Abstract
To identify cognitive measures that may be particularly sensitive to early cognitive decline in preclinical Alzheimer’s disease (AD), we investigated the relation between genetic risk for AD and cognitive task performance in a large population-based cohort study. We measured performance on memory, processing speed, executive function, crystallized intelligence and eye movement tasks in 5182 participants of the Rhineland Study, aged 30 to 95 years. We quantified genetic risk for AD by creating three weighted polygenic risk scores (PRS) based on the genome-wide significant single-nucleotide polymorphisms coming from three different genetic association studies. We assessed the relation of AD PRS with cognitive performance using generalized linear models. Three PRS were associated with lower performance on the Corsi forward task, and two PRS were associated with a lower probability of correcting antisaccade errors, but none of these associations remained significant after correction for multiple testing. Associations between age and trail-making test A (TMT-A) performance were modified by AD genetic risk, with individuals at high genetic risk showing the strongest association. We conclude that no single measure of our cognitive test battery robustly captures genetic liability for AD as quantified by current PRS. However, Corsi forward performance and the probability of correcting antisaccade errors may represent promising candidates whose ability to capture genetic liability for AD should be investigated further. Additionally, our finding on TMT-A performance suggests that processing speed represents a sensitive marker of AD genetic risk in old age and supports the processing speed theory of age-related cognitive decline.
Similar content being viewed by others
Background
Alzheimer’s disease (AD) can roughly be divided into three clinical disease stages: a pre-symptomatic phase characterised by pathological brain changes, a prodromal phase characterised by subtle cognitive impairment and then lastly the dementia stage in which impairments occur in multiple domains and lead to loss of function [1]. As only 10–15% of individuals with amnestic mild cognitive impairment (MCI) develop AD each year [2], prediction of disease progression is of great interest to identify those individuals best suited for disease-delaying interventions, such as drug trials [3]. A meta-analysis found that particularly episodic verbal memory performance (e.g., delayed recall of a word list) and performance in language tasks that implicate semantic memory and executive function (e.g., the word fluency task) have high predictive accuracy for disease progression [4].
Eye movement assessment may be an alternative promising method to identify individuals at high risk for AD as it provides language-independent and culture-fair measures [5, 6] of multiple cognitive, perceptual and motor processes, including attention, processing speed, motion processing, working memory, learning and inhibition [7, 8]. In people with AD, instability of fixation [9,10,11] and deficits in the prosaccade [9, 12,13,14], antisaccade [12,13,14,15,16] and smooth pursuit tasks [16, 17] have been reported.
In the prosaccade task, participants are asked to perform a saccade, i.e., a rapid eye movement executed to bring an object of interest onto the fovea, towards a sudden-onset peripheral target. Prosaccade tasks measure overt attention and response speed [18], and individuals with AD were found to have longer latencies, i.e., longer reaction times for the initiation of a saccade towards the peripheral target, compared to healthy controls [12,13,14]. The antisaccade task has the same task design as the prosaccade task but participants are asked to execute their first saccade in each trial in the opposite direction of the peripheral target [19]. In this task, which is a good measure of inhibitory control [20], individuals with AD and MCI have consistently been found to make more direction errors compared to controls, i.e., a first saccade within a trial towards the target instead of towards its mirror position [12, 14]. Additionally, they are also less likely to correct their direction errors than controls [13, 15, 16]. For antisaccade latencies, the majority of studies reported higher latencies in AD [13, 14]. Moreover, in both saccade tasks, individuals with AD and amnestic MCI were found to perform hypometric saccades, which is reflected by a low value in the spatial accuracy measure called amplitude gain (amplitude of the eye movement divided by the amplitude of the target movement) and is accompanied by a high spatial error [9, 14, 21]. Research on whether saccade velocity and antisaccade costs (antisaccade latency minus prosaccade latency) differ between individuals with AD and healthy controls is still largely lacking [14], but some evidence suggests that performance in these measures may also be impaired in AD [13, 21].
Smooth pursuit eye movements (SPEMs) are performed to keep a slowly moving object on the fovea [22]. SPEMs have been found to have a lower velocity gain (ratio of eye velocity to target velocity) in AD [16, 17].
Importantly, performance in many oculomotor measures has been found to correlate with dementia severity, for example, instability of fixation [11, 23], prosaccade and antisaccade latency and amplitude gain [11, 21, 24], antisaccade direction error rate [25, 26] and correction rate [24]. Additionally, some studies have found that oculomotor performance may also help to differentiate between individuals with amnestic MCI and non-amnestic MCI [24, 27]. This may be relevant for predicting disease progression to AD, as individuals with amnestic MCI seem to be more likely to develop AD than individuals with non-amnestic MCI [28]. However, the usefulness of eye movements in identifying individuals at high risk for AD remains largely unexplored.
Genetic factors play a substantial role in the development of AD [29]. Polygenic risk scores (PRS) for AD, which represent the weighted sum of AD risk alleles that an individual carries, are well-suited to quantify genetic risk for AD as they account for the complex polygenic nature of AD [30].
Studies on the association between AD PRS and performance in classical cognitive tests have been conducted in samples including mainly older individuals without dementia or a mixture of individuals with MCI and individuals without dementia. AD PRS have been found to be significantly associated with both baseline episodic verbal memory performance [31,32,33] and longitudinal decline in episodic verbal memory [32,33,34,35], yet other studies could not confirm these findings in individuals with MCI or healthy participants [36, 37]. AD PRS were not associated with baseline working memory in most studies [33, 37], although working memory was found to deteriorate faster with higher PRS [34, 35]. Similarly, AD PRS were not associated with baseline performance in processing speed in several population-based studies [31, 33], except for a subgroup of 70 to 99-year-olds [31]. However, AD PRS were related to decline in processing speed [34, 35]. Studies examining the relation between AD PRS and baseline executive function either reported negative [31] or no associations[32, 37], whereas studies exploring the relation between AD PRS and longitudinal change in executive function were inconclusive [38, 39]. We are only aware of one study that investigated the relation between genetic risk for AD and eye movement performance [18]. That study found that antisaccade performance was similar between apolipoprotein E (APOE) ε4 carriers and non-carriers, yet APOE ε4 carriers performed worse on the prosaccade task. However, the sample size was small (N = 97), the participants were relatively young (17–35 years) and AD genetic risk was only based on APOE ε4 carrier status [18].
Here, we aimed to assess which, if any, cognitive measures are sensitive to genetic susceptibility for AD in a large, population-based sample including a wide age range. We investigated the relation with both classical tests of cognitive function and eye movement performance. Additionally, we investigated whether genetic liability for AD modifies the association between age and cognitive performance.
Materials and methods
Participants
We used baseline data from the Rhineland Study, a community-based cohort study that includes inhabitants aged ≥30 years (current age range: 30 to 95 years) from two geographically defined areas in Bonn, Germany. The only exclusion criterion is not having sufficient command of the German language to provide written informed consent. The ethics committee of the Medical Faculty of the University of Bonn approved the study that was carried out in accordance with the recommendations of the International Council for Harmonisation Good Clinical Practice standards (ICH-GCP). Of originally 5801 participants who provided blood samples between March 2016 and October 2021, 5189 remained after quality control of genetic data (see Section 2.2). Of those, 5182 had data in at least one cognitive task and were therefore included in the analyses.
Genetic data and polygenic risk scores
Blood samples were genotyped using Illumina Omni-2.5 exome arrays containing 2,612,357 single-nucleotide polymorphisms (SNPs). Genotype data were processed using GenomeStudio (version 2.0.5) and quality controlled using PLINK software (version 1.9). SNP exclusion criteria were Hardy-Weinberg disequilibrium (p < 1*10−6), minor allele frequency, (<0.01) and poor genotyping rate (<99%). Participants with poor DNA samples were excluded, which comprised 41 cases with poor call rate (<95%), 86 cases with abnormal heterozygosity, 290 cases with cryptic relatedness and 30 cases with gender mismatch. Because variation in population structure can cause systematic differences in allele frequencies [40], we used EIGENSTRAT (version 16000), which uses principal components to detect and correct for variation in population structure [40] (exclusion of N = 165 participants). Finally, we imputed missing SNPs based on the 1000 Genomes reference panel [41] using IMPUTE (version 2) [42]. To include only SNPs with high imputation quality, we checked for an info score metric greater than 0.3 as this value is considered to indicate reliable imputation quality [43].
Using PLINK (version 1.9), we created three different weighted AD PRS scores based on the genome-wide significant SNPs (i.e., those SNPs that had a p-value below 5*10−8 in the respective genome-wide association study (GWAS)). One PRS (PRSJansen) was created based on 29 genome-wide significant SNPs that were found in the meta-analysis by Jansen et al. in 2019 [44] (https://ctg.cncr.nl/software/summary_statistics; retrieved on January 15, 2021). The two additional PRS scores were created based on the genome-wide significant SNPs identified in two more recent meta-analyses by Wightman et al. [45] (PRSWightman) and Schwartzentruber et al. [46] (PRSSchwartzentruber). The study by Wightman et al. [45] is an extension of the study by Jansen et al. [44]. This study included a larger number of participants in one of the included cohorts as well as data from 12 additional cohorts (in total: N = 1,126,563 participants), and identified 38 risk loci. However, the authors could only provide us with the beta estimates from the summary statistics excluding the UK biobank (N = 364,859) and the 23andMe data (N = 363,646). Thus, we compared the signs of the z-scores they had reported for the original data set with those of the beta estimates they had provided and found that they were consistent. Additionally, one SNP (rs115186657) was missing in the summary statistics that they had provided and one SNP (rs2632516) was not available in our data. Therefore, we were able to include 36 SNPs in PRSWightman. To create PRSSchwartzentruber, we used all 37 risk loci for AD that were identified in the meta-analysis by Schwartzentruber et al. [46]. This meta-analysis combined the data of the study by Kunkle et al. from 2019 [47] and the updated results of a GWAS study of UK Biobank participants with a family history of AD. Earlier results from the GWAS analysis of the UK Biobank AD proxy cases were also included in the Jansen et al. publication [44]. PRSWightman and PRSSchwartzentruber were highly correlated with each other (Pearson’s r = 0.95) but their correlations were lower with PRSJansen (PRSWightman: r = 0.60; PRSSchwartzentruber: r = 0.63). This may be due to the fact that the two more recent GWAS only partially replicated the genome-wide significant loci reported by Jansen et al. [44] (Schwartzentruber: replication of 23 loci out of 29 from Jansen; Wightman: replication of 22 loci out of 29 from Jansen).
Outcome measures
We measured cognitive performance using classical tests of working memory, episodic verbal memory, processing speed, executive function and crystallized intelligence, along with an eye movement test battery. The examinations were administered following a standardized procedure by certified study technicians. Working memory was assessed with the forward and backward digit span task and the forward and backward Corsi block-tapping test (Corsi), adapted from the PEBL battery [48]. The Auditory Verbal Learning and Memory Test (AVLT) was used to assess episodic verbal memory (immediate recall: sum of correctly recalled nouns in the first five trials, delayed recall: number of correctly recalled words after a time delay of 20 to 30 min) [49]. Processing speed was measured with a numbers-only trail-making test (TMT-A: time to completion). Executive function was assessed with a 60 s categorical word fluency task (number of uniquely named animals) and a number-and-letters trail-making test (TMT-B: time to completion). Crystallized intelligence was measured with the 37-item Mehrfachwahl-Wortschatz-Intelligenztest (MWT-B), a vocabulary test in which participants had to select an existing German word among four non-words in each of 37 trials [50].
The eye movement test battery consisted of fixation, SPEM, prosaccade and antisaccade tasks. For recording of eye movements, we used video-based infrared oculography (EyeLink 1000 and EyeLink 1000 Plus; SR Research Ltd) at 1000 Hz. Fixations were defined as periods of at least 100 ms duration without blinks or saccades directed toward the target (a white circle 0.35° in diameter on black background). The target appeared first in the centre (x = 0°, y = 0°) for 5 s and then in a random order for 10 s each at the top (x = 0°, y = 9.63°), bottom (x = 0°, y = −9.63°), left (x = −9.63°, y = 0°), or right (x = 9.63°, y = 0°), always returning to the centre after each of these four eccentric locations. Thus, the central position had to be fixated four times in total. To obtain measures for fixation stability, we calculated the mean spatial error of gaze position (in degree of visual angle), mean saccade rate (saccades/second) and mean blink rate (blinks/second) during fixation. In the 21 s long SPEM task, the target started in the centre and then moved horizontally for ten full cycles in a sinusoidal waveform between ±9.63° at a frequency of 0.5 Hz. All eye movements with velocity <30°/s and duration ≥50 ms were classified as SPEMs. We determined the mean SPEM gain for the middle two quarters of each half-cycle of target motion (left to right or right to left) separately and then took the average of these values to calculate the mean velocity gain (in %). In all tasks, saccades were defined as eye movements with an amplitude >1° and either a velocity ≥60°/s or a velocity ≥22°/s and an acceleration ≥3800°/s2. We calculated the mean saccade rate (in saccades/second) during smooth pursuit. Prosaccade and antisaccade tasks consisted of 30 trials each (plus six antisaccade practice trials). In each trial, the target appeared first in the centre for a random duration of 1–2 s (average 1.5 s) and then stepped randomly to the left or right (x = ±9.63°, y = 0°, 15 times per side), where it remained for 1 s before returning to the centre for the next trial. For both saccade tasks, we calculated mean latencies (in ms), the two spatial accuracy measures amplitude gain and spatial error (both in %), and amplitude-adjusted and unadjusted peak velocities (in degree of visual angle/s) for valid trials with a directionally correct initial saccade. For the antisaccade task, we additionally calculated costs (in ms), direction error rate (in %), and correction rate (the percentage of direction errors corrected by participants who made at least 5 antisaccade direction errors by performing a saccade toward the mirror position that crossed at least the midline) for valid trials. Trials were defined as valid when the fixation on the central fixation point started at least 100 ms before peripheral target onset and was no more than 3° off the fixation point. Further, the initial saccade had to end before the peripheral target timed out and saccades with amplitude <1° or latency <80 ms were excluded. Additionally, no saccade or blink was allowed to occur during this period. To obtain reliable data, there had to be ≥7 valid and correct trials for prosaccade and antisaccade outcomes, except for the direction error and correction rate, for which only the criterion of valid but not correct trials applied. Additionally, for all antisaccade outcomes, at least one corrective saccade had to occur in case of ≥5 direction errors. A more detailed description of the oculomotor data acquisition can be found in a previous publication [51].
Statistical analyses
Statistical analyses were performed in RStudio (version 1.3.959, R-base version 4.0.3) using a two-sided significance test with an alpha level of 0.05. We assessed the associations between genetic risk for AD and cognitive performance separately for the three different AD PRS scores using multivariable linear or one-inflated beta regression models for each cognitive outcome. Models included z-standardized AD PRS as the predictor variable and were adjusted for age, age2 and sex, using mean-centred age to reduce collinearity between the main and quadratic term [52]. In order to correct for population stratification, we additionally adjusted for the first six genetic principal components [40]. We imputed missing covariate data using predictive mean matching (Hmisc package, 10 bootstrap replicates). We report unadjusted and false discovery rate adjusted (FDR-adjusted, N = 28 comparisons) p-values. We were particularly interested in cognitive outcomes that were consistently associated with all three different PRS to identify the most robust cognitive indicators of genetic risk for AD.
As age is a key risk factor for AD [53], we further examined whether genetic risk for AD modified the associations between age and cognitive outcomes by including PRS*age and PRS*age2 in the models and comparing the model fit with a likelihood ratio test. In case of significant interactions, we plotted the association between age and the respective cognitive outcome for three different PRS groups (low: z-standardised PRS score below −1; medium: z-standardised PRS score between −1 and 1; high: z-standardized PRS score above 1) separately to visualize how age interacts with genetic susceptibility to influence cognitive decline. Additionally, we tested differences in the slopes between the three PRS groups using Tukey post-hoc tests (pairs-function of the emmeans package [54] in R).
All models were checked for multicollinearity (variance inflation factor, R package car, vif-function), homoscedasticity (scale-location plot) and normality of residuals (quantile-quantile-plot). Because the normality assumption was violated for performance in TMT-A and TMT-B, prosaccade and antisaccade spatial error, and the three fixation outcomes spatial error, saccade rate and blink rate, we log-transformed those outcome variables. Because severe skewness of performance in antisaccade correction rate could not be reduced by log-transformation, we used a one-inflated beta regression model (gamlss package) instead, which is a mixture model consisting of a logistic regression model and a beta regression model. The logistic regression part of the one-inflated beta regression models whether or not AD PRS is associated with the probability of correcting all versus not correcting all antisaccade direction errors. In a second step, the beta regression model part tests whether AD PRS is associated with the percentage of uncorrected antisaccade direction errors in those individuals who did not correct all of their antisaccade direction errors.
We additionally performed a post-hoc power analysis using G-Power (version 3.1) [55] to evaluate which effect sizes for the associations between AD PRS and cognitive outcomes we would be able to detect with our sample size with a statistical power of between 80% to 90%. For this, we performed an F-test with one predictor, setting the sample size to 5182 participants, and the type I error rate to 0.05.
Results
Study sample
Sample characteristics are displayed in Table 1. Participants were overall highly educated and only 0.1% reported a diagnosis of AD. The eye movement measure antisaccade correction rate was computed for 3053 participants, representing the number of participants who made at least 5 antisaccade direction errors and corrected at least one of these direction errors. Of these 3053 participants, 677 participants did not correct all of their antisaccade direction errors.
Associations between AD PRS and cognitive performance
The associations between AD PRSJansen, PRSWightman, PRSSchwartzentruber and cognitive outcomes are displayed in Table 2.
Higher genetic risk for AD was significantly associated with lower performance in the Corsi forward task across all three AD PRS scores but these associations did not remain significant after correction for multiple testing. Additionally, before correcting for multiple testing, a higher PRSJansen score was associated with lower saccade frequency in the smooth pursuit task, higher prosaccade latency, and a lower probability of correcting all antisaccade direction errors (odds ratio and 95% confidence interval (OR and 95%-CI): 0.884 (0.810–0.964); p = 0.005; FDR-adjusted p = 0.140), but not with the proportion of uncorrected errors in those participants who did not correct all of their direction errors (OR and 95%-CI: 0.997 (0.943–1.054); p = 0.908). The uncorrected p-value also indicated that PRSSchwartzentruber was associated with a lower probability of correcting all antisaccade direction errors (OR and 95%-CI: 0.916 (0.840–0.999); p = 0.047; FDR-adjusted p = 0.235), but not with the percentage of uncorrected direction errors in those who did not correct all of their antisaccade direction errors (OR and 95%-CI: 0.990 (0.935–1.048); p = 0.727). As for the other two PRS, only the uncorrected p-values indicated that a higher PRSWightman score was associated with better performance in the digit span backward and lower TMT-A performance. PRSWightman was neither associated with the probability of correcting all versus not all antisaccade direction errors (OR and 95%-CI: 0.920 (0.844–1.003); p = 0.058), nor with the percentage of uncorrected errors in those who did not correct all of their antisaccade errors (OR and 95%-CI: 0.988 (0.933–1.047); p = 0.685).
Exclusion of AD cases (N = 5, Table 1) from the sample, or adding educational level as an additional covariate, did not materially change the results (data not shown).
Interaction effects
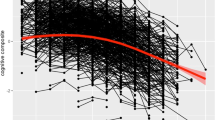
We found significant interactions between the three different PRS and age and age2 for TMT-A performance that remained significant after correcting for multiple testing (Table 3). For AVLT (immediate and delayed recall), the interactions between PRS and age and age2 were also significant for all three different PRS, but only the interactions between PRSJansen and age and age2 for AVLT immediate recall remained significant after correcting for multiple testing. In addition, we found significant interaction effects between PRSWightman, and PRSSchwartzentruber and age and age2 for saccade frequency during smooth pursuit, but they did not survive correction for multiple testing. Visualisation of the interaction effects showed that individuals with the highest genetic risk for AD showed the strongest age-related decline in AVLT (immediate and delayed recall) and TMT A performances (Fig. 1). For saccade frequency during smooth pursuit, the scatterplot did not reveal a clear pattern (Fig. 1). Post-hoc comparisons using the Tukey test revealed that delayed recall performance in individuals at highest genetic risk, based on PRSWightman and PRSSchwartzentruber was worse compared to those in the medium (PRSWightman model: p = 0.001, PRSSchwartzentruber model: p = 0.025) and low (PRSWightman model: p = 0.017, PRSSchwartzentruber model: p = 0.031) genetic risk groups. Additionally, high genetic risk individuals performed worse than medium (PRSWightman model: p = 0.018, PRSSchwartzentruber model: p = 0.016) and low (PRSWightman model: p < 0.001, PRSJansen model: p = 0.003) genetic risk individuals in TMT-A performance. Further, in the PRSWightman model, medium genetic risk individuals differed from low genetic risk individuals in TMT-A performance (p = 0.016). All other post-hoc comparisons were non-significant.
The scatterplots show how the associations between age and different cognitive outcomes vary with genetic risk for Alzheimer’s disease. Each column represents a different polygenic risk score and each row represents a cognitive outcome. The colours represent three different genetic risk groups for Alzheimer’s disease (orange = high risk/ z-standardized PRS score above 1; blue = medium risk/ z-standardised PRS score between −1 and 1; green = low risk/ z-standardised PRS score below −1). For each genetic risk group there exists one superimposed function for the development of the cognitive outcome across the adult life span. The functions were obtained from a multivariable regression model with the following formula: cognitive outcome ~ b0 + age*b1 + age2*b2 + residual error. The grey area around the risk group-specific regression lines indicates the 95% confidence interval in each case. AVLT Auditory Verbal Learning and Memory Test; TMT-A Trail-making test A, N = number.
Statistical power analysis
Our post-hoc analysis showed that we could detect effect sizes (Cohen’s f2) of 0.0020, 0.0015 and 0.0010 with a statistical power of 90%, 80% and 62%, respectively. To illustrate the magnitude of the effect sizes that we were able to detect, we calculated the effect sizes for the associations between the three different AD PRS scores and Corsi forward performance. The effect sizes were f2 = 0.0011 for PRSJansen, f2 = 0.0010 for PRSWightman and f2 = 0.0016 for PRSSchwartzentruber.
Discussion
We found that genetic risk for AD was not significantly associated with any cognitive or oculomotor measure from our test battery after correcting for multiple testing. However, prior to correcting for multiple testing, all three AD PRS were significantly associated with lower performance in the Corsi forward working memory task, and two AD PRS with a lower probability of correcting versus not correcting all antisaccade errors. Further, the association between age and TMT-A performance varied with genetic risk for AD and was strongest in those individuals at highest genetic risk for AD.
The unadjusted p-values indicated an association between all three AD PRS and visuo-spatial working memory performance as measured by the Corsi forward task, which has not been found in previous studies [33, 37]. We found that the associations between AD PRS and Corsi forward performance did not vary with age, suggesting that the discrepancy between our and previous studies is unlikely to be due to differences in the age distribution. One reason for this finding may be that we created the PRS based on more recent genome-wide association studies and, therefore, included at least seven more SNPs in our PRS than previous studies. However, a previous study comparing visuo-spatial working memory performance between homozygous APOE ε4 carriers and non-ε4 carriers reported lower Corsi performance (combined score for forward and backward performance) in homozygous APOE ε4 carriers [56]. Still, the associations between AD PRS and Corsi forward performance did not remain significant after correcting for multiple testing. FDR-correction probably was too conservative as discussed further below this. Nevertheless, our results should be considered as suggestive until validated in independent studies. Concerning the other tests for visuo-spatial working memory, we found that a higher PRSWightman score was associated with a better digit span backward performance. However, this association was not found using PRSJansen and PRSSchwartzentruber, thus likely representing a false positive observation.
Regarding associations between genetic risk for AD and episodic verbal memory performance, previous studies have reported significant associations [31,32,33], which we could not confirm across the entire range of 30+ year-olds. However, our results suggest that the association between age and AVLT immediate recall varied with genetic risk for AD (Table 3), and was strongest in those individuals at highest genetic risk for AD (Fig. 1). For PRSJansen, this interaction effect remained significant after correction for multiple testing. Additionally, the association between age and AVLT delayed recall was also modified by genetic risk for AD, with AVLT delayed recall declining strongest in those individuals at highest genetic risk for AD, as indicated by Fig. 1 and the results of Tukey post-hoc tests for PRSWightman and PRSSchwartzentruber. However, these interactions did not remain significant after correction for multiple testing. Thus, our findings overall suggest that differences in episodic verbal memory performance among the three genetic risk groups may become more pronounced at older ages, which is compatible with the finding that age is a major risk factor for AD [53].
Associations between all three PRS scores and TMT-A performance varied robustly with age, as the interaction terms remained significant even after correcting for multiple testing. We observed that differences in TMT-A performance among the three PRS groups were strongest at older ages (Fig. 1). Across the entire age range, only PRSWightman was associated with lower TMT-A performance, but this association did not remain significant after correction for multiple testing. A previous population-based study reported no association between AD PRS and processing speed across the sample but only in the 70- to 99-year-olds [31]. Thus, our results support the previous finding that associations between AD PRS and TMT-A performance are more likely to emerge in old age. Additionally, our robust finding that genetic risk for AD gradually affects the magnitude of age-related decline in processing speed, but not in other cognitive domains across the adult lifespan, supports Salthouse’s processing speed theory of age-related cognitive decline [57]. According to this theory, slowing of processing speed is the global mechanism underlying age-related cognitive decline [57]. This suggests that AD partly results from individuals at high genetic risk for AD experiencing a stronger age-related decline in processing speed compared to individuals at low genetic risk for AD, resulting in lower cognitive performance across all domains in the long term. Our finding is also in line with previous reports of AD PRS being related to longitudinal decline in processing speed [34, 35].
Consistent with some previous studies [32, 37], we found no associations between AD PRS and executive function, as measured by performance in TMT-B and the word fluency task. Associations between AD PRS and oculomotor measures had not been assessed before. Using AD PRSJansen, we found that higher genetic risk was associated with higher prosaccade latency, lower saccade frequency during pursuit, and lower antisaccade error correction probability. However, as neither of those associations could be found with the other two AD PRS scores and as none of the findings survived correction of multiple testing, they should be interpreted with caution as they may represent false positive findings.
Our finding of a lower probability of correcting antisaccade errors in individuals with higher genetic risk for AD may be more robust as it was found using both PRSJansen and PRSSchwartzentruber. Still, neither association remained significant after correction for multiple testing. The association between genetic risk for AD and a lower probability of correcting antisaccade errors agrees with previous reports of lower antisaccade error correction probabilities in individuals with AD and MCI [13, 15, 16]. Moreover, scores in dementia screening tests have also been found to correlate with the probability of correcting antisaccade errors [24]. Still, the association between genetic risk for AD and antisaccade corrections probability requires further investigation as it was not found using PRSWightman and did not survive correction for multiple testing.
A potential limitation of our study is lack of longitudinal data, precluding assessment of the associations between AD PRS and change in cognitive outcomes. However, our sample included a wide age range, which allowed us to investigate associations between AD PRS and cognitive outcomes across the adult lifespan, and how the associations between age and cognitive tests vary between different AD genetic risk groups. Further, we employed an extensive cognitive test battery including eye movement outcomes that were not part of the cognitive test batteries in previous large population studies.
Another potential limitation of our study relates to statistical power. The associations between AD PRS and cognitive measures did not remain significant after FDR-correction. However, our approach for correcting for multiple comparisons may have been too conservative as it is only appropriate in case of disjunction testing [58]. On the one hand, we wanted to infer from the individual cognitive measures which cognitive domain is most sensitive to capturing genetic risk for AD. In this scenario, one could argue that our testing approach represents disjunction testing, as a significant association between genetic risk and a cognitive measure would be taken as an indication that the represented cognitive domain in general is especially sensitive to capturing genetic risk for AD [58]. On the other hand, we aimed to identify the most sensitive individual cognitive measure of genetic risk for AD without making a general statement about the associated cognitive domain. This approach would clearly fall into the category of individual testing, for which correction for multiple testing is not appropriate [58]. Thus, as long as we do not overgeneralize from single tests to cognitive domains, correction for multiple testing may be too conservative. Importantly, we also conducted the analyses using three different AD PRS scores to identify the most consistent associations. Moreover, it should be noted that current AD PRS only explain about 7% of AD heritability at optimal p-value threshold for SNP inclusion [44], despite heritability estimates for AD ranging from 58% to 79% [59]. This may be due to PRS being based on summary statistics of GWAS that rely on conventional genotyping arrays that capture common variants but not rare or structural variants [29]. Finally, AD is a heterogeneous disease and influenced by a complex interplay between both genetic and environmental factors [60]. Thus, very strong associations between AD PRS and cognitive outcome are unlikely to occur, exemplified by the small effect sizes (Cohen’s f2 ≤ 0.0016) for the associations between the three different AD PRS scores and Corsi forward performance. Therefore, Corsi forward performance and the likelihood of correcting antisaccade errors may be promising candidate measures whose ability to capture the genetic predisposition to AD should be investigated further in future studies. Lastly, the suitability of TMT-A performance in detecting genetic liability for AD in old age also requires further investigation.
Conclusion
PRS for AD were not robustly associated with any of our cognitive and oculomotor measures. Of all our cognitive measures, Corsi forward performance and the probability of correcting antisaccade errors may be the most suitable candidates for capturing genetic liability for AD across the adult lifespan, but these associations require confirmation in independent samples. In addition, TMT-A, which measures processing speed performance, may be a sensitive marker of genetic susceptibility to AD in old age. Lastly, our finding of a stronger association between age and processing speed performance in individuals at high genetic risk for AD supports the processing speed theory of age-related cognitive decline by Salthouse, suggesting a decline in processing speed as the global mechanism underlying general cognitive decline.
Data availability
The datasets for this manuscript are not publicly available because of data protection regulations. Access to data can, however, be provided to scientists in accordance with the Rhineland Study’s Data Use and Access Policy. Requests to access the datasets should be directed to Dr Monique Breteler, RS-DUAC@dzne.de.
References
Jack CR Jr, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner W, et al. Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol. 2010;9:119–28.
Pandya SY, Clem MA, Silva LM, Woon FL. Does mild cognitive impairment always lead to dementia? A review. J Neurol Sci. 2016;369:57–62.
Anderson ND. State of the science on mild cognitive impairment (MCI). CNS Spectr. 2019;24:78–87.
Belleville S, Fouquet C, Hudon C, Zomahoun HTV, Croteau J. Neuropsychological measures that predict progression from mild cognitive impairment to Alzheimer’s type dementia in older adults: A systematic review and meta-analysis. Neuropsychol Rev. 2017;27:328–53.
Anderson TJ, MacAskill MR. Eye movements in patients with neurodegenerative disorders. Nat Rev Neurol. 2013;9:74–85.
Noiret N, Vigneron B, Diogo M, Vandel P, Laurent É. Saccadic eye movements: what do they tell us about aging cognition? Aging, Neuropsychol Cogn. 2017;24:575–99.
Hutton SB. Cognitive control of saccadic eye movements. Brain Cogn. 2008;68:327–40.
Massen C. Parallel programming of exogenous and endogenous components in the antisaccade task. Q J Exp Psychol Sect A Hum Exp Psychol. 2004;57:475–98.
Fletcher WA, Sharpe JA. Saccadic eye movement dysfunction in Alzheimer’s disease. Ann Neurol. 1986;20:464–71.
Jones A, Friedland RP, Koss B, Stark L, Thompkins-Ober BA. Saccadic intrusions in Alzheimer-type dementia. J Neurol. 1983;229:189–94.
Schewe HJ, Uebelhack R, Vohs K. Abnormality in saccadic eye movement in dementia. Eur Psychiatry. 1999;17:1–3.
Levy NK, Lavidor M, Vakil E. Prosaccade and antisaccade paradigms in persons with Alzheimer’s disease: a meta-analytic review. Neuropsychol Rev. 2018;28:16–31.
Noiret N, Carvalho N, Laurent É, Chopard G, Binetruy M, Nicolier M, et al. Saccadic eye movements and attentional control in Alzheimer’s disease. Arch Clin Neuropsychol. 2018;33:1–13.
Opwonya J, Doan DNT, Kim SG, Kim JIL, Ku B, Kim S et al. Saccadic eye movement in mild cognitive impairment and Alzheimer’s disease: A systematic review and meta-analysis. Neuropsychol Rev. https://doi.org/10.1007/s11065-021-09495-3 2021.
Crawford TJ, Higham S, Mayes J, Dale M, Shaunak S, Lekwuwa G. The role of working memory and attentional disengagement on inhibitory control: effects of aging and Alzheimer’s disease. Age (Omaha). 2013;35:1637–50.
Garbutt S, Matlin A, Hellmuth J, Schenk AK, Johnson JK, Rosen H, et al. Oculomotor function in frontotemporal lobar degeneration, related disorders and Alzheimer’s disease. Brain. 2008;131:1268–81.
Fletcher WA, Sharpe JA. Smooth pursuit dysfunction in Alzheimer’s disease. Neurology. 1988;38:272–7.
Niechwiej-Szwedo E, Tapper A, Gonzalez D, Bradley RM, Duncan R. Saccade latency delays in young apolipoprotein E (APOE) epsilon 4 carriers. Behav Brain Res. 2018;353:91–97.
Hallett PE. Primary and secondary saccades to goals defined by instructions. Vis Res. 1978;18:1279–96.
Mirsky JB, Heuer HW, Jafari A, Kramer JH, Schenk K, Viskontas IV, et al. Anti-saccade performance predicts executive function and brain structure in normal elders. Cogn Behav Neurol. 2011;24:50–8.
Chehrehnegar N, Nejati V, Shati M, Esmaeili M, Rezvani Z, Haghi M, et al. Behavioral and cognitive markers of mild cognitive impairment: diagnostic value of saccadic eye movements and Simon task. Aging Clin Exp Res. 2019;31:1591–1600.
Lencer R, Trillenberg P. Neurophysiology and neuroanatomy of smooth pursuit in humans. Brain Cogn. 2008;68:219–28.
Bylsma FW, Rasmusson DX, Rebok GW, Keyl PM, Tune L, Brandt J. Changes in visual fixation and saccadic eye movements in Alzheimer’s disease. Int J Psychophysiol. 1995;19:33–40.
Koçoğlu K, Hodgson TL, Eraslan Boz H, Akdal G. Deficits in saccadic eye movements differ between subtypes of patients with mild cognitive impairment. J Clin Exp Neuropsychol. 2021;43:187–98.
Shafiq-Antonacci R, Maruff P, Masters C, Currie J. Spectrum of saccade system function in Alzheimer disease. Arch Neurol. 2003;60:1272–8.
Currie J, Ramsden B, Mcarthur C, Maruff P. Validation of a clinical antisaccadic eye movement test in the assessment of dementia. Arch Neurol. 1991;48:644–8.
Wilcockson TDW, Mardanbegi D, Xia B, Taylor S, Sawyer P, Gellersen HW, et al. Abnormalities of saccadic eye movements in dementia due to Alzheimer’s disease and mild cognitive impairment. Aging (Albany NY). 2019;11:5389–98.
Oltra-Cucarella J, Ferrer-Cascales R, Alegret M, Gasparini R, Díaz-Ortiz LM, Ríos R, et al. Risk of progression to Alzheimer’s disease for different neuropsychological Mild Cognitive Impairment subtypes: a hierarchical meta-analysis of longitudinal studies. Psychol Aging. 2018;33:1007–21.
Sims R, Hill M, Williams J. The multiplex model of the genetics of Alzheimer’s disease. Nat Neurosci. 2020;23:311–22.
Escott-Price V, Sims R, Bannister C, Harold D, Vronskaya M, Majounie E, et al. Common polygenic variation enhances risk prediction for Alzheimer’s disease. Brain. 2015;138:3673–84.
Verhaaren BFJ, Vernooij MW, Koudstaal PJ, Uitterlinden AG, Van Duijn CM, Hofman A, et al. Alzheimer’s disease genes and cognition in the nondemented general population. Biol Psychiatry. 2013;73:429–34.
Mormino EC, Sperling RA, Holmes AJ, Buckner RL, De Jager PL, Smoller JW, et al. Polygenic risk of Alzheimer disease is associated with early- and late-life processes. Neurology. 2016;87:481–8.
Andrews SJ, Das D, Cherbuin N, Anstey KJ, Easteal S. Association of genetic risk factors with cognitive decline: the PATH through life project. Neurobiol Aging. 2016;41:150–8.
Felsky D, Patrick E, Schneider JA, Mostafavi S, Gaiteri C, Patsopoulos N, et al. Polygenic analysis of inflammatory disease variants and effects on microglia in the aging brain. Mol Neurodegener. 2018;13:1–10.
Tasaki S, Gaiteri C, Mostafavi S, De Jager PL, Bennett DA. The molecular and neuropathological consequences of genetic risk for Alzheimer’s dementia. Front Neurosci. 2018;12:699.
Louwersheimer E, Wolfsgruber S, Espinosa A, Lacour A, Heilmann-Heimbach S, Alegret M, et al. Alzheimer’s disease risk variants modulate endophenotypes in mild cognitive impairment. Alzheimer’s Dement. 2016;12:872–81.
Darst BF, Koscik RL, Racine AM, Oh JM, Krause RA, Carsson CM, et al. Pathway-specific polygenic risk scores as predictors of β-amyloid deposition and cognitive function in a sample at increased risk for Alzheimer’s disease. J Alzheimers Dis. 2017;55:473–84.
Ridge PG, Mukherjee S, Crane PK, Kauwe JSK. Alzheimer’s disease: analyzing the missing heritability. PLoS One. 2013;8:1–10.
Vivot A, Glymour MM, Tzourio C, Amouyel P, Chêne G, Dufouil C. Association of Alzheimer’s related genotypes with cognitive decline in multiple domains: results from the Three-City Dijon study. Mol Psychiatry. 2015;20:1173–8.
Price AL, Patterson NJ, Plenge RM, Weinblatt ME, Shadick NA, Reich D. Principal components analysis corrects for stratification in genome-wide association studies. Nat Genet. 2006;38:904–9.
Auton A, Abecasis GR, Altshuler DM, Durbin RM, Bentley DR, Chakravarti A, et al. A global reference for human genetic variation. Nature. 2015;526:68–74.
Howie BN, Donnelly P, Marchini J. A flexible and accurate genotype imputation method for the next generation of genome-wide association studies. PLoS Genet. 2009;5:e1000529.
Verma SS, de Andrade M, Tromp G, Kuivaniemi H, Pugh E, Namjou-Khales B, et al. Imputation and quality control steps for combining multiple genome-wide datasets. Front Genet. 2014;5:370.
Jansen IE, Savage JE, Watanabe K, Bryois J, Williams DM, Steinberg S, et al. Genome-wide meta-analysis identifies new loci and functional pathways influencing Alzheimer’s disease risk. Nat Genet. 2019;51:404–13.
Wightman DP, Jansen IE, Savage JE, Shadrin AA, Bahrami S, Holland D, et al. A genome-wide association study with 1,126,563 individuals identifies new risk loci for Alzheimer’s disease. Nat Genet. 2021;53:1276–82.
Schwartzentruber J, Cooper S, Liu JZ, Barrio-hernandez I, Bello E, Kumasaka N, et al. Genome-wide meta-analysis, fine-mapping and integrative prioritization implicate new Alzheimer’s disease risk genes. Nat Genet. 2021;53:392–402.
Kunkle BW, Grenier-Boley B, Sims R, Bis JC, Damotte V, Naj AC, et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. Nat Genet. 2019;51:414–30.
Mueller ST, Piper BJ. The psychology experiment building language (PEBL) and PEBL test battery. J Neurosci Methods. 2014;222:250–9.
Boenniger MM, Staerk C, Coors A, Huijbers W, Ettinger U, Breteler MMB. Ten parallel German versions of Rey’s Auditory Verbal Learning Test: age and sex effects in 4000 adults of the Rhineland Study. J Clin Exp Neuropsychol. 2021;43:637–53.
Lehrl S. Mehrfachwahl-Wortschatz-Intelligenztest MWT-B. Spitta Verlag: Balingen, Germany, 2005.
Coors A, Merten N, Ward DD, Schmid M, Breteler MMB, Ettinger U. Strong age but weak sex effects in eye movement performance in the general adult population: evidence from the Rhineland Study. Vis Res. 2021;178:124–33.
Iacobucci D, Schneider MJ, Popovich DL, Bakamitsos GA. Mean centering helps alleviate “micro” but not “macro” multicollinearity. Behav Res Methods. 2016;48:1308–17.
Niu H, Álvarez-Álvarez I, Guillén-Grima F, Aguinaga-Ontoso I. Prevalence and incidence of Alzheimer’s disease in Europe: A meta-Anal NeurolíA. 2017;32:523–32.
Lenth R V. emmeans: Estimated marginal means, aka least-squares means. 2022. https://cran.r-project.org/package=emmeans.
Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–60.
Goltermann J, Redlich R, Dohm K, Zaremba D, Repple J, Kaehler C, et al. Apolipoprotein E homozygous ε4 allele status: A deteriorating effect on visuospatial working memory and global brain structure. Front Neurol. 2019;10:1–11.
Salthouse TA. The nature of the influence of speed on adult age differences in cognition. Dev Psychol. 1994;30:240–59.
Rubin M. When to adjust alpha during multiple testing: a consideration of disjunction, conjunction, and individual testing. Synthese. 2021;199:10969–11000.
Gatz M, Reynolds CA, Fratiglioni L, Johansson B, Mortimer JA, Berg S, et al. Role of genes and environments for explaining Alzheimer disease. Arch Gen Psychiatry. 2006;63:168–74.
Dunn AR, O’Connell KMS, Kaczorowski CC. Gene-by-environment interactions in Alzheimer’s disease and Parkinson’s disease. Neurosci Biobehav Rev. 2019;103:73–80.
Acknowledgements
We thank Christof Meigen, André Medek, Benjamin Meier, Mohammad Shahid, Thomas Schmidt, Simon Harmata, Jannis Warnat, Fabrice Hess, Astrid Seidel, Sam Hutton and Kurt Debono for their contributions in data handling and management and/or excellent technical support with the eye-tracker. We also thank all the staff members and participants of the Rhineland Study.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
AC: conceptualization, methodology, validation, formal analysis, investigation, data curation, writing – original draft, writing – review & editing. M-AI: conceptualization, methodology, writing – review & editing. MMB: investigation, writing – review & editing. NAA: conceptualization, methodology, writing – review & editing. MMBB: conceptualization, methodology, validation, resources, writing – review & editing, supervision, project administration, funding acquisition. UE: conceptualization, methodology, validation, writing – review & editing, supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Coors, A., Imtiaz, MA., Boenniger, M.M. et al. Associations of genetic liability for Alzheimer’s disease with cognition and eye movements in a large, population-based cohort study. Transl Psychiatry 12, 337 (2022). https://doi.org/10.1038/s41398-022-02093-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-022-02093-8