Abstract
Suicidality in mood disorder patients is common, especially in emergency department (ED), but the patterns and associated factors of suicidality are not clear. This study compared biomarkers and mental health symptoms (i.e., depression, anxiety, and psychiatric symptoms) between mood disorder patients with and without the whole range of suicidality comprising suicidal ideation (SI), suicide plan (SP), and suicide attempt (SA). This cross-sectional, comparative, convenient-sampling study was conducted between January 2021 and March 2022, in emergency department of Beijing Anding Hospital, China. Patients with mood disorders at a psychiatric emergency department were assessed, with measurements of suicidality, biomarkers, depressive, anxiety, and psychiatric symptoms were assessed using the 24 items-Hamilton Depression Rating Scale (HAMD-24), Hamilton Anxiety Rating Scale (HAMA), Young Manic Rating Scale (YMRS) and Brief Psychiatric Rating Scale (BPRS), respectively. The propensity score matching (PSM) method was used to identify patients in mood disorder with and without SI, SP, and SA. A generalized linear model (GLM) was used to assess the differences in biomarkers, depressive, anxiety, and psychiatric symptoms between patients in mood disorder with and without SI, SP, and SA. In total, 898 participated in this survey and completed the assessment. Illness duration was significantly negatively associated with SA (OR = 0.969, 95%CI = 0.939–0.999, P = 0.046). HAMD-24 total score was significantly positively associated with the SI (OR = 1.167, 95%CI = 1.134–1.201, p < 0.001), SP (OR = 1.159, 95%CI = 1.126–1.192, p < 0.001) and SA (OR = 1.189, 95%CI = 1.144–1.235, p < 0.001) of the matched samptched sample. However, YMRS total score was significantly negatively associated with the SI (OR = 0.928, 95%CI = 0.905–0.951, p < 0.001), SP (OR = 0.920, 95%CI = 0.897–0.944, p < 0.001) and SA (OR = 0.914, 95%CI = 0.890–0.938, p < 0.001) of the matched sample after adjusting for age, gender, marital status, and occupation. The duration of illness, severity of depressive symptoms and severity of manic symptoms appeared to be more likely to influence suicidality. Considering the significant risk of suicide in mood disorders on psychiatric emergency care, timely treatment and effective management of suicidality in this population group need to be developed.
Similar content being viewed by others
Introduction
Suicide, responsible for an estimated 703,000 deaths worldwide each year, remains a significant public health issue [1]. Beyond the immediate personal and familial distress that it causes, suicide also amplifies the healthcare burden. While various factors can lead to suicide in the general population, the presence of psychiatric conditions, especially mood disorders, elevates the risk significantly. As a lifelong episodic illness, mood disorder can result in various setbacks, from functional, occupational, and cognitive impairments [2] to severe outcomes like suicidality [3]. Notably, emergency department (ED) visits in the USA related to suicidality more than doubled from 244,000 in 1993–1996 to 538,000 in 2005–2008 [4]. Furthermore, an estimated one in ten patients exhibiting suicidality had visited an emergency room within two months preceding their death [5]. Compared to those without psychiatric disorders, individuals with mood disorders exhibit substantially higher rates of suicidality [6], sparking widespread international concern.
Suicidal behaviors, which collectively escalate the risk for suicide, include suicidal ideation (SI), suicide plans (SP), and suicide attempts (SA) [3, 7]. SI, colloquially termed as suicidal thoughts, encompasses all suicidal considerations without necessarily progressing to more overt acts. SP pertains to the strategizing of self-harm with the intent to end one’s life [8], while SA involves actual actions taken with this intent. Within the context of major depressive depression (MDD), the prevalence of SI is observed to be 37.7% (95% CI: 32.3–43.4%), whereas SP is reported at a pooled prevalence of 15.1% (95% CI: 8.0–26.8%) [9]. SI, SP, and SA are often predictors of eventual suicide, forming a spectrum characterized by escalating psychological distress and neuroendocrine alterations [10]. Notably, around one-third of adolescents who exhibit SI eventually develop SP, and close to 60% with SP transition to SA [11]. Given the diverse prevalence rates, clinical manifestations, and outcomes of these behaviors, there remains an uncharted territory regarding their patterns and associated factors within ED settings. As the ED serves as a pivotal interface in the healthcare system, the immediate need is to devise proficient screening and risk assessment mechanisms integrating multiple biomarkers, thereby ensuring efficacious suicide prevention during ED consultations [12].
A substantial body of evidence implicates inflammation, nutrition, and neurohormones as significant contributors to the genesis of suicidality (Oliveira et al., 2017). Specifically, alterations in immune markers like C-reactive protein (CRP) have been identified in the peripheral blood. Notably, MDD patients consistently show elevated CRP levels compared to their non-affected counterparts [13,14,15]. The hormones cortisol and adrenocorticotropic hormone (ACTH) offer critical insights into the functioning of the hypothalamic-pituitary-adrenal (HPA) axis. Disrupted secretion patterns of these hormones are discernible across MDD [16], BD [17], and Schizophrenia (SCZ) [18] which are further consolidated by meta-analyses [17, 19]. The most consistent observation relating to suicide has been its association with HPA axis anomalies. Moreover, recent research suggests testosterone, a sex hormone, plays a partial role in modulating suicidal behaviors [20]. In light of this, we have incorporated these elements as prospective biomarkers in our investigation.
Traditionally, suicidality in mood disorders is conceptualized as observable expressions of a single underlying condition. This perspective, however, tends to oversimplify by overlooking the unique causality, progression, and heterogeneity of individual symptoms. In traditional methodology approach, suicidality was acted as the dependent variable and effected by many covariates. It also neglects the intricate interrelations among these symptoms [21]. Enter the Propensity Score Matching (PSM) method, an innovative approach for balancing covariates between experimental and control groups, especially when an ideal randomized experimental design is unfeasible [22]. PSM stands out for its capability to discern the influence of an independent variable while substantially reducing the selection bias, thereby ensuring the validity of the results [22,23,24]. Recognizing its advantages, we incorporated PSM in our study to equate demographic variances between mood disorder patients, segmented based on the presence or absence of SI, SP, and SA. Such methodological refinement elevates our capacity to estimate suicidality risk in vulnerable individuals. The aim of this study was to provide the potential targets for warranting the physicians’ attention in the evaluation protocol.
Methods
Study setting and participants
This cross-sectional comparative study was conducted between January 2021 and March 2022, in emergency department of Beijing Anding Hospital, which has a 300-bed Mood Disorders Centre. The Psychiatric Emergency Department is divided into an emergency treatment area consisting of a 17-bed emergency observation ward and 4 ICU beds. The average number of emergency room visits per month was 2000. It provides the only 24-h emergency service for psychiatric hospitals in Beijing and neighboring provinces in North China.
Patients attending the emergency outpatient clinics were invited to participate in the study. To be eligible, participants needed to meet the following criteria: 1) aged 18 years or older; 2) diagnosed with mood disorder according to the F30-39 section of the tenth revision of the International Classification of Disease (ICD-10) [25] by a consensus of two senior psychiatrists; 3) able to understand the aim and contents of the assessment and provide verbal informed consent. Persons with cognitive impairment were excluded. The study was conducted on a voluntary and confidential basis and the study protocol was approved by the Ethics Committee of Beijing Anding Hospital.
Data collection and assessment tools
A data collection form was used to collect demographic information, including age, gender, education level, occupation, living status, marital status, medical insurance, family history of mental health, health status, relationship with friends or family members, whether irritability is a personal characteristic, family support, whether a stress event occurred, and interpersonal communication. Clinical data included illness duration (years) and age at first episode. The 24-item Hamilton Depression Rating Scale (HAMD-24) was used to assess depressive symptoms. The Chinese version of the HAMD-24 has been validated with satisfactory psychometric properties (e.g., Cronbach’s alpha of α = 0.92) [26]. The Hamilton Anxiety Rating Scale (HAMA) was used to assess anxiety symptoms. The Chinese version of the HAMA has been validated with satisfactory psychometric properties (e.g., Cronbach’s alpha of α = 0.93) [27]. The Young Mania Rating Scale (YMRS) is one of the most frequently utilized rating scales to assess manic symptoms [28]. The Brief Psychiatric Rating Scale (BPRS) [29] was used to estimate psychiatric symptoms. The Chinese version of the BPRS has been validated with satisfactory psychometric properties [30]. These psychiatrists were trained on the assessment of HAMD, HAMA, YMRS, and BPRS in a clinical study before the study began. The inter-rater correlation coefficient of HAMD, HAMA, BPRS, and PANSS scores of psychiatrists were all more than 0.8.
In this study, current SI, SP, and SA were assessed through face-to-face interview. SI was assessed with a standard question (“Have you thought that you would be better off dead currently?”) that included a binary response option (yes/no). SP was assessed with a standard question (“Have you made a plan for suicide currently?”) featuring a binary response option (yes/no). SA were evaluated with a standard question (“Have you attempted suicide currently?”), including a binary response option (yes/no).
Biochemical parameters measurements
All subjects had their peripheral blood taken before 10 o’clock in the morning within 24–72 h after admission to the hospital, and some participants also received their blood test before being discharged from the hospital. Fasting biochemical indexes were measured, including CRP, cortisone, ACTH, and testosterone were collected from medical records available in the hospital.
Statistical analyses
Propensity score matching
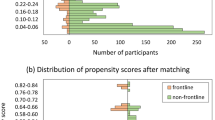
Due to different demographic characteristics between the mood disorder patients with suicidality and non-suicidality patients in this study, the optimal fixed ratio matching based on propensity scores was used to identify comparable suicidality and non-suicidality mood disorders patients with a matching ratio of 1:1. Propensity score is the probability of a participant being assigned to a particular group (i.e., age, gender, marital status and occupation in this study), calculated by a logistic regression model based on a given set of observed covariates (i.e., confounders) [31]. The propensity score matching procedure would match each participant in suicidality groups with one non-suicidality, thereby balancing the potential confounders between the two groups [31, 32]. The propensity score analysis could help reduce bias in research results by minimizing the confounding effects caused by unmatched demographic characteristics [32]. Confounders refer to variables that affect both the outcome variable and the grouping variable; the potential confounders matched in the propensity score model are selected based on the variable-grouping relationships and the variable-outcome relationships [32, 33]. In this study, the variable-grouping relationships and the variable-outcome relationships were assessed using independent two-sample t tests, Wilcoxon rank-sum tests, and chi-square tests as appropriate. Confounders were selected based on an expert consensus and the findings of previous studies in the propensity score model [34].
Univariable analyses
In univariable analyses before and after matching, the demographic and clinical characteristics between the MD patients with suicidality to those without suicidality. Suicidality MD patients and non-suicidality MD patients were compared using independent two-sample t tests, Wilcoxon rank-sum tests, and χ2 tests as appropriate. In the matched study sample, demographic characteristics that were significant in the univariable analyses were adjusted for in multivariable analysis models.
Multivariable analyses
In the matched study sample, the binary logistic regression was used to examine independent correlates of suicide behaviors. SI, SP, and SA were entered as separate dependent variables while measures with significant suicidality versus no suicidality group differences in univariate analyses were independent variables, while adjusting for the demographic characteristics that were still significant in the univariable analyses after matching. All data analyses were conducted using the “MatchIt” function of R [35]. Two-tailed p values <0.05 were considered as statistically significant.
Results
Demographic and clinical characteristics of the whole sample
Altogether, 898 participants in this survey and completed the assessment. Suicidality and non-suicidality participants were statistically different in gender occupation, unmarried, irritability personal characteristics, stress event, less interpersonal communication, age, education background, illness duration, first episode age, Cortisone, ACTH, sex, Testosterone, HAMD-24 total, HAMA total, YMRS total and BRPS total (all p values < 0.05; Supplementary Table 1).
Potential confounder selection for propensity score matching
According to the preliminary results of the variable-grouping and the variable-outcome relationships (Supplementary Tables 1), occupation, and marital status of the MD patients were selected as the potential confounders, all of which were matched in the propensity score model. Additionally, since age and gender were the most commonly used confounders in previous studies [36,37,38], age and gender were also selected for matching in the propensity score model.
The propensity scores matching procedure identified 280 comparable patients with SI and patients without SI in each group, composing a matched study sample of 560 participants. The propensity scores matching procedure identified 273 comparable patients with suicide plan and patients without suicide plan in each group, composing a matched study sample of 546 participants. The propensity scores matching procedure identified 275 comparable patients with suicide attempt and patients without suicide attempt in each group, composing a matched study sample of 550 participants.
Univariate and multivariate analysis of the matched sample
The demographic and clinical characteristics of the matched two samples are shown in Table 1. Univariate analyses revealed that the patients with SI and their matched patients without SI were comparable in age, sex, occupation, and marital status (all p values > 0.05). There were significant differences between the patients with SI and patients without SI in terms of the irritability personal characteristics, stress event, less interpersonal communication, education background, illness duration, HAMD-24 total, HAMA total, and YMRS total scores (all p values < 0.05; Supplementary Figs. 1–3).
Univariate analyses revealed that the patients with suicide plan and their matched patients without SP were comparable in age, sex, occupation, and marital status (all p values > 0.05). There were significant differences between the patients with SP and patients without SP in terms of the irritability personal characteristics, stress event, less interpersonal communication, lower education background, illness duration, HAMD-24 total, HAMA total, and YMRS total scores (all p values < 0.05).
Univariate analyses revealed that the patients with SA and their matched patients without SA were comparable in age, sex, occupation, and marital status (all p values > 0.05). There were significant differences between the patients with SA and patients without SA in terms of the irritability personal characteristics, stress event, less interpersonal communication, education background, illness duration, HAMD-24 total, HAMA total, and YMRS total scores (all p values < 0.05).
Table 2 presents results of binary logistic regression analyses. There are significant correlation (p < 0.001) between HAMD-24 total score and HAMA total score among the SI (p < 0.001, OR: 1.167, 95%CI: 1.134–1.201), SP (p < 0.001, OR: 1.159, 95%CI: 1.126–1.192) and SA (p < 0.001, OR: 1.189, 95%CI: 1.144–1.235) of the matched sample, respectively. Illness duration was significantly negatively associated with SA (OR = 0.969, 95%CI = 0.939–0.999, p = 0.046). HAMD-24 total score was significantly positively associated with the SI (OR = 1.167, 95%CI = 1.134–1.201, p < 0.001), SP (OR = 1.159, 95%CI = 1.126–1.192, p < 0.001) and SA (OR = 1.189, 95%CI = 1.144–1.235, p < 0.001) of the matched sample. However, YMRS total score was significantly negatively associated with the SI (OR = 0.928, 95%CI = 0.905–0.951, p < 0.001), SP (OR = 0.920, 95%CI = 0.897–0.944, p < 0.001) and SA (OR = 0.914, 95%CI = 0.890–0.938, p < 0.001) of the matched sample (Table 2).
Discussion
In this study conducted in China’s Emergency departments, we observed for the first time that patients with mood disorders and suicidality presented with higher HAMD total scores, increased symptoms of hypomania, and a shorter duration of illness compared to their non-suicidal counterparts with mood disorders. Notably, there were no significant disparities in anxiety levels, inflammation markers like CRP, or biological indicators such as Cortisol and ACTH levels.
Early in the course of the disease, the risk of the suicidality is peak. Consistently, our findings depicted a negative correlation between the duration of the illness and SA. This contrasts with previous research that suggested an association between longer illness duration and more severe outcomes in BD, especially in the context of suicidality [39]. Upon being diagnosed with a mood disorder, patients may grapple with feelings of hopelessness, an overwhelming symptom burden, diminished overall functionality, and an increased reliance on mental health services. Any of these factors could precipitate suicidal attempts.
Moreover, while sociocultural elements play a part, previous studies indicate that the increased risk of suicidality in patients with a short illness duration might be linked to biological factors. These include disrupted N-acetylaspartate (NAA)-glutamatergic metabolism in the anterior cingulate cortex [40], and compromised executive functioning and impulse control due to decreased structural connectivity in the frontal subcortical circuit [41].
Among mood disorder inpatients, the severity of depressive symptoms was significantly positively associated with SI, SP, and SA, which is also true of MDD patients [9, 42, 43]. This pattern can probably be attributed to the more severe psychotic symptoms [44, 45] and somatic symptoms [46] among mood disorders patients. Recent findings also indicate that more severe psychiatric symptoms are linked to higher suicide risk in both the MDD and general population and for those with pre-existing psychiatric conditions during the pandemic [47, 48]. Residual psychiatric symptoms such as depressive symptoms may be reflections of past suicidality or serve as prognosticators for worse outcomes, including increased risk for relapse, recurrence, and suicidality [49, 50]. Hence, these symptoms should be addressed in maintenance treatment and rehabilitation for patients when they visit emergency department.
One reason might be that inpatients may have hallucinations commanding them to self-harm. Moreover, mood disorders patients tend to have more severe and multimorbid psychopathology, a higher burden of symptoms, poorer global functioning, and higher usage of mental health services, all of which were associated with SI, SP, and SA. The severity of depressive symptoms is also a manifestations of illness episodes which has recently been shown to be associated with occurrence of suicide attempts [51]. As expected, patients with depressive course of illness have a 2-fold risk of suicide attempts, compared with predominantly manic patients; including patients with mixed states into depressive polarity strengthens the association to 4.5-fold [51]. Recent findings also indicate that more severe psychiatric symptoms are linked to higher suicide risk in both the general population and those with pre-existing psychiatric conditions during the pandemic [52]. Residual psychiatric symptoms such as fatigue, pain, and depressive symptoms may be reflections of past suicidality or serve as prognosticators for worse outcomes, including increased risk for relapse, recurrence, and suicidality [49, 50]. Hence, these symptoms should be addressed in maintenance treatment and rehabilitation for clinically stable psychiatric patients during the pandemic.
In our study, we found that the severity of manic symptoms was negatively related to the SI, SP, and SA among mood disorders patients. The result was consistent with the previous findings that hypomania symptoms have been related to mood instability, impulsive behaviors, and increased risk of suicidality in individuals with bipolar disorder [53,54,55]. In the same line, suicidality was related to manic, depressive symptoms and emotion dysregulation, especially to emotional impulsivity and to difficulties in regulatory strategies, as previously observed [56]. Indeed, emotional impulsivity and manic symptoms were the factors more strongly related to suicidality. Manic symptoms as a component of one type of emotion dysregulation is defined as an impairment in the modulation of some aspects of emotional functioning including early emotional processes, the appraisal and evaluation of stimuli and emotional response with its behavioral and physiological components in both the immediate context and in the long-term objectives/goals of individuals [55]. Furthermore, our included participants were patients who seek medical help in an emergency center and were in the episode state.
The strengths of this study included using the propensity score matching method and collecting participants in emergency department. However, several limitations should be noted. First, patients were the inpatients who presented to the emergency department, psycho-social variables might be more serious than other department patients, which might have recall and reporting bias. Second, the data were collected based on self-report; therefore, the possibility of recall bias could not be excluded. Third, for logical reasons, this was cross-sectional research that was unable to assess the causal relationships among study variables. Longitudinal studies closely examining the development of psychiatric disorders, illness episode, cooccurring disorders, and suicide, are needed to answer these crucial questions of causation. Fourth, the analyses primarily made use of dichotomous dependent variables (e.g., have or have not attempted suicide), providing no information regarding the severity of assigned suicidal ideation or attempts. Finally, the information about the use of psychotropic medications was not recorded.
In conclusion, as most psychiatric patients suffering from a major depressive or a mixed mood episode actually consider, plan, or attempt suicide, mere suffering from a major mood disorder itself explains much of the associated suicidal behaviors. As a promising setting for suicide prevention, the emergency department needs to establish some appropriate strategies for universal screening, risk assessment and follow-up care. However, the temporal and dose-exposure association with severity of illness, duration of illness risk states are the prevention components that need to be focused on.
Data availability
The data of the investigation will be made publicly available if necessary.
References
World Health Organization. Suicide. https://www.whoint/news-room/fact-sheets/detail/suicide (access 20 Jan 2023) 2022.
Melhem NM, Porta G, Oquendo MA, Zelazny J, Keilp JG, Iyengar S, et al. Severity and variability of depression symptoms predicting suicide attempt in high-risk individuals. JAMA Psychiatry. 2019;76:603–13.
Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. 2016;387:1227–39.
Ting SA, Sullivan AF, Boudreaux ED, Miller I, Camargo CA Jr. Trends in US emergency department visits for attempted suicide and self-inflicted injury, 1993-2008. Gen Hosp Psychiatry. 2012;34:557–65.
Laliberte AZ, Roth B, Edwards B, Chen JI. Suicide screening and risk assessment in the emergency department: case review of a suicide attempt survivor. J Emerg Nurs. 2021;47:846–51.
Miller JN, Black DW. Bipolar disorder and suicide: a review. Curr Psychiatry Rep. 2020;22:6.
Voracek M. National differences in intelligence and population rates of suicidal ideation, suicide plans, and attempted suicide. Percept Mot Skills. 2007;105:355–61.
Linthicum KP, Ribeiro JD. Suicide plan prevalence, recurrence, and longitudinal association with nonfatal suicide attempt. Suicide Life Threat Behav. 2022;52:1062–73.
Cai H, Jin Y, Liu S, Zhang Q, Zhang L, Cheung T, et al. Prevalence of suicidal ideation and planning in patients with major depressive disorder: a meta-analysis of observation studies. J Affect Disord. 2021;293:8–58.
Tuisku V, Pelkonen M, Karlsson L, Kiviruusu O, Holi M, Ruuttu T, et al. Suicidal ideation, deliberate self-harm behaviour and suicide attempts among adolescent outpatients with depressive mood disorders and comorbid axis I disorders. Eur Child Adolesc Psychiatry. 2006;15:199–206.
Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192:98–105.
Bird S, Lago L, Eagar K, Pai N. Suicide prevention: emergency departments are crucial for surveillance of self-harm and suicide-related behaviours. Aust N Z J Psychiatry. 2021;55:729–30.
Fernandes BS, Steiner J, Molendijk ML, Dodd S, Nardin P, Gonçalves CA, et al. C-reactive protein concentrations across the mood spectrum in bipolar disorder: a systematic review and meta-analysis. Lancet Psychiatry. 2016;3:1147–56.
Orsolini L, Sarchione F, Vellante F, Fornaro M, Matarazzo I, Martinotti G, et al. Protein-C reactive as biomarker predictor of schizophrenia phases of illness? A systematic review. Curr Neuropharmacol. 2018;16:583–606.
Yuan Y, Long P, Liu K, Xiao Y, He S, Li J, et al. Multiple plasma metals, genetic risk and serum C-reactive protein: a metal-metal and gene-metal interaction study. Redox Biol. 2020;29:101404.
Asadikaram G, Khaleghi E, Sayadi A, Foulady S, Ghasemi MS, Abolhassani M, et al. Assessment of hormonal alterations in major depressive disorder: a clinical study. Psych J. 2019;8:423–30.
Belvederi Murri M, Prestia D, Mondelli V, Pariante C, Patti S, Olivieri B, et al. The HPA axis in bipolar disorder: systematic review and meta-analysis. Psychoneuroendocrinology. 2016;63:327–42.
Nordholm D, Rostrup E, Mondelli V, Randers L, Nielsen M, Wulff S, et al. Multiple measures of HPA axis function in ultra high risk and first-episode schizophrenia patients. Psychoneuroendocrinology. 2018;92:72–80.
Zorn JV, Schür RR, Boks MP, Kahn RS, Joëls M, Vinkers CH. Cortisol stress reactivity across psychiatric disorders: a systematic review and meta-analysis. Psychoneuroendocrinology. 2017;77:25–36.
Sher L, Sublette ME, Grunebaum MF, Mann JJ, Oquendo MA. Plasma testosterone levels and subsequent suicide attempts in males with bipolar disorder. Acta Psychiatr Scand. 2022;145:223–5.
Fried EI, Nesse RM. Depression sum-scores don’t add up: why analyzing specific depression symptoms is essential. BMC Med. 2015;13:72.
Kane LT, Fang T, Galetta MS, Goyal DKC, Nicholson KJ, Kepler CK, et al. Propensity score matching: a statistical method. Clin Spine Surg. 2020;33:120–2.
Xu RH, Zhou LM, Wong EL, Chang J, Wang D. Satisfaction with patient engagement and self-reported depression among hospitalized patients: a propensity-score matching analysis. Front Psychiatry. 2022;13:751412.
Mak HW, Bu F, Fancourt D. Mental health and wellbeing among people with informal caring responsibilities across different time points during the COVID-19 pandemic: a population-based propensity score matching analysis. Perspect Public Health 2022 https://doi.org/10.1177/17579139221104.
World Health Organization. The ICD-10 Classification Of Mental And Behavioural Disorders: Clinical Descriptions And Diagnostic Guidelines. Geneva: World Health Organization1992.
Zheng Y, Zhao J, Phillips M, Liu J, Cai M, Sun S, et al. Validity and reliability of the Chinese Hamilton depression rating scale. Br J Psychiatry. 1988;152:660–4.
Zhang Y, Zhang M. Hamilton Anxiety Rating Scale (HAMA) Shanghai. Psychiatry. 1984;2:64–5.
Zhang Y, Long X, Ma X, He Q, Luo X, Bian Y, et al. Psychometric properties of the Chinese version of the Functioning Assessment Short Test (FAST) in bipolar disorder. J Affect Disord. 2018;238:156–60.
Woerner MG, Mannuzza S, Kane JM. Anchoring the BPRS: an aid to improved reliability. Psychopharmacol Bull. 1988;24:112–7.
Chan DW, Lai B. Assessing psychopathology in Chinese psychiatric patients in Hong Kong using the brief psychiatric rating scale. Acta Psychiatr Scand. 1993;87:37–44.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55.
Austin PC. A critical appraisal of propensity‐score matching in the medical literature between 1996 and 2003. Stat Med. 2008;27:2037–49.
Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Stürmer T. Variable selection for propensity score models. Am J Epidemiol. 2006;163:1149–56.
Montastruc F, Nie R, Loo S, Rej S, Dell’Aniello S, Micallef J, et al. Association of aripiprazole with the risk for psychiatric hospitalization, self-harm, or suicide. JAMA Psychiatry. 2019;76:409–17.
R Core Team. R: A Language And Environment For Statistical Computing. 2013.
Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005-17. J Abnorm Psychol. 2019;128:185.
Möller-Leimkühler AM. The gender gap in suicide and premature death or: why are men so vulnerable? Eur Arch psychiatry Clin Neurosci. 2003;253:1–8.
Hawton KI, Comabella CC, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013;147:17–28.
Altamura AC, Dell’Osso B, Berlin HA, Buoli M, Bassetti R, Mundo E. Duration of untreated illness and suicide in bipolar disorder: a naturalistic study. Eur Arch Psychiatry Clin Neurosci. 2010;260:385–91.
Lewis CP, Port JD, Blacker CJ, Sonmez AI, Seewoo BJ, Leffler JM, et al. Altered anterior cingulate glutamatergic metabolism in depressed adolescents with current suicidal ideation. Transl Psychiatry. 2020;10:119.
Myung W, Han CE, Fava M, Mischoulon D, Papakostas GI, Heo JY, et al. Reduced frontal-subcortical white matter connectivity in association with suicidal ideation in major depressive disorder. Transl Psychiatry. 2016;6:e835.
Dong M, Wang SB, Li Y, Xu DD, Ungvari GS, Ng CH, et al. Prevalence of suicidal behaviors in patients with major depressive disorder in China: a comprehensive meta-analysis. J Affect Disord. 2018;225:32–9.
Dong M, Zeng L-N, Lu L, Li X-H, Ungvari GS, Ng CH, et al. Prevalence of suicide attempt in individuals with major depressive disorder: a meta-analysis of observational surveys. Psychol Med. 2019;49:1691–704.
Li X, Liu H, Hou R, Baldwin DS, Li R, Cui K, et al. Prevalence, clinical correlates and IQ of suicidal ideation in drug naive Chinese Han patients with major depressive disorder. J Affect Disord. 2019;248:59–64.
Dolsen EA, Prather AA, Lamers F, Penninx BWJH. Suicidal ideation and suicide attempts: associations with sleep duration, insomnia, and inflammation. Psychol Med. 2021;51:2094–2103.
Fang X, Zhang C, Wu Z, Peng D, Xia W, Xu J, et al. The association between somatic symptoms and suicidal ideation in Chinese first-episode major depressive disorder. J Affect Disord. 2019;245:17–21.
Zhang L, Cai H, Bai W, Zou S-Y, Feng K-X, Li Y-C, et al. Prevalence of suicidality in clinically stable patients with major depressive disorder during the COVID-19 pandemic. J Affect Disord. 2022;307:142–8.
Na PJ, Tsai J, Hill ML, Nichter B, Norman SB, Southwick SM, et al. Prevalence, risk and protective factors associated with suicidal ideation during the COVID-19 pandemic in US military veterans with pre-existing psychiatric conditions. J Psychiatr Res. 2021;137:351–9.
Judd LL, Paulus MJ, Schettler PJ, Akiskal HS, Endicott J, Leon AC, et al. Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? Am J Psychiatry. 2000;157:1501–04.
Kennedy N, Paykel E. Residual symptoms at remission from depression: impact on long-term outcome. J Affect Disord. 2004;80:135–44.
Carballo JJ, Harkavy-Friedman J, Burke AK, Sher L, Baca-Garcia E, Sullivan GM, et al. Family history of suicidal behavior and early traumatic experiences: additive effect on suicidality and course of bipolar illness? J Affect Disord. 2008;109:57–63.
Fitzpatrick KM, Harris C, Drawve G. Living in the midst of fear: Depressive symptomatology among US adults during the COVID‐19 pandemic. Depress Anxiety. 2020;37:957–64.
Gross JJ, Thompson RA. Handbook of Emotion Regulation. 2006.
Henry C, Phillips M, Leibenluft E, M’bailara K, Houenou J, Leboyer M. Emotional dysfunction as a marker of bipolar disorders. Front Biosci (Elite Ed). 2012;4:2722.
Palagini L, Cipollone G, Masci I, Caruso D, Paolilli F, Perugi G, et al. Insomnia symptoms predict emotional dysregulation, impulsivity and suicidality in depressive bipolar II patients with mixed features. Compr Psychiatry. 2019;89:46–51.
Johnson SL, Carver CS, Tharp JA. Suicidality in bipolar disorder: The role of emotion‐triggered impulsivity. Suicide Life‐Threatening Behav. 2017;47:177–92.
Acknowledgements
The study was supported by the project initiated by the researchers in Beijing Anding Hospital (2022(30)).
Author information
Authors and Affiliations
Contributions
(I) Conception and design: XJ, HC, and XX. (II) Administrative support: XJ, YL, and YFW. (III) Provision of study materials or patients: HZ, TJ, YL, TH, and JL. (IV) Collection and assembly of data: HZ, TJ, YFW, YL, TH, and JL. (V) Data analysis and interpretation: XX and HC. (VI) Manuscript writing: all authors. (VII) Final approval of manuscript: all authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study involving human participants were reviewed and approved by Human Research and Ethics Committee of Beijing Anding Hospital, Capital Medical University. All the study procedures were carried out in accordance with relevant guidelines.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xie, Xm., Wang, YF., Han, T. et al. Suicidality and its associated factors among mood disorder patients in emergency department in China: a comparative study using propensity score matching approach. Transl Psychiatry 13, 372 (2023). https://doi.org/10.1038/s41398-023-02675-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-023-02675-0