar II than bipolar I disorder treated adjunctively with second-generation antidepressants. Am J Psychiatry. 2006;163:313–5.
Fanelli G, Benedetti F, Kasper S, Zohar J, Souery D, Montgomery S, et al. Higher polygenic risk scores for schizophrenia may be suggestive of treatment non-response in major depressive disorder. Prog Neuro-Psychopharmacol Biol Psychiatry. 2021;108:110170.
Lu Y, Xiong Y, Karlsson R, Song J, Kowalec K, Ruck C, et al. Investigating genetic overlap between antidepressant and lithium response and treatment resistance in major depressive disorder. PREPRINT (Version 1) available at Research Square (2023).
Chen CK, Wu LSH, Huang MC, Kuo CJ, Cheng ATA. Antidepressant treatment and manic switch in bipolar I disorder: A clinical and molecular genetic study. J Personal Med. 2022;12:615.
Zai CC, Squassina A, Tiwari AK, Pisanu C, Pinna M, Pinna F, et al. A genome-wide association study of antidepressant-induced mania. Progress Neuro-Psychopharmacol Biol Psychiatry. 2023;127:110800.
Coleman JR, Gaspar HA, Bryois J, Bipolar Disorder Working Group of the Psychiatric Genomics Consortium, Major Depressive Disorder Working Group of the Psychiatric Genomics Consortium, Breen G. The genetics of the mood disorder spectrum: genome-wide association analyses of more than 185,000 cases and 439,000 controls. Biol Psychiatry. 2020;88:169–84.
Tomassoni-Ardori F, Fulgenzi G, Becker J, Barrick C, Palko ME, Kuhn S, et al. Rbfox1 up-regulation impairs BDNF-dependent hippocampal LTP by dysregulating TrkB isoform expression levels. Elife. 2019;8:e49673.
Yates C, Kruse JL, Price JB, Robertson AA, Tye SJ. Modulating neuroplasticity: lessons learned from antidepressants and emerging novel therapeutics. Curr Treat Opt Psychiatry. 2021;8:229–57.
Casarotto PC, Girych M, Fred SM, Kovaleva V, Moliner R, Enkavi G, et al. Antidepressant drugs act by directly binding to TRKB neurotrophin receptors. Cell. 2021;184:1299–313.e1219.
Ignácio ZM, Reus GZ, Arent CO, Abelaira HM, Pitcher MR, Quevedo J. New perspectives on the involvement of mTOR in depression as well as in the action of antidepressant drugs. Br J Clin Pharmacol. 2016;82:1280–90.
Dwyer JM, Lepack AE, Duman RS. mTOR activation is required for the antidepressant effects of mGluR2/3 blockade. Int J Neuropsychopharmacol. 2012;15:429–34.
Price JB, Bronars C, Erhardt S, Cullen KR, Schwieler L, Berk M, et al. Bioenergetics and synaptic plasticity as potential targets for individualizing treatment for depression. Neurosci Biobehav Rev. 2018;90:212–20.
Zhou W, Xu N, Kong L, Sun S-C, Xu X-F, Jia M-Z, et al. The antidepressant roles of Wnt2 and Wnt3 in stress-induced depression-like behaviors. Transl Psychiatry. 2016;6:e892.
Andreazza AC, Duong A, Young LT. Bipolar disorder as a mitochondrial disease. Biol Psychiatry. 2018;83:720–1.
Kato T. Mitochondrial dysfunction in bipolar disorder. Biomark Bipolar Disord. 2022. chapter 9, 141–56.
Gardea-Resendez M, Coombes BJ, Veldic M, Tye SJ, Romo-Nava F, Ozerdem A, et al. Antidepressants that increase mitochondrial energetics may elevate risk of treatment-emergent mania. Mol Psychiatry. 2023;28:1020–6.
Choi SW, Mak TS-H, O’Reilly PF. Tutorial: a guide to performing polygenic risk score analyses. Nat Protoc. 2020;15:2759–72.
Beaupre LMM, Tiwari AK, Goncalves VF, Lisoway AJ, Harripaul RS, Müller DJ, et al. Antidepressant-associated mania in bipolar disorder: a review and meta-analysis of potential clinical and genetic risk factors. J Clin Psychopharmacol. 2020;40:180–5.
Viktorin A, Lichtenstein P, Thase ME, Larsson H, Lundholm C, Magnusson PKE, et al. The risk of switch to mania in patients with bipolar disorder during treatment with an antidepressant alone and in combination with a mood stabilizer. Am J Psychiatry. 2014;171:1067–73.
Acknowledgements
We acknowledge Regeneron Genetics Center for providing genetic data for a portion of the bipolar biobank participants for the analysis. Project Generation were supported in part by Mayo Clinic’s Center for Individualized Medicine. Funding for the study was provided by the Marriott Foundation and the Dauton Family. The foundation and family had no further role in the study design, analysis or interpretation of the data, in the writing of the report, or in the decision to submit the paper for publication. We would also like to thank Mr. Larry Prokop from the Mayo Clinic Library, Mayo Clinic Rochester, MN, USA for helping and conducted the literature search. Presented at the Annual meeting of the Society of Biological Psychiatry. San Diego, April 27–29, 2023.
Author information
Authors and Affiliations
Contributions
All authors have contributed to the manuscript in accordance with the ICMJE’s criteria for authorship. Conceptualization: NAN, BJC, JMB, SJT, MAF; methodology: NAN, BJC, LMB, GJ, JMB, MAF; original draft preparation: NAN, BJC, LMB, SJT, SLM, JMB, MAF; writing—review and editing: all authors; supervision: SJT, JMB, MAF. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
NAN reports no financial relationships with commercial interests. BJC reports no financial relationships with commercial interests. LMB reports no financial relationships with commercial interests. AO reports no financial relationships with commercial interests. MGR reports no financial relationships with commercial interests. FRN receives grant support from the National Institute of Mental Health K23 Award (K23MH120503) and from a 2017 NARSAD Young Investigator Award from the Brain and Behavior Research Foundation; has a U.S. Patent and Trademark Office patent # 10,857,356; receives consultant fees from Otsuka Pharmaceutical and has received non-financial research support from Soterix Medical. DJB has received research support from NIDA, NuBiyota, the University of Minnesota Foundation, and the University of Minnesota Department of Psychiatry and Behavioral Sciences MV reports no financial relationships with commercial interests. BS received grant support from Mayo Clinic. KMM reports no financial relationships with commercial interests. HKB reports no financial relationships with commercial interests. SK reports no financial relationships with commercial interests. MFS reports no financial relationships with commercial interests. ME reports no financial relationships with commercial interests. AM reports no financial relationships with commercial interests. JASR reports no financial relationships with commercial interests. GJ reports no financial relationships with commercial interests. AB reports no financial relationships with commercial interests. JGL reports no financial relationships with commercial interests. ACB reports no financial relationships with commercial interests. SJT reports no financial relationships with commercial interests. SLM is or has been a consultant to or member of the scientific advisory boards of Avanir, Allergan (now AbbVie), Bracket (now Signant Health), Idorsia, Intra-Cellular Therapies, Inc., Naurex, Otsuka, Shire (now Takeda), Sunovion, and Takeda. She is or has been a principal or co-investigator on studies sponsored by the Agency for Healthcare Research & Quality (AHRQ), Avenir, AstraZeneca, Cephalon, Forest, Jazz, Marriott Foundation, Medibio, National Institute of Mental Health, Orexigen Therapeutics, Inc., Otsuka, Shire (now Takeda), Sunovian, and Takeda Pharmaceutical Company Ltd. She is also an inventor on United States Patent No. 6,323,236 B2, Use of Sulfamate Derivatives for Treating Impulse Control Disorders, and along with the patent’s assignee, University of Cincinnati, Cincinnati, Ohio, has received payments from Johnson & Johnson, which has exclusive rights under the patent. JMB reports no financial relationships with commercial interests. MAF has received grant support from Assurex Health and Mayo Foundation, received CME travel and honraria from Carnot Laboratories, and has Financial Interest/Stock ownership/Royalties from Chymia LLC.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nuñez, N.A., Coombes, B.J., Beaupre, L.M. et al. Pharmacogenomic overlap between antidepressant treatment response in major depression & antidepressant associated treatment emergent mania in bipolar disorder. Transl Psychiatry 14, 93 (2024). https://doi.org/10.1038/s41398-024-02798-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-024-02798-y