Abstract
COVID-19 has imposed a very substantial direct threat to the physical health of those infected, although the corollary impact on mental health may be even more burdensome. Here we focus on assessing the mental health impact of COVID-19 and of other epidemics in the community. We searched five electronic databases until December 9, 2020, for all peer-reviewed original studies reporting any prevalence or correlates of mental disorders in the general population following novel epidemics in English, Chinese or Portuguese. We synthesised prevalence estimates from probability samples during COVID-19 and past epidemics. The meta-analytical effect size was the prevalence of relevant outcomes, estimated via random-effects model. I2 statistics, Doi plots and the LFK index were used to examine heterogeneity and publication bias. This study is pre-registered with PROSPERO, CRD42020179105. We identified 255 eligible studies from 50 countries on: COVID-19 (n = 247 studies), severe acute respiratory syndrome (SARS; n = 5), Ebola virus disease (n = 2), and 1918 influenza (n = 1). During COVID-19, we estimated the point prevalence for probable anxiety (20.7%, 95% CI 12.9–29.7), probable depression (18.1%, 13.0–23.9), and psychological distress (13.0%, 0–34.1). Correlates for poorer mental health include female sex, lower income, pre-existing medical conditions, perceived risk of infection, exhibiting COVID-19-like symptoms, social media use, financial stress, and loneliness. Public trust in authorities, availability of accurate information, adoption of preventive measures and social support were associated with less morbidity. The mental health consequences of COVID-19 and other epidemics could be comparable to major disasters and armed conflicts. The considerable heterogeneity in our analysis indicates that more random samples are needed. Health-care professionals should be vigilant of the psychological toll of epidemics, including among those who have not been infected.
Similar content being viewed by others
Introduction
COVID-19 has disrupted most aspects of daily life and resulted in wide-ranging psychosocial and economic stressors including fear of disease, loss of loved ones, lockdowns, social isolation, school closures, and economic recession [1, 2]. Prior systematic reviews and meta-analyses on COVID-19 have summarised the early findings on mental health available from mostly convenience samples [3,4,5,6,7,8,9]. Here, we focus on the prevalence of mental health disorders in probability samples and those with pre-pandemic mental health measures [10].
Mental health consequences of novel epidemics have been examined since the 1918 influenza pandemic to more recently Ebola virus disease and past coronavirus epidemics: severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) [2]. Research on COVID-19 and future epidemics could benefit from drawing upon the decades of epidemics-related literature (e.g. study design, potential findings) [11,12,13]. Accordingly, we conducted a systematic review and meta-analysis of the impact of COVID-19 and past epidemics on population mental health.
Methods
We pre-registered the study protocol on PROSPERO (CRD42020179105) [14] and followed the PRISMA guideline.
Search strategy
We searched PubMed, PsycINFO, Embase, CINAHL Plus, and Web of Science from their inception until December 9, 2020. Detailed search strategy and selection criteria are shown in Tables S1 and S2. The scope of our review was the prevalence or correlates of mental disorders in the general population exposed to any droplet-transmissible and airborne-transmissible viral outbreaks, which included novel epidemics of influenza viruses, Ebola virus and coronavirus [13]. Examples were COVID-19, Ebola virus disease, MERS, avian influenza A(H7N9), pandemic influenza A(H1N1), avian influenza A(H5N1), SARS and 1918 influenza [13]. Due to the unprecedented number of COVID-19 studies [15], we narrowed our original inclusion criteria to focus on mental disorders, which may have more clinical utility than the level of symptoms during population shocks [16, 17]. Outcomes were specific mental disorders or clinically significant level of mental distress (hereafter referred to as “psychological distress”), which were assessed by clinician interviews, diagnostic interviews (e.g. SCID, CIDI), or screening tools validated against clinician/diagnostic interviews (e.g. Patient Health Questionnaire-9, Generalized Anxiety Disorder Scale-7, General Health Questionnaire-12). Other transdiagnostic outcomes (e.g. insomnia) were excluded, except suicidality which has been identified as an urgent research priority [18]. Definitions and standardised measures of these outcomes are summarised in Table S3. Only original research studies published in peer-reviewed journals were eligible. In addition to articles in English, we included articles in Chinese and Portuguese based on the languages that known by the authors. We excluded studies focusing on subgroups (e.g. university students), conference abstracts, qualitative studies and modelling studies. We searched the reference lists of the identified studies, grey literature, Google Scholar, and previous review articles to identify additional studies.
Data extraction
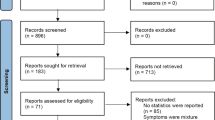
Six authors (CML, MKH, AAB, YW, MSC, and XF) worked independently in pairs for screening, data extraction, and evidence grading (Fig. 1) after training and concordance assessment. Any disagreements were first resolved by consensus, then by a third author. With a piloted form, we extracted data for setting, disease, phase of epidemic, study design, survey method, sampling, participation rate, sample size, age range of sample, measures, prevalence and correlates of outcomes, among others. We contacted authors for missing or incomplete prevalence data.
Evidence grading
We used the Newcastle-Ottawa Scale (NOS) recommended by the Cochrane collaboration to appraise study quality [19]. The NOS was modified for assessing cross-sectional studies with reference to previous adaptations (Table S4) [12, 20,21,22]. Total NOS scores ranged from 0 to 9 for longitudinal and case-control studies and from 0 to 6 for cross-sectional studies. Study quality was classified as low (0–3), medium (4–6), and high (7–9) [12]. We evaluated the certainty of evidence for each outcome from very low, low, moderate, to high using the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) [23].
Data synthesis
We prioritised methodologically sound studies in our data synthesis, given the large number of studies in the extant literature. Meta-analysis was added to this review, because we had identified a number of new probability samples after the PROSPERO registration. We synthesised prevalence estimates only from probability samples, which were recruited via any random sampling procedures (e.g., random-digit-dialling, address-based sampling) [10]. Correlates were summarised only when they were identified via multivariable analyses [24]. These included those consistently identified by at least two studies, and some others that were uniquely reported but may be potentially important predictors of mental disorders during epidemics. We tabulated the results by outcomes and epidemics if applicable. Meta-analysis was conducted using the double arcsine transformation [25]. We used a random-effects model that considers sample size and study quality [26]. The meta-analytical effect size was the pooled prevalence of relevant outcomes with 95% CI. We selected only studies comparable in terms of phase of epidemic (e.g. during, after epidemic) to reduce heterogeneity. In case of duplicate data, we included only the one with largest sample size. For cohort studies, we included only the first survey after the outbreak. Raw data for meta-analysis is provided in Table S5. Forest plots with I2 statistics were used to examine any study heterogeneity. Given the small number of probability samples, Doi plots and Luis Furuya-Kanamori (LFK) index were used to detect publication bias where applicable [27]. All statistical analyses were done by MetaXL 5.3 [28].
Results
Study characteristics
Of the 41,095 unique records screened, we identified 255 eligible studies that examined prevalence or correlates of mental disorders or suicidality during novel epidemics (Fig. 1). These included 247 studies on COVID-19 (97%) involving over 1.2 million participants and 48 countries (Table 1). A quarter of COVID-19 studies were conducted in China (n = 64), more than other individual countries worldwide (Fig. 2, Table S6). Nearly 90% (n = 220) of COVID-19 studies had used convenience samples or opt-in online panels, compared to 12.5% (n = 1) of studies on past epidemics.
A Number of confirmed Coronavirus Disease 2019 (COVID-19) cases as of January 21, 2021. B Number of published studies on COVID-19 and mental health as of December 9, 2020. C Ranking of countries based on panels (A) confirmed COVID-19 cases and (B) number of studies on COVID-19 and mental health. Data source: Center for Systems Science and Engineering at Johns Hopkins University. Grey regions indicate regions with no available data.
For all epidemics, we identified 33 studies (13%) that assessed prevalence of mental disorders or suicidality in probability samples or whole populations (Table S7) [29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61]. Nine of these studies reported pre-epidemic baseline prevalence of mental disorders [33, 35,36,37, 47, 51, 53, 55, 58], but six of these relied on other samples for baseline data. The remaining three studies examined psychological distress before and during COVID-19 using the same panel of individuals in the UK Household Longitudinal Study (Table 2) [47, 53, 55]. We included 15 studies for meta-analysis of prevalence estimates during epidemics (Table S5).
Assessment of mental health outcomes
Probable depression was most frequently assessed, followed by probable anxiety, suspected post-traumatic stress disorder (PTSD), and psychological distress (Table 1). We use the term probable as most studies used screening instruments. We used the term suspected PTSD as nearly all studies were conducted during epidemics, and often DSM Criterion A was not assessed or clearly defined. Table 2 lists the studies that assessed prevalence of mental disorders in probability samples during or after epidemics. Table 3 summarises the correlates consistently identified by at least two studies during COVID-19.
Anxiety
Prevalence
The prevalence of probable anxiety ranged from 14.0% to 32.8% in the general population during COVID-19 (Table 2) [29,30,31,32,33,34]. No eligible studies were identified for past epidemics. The pooled prevalence was 20.7% (95% CI 12.9–29.7), with high heterogeneity (I2 = 99%; Fig. S1) and major asymmetry indicated by the DOI plot and LFK index of −8.6 (Fig. S2). Anxiety levels appeared to be higher during COVID-19 compared to the reported baselines (Table 2) [33, 35]. In the US, anxiety prevalence has remained high five months into the COVID-19 epidemic, where anxiety was documented to have increased from 8.2% before the epidemic to 29.4% [33].
Correlates
During COVID-19, higher risk of probable anxiety was observed in females, those who were unemployed or lived alone (Table 3). Higher perceived susceptibility and severity [32, 62], having multiple COVID-19 risk factors [63], masks shortage [30], frequent traditional and social media exposure [64,65,66], lockdown or mass stay-at-home orders [67, 68], perceived inadequate housing conditions to cope with lockdowns [69], loneliness [70, 71], reduced outside or physical activities [68, 72], greater impact on daily life [62], and adverse economic impacts [62] were associated with probable anxiety. Higher resilience [73], social support [66], getting reliable, adequate and timely epidemic information [74], perceived effectiveness and adoption of physical distancing and personal preventive measures [32, 34], and having enough basic supplies [74] were associated with a lower risk of probable anxiety.
Depression
Prevalence
The prevalence of probable depression ranged from 9.5% to 27.8% in the general population during COVID-19 (Table 2) [29,30,31, 33,34,35,36,37,38,39,40, 50]. The pooled prevalence was 18.1% (95% CI 13.0–23.9), with high heterogeneity (I2 = 99%; Fig. S1) and major asymmetry indicated by the DOI plot and LFK index of −4.42 (Fig. S2). Compared to pre-COVID-19 periods, depression appeared to have increased during COVID-19 in Hong Kong (from 6.3% to 14.8%) and US (from 6.6% to 24.9%) [33, 35]. For past epidemics, probable depression was 3.7% in Taiwan one month after the SARS epidemic [40].
Correlates
During COVID-19, females, those who were unemployed or lived alone had a higher risk of probable depression (Table 3). Higher perceived susceptibility and severity [62, 75], COVID-like-symptoms [75, 76], frequent traditional and social media exposure [65, 66], masks shortage [30, 75], unclear mask reuse guidelines [75], disruptions to daily life [62], financial stressors and uncertainties [38, 62], marital conflict [77], experiences of physical and psychological abuse [78], home confinement [34, 79, 80], perceived inadequate housing conditions to cope with lockdowns [69], and loneliness [71] were associated with probable depression. Higher resilience [73], social support [66, 78], increased physical activity [69, 72], accurate and timely epidemic information [74], promotion of preventive measures by government [75], perceived effectiveness and adoption of physical distancing and personal preventive measures [34, 74] and sufficient basic supplies [74] were protective against probable depression.
Post-traumatic stress disorder
Prevalence
The prevalence of suspected PTSD for COVID-19 has not been examined in a random sample. Among non-probability samples, the prevalence ranged from 1.7% to 100% indicating the importance of using population-representative samples (Table S8). For Ebola virus disease and SARS, the pooled prevalence of suspected PTSD was 16.0% (95% CI 14.9–17.1), with low heterogeneity between studies (I2 = 0%; Fig. S1) [42,43,44].
Correlates
The threat of death during COVID-19 (e.g. having COVID-19-like symptoms [81], being unsure if oneself had contracted the virus or had close contact with infected people [82], knowing someone who were infected or died from COVID-19 [82]) and media exposure to COVID-19 news [83] were associated with suspected PTSD. Individuals with lower resilience and stressful life events had elevated risk of suspected PTSD [84, 85].
Psychological distress
Prevalence
The prevalence of psychological distress ranged from <1% to 37.8% in the general population during COVID-19 (Table 2) [29, 46,47,48,49,50,51,52,53, 55,56,57]. Our meta-analysis included the very low estimate in Norway (<1% vs ≥11.2% in other studies) [48], though it might be an outlier. The pooled prevalence was 13.0% (95% CI 0–34.1), with high heterogeneity (I2 = 100%; Fig. S1) yet minor asymmetry indicated by the DOI plot and LFK index of −1.62 (Fig. S2). Compared with pre-COVID-19 periods, psychological distress increased during COVID-19 in UK (from 18.9% to 27.3%) and US (3.9% to 13.6%) [51, 55]. However, separate studies have detected a stagnating or even declining trend in psychological distress in the US (from 14.2% to 13.0%) and UK (from 37.2% to 25.8%) from April to July 2020 [46, 52]. Studies on past epidemics indicated potential enduring mental health impact of novel epidemics. For example, the prevalence of psychological distress remained at around 6% and 45.6% respectively in Sierra Leone and Équateur of Congo towards and after the end of the Ebola virus disease epidemic [42, 45]. A study in Taiwan also reported 11.7% of adults having psychological distress four months after SARS [54].
Correlates
During COVID-19, females and those who were younger and had lower income showed a higher risk of psychological distress (Table 3). COVID-19-like symptoms [50, 86], worries of self-infection [82], increased risk of exposure to virus [45, 86], media exposure [87, 88], income loss [88, 89], other disruptions of daily life [90], family conflicts [91], and adoptions of preventive measures not recommended by WHO (e.g. taking antibiotics [92, 93]) were associated with psychological distress. Trust in the government and health system [81, 87], perceived effectiveness of preventive measures [87], and adoption of physical distancing [87] were associated with less psychological distress.
Other mental disorders
During COVID-19, the prevalence of alcohol use disorders increased from 25.1% before the lockdown to 38.3% during lockdown in England (Table 2) [58]. No prevalence data for acute stress disorder and obsessive-compulsive disorder were available from probability samples. Correlates for acute stress disorder during COVID-19 included younger age, lower income, pre-existing health conditions, self or family or friends being infected or quarantined, and increased exposure to virus (e.g., frontline workers; those living in high-risk areas) [94]. Higher resilience was associated with less obsessive-compulsive disorder [95].
Suicidality
None of the identified studies examined suicidal ideation in probability samples during or after an epidemic, although national registers showed that suicide rates in Norway and Queensland, Australia remained largely unchanged during COVID-19 [59, 60]. In non-probability samples, the prevalence of suicidal ideation during COVID-19 ranged from 2.8% to 14.2% (Table S8).
Correlates
Younger age [96], lower socioeconomic status [96], pre-existing mental health conditions [96], insomnia [97], serious marital conflicts [77], stress due to the pandemic [97], and COVID-19 health-related and economic worries [98] were associated with suicidal ideation during COVID-19.
Evidence appraisal
Study quality ranged from low to high (total NOS score 0–7 out of 9), with 2% classified as high quality (n = 6) and 70% (n = 179) as medium quality (Table S9). Yet, the quality of these studies might have been underestimated, as all studies had scored 0 for “ascertainment of exposure” and “selection of non-exposed sample” due to the lack of standardised, validated measures of exposure and non-exposed samples. Certainty of evidence based on the GRADE rating was low for anxiety, depression, psychological distress, and suicidality, and very low for PTSD and other mental outcomes. Major issues included lack of longitudinal data, high heterogeneity across studies, convenience sampling, paucity of diagnostic interviews, and potential publication bias. Nonetheless, the prevalence studies in general provided evidence for sample representativeness. These studies adopted probability-based sampling with weighting strategies to account for response bias, attribution bias, and differences with the underlying population (Table 2). The reported median response rate was 63.8% (Table 2), which is quite high given the context of an ongoing pandemic and overall declining trends in participation rates in epidemiologic studies [99].
Discussion
To date, this is the most comprehensive systematic review of novel epidemics and population mental health. Our meta-analysis showed that COVID-19 and other epidemics of a smaller scale were all associated with a substantial population mental health burden (Fig. S1). In randomly sampled populations, one in five adults had a probable mental disorder during COVID-19 (Fig. S1). This would be comparable to the levels observed in previous epidemics (i.e. Ebola virus disease), major disasters and armed conflicts [100,101,102], though mental health response to COVID-19 pandemic may vary greatly across settings. Where pre-pandemic prevalence was reported, our identified studies generally indicated an increase in anxiety, depression, psychological distress, and alcohol use disorders during COVID-19 (Table 2). This is consistent with the recent estimation that the global burden of anxiety and depression had increased during the COVID-19 pandemic [103]. We summarised correlates for poor mental health during COVID-19 (Table 3), which is crucial to identifying vulnerable groups when mental health responses are highly heterogeneous [104, 105]. Perceived risk of infection [62], exhibiting COVID-19-like symptoms [75, 76], masks shortage [30, 75], and unclear mask reuse guidelines [75] were associated with anxiety and depression. Providing accurate information and timely tests may therefore allay anxiety [74, 106]. Notably, lockdowns and home confinement during COVID-19 may also have exacerbated mental health conditions [34, 67, 68, 79, 80], particularly among those who had marital or family conflicts [77, 91], experiences of physical and psychological abuse [78], and inadequate housing conditions to cope with lockdowns [69]. While the scale of lockdowns and the infodemic during COVID-19 are unprecedented [107, 108], the psychological toll of lockdowns could be mitigated by social support, acting as a buffer for stressful environments [66, 109]. Social media appears to have become more influential on mental health than traditional media during recent major population events [66, 110, 111]. Indeed, heavy COVID-19-related social media use was associated with anxiety, depression and acute stress, possibly due to the spread of the “emotional contagion”, conflicting COVID-19 information, and fear-inducing misinformation via online social networks [64, 66, 112, 113]. These findings support the WHO’s recommendations on enhancing social support during the pandemic and reducing time spent on distressing COVID-19-related news [114].
Policy makers and service providers need to know who is the most vulnerable to guide priority setting and interventions [10, 18]. While all age groups have experienced poorer mental health during COVID-19 [55], the young can be disproportionately affected by countermeasures [55, 115]. Young adults, women, and those living with young children were found to be at higher risk for poor mental health during the lockdown in the UK [55]. In the US, young adults had the highest prevalence of anxiety or depressive disorders, COVID-19-related trauma- and stressor-related disorders, initiation of or increased substance use, and serious suicidal ideation in the previous month [115]. Decreased time for learning and living conditions during lockdown also had a clear impact on mental health of students [116]. Other vulnerable groups include survivors, health care workers, ethnic minorities, essential workers, unpaid caregivers for adults, those with low income and job loss, and people with pre-existing medical conditions including mental health disorders [37, 91, 96, 115, 117, 118]. In contrast, better mental health during COVID-19 was hypothesised for those with high levels of socioeconomic security due to the ability to work from home and having more time with family, but this has not been established [55]. Nevertheless, individuals and populations often exhibit remarkable resilience following major emergencies, with the majority not developing psychopathology [22, 119]. This lends support for targeted interventions following epidemics rather than mass interventions [120]. The stepped care model has been recommended during COVID-19 where the most effective, least resource-intensive treatments are provided to patients first, and more resource-heavy interventions then stepped up according to patients’ needs [121]. Digital psychological interventions have shown promise in LMICs [122], however, the epidemic and interventions could also widen entrenched patterns of inequities across settings [123]. Nurse-led approaches within a non-specialist setting could help deliver mental health and psychosocial support services to individuals when psychiatric hospitals are closed during epidemics [124]. Upstream approaches targeting the population determinants of health could address inequities by preserving the economy, reducing job loss, and implementing social policies to prevent substance use and domestic violence [125,126,127].
The COVID-19 pandemic represents a three-way tug-of-war between COVID-19 suppression, economic preservation, and population well-being [128]. An uncontrolled epidemic, prolonged stringent interventions such as lockdowns, and economic recession could all profoundly affect population mental health. In contrast, addressing the emerging and prevailing determinants of mental health would mitigate the psychological toll of the pandemic. This in turn could reduce pandemic fatigue, promote social acceptance and adherence to interventions [128,129,130]. Protecting population mental health has therefore become even more important during COVID-19 [131]. Yet the psychobehavioural responses to epidemics depend on a interplay between threat perception, stress and coping, individual and collective interests, social context, leadership, and risk communication [130, 132]. Maintaining public trust in authorities and incorporating altruism in health messaging could improve mental well-being and adherence to interventions [11, 18, 130, 133, 134]. Indeed, adoption of physical distancing and personal preventive measures in general have been associated with lower risk of anxiety, depression and psychological distress.
Nevertheless, our review did not include studies on mental health symptoms and transdiagnostic outcomes, thereby limiting the assessment of mental health impact of COVID-19 and other epidemics. In particular, insomnia is a very prevalent mental health condition during epidemics, with an estimation of one in three adults reporting insomnia during COVID-19 [4]. Furthermore, we have identified several major limitations of the extant literature. First, as with other reviews on COVID-19 and previous epidemics [3,4,5,6,7,8,9, 12, 13, 102], there was considerable heterogeneity across studies, possibly due to differences in study design and the magnitude of epidemics, countermeasures, and consequences (e.g. social and economic costs) [10, 135]. However, this limitation is inherent to psychiatric epidemiological research following major emergencies [101], and was partly addressed by including more comparable random samples for our meta-analysis. Second, more random samples are needed to provide reliable estimates of the mental health burden of epidemics and to allow a meta-regression to explore reasons for the observed heterogeneity [10]. For instance, the pooled prevalence of psychological distress was lower than specific mental disorders due to the inclusion of a study in Norway which reported a very low prevalence estimate (<1%) [48]. Prior meta-analyses that have relied on convenience samples or opt-in online panels would have included more studies but may have overestimated the population mental health burden associated with COVID-19 [3,4,5,6, 8, 9]. The high proportion of probability samples during past epidemics (87.5%) compared to COVID-19 (~10%) suggests that probability samples are possible during epidemics (e.g. via random-digit-dialling, address-based sampling) and should be used to generate high-quality evidence during COVID-19 [10]. Third, longitudinal, population-representative cohorts with baseline data are needed. In this review, we were only able to identify one such cohort (i.e. UK Household Longitudinal Study) [47, 53, 55]. All other studies with pre-pandemic baseline data were cross-sectional and compared different samples. Due to the inherent differences among individuals, it is difficult to discern the changes in prevalence attributable to the COVID-19 pandemic. Baseline data is particularly important when unexpected values of prevalence estimates (e.g. <1% of psychological distress in Norway [48]) were found. Also, psychological distress remained high after the Ebola virus disease epidemic [42, 45], indicating that ongoing surveillance of population mental health and long-term studies are needed for COVID-19 even when we have exited the pandemic. Future research should prioritise longitudinal, population-representative samples with pre-epidemic data and long-term outcomes [10, 18]. This may be difficult but have been successfully implemented by nesting follow-ups in existing random samples where available (e.g. UK Household Longitudinal Study, Hong Kong FAMILY Cohort) [66, 110]. Such cohorts could be instrumental to informing the appropriate response and mobilisation of resources and mental health services [10, 55, 110, 136]. Fourth, all random samples during COVID-19 were conducted in high-income settings. Language restrictions of our search may have excluded studies published in other languages. Resources and studies in low and middle-income countries where COVID-19 has a large impact are needed, and the health system and economy of individual countries could be particularly vulnerable to the consequences of the pandemic [137]. Fifth, most studies relied on screening instruments, and the findings could represent acute reactions to a stressful event as opposed to true psychopathology [138]. However, the screening instruments have been shown to be valid and reliable (Table S3) and we excluded studies using non-validated mental health measures (e.g. self-conceived questions, single-item measures) [10]. Lastly, to date, the prevalence of PTSD or obsessive-compulsive disorder during COVID-19 has not been examined using a random sample. It is well-known that PTSD is highly prevalent following population shocks [139]. By including findings from SARS and Ebola virus disease in our review, we estimated that the prevalence of suspected PTSD may approximate 16% during epidemics. Yet, the applicability of these findings to COVID-19 is unclear.
Conclusion
Our study shows that the psychological toll of COVID-19 and past epidemics was substantial and widespread in the community. Novel infectious diseases can therefore spill over from infected individuals to the community-at-large, where even those not directly exposed to the pathogen experience psychiatric sequelae. Health-care professionals need to be vigilant in recognising mental health sequelae in the general population. However, the resources available for prevention and treatment of mental disorders in most countries have diminished given competing demands [131]. This needs to be urgently redressed as mental health is uniquely placed to improve the whole spectrum of well-being, and thus should be at the forefront of the health agenda [129, 140]. With further waves of COVID-19 anticipated and the inevitability of new epidemics [141, 142], ongoing surveillance of the mental health impact of epidemics and public mental health interventions to build community resilience should be integrated into preparedness plans worldwide [143].
References
Brooks SK, Smith LE, Webster RK, Weston D, Woodland L, Hall I, et al. The impact of unplanned school closure on children’s social contact: rapid evidence review. Eur Surveill. 2020;25:2000188.
Chu IY, Alam P, Larson HJ, Lin L. Social consequences of mass quarantine during epidemics: a systematic review with implications for the COVID-19 response. J Travel Med. 2020;27:taaa192.
Cooke JE, Eirich R, Racine N, Madigan S. Prevalence of posttraumatic and general psychological stress during COVID-19: a rapid review and meta-analysis. Psychiatry Res. 2020;292:113347.
Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - a systematic review and meta-analysis. Psychiatry Res. 2020;291:113190.
Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. 2020;16:57.
Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2021;281:91–8.
Cénat JM, Blais-Rochette C, Kokou-Kpolou CK, Noorishad P-G, Mukunzi JN, McIntee S-E, et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295:113599.
Fan FC, Zhang SY, Cheng Y. Incidence of psychological illness after coronavirus outbreak: a meta-analysis study. J Epidemiol Community Health 2021;75:836–42.
Yuan K, Gong YM, Liu L, Sun YK, Tian SS, Wang YJ, et al. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review. Mol Psychiatry 2021;26:4982–98.
Pierce M, McManus S, Jessop C, John A, Hotopf M, Ford T, et al. Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry 2020;7:567–8.
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020;395:912–20.
Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020;7:611–27.
Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642.
Leung C, Ho M, Bharwani A, Ni MY. Mental health consequences of viral epidemics in the community: a systematic review. 2020. https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=179105. Accessed 1 Sept 2020.
Else H. How a torrent of COVID science changed research publishing—in seven charts. Nature 2020;588:553.
North CS, Pfefferbaum B. Mental health response to community disasters: a systematic review. JAMA 2013;310:507–18.
Kendell R, Jablensky A. Distinguishing between the validity and utility of psychiatric diagnoses. Am J Psychiatry 2003;160:4–12.
Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020;7:547–60.
Higgins JPT, Green S. Tools for assessing methodological quality or risk of bias in non-randomized studies. 2012. http://handbook.cochrane.org/chapter_13/13_5_2_3_tools_for_assessing_methodological_quality_or_risk_of.htm. Accessed 1 Sept 2020.
Patra J, Bhatia M, Suraweera W, Morris SK, Patra C, Gupta PC, et al. Exposure to second-hand smoke and the risk of tuberculosis in children and adults: a systematic review and meta-analysis of 18 observational studies. PLoS Med. 2015;12:e1001835.
Anglin RES, Samaan Z, Walter SD, McDonald SD. Vitamin D deficiency and depression in adults: systematic review and meta-analysis. Br J Psychiatry 2013;202:100–7.
Ni MY, Kim Y, McDowell I, Wong S, Qiu H, Wong IOL, et al. Mental health during and after protests, riots and revolutions: a systematic review. Aust N Z J Psychiatry 2020;54:232–43.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–6.
Rothman KJ, Gallacher JE, Hatch EE. Why representativeness should be avoided. Int J Epidemiol. 2013;42:1012–4.
Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health 2013;67:974–8.
Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Smith GD and Altman DG (ed). Systematic Reviews in Health Care: Meta‐Analysis in Context. BMJ Publishing Group: London, 2001, pp 285–312.
Furuya-Kanamori L, Barendregt JJ, Doi SAR. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int J Evid Based Healthc. 2018;16:195–203.
Doi SA, Barendregt JJ, Khan S, Thalib L, Williams GM. Advances in the meta-analysis of heterogeneous clinical trials II: the quality effects model. Contemp Clin Trials. 2015;45:123–9.
Bruine de Bruin W. Age differences in COVID-19 risk perceptions and mental health: evidence from a national U.S. survey conducted in March 2020. J Gerontol B Psychol Sci Soc Sci. 2021;76:e24–9.
Choi EPH, Hui BPH, Wan EYF. Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health 2020;17:3740.
Holingue C, Kalb LG, Riehm KE, Bennett D, Kapteyn A, Veldhuis CB, et al. Mental distress in the United States at the beginning of the COVID-19 pandemic. Am J Public Health 2020;110:1628–34.
Qian M, Wu Q, Wu P, Hou Z, Liang Y, Cowling BJ, et al. Anxiety levels, precautionary behaviours and public perceptions during the early phase of the COVID-19 outbreak in China: a population-based cross-sectional survey. BMJ Open 2020;10:e040910.
Twenge JM, Joiner TE. U.S. Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress Anxiety 2020;37:954–6.
Zhao SZ, Wong JYH, Wu YD, Choi EPH, Wang MP, Lam TH. Social distancing compliance under COVID-19 pandemic and mental health impacts: a population-based study. Int J Environ Res Public Health 2020;17:6692.
Zhao SZ, Wong JYH, Luk TT, Wai AKC, Lam TH, Wang MP. Mental health crisis under COVID-19 pandemic in Hong Kong, China. Int J Infect Dis. 2020;100:431–3.
Daly M, Sutin AR, Robinson E. Depression reported by US adults in 2017-2018 and March and April 2020. J Affect Disord. 2021;278:131–5.
Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open 2020;3:e2019686.
Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Low assets and financial stressors associated with higher depression during COVID-19 in a nationally representative sample of US adults. J Epidemiol Community Health 2021;75:501–8.
Garre-Olmo J, Turro-Garriga O, Marti-Lluch R, Zacarias-Pons L, Alves-Cabratosa L, Serrano-Sarbosa D, et al. Changes in lifestyle resulting from confinement due to COVID-19 and depressive symptomatology: a cross-sectional a population-based study. Compr Psychiatry 2021;104:152214.
Ko C-H, Yen C-F, Yen J-Y, Yang M-J. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin Neurosci. 2006;60:397–403.
Li TW, Lee TMC, Goodwin R, Ben-Ezra M, Liang L, Liu H, et al. Social capital, income loss, and psychobehavioral responses amid COVID-19: a population-based analysis. Int J Environ Res Public Health 2020;17:8888.
Jalloh MF, Li WS, Bunnell RE, Ethier KA, O’Leary A, Hageman KM, et al. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob Health 2018;3:e000471.
Lau JTF, Yang X, Pang E, Tsui HY, Wong E, Wing YK. SARS-related perceptions in Hong Kong. Emerg Infect Dis. 2005;11:417–24.
Lau JT, Yang X, Tsui HY, Pang E, Wing YK. Positive mental health-related impacts of the SARS epidemic on the general public in Hong Kong and their associations with other negative impacts. J Infect. 2006;53:114–24.
Cenat JM, McIntee SE, Guerrier M, Derivois D, Rousseau C, Dalexis RD, et al. Psychological distress among adults from the urban and rural areas affected by the Ebola virus disease in the Democratic Republic of the Congo. Soc Psychiatry Psychiatr Epidemiol. 2021;56:57–62.
Chandola T, Kumari M, Booker CL, Benzeval M. The mental health impact of COVID-19 and lockdown-related stressors among adults in the UK. Psychol Med. 2020. https://doi.org/10.1017/S0033291720005048.
Daly M, Sutin A, Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychol Med. 2020. https://doi.org/10.1017/S0033291720004432.
Harris SM, Sandal GM. COVID-19 and psychological distress in Norway: the role of trust in the healthcare system. Scand J Public Health 2021;49:96–103.
Kämpfen F, Kohler IV, Ciancio A, Bruine de Bruin W, Maurer J, Kohler HP. Predictors of mental health during the Covid-19 pandemic in the US: role of economic concerns, health worries and social distancing. PLoS ONE 2020;15:e0241895.
Li LZ, Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 2020;291:113267.
McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA 2020;324:93–4.
McGinty EE, Presskreischer R, Anderson KE, Han H, Barry CL. Psychological distress and COVID-19-related stressors reported in a longitudinal cohort of US adults in April and July 2020. JAMA 2020;324:2555–7.
Niedzwiedz CL, Green MJ, Benzeval M, Campbell D, Craig P, Demou E, et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK Household Longitudinal Study. J Epidemiol Community Health 2021;75:224–31.
Peng EY, Lee MB, Tsai ST, Yang CC, Morisky DE, Tsai LT, et al. Population-based post-crisis psychological distress: an example from the SARS outbreak in Taiwan. J Formos Med Assoc. 2010;109:524–32.
Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020;7:883–92.
Riehm KE, Holingue C, Kalb LG, Bennett D, Kapteyn A, Jiang Q, et al. Associations between media exposure and mental distress among us adults at the beginning of the COVID-19 pandemic. Am J Prev Med. 2020;59:630–8.
Robinson E, Daly M. Explaining the rise and fall of psychological distress during the COVID‐19 crisis in the United States: longitudinal evidence from the Understanding America Study. Br J Health Psychol. 2021;26:570–87.
Jackson SE, Garnett C, Shahab L, Oldham M, Brown J. Association of the COVID-19 lockdown with smoking, drinking and attempts to quit in England: an analysis of 2019-20 data. Addiction 2021;116:1233–44.
Leske S, Kolves K, Crompton D, Arensman E, de Leo D. Real-time suicide mortality data from police reports in Queensland, Australia, during the COVID-19 pandemic: an interrupted time-series analysis. Lancet Psychiatry 2021;8:58–63.
Qin P, Mehlum L. National observation of death by suicide in the first 3 months under COVID-19 pandemic. Acta Psychiatr Scand. 2021;143:92–3.
Wasserman IM. The impact of epidemic, war, prohibition and media on suicide: United States, 1910–1920. Suicide Life Threat Behav. 1992;22:240–54.
Li J, Yang Z, Qiu H, Wang Y, Jian L, Ji J, et al. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry 2020;19:249–50.
Elton-Marshall T, Wells S, Jankowicz D, Nigatu YT, Wickens CM, Rehm J, et al. Multiple COVID-19 risk factors increase the likelihood of experiencing anxiety symptoms in Canada. Can J Psychiatry 2020;66:56–8.
Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 2020;15:e0231924.
Peretti-Watel P, Alleaume C, Leger D, Beck F, Verger P, Grp C. Anxiety, depression and sleep problems: a second wave of COVID-19. Gen Psychiatr. 2020;33:e100299.
Ni MY, Yang L, Leung CMC, Li N, Yao XI, Wang Y, et al. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: cross-sectional survey. JMIR Ment Health 2020;7:e19009.
Benke C, Autenrieth LK, Asselmann E, Pane-Farre CA. Stay-at-home orders due to the COVID-19 pandemic are associated with elevated depression and anxiety in younger, but not older adults: results from a nationwide community sample of adults from Germany. Psychol Med. 2020. https://doi.org/10.1017/S0033291720003438.
Pouso S, Borja A, Fleming LE, Gomez-Baggethun E, White MP, Uyarra MC. Contact with blue-green spaces during the COVID-19 pandemic lockdown beneficial for mental health. Sci Total Environ. 2021;756:143984.
Jacques-Avino C, Lopez-Jimenez T, Medina-Perucha L, de Bont J, Goncalves AQ, Duarte-Salles T, et al. Gender-based approach on the social impact and mental health in Spain during COVID-19 lockdown: a cross-sectional study. BMJ Open 2020;10:e044617.
Jia R, Ayling K, Chalder T, Massey A, Broadbent E, Coupland C, et al. Mental health in the UK during the COVID-19 pandemic: cross-sectional analyses from a community cohort study. BMJ Open 2020;10:e040620.
Palgi Y, Shrira A, Ring L, Bodner E, Avidor S, Bergman Y, et al. The loneliness pandemic: loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J Affect Disord. 2020;275:109–11.
Makhashvili N, Javakhishvili JD, Sturua L, Pilauri K, Fuhr DC, Roberts B. The influence of concern about COVID-19 on mental health in the Republic of Georgia: a cross-sectional study. Glob Health 2020;16:111.
Barzilay R, Moore TM, Greenberg DM, DiDomenico GE, Brown LA, White LK, et al. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl Psychiatry 2020;10:291.
Huang J, Liu F, Teng Z, Chen J, Zhao J, Wang X, et al. Public behavior change, perceptions, depression, and anxiety in relation to the COVID-19 outbreak. Open Forum Infect Dis. 2020;7:ofaa273.
Bressington DT, Cheung TCC, Lam SC, Suen LKP, Fong TKH, Ho HSW, et al. Association between depression, health beliefs, and face mask use during the COVID-19 pandemic. Front Psychiatry 2020;11:571179.
Skapinakis P, Bellos S, Oikonomou A, Dimitriadis G, Gkikas P, Perdikari E, et al. Depression and its relationship with coping strategies and illness perceptions during the COVID-19 lockdown in Greece: a cross-sectional survey of the population. Depress Res Treat. 2020;2020:3158954.
Bryan CJ, Bryan AO, Baker JC. Associations among state-level physical distancing measures and suicidal thoughts and behaviors among U.S. adults during the early COVID-19 pandemic. Suicide Life Threat Behav. 2020;26:e12653.
Iob E, Frank P, Steptoe A, Fancourt D. Levels of severity of depressive symptoms among at-risk groups in the UK during the COVID-19 pandemic. JAMA Netw Open 2020;3:e2026064.
Wang S, Zhang Y, Ding W, Meng Y, Hu H, Liu Z, et al. Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: a nationwide multicenter crosssectional study. Eur Psychiatry 2020;63:e77.
Zhang Y, Wang S, Ding W, Meng Y, Hu HT, Liu ZH, et al. Status and influential factors of anxiety depression and insomnia symptoms in the work resumption period of COVID-19 epidemic: a multicenter cross-sectional study. J Psychosom Res. 2020;138:110253.
Mohammadi MR, Zarafshan H, Bashi SK, Mohammadi F, Khaleghi A. The role of public trust and media in the psychological and behavioral responses to the COVID-19 pandemic. Iran J Psychiatry 2020;15:189–204.
Forte G, Favieri F, Tambelli R, Casagrande M. The enemy which sealed the world: effects of COVID-19 diffusion on the psychological state of the Italian population. J Clin Med. 2020;9:1802.
Fekih-Romdhane F, Ghrissi F, Abbassi B, Cherif W, Cheour M. Prevalence and predictors of PTSD during the COVID-19 pandemic: findings from a Tunisian community sample. Psychiatry Res. 2020;290:113131.
Kolacz J, Dale LP, Nix EJ, Roath OK, Lewis GF, Porges SW. Adversity history predicts self-reported autonomic reactivity and mental health in US residents during the COVID-19 pandemic. Front Psychiatry 2020;11:577728.
Alshehri FS, Alatawi Y, Alghamdi BS, Alhifany AA, Alharbi A. Prevalence of post-traumatic stress disorder during the COVID-19 pandemic in Saudi Arabia. Saudi. Pharm J. 2020;28:1666–73.
Gómez-Salgado J, Andrés-Villas M, Domínguez-Salas S, Díaz-Milanés D, Ruiz-Frutos C. Related health factors of psychological distress during the COVID-19 pandemic in Spain. Int J Environ Res Public Health 2020;17:3947.
Dominguez-Salas S, Gomez-Salgado J, Andres-Villas M, Diaz-Milanes D, Romero-Martin M, Ruiz-Frutos C. Psycho-emotional approach to the psychological distress related to the COVID-19 pandemic in Spain: a cross-sectional observational study. Healthcare 2020;8:190.
Duarte MQ, Santo M, Lima CP, Giordani JP, Trentini CM. Covid-19 and the impacts on mental health: a sample from Rio Grande do Sul, Brazil. Cien Saude Colet. 2020;25:3401–11.
Shevlin M, McBride O, Murphy J, Miller JG, Hartman TK, Levita L, et al. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open 2020;6:e125.
Zhu S, Wu Y, Zhu CY, Hong WC, Yu ZX, Chen ZK, et al. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain Behav Immun. 2020;87:56–8.
Guo Y, Cheng C, Zeng Y, Li YR, Zhu MT, Yang WX, et al. Mental health disorders and associated risk factors in quarantined adults during the COVID-19 outbreak in China: cross-sectional study. J Med Internet Res. 2020;22:e20328.
Ben-Ezra M, Cary N, Goodwin R. The association between COVID-19 WHO non-recommended behaviors with psychological distress in the UK population: a preliminary study. J Psychiatr Res. 2020;130:286–8.
Ben-Ezra M, Sun S, Hou WK, Goodwin R. The association of being in quarantine and related COVID-19 recommended and non-recommended behaviors with psychological distress in Chinese population. J Affect Disord. 2020;275:66–8.
Shi L, Lu Z-A, Que J-Y, Huang X-L, Liu L, Ran M-S, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open 2020;3:e2014053.
Munk AJL, Schmidt NM, Alexander N, Henkel K, Hennig J. COVID-19-beyond virology: potentials for maintaining mental health during lockdown. PLoS ONE 2020;15:e0236688.
O’Connor RC, Wetherall K, Cleare S, McClelland H, Melson AJ, Niedzwiedz CL, et al. Mental health and wellbeing during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry 2021;218:326–33.
Caballero-Dominguez CC, Jimenez-Villamizar MP, Campo-Arias A. Suicide risk during the lockdown due to coronavirus disease (COVID-19) in Colombia. Death Stud. 2022;46:885–90.
Winkler P, Formanek T, Mlada K, Kagstrom A, Mohrova Z, Mohr P, et al. Increase in prevalence of current mental disorders in the context of COVID-19: analysis of repeated nationwide cross-sectional surveys. Epidemiol Psychiatr Sci. 2020;29:e173.
Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol. 2007;17:643–53.
Goldmann E, Galea S. Mental health consequences of disasters. Annu Rev Public Health 2014;35:169–83.
Charlson F, van Ommeren M, Flaxman A, Cornett J, Whiteford H, Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet 2019;394:240–8.
Cénat JM, Felix N, Blais-Rochette C, Rousseau C, Bukaka J, Derivois D, et al. Prevalence of mental health problems in populations affected by the Ebola virus disease: a systematic review and meta-analysis. Psychiatry Res. 2020;289:113033.
Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021;398:1700–12.
Pierce M, McManus S, Hope H, Hotopf M, Ford T, Hatch SL, et al. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry 2021;8:610–9.
Shevlin M, Butter S, McBride O, Murphy J, Gibson-Miller J, Hartman TK, et al. Refuting the myth of a ‘tsunami’ of mental ill-health in populations affected by COVID-19: evidence that response to the pandemic is heterogeneous, not homogeneous. Psychol Med. 2021. https://doi.org/10.1017/s0033291721001665.
Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA 2020;323:2133–4.
The Lancet. The truth is out there, somewhere. Lancet 2020;396:291.
FT Visual & Data Journalism Team, Financial Times. Exiting lockdowns: tracking governments’ changing coronavirus responses. 2020. https://ig.ft.com/coronavirus-lockdowns/. Accessed 1 Sept 2020.
Ni MY, Li TK, Pang H, Chan BHY, Kawachi I, Viswanath K, et al. Longitudinal patterns and predictors of depression trajectories related to the 2014 Occupy Central/Umbrella Movement in Hong Kong. Am J Public Health 2017;107:593–600.
Ni MY, Yao XI, Leung KSM, Yau C, Leung CMC, Lun P, et al. Depression and post-traumatic stress during major social unrest in Hong Kong: a 10-year prospective cohort study. Lancet 2020;395:273–84.
Ni MY, Li TK, Pang H, Chan BHY, Yuan BY, Kawachi I, et al. Direct participation in and indirect exposure to the Occupy Central Movement and depressive symptoms: a longitudinal study of Hong Kong adults. Am J Epidemiol. 2016;184:636–43.
Kramer ADI, Guillory JE, Hancock JT. Experimental evidence of massive-scale emotional contagion through social networks. Proc Natl Acad Sci USA 2014;111:8788–90.
Holman EA, Thompson RR, Garfin DR, Silver RC. The unfolding COVID-19 pandemic: a probability-based, nationally representative study of mental health in the United States. Sci Adv. 2020;6:eabd5390.
World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak. 2020. https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf?sfvrsn=6d3578af_2. Accessed 30 Aug 2020.
Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1049–57.
Baumann C, Rousseau H, Tarquinio C, Batt M, Tarquinio P, Lebreuilly R, et al. Effect of the COVID-19 outbreak and lockdown on mental health among post-secondary students in the Grand Est region of France: results of the PIMS-CoV19 study. Health Qual Life Outcomes 2021;19:265.
Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry 2020;7:813–24.
Zürcher SJ, Kerksieck P, Adamus C, Burr CM, Lehmann AI, Huber FK, et al. Prevalence of mental health problems during virus epidemics in the general public, health care workers and survivors: a rapid review of the evidence. Front Public Health 2020;8:560389.
Norris FH, Tracy M, Galea S. Looking for resilience: understanding the longitudinal trajectories of responses to stress. Soc Sci Med. 2009;68:2190–8.
Van Emmerik AAP, Kamphuis JH, Hulsbosch AM, Emmelkamp PMG. Single session debriefing after psychological trauma: a meta-analysis. Lancet 2002;360:766–71.
Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180:817–8.
Fu Z, Burger H, Arjadi R, Bockting CLH. Effectiveness of digital psychological interventions for mental health problems in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Psychiatry 2020;7:851–64.
Galea S. Compassion in a time of COVID-19. Lancet 2020;395:1897–8.
Kamara S, Walder A, Duncan J, Kabbedijk A, Hughes P, Muana A. Mental health care during the Ebola virus disease outbreak in Sierra Leone. Bull World Health Organ. 2017;95:842–7.
The Lancet Planetary Health. Post-COVID-19 spending. Lancet Planet Health 2020;4:e168.
Du J, Fan N, Zhao M, Hao W, Liu T, Lu L, et al. Expert consensus on the prevention and treatment of substance use and addictive behaviour-related disorders during the COVID-19 pandemic. Gen Psychiatr. 2020;33:e100252.
Chandan JS, Taylor J, Bradbury-Jones C, Nirantharakumar K, Kane E, Bandyopadhyay S. COVID-19: a public health approach to manage domestic violence is needed. Lancet Public Health 2020;5:e309.
Leung GM, Cowling BJ, Wu JT. From a sprint to a marathon in Hong Kong. N. Engl J Med. 2020;382:e45.
Ni MY, Yao XI, Cheung F, Wu JT, Schooling CM, Pang H, et al. Determinants of physical, mental and social well-being: a longitudinal environment-wide association study. Int J Epidemiol. 2020;49:380–9.
Wu JT, Leung K, Lam TTY, Ni MY, Wong CKH, Peiris JSM, et al. Nowcasting epidemics of novel pathogens: lessons from COVID-19. Nat Med. 2021;27:388–95.
Phillips MR. Perspectives: World Mental Health Day 2020: promoting global mental health during COVID-19. China CDC Wkly 2020;2:844–7.
Van Bavel JJ, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav. 2020;4:460–71.
Lau LS, Samari G, Moresky RT, Casey SE, Kachur SP, Roberts LF, et al. COVID-19 in humanitarian settings and lessons learned from past epidemics. Nat Med 2020;26:647–8.
Cheung CK, Tse JW. Institutional trust as a determinant of anxiety during the SARS crisis in Hong Kong. Soc Work. Public Health 2008;23:41–54.
Singer M, Bulled N, Ostrach B, Mendenhall E. Syndemics and the biosocial conception of health. Lancet 2017;389:941–50.
Ni MY, Leung CMC, Leung GM. The epidemiology of population mental wellbeing in China. Lancet Public Health 2020;5:e631–2.
Kola L. Global mental health and COVID-19. Lancet Psychiatry 2020;7:655–7.
North CS. Current research and recent breakthroughs on the mental health effects of disasters. Curr Psychiatry Rep. 2014;16:481.
Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008;38:467–80.
Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The Lancet Commission on global mental health and sustainable development. Lancet 2018;392:1553–98.
Fauci AS, Morens DM. The perpetual challenge of infectious diseases. N. Engl J Med. 2012;366:454–61.
Scudellari M. How the pandemic might play out in 2021 and beyond. Nature 2020;584:22–5.
Adhanom Ghebreyesus T. Addressing mental health needs: an integral part of COVID-19 response. World Psychiatry 2020;19:129–30.
Acknowledgements
This work was financially supported by the Government of the Hong Kong Special Administrative Region. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. We thank Mr. Hoi-wa Wong, Miss Natalie Choi, and Miss Hebe Lai for their technical support, and Prof Wändi Bruine de Bruin and National Science Foundation (#2028683) for the COVID-19 data on mental health in the US.
Author information
Authors and Affiliations
Contributions
MYN and CML conceived and designed the study. CML devised the search strategy with input from MKH, AAB and MYN. CML, MKH, AAB, YW, MSC and XF conducted the search, data extraction, and appraisal. CML, HCM and MYN analysed the data. All authors interpreted the data. MYN and CML wrote the manuscript with input from MKH and AAB. All authors were involved in editing and approving the manuscript. The corresponding author attests that all listed authors meet authorship criteria.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Leung, C.M.C., Ho, M.K., Bharwani, A.A. et al. Mental disorders following COVID-19 and other epidemics: a systematic review and meta-analysis. Transl Psychiatry 12, 205 (2022). https://doi.org/10.1038/s41398-022-01946-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-022-01946-6