Abstract
Conventional medicines optimisation interventions in people with multimorbidity and polypharmacy are complex and yet limited; a more holistic and integrated approach to healthcare delivery is required. Pharmacogenetics has potential as a component of medicines optimisation. Studies involving multi-medicine pharmacogenetics in adults with multimorbidity or polypharmacy, reporting on outcomes derived from relevant core outcome sets, were included in this systematic review. Narrative synthesis was undertaken to summarise the data; meta-analysis was inappropriate due to study heterogeneity. Fifteen studies of diverse design and variable quality were included. A small, randomised study involving pharmacist-led medicines optimisation, including pharmacogenetics, suggests this approach could have significant benefits for patients and health systems. However, due to study design heterogeneity and the quality of the included studies, it is difficult to draw generalisable conclusions. Further pragmatic, robust pharmacogenetics studies in diverse, real-world patient populations, are required to establish the benefit of multi-medicine pharmacogenetic screening on patient outcomes.
Similar content being viewed by others
Introduction
The population is rapidly ageing. By 2050, the number of elderly people (≥65 years) worldwide is expected to increase two-fold [1]. There is a well-recognised association between ageing and the presence of multimorbidity (two or more chronic conditions) and polypharmacy (the prescribing of four or more medications, although various definitions are used) [2,3,4,5]. In older persons, the prevalence of multimorbidity is estimated to range from 55% to 98% [6]. Furthermore, the occurrence of associated polypharmacy is increasing. A population database analysis in Scotland found that between 1995 and 2010, the proportion of adults dispensed five or more medicines doubled to 20.8% and the proportion of elderly patients prescribed ≥10 medicines more than tripled to 17.2% [7]. However, the issue of multimorbidity and polypharmacy is not restricted to age, with a substantial number of young and middle-aged people also affected [4, 7]. Several negative health outcomes are associated with multimorbidity and polypharmacy, including increased healthcare utilisation, mortality rates, healthcare costs, and poorer health-related quality of life [6, 8,9,10,11]. Nevertheless, the organisation and delivery of healthcare, as well as the development of clinical guidelines, are primarily built around singular diseases [4, 12].
A more holistic and integrated approach to healthcare delivery and medicines optimisation is needed to carefully identify the correct balance between appropriate and inappropriate polypharmacy for each multimorbid patient. The World Health Organisation (WHO) has emphasised the importance of refining healthcare systems to enable safer primary care for those with multimorbidity through personalisation of treatments and by combining best available evidence with clinical knowledge and judgement [13]. The National Institute for Health and Care Excellence (NICE) guidelines for multimorbidity management and the Scottish Government’s guidance on polypharmacy also advocate for a personalised approach to care [14, 15]. Such individualised approaches aim to improve treatment outcomes and appropriate polypharmacy by reducing inappropriate treatment burden and uncoordinated care, thereby avoiding medication-related problems, such as adverse drug events and drug interactions.
Drug interactions are associated with both appropriate treatment of chronic diseases and a majority of preventable drug-related hospitalisations (up to 87% in some studies) [7, 16]. For the purposes of this review, drug interactions are defined as drug-drug, drug-gene and drug-drug-gene interactions (those caused by a combination of drug-drug and drug-gene interactions) [17]. Drug-drug-gene interactions may involve inhibitory, induction or phenoconversion interactions, whereby the genetic variant and the perpetrator drug combine to act on transporter or metabolism pathways to significantly alter drug concentrations [17]. Pharmacogenetic analysis enables assessment of these gene-based variations in drug responses, which is significant as genetic polymorphisms are estimated to cause 15–30% of individual drug response variability [18], and >95% of all individuals carry at least one actionable genotype when tested for a panel of up to 12 genes [19,20,21]. Therefore, pharmacogenetic testing offers clinicians the opportunity to act prospectively rather than retrospectively, enabling the provision of the right medication at the right dose at the right time to individual patients [22]. Although the literature suggests that drug-gene and drug-drug-gene interactions are prevalent and clinically relevant [23,24,25], pharmacogenetics is not considered in the WHO, NICE and Scottish guidelines, and is rarely applied as part of medicines optimisation despite its enormous potential [13,14,15, 26]. Furthermore, two Cochrane reviews investigating interventions to improve outcomes for patients with multimorbidity and polypharmacy were found to have uncertain effectiveness [2, 3]; however, interventions incorporating pharmacogenetics were not identified.
Countless pharmacogenetic studies have been performed in recent years, yielding a substantial body of knowledge on gene-based variations affecting drug susceptibility. Evidence for the efficacy of pharmacogenetics to guide prescribing has been predominantly guided by studies and systematic reviews focused on single drug-gene or disease-gene pairs. For example, the various studies on pharmacogenetic-guided abacavir [27], anticoagulant [28,29,30,31], antidepressant [32,33,34], antipsychotic [35], clopidogrel [36], statin [37] and thiopurine therapy [38]. As a result, pharmacogenetics is gaining momentum in healthcare delivery in some countries, with various completed and ongoing implementation studies in the US, Canada, Europe, and Asia [39,40,41,42]. Worldwide, pharmacogenetic testing largely remains within the remit of specialist secondary and tertiary care settings [42, 43]. Outside of these environments, pharmacogenetics is emerging in primary care, where importantly, most prescribing and dispensing of medicines occurs [44]. Community pharmacy pharmacogenetic testing models have been investigated and demonstrate promise [45,46,47]. Furthermore, in the UK, the NHS England plan to incorporate pharmacogenetics in primary care by 2025 through adoption of a pre-emptive panel-based strategy for drug-gene pairs with the most evidence of (cost-)effectiveness [48].
Such clinical evidence is available in guidelines published by the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the Dutch Pharmacogenetics Working Group (DPWG), providing actionable, genotype-based prescribing recommendations [49]. CPIC and DPWG have independently reviewed over 100 drug-gene interactions and have actionable recommendations for 60 and 55 individual drug-gene interactions respectively [50]. Despite established guidelines, the application of pharmacogenetics in routine patient care has been slow. Several barriers are frequently cited, including pharmacogenetics education, conflicting conclusions on clinical utility and cost-effectiveness, regulatory and reimbursement concerns, the need for informatics to support pharmacogenetics-informed prescribing decisions, and concerns over data sharing as well as other ethical, legal, and social implications surrounding pharmacogenetics [42, 43, 51,52,53,54,55]. It is envisaged that overcoming these barriers will provide the impetus for the widespread adoption of pharmacogenetic guidelines, enabling the realisation of the potential of pharmacogenetics [41].
Consequently, pharmacogenetics may have a role in improving the current approaches to medication usage, with potential for improving appropriate polypharmacy and preventing medication-related problems. However, the effectiveness of multi-gene, multi-drug, multi-disease pharmacogenetic interventions in adults with multimorbidity or prescribed polypharmacy is yet to be established. This systematic review aimed to establish the efficacy of such interventions in all healthcare settings, and to inform the implementation of pharmacogenetic-guided therapy into clinical practice.
Results
Search results
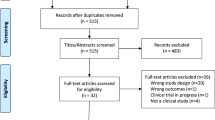
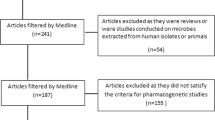
Through the database searches, 12,433 records were retrieved, and 10,725 records were screened after de-duplication. Of these, 10,623 studies did not meet the inclusion criteria, and were excluded. Following assessment of the remaining 102 records in full text, 87 were excluded. Reasons for exclusion can be found in the PRISMA Flow Diagram (Fig. 1) and in the Supplementary Materials (Supplementary Table 1). Fifteen studies were eligible for inclusion, three of which are ongoing. Therefore, the narrative synthesis included twelve studies.
Study characteristics
Twelve studies investigated multi-gene, multi-drug, multi-disease pharmacogenetic interventions in adults with multimorbidity and polypharmacy (Table 1). Six non-comparative studies [56,57,58,59,60,61], three observational studies [62,63,64], and three randomised controlled trials were included [65,66,67]. Meta-analysis was not suitable for the randomised studies; there was clinical and methodological diversity in these studies owing to variability in the outcomes assessed. The studies were predominantly US-based [56, 57, 59,60,61, 63,64,65,66,67], with the remainder conducted in Canada [58] and the Netherlands [62]. The comparative studies often used a control group untested for pharmacogenetics [64,65,66], or the control group was tested and the results withheld [67]. In the nested case-control and cross-sectional study, each participant underwent pharmacogenetic testing; in the former, comparisons were made between cases with frequent and controls with infrequent hospitalisations [63], while the latter made comparisons against a group lacking drug-gene interactions [62].
The included studies predominantly took place in primary care, except for one study assessing the impact of pharmacogenetic profiling on in-hospital prescribing [61]. The majority of the included studies involved explicit pharmacist-led medication management with recommendations forwarded to patients’ physicians. Mean age ranged from 57 to 78 years, the proportion of males ranged from 31% to 67%, the mean number of conditions and medications ranged from 5 to 8 and 4 to 20, respectively, and most participants were of Caucasian ethnicity (67–99%). Similarities were evident in the genetic testing approach, with a core panel consisting of CYP2C9, CYP2C19, CYP2D6, CYP3A4, CYP3A5 and VKORC1. Various clinical decision support (CDS) systems were employed: YouScript [64,65,66], GENETWORx [59, 63], IDgenetix [57, 67], GeneYouIn [58], uMETHOD Health [60], Genomic Prescribing System [61], and PRIMER [56].
Summary of results
Four studies investigated the impact of pharmacogenetic interventions on healthcare utilisation. Reductions in hospitalisations and emergency department visits were observed following genetic testing and medicines optimisation [64, 66]. Brixner et al. reported reductions in hospitalisations and emergency department visits by 40% (p < 0.05) and 70% (p < 0.001), respectively [64], while Elliott et al. found reductions of 52% (p < 0.01) and 42% (p < 0.05), respectively [66]. A 47% increase in outpatients visits (p < 0.0001) in patients undergoing pharmacogenetic testing was reported by Brixner et al. [64]. Elevated rates of hospitalisation in elderly patients with pharmacogenetic polymorphisms was recorded by Finkelstein et al. (p < 0.05) [63]. Van der Wouden et al. found no significant differences in healthcare utilisation [62].
Estimated improvements in healthcare costs were reported in several studies. Brixner et al. found the cost of genetic testing was nearly or completely offset by savings resulting from decreased healthcare utilisation using mean and median national data. Using the mean, savings of $1132 per patient were made, while the median resulted in savings of $788 during the 16-week follow-up [64]. Elliott et al. modelled cost saving based on Medicare average all-cause readmission and emergency department cost, yielding savings of $4 382 per patient over the 8-week follow-up [66]. Two studies performed in long-term care facilities estimated cost savings of ~$1430 and $3000 over 2.3 years (average length of stay) [57, 67].
Actionable pharmacogenetic polymorphisms were ubiquitous. The potential for enhanced medication safety through drug interaction management was demonstrated, with up to seven gene-based drug interaction recommendations per patient [56,57,58,59,60,61,62,63,64,65,66,67]. Elliott et al. reported most patients carried at least one aberrant CYP variant [66]. Reynolds et al. identified drug-gene interactions in 78% of their participants [56]. Sugarman et al. reported medication change reasons were exclusively genetic in 28% of patients. For patients whose medications remained unchanged, a high proportion of genetic variations that could impact future prescriptions was observed [57]. Van der Wouden et al. identified targets for pharmacogenetic testing, reporting the number of newly initiated prescriptions with potential drug-gene interactions increases with age and number of comorbidities and comedications, but this was not found to be statistically significant [62]. Lee et al. suggested inpatient prescribing could be informed by pre-emptive genotyping those at risk of hospitalisation (elderly polypharmacy patients), as many prescriptions initiated in hospital included pharmacogenetic medications [61].
Clinical decision-making appeared reinforced by the interventions. Physicians followed between 30% and 79% of the medication-related problem recommendations [56, 58, 64,65,66]. Associations were found between physician acceptance and recommendation seriousness [64, 65] and if the recommendation involved pharmacogenetics [58]. Van der Wouden et al. demonstrated the importance of accurate record keeping to maintain the value of genetic testing. Within 2.5 years, a mean of 2.71 drugs for which results were available were prescribed; 24% of these were actionable drug-gene interactions. Pharmacists were found to be better able to record pharmacogenetic data than general practitioners (96% vs. 68%) [62]. Clinical outcomes, while prioritised in the core outcome sets [68, 69], were only described in Elliott et al. [66]. A statistically insignificant reduction in mortality was reported; however, the study was not powered for mortality and included this outcome post-hoc. Select quality metrics (such as pain, depression, and anxiety) and the number of falls were also recorded, demonstrating relatively small differences [66].
Risk of bias
The risk of bias assessment is detailed in the Supplementary Materials (Supplementary Table 2) and summarised in Figs. 2, 3. Overall, the risk of bias ranged from moderate/some concerns to high risk. RoB 2 was used for two randomised studies [65, 66]. Elliott et al. was found to be at high risk of bias [66], while Kim et al. had some concerns [65]. ROBINS-I was used for two non-randomised studies [62, 64]; both were found to be at moderate risk of bias. The study by Saldivar et al. was designed as a randomised trial; however, it is an “initial assessment” and provides non-comparative results [67]. Similarly, the case-control study by Finkelstein et al. did not compare the effect of the intervention received [63]. It was not possible to assess non‐comparative studies because it is a prerequisite in ROBINS-I that there is a comparative study. Non‐comparative studies were considered at critical risk of bias mostly due to confounding factors [70].
Summary of relevant ongoing studies
Three ongoing trials were eligible [41, 71, 72]. Recruitment is ongoing for Stingl et al. (DRKS00006256) and Delate et al. (NCT04120480), while the third trial by van der Wouden et al. (NCT03093818) is active but not recruiting. The German iDrug primary care randomised controlled trial (Stingl et al.) involves elderly multimorbid and polypharmacy patients randomised to receive an individual risk assessment (including drug-drug interactions and pharmacogenetics) or a standardised risk assessment (without individualised information) to analyse the effect this information has on adverse events [71]. Outcomes include mortality, healthcare utilisation, costs, medication changes, adverse drug reactions and quality of life. The estimated completion date is not reported.
In the United States, Delate et al. are conducting a pharmacist-led randomised controlled trial involving high-risk polypharmacy patients randomised to receive pharmacogenetic-guided treatment or usual care to determine clinical and economic effectiveness [72]. The investigators hypothesise that pharmacogenetic testing and pharmacist review of medication appropriateness will lower one-year healthcare utilisation and costs compared to controls. Outcomes include healthcare utilisation, costs, medication changes, medication congruence and adherence. The estimated completion date is December 2022.
The PREPARE randomised controlled trial (van der Wouden et al.) conducted in several European countries has an estimated completion date of April 2021, with results yet to be published [41]. In this trial, adults receiving a first prescription for one or more of 42 medications with a DPWG guideline were randomised to receive pharmacogenetic-guided treatment or usual care. In the intervention group, pharmacogenetic results may be used to guide medication and dose selection per DPWG guidelines. Patients receive a “Safety-Code card” containing their pharmacogenetic results, which can be used by other healthcare professionals during subsequent prescriptions. Outcomes include costs, adverse drug reactions, medication changes, quality of life, attitude towards and knowledge of pharmacogenetics, and physician and pharmacist adherence to DPWG guidelines.
General process model
To aid the development of future pharmacogenetic interventions, a process diagram derived from the steps described in each of the included studies was produced (Fig. 4). This model outlines the steps required for a pharmacogenetic intervention that can prompt medicines optimisation, patient benefit and reduction in adverse events.
Discussion
This is the first systematic review to examine the effectiveness of multi-drug pharmacogenetic interventions in the management of those with multimorbidity and/or prescribed polypharmacy. This study demonstrates that once the scope of the review extends beyond single drug-gene interactions there is limited available evidence. Following retrieval of 10,725 records, fifteen studies were eligible for inclusion, three of which are ongoing, limiting the conclusions that can be drawn. Nevertheless, the included study by Elliott et al. provides randomised controlled trial evidence, albeit in a small, selected population, in favour of the incorporation of pharmacogenetic testing in primary care to improve outcomes for those with multimorbidity and polypharmacy [66]. Interpretations from the other randomised studies are limited by the post-hoc design of Kim et al. and the lack of information provided by Saldivar et al. [65, 67]. In general, medicines optimisation approaches currently do not incorporate pharmacogenetics as a cause of medication-related problems [73, 74]. Conversely, pharmacogenetics is a source of such problems, and could add an important new dimension to conventional drug interaction assessment processes. Most of the search results were published in just the past decade, highlighting that pharmacogenetics is an emerging field. Three ongoing trials, one of which is being conducted throughout Europe (the PREPARE study), has recruited almost 7000 participants and will provide important new evidence [41]. These and more pragmatic studies in diverse, real-world patient populations, are required to establish the benefit of multi-medicine pharmacogenetics.
The heterogeneity of study designs employed in this space must be addressed. Lack of evidence from gold standard randomised controlled trials is frequently cited as a reason to delay pharmacogenetics implementation, despite a substantial evidence base and published guidelines. This necessity has been challenged [75,76,77,78]; many argue that the perceived mandatory requirement for prospective evidence to support the clinical validity of a pharmacogenetic test, prior to its implementation into routine care, is inappropriate and unreasonable [75,76,77,78]. There are suggestions to use alternative forms of evidence such as smaller-scale, non-randomised clinical studies, and strong observational evidence [52, 79,80,81,82]. However, limitations exist, and designs such as case-control and cohort studies, that are very common in pharmacogenetics, can be prone to confounding and various biases [79, 83]. Thus, the conclusions that can be drawn from included studies using such alternative designs are limited [56,57,58,59,60,61,62,63,64, 67]. This underlines the importance of and need for more robust, well-designed, pragmatic, randomised controlled trials with large sample sizes, such as the PREPARE study [41]. Further good quality evidence will help establish the true efficacy and utility of pharmacogenetics in personalised patient care, and to advance the discovery and development of appropriate patient outcome improvement strategies.
This systematic review provides various considerations for future studies. A collaborative, primary care approach involving physicians, pharmacists, and patients was shown to underly the implementation of pharmacogenetics (Fig. 4). With their training, frequent patient contact and role in medicines optimisation as well as medication surveillance, pharmacists may be leading candidates to manage incorporating pharmacogenetics into medicines optimisation [84]. Pharmacists’ knowledge of pharmacokinetics and pharmacodynamics may be useful in the clinical application of pharmacogenetics [85]. This is supported by the majority of studies included in this review involving pharmacist-led medication management, as well as by other pilot studies performed in pharmacy settings [45,46,47, 86, 87]. Studies have demonstrated pharmacists’ interest in incorporating pharmacogenetic services into their practices, albeit further education may be required [88,89,90]. Comprehensive continuing professional development courses, that developed in the PRIME study [39], may improve knowledge, readiness and comfort in applying pharmacogenetics to patient care [39, 91]. Both community pharmacists and general practitioners may have long-term, regular roles in the care of polypharmacy patients and are able to record the results of pharmacogenetics tests in their EHRs [62], a pivotal facilitator of clinical utility and cost-effectiveness of pharmacogenetic testing. Thus, pharmacogenetic testing in pharmacy practice may be considered appropriate and could play an important role in moving pharmacogenetics from research to patient care.
However, pharmacogenetics implementation barriers exist. Evidence of cost-effectiveness and testing utility is another major barrier to the broader implementation of pharmacogenetics [18, 42, 51, 53, 55]. There has been considerable debate around the optimal approach to pharmacogenetic testing in clinical practice, particularly the methodology of genotyping [92]. Some support reactive genotyping for a single drug-gene interaction at the point of prescribing, and others a pre-emptive panel-based approach prior to prescribing [92]. The former approach has several disadvantages. For instance, if patients receive prescriptions for multiple drugs with pharmacogenetic implications, they may require additional testing for multiple single genes. Here, the cost of testing is amplified, and treatment may be delayed awaiting the test results [62, 92]. Since the overall cost of panel-based and single gene tests are similar, a pre-emptive panel approach may alleviate these concerns, as highlighted by the PREDICT study [24]. The ordering of 14,656 genetic tests was avoided when data on multiple genes was available beforehand, thereby saving genotyping test costs by reducing the number of single tests by 60% [24]. The multi-drug, multi-gene scope of this review provided auspicious estimates of cost-savings [57, 64, 66, 67]. Considering the follow-up durations were short and that the pharmacogenetic test results are lifelong, the value obtained from a one-time expense of testing is likely to increase over time with ongoing patient management. Compared to the previous testing methods, whole genome sequencing offers more in-depth information [44]; however, the associated expense, immense data, extended test turnaround times, and complex interpretation arguably makes a panel-based approach a better suited technology for larger scale implementation at present [42, 44]. Another important consideration is the cost to the healthcare professional, for instance, unreimbursed time spent counselling, ordering pharmacogenetic tests, and conducting medicines optimisation [55].
Furthermore, primary care workforce education and support regarding pharmacogenetics and a proper infrastructure for the integration of pharmacogenetics are crucial to pave the way for accessible pharmacogenetics [41, 42, 51,52,53,54,55]. The latter barrier may be overcome by greater integration of pharmacogenetic results into electronic health records (EHRs), and development and deployment of CDS as part of EHRs [93]. In the US, several implementation studies integrating pharmacogenetic test results into the EHR and CDS systems have been initiated, such as the eMERGE-PGx, IGNITE, INGENIOUS, and PG4KDS studies [18, 41]. For healthcare systems with limited EHR infrastructure, the “Safety Code card” used in European PREPARE study may be a viable option to make pharmacogenetic data and CDS available [41, 94]. This card is part of a mobile-based CDS system that is independent of existing information technology infrastructures, and after scanning the quick response code, enables retrieval of patient-relevant pharmacogenetic dosing guidelines [94]. In lieu of a nationwide EHR, an approach such as this may ameliorate accessibility and sharing of pharmacogenetic results within and between different healthcare setting and healthcare professionals.
This review is strengthened by its pragmatic focus, examining the effectiveness of multi-drug pharmacogenetic-guided therapy in the care of those with multimorbidity or polypharmacy compared with the established literature focusing on one singular drug, disease, or limited drug-gene combinations. This review placed no restriction on language or geographical region, enabling a broader view of pharmacogenetic interventions internationally. Our review is also strengthened by the robust methodology used and was developed in accordance with the PRISMA statement and Cochrane tools were used to assess the risk of bias.
Limitations
This study has some limitations to consider. First, only a narrative analysis was performed due to significant heterogeneity in the articles included. Thus, the results only provide a high-level representation of the impact of pharmacogenetic testing in patients with multimorbidity and/or polypharmacy. Second, we are constrained by the sparsity of evidence available on the efficacy of pharmacogenetics in this area. The dearth of gold-standard randomised controlled trial evidence in this area necessitated the need to include observational studies and non-comparative studies. Finally, studies undertaken in multimorbid populations with a specific focus on a single drug or drug class were not included, and we await the results of the largest, pragmatic study of pharmacogenetics undertaken to date [41].
Conclusions
The incorporation of pharmacogenetic testing into the medicines optimisation process could have significant benefits for healthcare providers and for patients by reducing healthcare utilisation and costs, enhancing identification of clinically significant drug interactions, and improving clinical decision-making. Due to a lack of methodologically robust, high quality studies, small sample sizes, and relatively short follow-up durations, we found limited evidence on the efficacy of pharmacogenetic interventions to improve outcomes in patients with multimorbidity or prescribed polypharmacy. In one small, randomised study, encouraging results using a multi-gene, multi-disease, multi-drug pharmacogenetic approach as part of medicines optimisation by a pharmacist were found. We conclude that pharmacogenetic-guided therapy holds promise for individualising therapy; however, further robust, pragmatic studies, in all patient care settings, are required to establish the impact pharmacogenetic screening has on patient outcomes.
Materials and methods
This systematic review was registered with PROSPERO (registration number CRD42020178126), and was developed in accordance with the PRISMA 2020 statement [95, 96]. Study inclusion was based on the Cochrane EPOC Checklist (which included randomised trials, non-randomised trials, controlled before-after studies, and interrupted time series analyses) [97], as well as observational and non-comparative studies. Broad study designs were included to ensure a comprehensive report on the available literature was produced.
Search strategy
We systematically searched PubMed, Embase, Cochrane CENTRAL, CINAHL, AMED, and PsycInfo from inception to April 2020, using keywords and controlled vocabulary related to ‘pharmacogenetics’, ‘pharmacogenomics’, ‘multimorbidity’ and ‘polypharmacy’ without restricting the language of publication. The search strategy was developed in collaboration with an expert subject librarian. We conducted searches for ongoing or unpublished trials on ClinicalTrials.gov (www.clinicaltrials.gov), the EU Clinical Trials Register (www.clinicaltrialsregister.eu), and the WHO International Clinical Trials Register (http://apps.who.int/trialsearch). The search strategy is reported in the Supplementary Materials (Supplementary Table 3).
Study selection
Studies were included if they met the following criteria: investigated interventions involving multi-gene, multi-drug, multi-disease pharmacogenetic-guided treatment; recruited participants ≥18 years experiencing multimorbidity (the presence of two or more chronic conditions in the same individual [2]) or prescribed polypharmacy (the prescribing of four or more medicines [3]); and reported on at least two outcomes derived from multimorbidity and polypharmacy consensus-based core outcome sets in Table 2 [68, 69]. We included all healthcare settings and interventions provided by any healthcare professional. Studies involving single gene, single drug, single disease pharmacogenetic interventions, malignancy, palliative care, human immunodeficiency virus and hepatitis were excluded. Study selection involved a two-phase screening and eligibility determination process by two reviewers independently through Covidence [98]. Initially, titles and abstracts were assessed for relevancy, followed by a full-text review.
Data extraction
Data extraction was conducted by two reviewers independently, focusing on four domains: [1] characteristics of study (study design, sample size, follow-up duration, inclusion criteria), [2] patient demographics (age, gender, ethnicity, number of chronic conditions and concomitant medications), [3] details about the intervention (pharmacogenetic component(s), description of the intervention and control) and [4] study findings (outcomes and results). Additional information related to the publication (funding and conflicts of interest) was also collected to assess study quality.
Quality assessment
The risk of bias was assessed by two reviewers independently using the Cochrane RoB 2 and ROBINS-I tools for randomised and non-randomised studies, respectively [70, 99]. The RoB 2 tool provides a framework for assessing the risk of bias against five domains: the randomisation process; deviations from the intended interventions; missing outcome data; measurement of the outcome; and selection of the reported result. ROBINS-I has seven domains: confounding; selection of participants into the study; classification of interventions; deviations from intended interventions; missing data; measurement of outcomes; and selection of the reported result. The potential sources of bias in RoB 2 were graded ‘low’, ‘some concerns’ or ‘high’, and ROBINS-I as ‘low’, ‘moderate’, ‘serious’ or ‘critical’. The risk of bias figures were generated using robvis [100].
Presentation of results
Because of the heterogeneity in the methods and outcomes of included studies, it was not possible to conduct a meta-analysis. The findings of this study are reported as a narrative synthesis and include a description of the study characteristics and a summary of the study results.
Change history
30 March 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41397-022-00273-9
References
United Nations, 2019. World population prospects. Volume II: Demographic profiles. Department of Economic and Social Affairs.
Smith SM, Wallace E, O'Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2016;3:CD006560.
Rankin A, Cadogan CA, Patterson SM, Kerse N, Cardwell CR, et al. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev. 2018;9:CD008165.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet. 2012;380:37–43.
Midao L, Giardini A, Menditto E, Kardas P, Costa E. Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Arch Gerontol Geriatr. 2018;78:213–20.
Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10:430–9.
Guthrie B, Makubate B, Hernandez-Santiago V, Dreischulte T. The rising tide of polypharmacy and drug-drug interactions: population database analysis 1995–2010. BMC Med. 2015;13:74.
Chamberlain AM, Rutten LJF, Jacobson DJ, Fan C, Wilson PM, Rocca WA, et al. Multimorbidity, functional limitations, and outcomes: interactions in a population-based cohort of older adults. J Comorb. 2019;9:2235042X19873486–42X.
Glynn LG, Valderas J, Healy P, Burke E, Newell J, Gillespie P, et al. the prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pr. 2011;28:516–23.
Fried TR, O’Leary J, Towle V, Goldstein MK, Trentalange M, Martin DK. Health outcomes associated with polypharmacy in community-dwelling older adults: a systematic review. J Am Geriatr Soc. 2014;62:2261–72.
Cahir C, Fahey T, Teeling M, Teljeur C, Feely J, Bennett K. Potentially inappropriate prescribing and cost outcomes for older people: a national population study. Br J Clin Pharm. 2010;69:543–52.
Hughes LD, McMurdo MET, Guthrie B. Guidelines for people not for diseases: the challenges of applying UK clinical guidelines to people with multimorbidity. Age Ageing. 2012;42:62–9.
World Health Organisation (WHO). Multimorbidity: technical series on safer primary care. 2016. Available at: http://apps.who.int/iris/bitstream/handle/10665/252275/9789241511650-eng.pdf;jsessionid=ADDF324823B1FE41ED08BAA0DF247550?sequence=1. Accessed on: April 28, 2021.
National Institute for Health and Care Excellence (NICE). Multimorbidity: clinical assessment and management NICE Guideline [NG56]. 2016. Available at: https://www.nice.org.uk/guidance/ng56/resources/multimorbidity-clinical-assessment-and-management-pdf-1837516654789. Accessed on: April 28, 2021.
Scottish Government Polypharmacy Model of Care Group. Polypharmacy guidance, realistic prescribing 3rd edition. 2018. Available at: https://www.therapeutics.scot.nhs.uk/wp-content/uploads/2018/04/Polypharmacy-Guidance-2018.pdf. Accessed on: April 28, 2021.
El Morabet N, Uitvlugt EB, van den Bemt BJF, van den Bemt PMLA, Janssen MJA, Karapinar-Çarkit F. Prevalence and preventability of drug-related hospital readmissions: a systematic review. J Am Geriatr Soc. 2018;66:602–8.
Malki MA, Pearson ER. Drug-drug-gene interactions and adverse drug reactions. Pharmacogenomics J. 2020;20:355–66.
Eichelbaum M, Ingelman-Sundberg M, Evans WE. Pharmacogenomics and individualized drug therapy. Annu Rev 842 Med. 2006;57:119–37.
Dunnenberger HM, Crews KR, Hoffman JM, Caudle KE, Broeckel U, Howard SC, et al. Preemptive clinical pharmacogenetics implementation: current programs in five US medical centers. Annu Rev Pharm Toxicol. 2015;55:89–106.
Bush WS, Crosslin DR, Owusu-Obeng A, Wallace J, Almoguera B, Basford MA, et al. Genetic variation among 82 pharmacogenes: the PGRNseq data from the eMERGE network. Clin Pharm Ther. 2016;100:160–9.
Ji Y, Skierka JM, Blommel JH, Moore BE, VanCuyk DL, Bruflat JK, et al. Preemptive pharmacogenomic testing for precision medicine: a comprehensive analysis of five actionable pharmacogenomic genes using next-generation DNA sequencing and a customized CYP2D6 genotyping cascade. J Mol Diagn. 2016;18:438–45.
Pirmohamed M. Pharmacogenetics and pharmacogenomics. Br J Clin Pharm. 2001;52:345–7.
Verbeurgt P, Mamiya T, Oesterheld J. How common are drug and gene interactions? Prevalence in a sample of 1143 patients with CYP2C9, CYP2C19 and CYP2D6 genotyping. Pharmacogenomics. 2014;15:655–65.
Van Driest SL, Shi Y, Bowton EA, Schildcrout JS, Peterson JF, Pulley J, et al. Clinically actionable genotypes among 10,000 patients with preemptive pharmacogenomic testing. Clin Pharm Ther. 2014;95:423–31.
Youssef E, Kirkdale CL, Wright DJ, Guchelaar HJ, Thornley T. Estimating the potential impact of implementing pre-emptive pharmacogenetic testing in primary care across the UK. Br J Clin Pharmacol. 2021;87:2907–25.
Brockmoller J, Stingl JC. Multimorbidity, polypharmacy and pharmacogenomics in old age. Pharmacogenomics. 2017;18:515–7.
Mallal S, Phillips E, Carosi G, Molina JM, Workman C, Tomažič J, et al. HLA-B*5701 screening for hypersensitivity to abacavir. N. Engl J Med. 2008;358:568–79.
Pirmohamed M, Burnside G, Eriksson N, Jorgensen AL, Toh CH, Nicholson T, et al. A randomized trial of genotype-guided dosing of warfarin. N. Engl J Med. 2013;369:2294–303.
Roberts JD, Wells GA, Le May MR, Labinaz M, Glover C, Froeschl M, et al. Point-of-care genetic testing for personalisation of antiplatelet treatment (RAPID GENE): a prospective, randomised, proof-of-concept trial. Lancet. 2012;379:1705–11.
Kimmel SE, French B, Kasner SE, Johnson JA, Anderson JL, Gage BF, et al. A pharmacogenetic versus a clinical algorithm for warfarin dosing. N. Engl J Med. 2013;369:2283–93.
Verhoef TI, Ragia G, de Boer A, Barallon R, Kolovou G, Kolovou V, et al. A randomized trial of genotype-guided dosing of acenocoumarol and phenprocoumon. N. Engl J Med. 2013;369:2304–12.
Bradley P, Shiekh M, Mehra V, Vrbicky K, Layle S, Olson MC, et al. Improved efficacy with targeted pharmacogenetic-guided treatment of patients with depression and anxiety: a randomized clinical trial demonstrating clinical utility. J Psychiatr Res. 2018;96:100–7.
Greden JF, Parikh S, Rothschild AJ, Thase ME, Dunlop BW, DeBattista C, et al. Impact of pharmacogenomics on clinical outcomes in major depressive disorder in the GUIDED Trial: a large, patient- and rater-blinded, randomized, controlled study. J Psychiatr Res. 2019;111:59–67.
Ruano G, Robinson S, Holford T, Mehendru R, Baker S, Tortora J, et al. Results of the CYP-GUIDES randomized controlled trial: Total cohort and primary endpoints. Contemp Clin Trials. 2020;89:105910.
Herbild L, Andersen SE, Werge T, Rasmussen HB, Jürgens G. Does pharmacogenetic testing for CYP450 2D6 and 2C19 among patients with diagnoses within the schizophrenic spectrum reduce treatment costs? Basic Clin Pharm Toxicol. 2013;113:266–72.
Notarangelo FM, Maglietta G, Bevilacqua P, Cereda M, Merlini PA, Villani GQ, et al. Pharmacogenomic approach to selecting antiplatelet therapy in patients with acute coronary syndromes: The PHARMCLO trial. J Am Coll Cardiol. 2018;71:1869–77.
Peyser B, Perry EP, Singh K, Gill RS, Mehan MR, Haga SB, et al. Effects of delivering SLCO1B1 pharmacogenetic information in randomized trial and observational settings. Circ Genom Precis Med. 2018;11:e002228.
Coenen MJH, de Jong DJ, van Marrewijk CJ, Derijks LJJ, Vermeulen SH, Wong DR, et al. Identification of patients with variants in TPMT and dose reduction reduces hematologic events during thiopurine treatment of inflammatory bowel disease. Gastroenterology. 2015;149:907–17.e7.
Crown N, Sproule BA, Luke MJ, Piquette-Miller M, McCarthy LM. A continuing professional development program for pharmacists implementing pharmacogenomics into practice. Pharmacy. 2020;8:55.
Herbert D, Neves-Pereira M, Baidya R, Cheema S, Groleau S, Shahmirian A, et al. Genetic testing as a supporting tool in prescribing psychiatric medication: Design and protocol of the IMPACT study. J Psychiatr Res. 2018;96:265–72.
van der Wouden CH, Cambon-Thomsen A, Cecchin E, Cheung KC, Dávila-Fajardo CL, Deneer VH, et al. Implementing pharmacogenomics in Europe: design and implementation strategy of the Ubiquitous Pharmacogenomics Consortium. Clin Pharm Ther. 2017;101:341–58.
Krebs K, Milani L. Translating pharmacogenomics into clinical decisions: do not let the perfect be the enemy of the good. Hum Genomics. 2019;13:39.
Klein ME, Parvez MM, Shin JG. Clinical implementation of pharmacogenomics for personalized precision medicine: Barriers and solutions. J Pharm Sci. 2017;106:2368–79.
Rollinson V, Turner R, Pirmohamed M. Pharmacogenomics for primary care: an overview. Genes (Basel). 2020;11:1337.
Ferreri SP, Greco AJ, Michaels NM, O’Connor SK, Chater RW, Viera AJ, et al. Implementation of a pharmacogenomics service in a community pharmacy. J Am Pharm Assoc. 2003;2014:172–80.
Swen J, Straaten T, Wessels J, Bouvy M, Vlassak E, Assendelft W, et al. Feasibility of pharmacy-initiated pharmacogenetic screening for CYP2D6 and CYP2C19. Eur. J Clin Pharm. 2012;68:363–70.
Bank PCD, Swen JJ, Schaap RD, Klootwijk DB, Baak-Pablo R, Guchelaar HJ. A pilot study of the implementation of pharmacogenomic pharmacist initiated pre-emptive testing in primary care. Eur J Hum Genet. 2019;27:1532–41.
GOV.UK. Department of Health and Social Care. Genome UK: the future of healthcare. 2020. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/920378/Genome_UK_-_the_future_of_healthcare.pdf. Accessed on: April 28, 2021.
Bank PCD, Caudle KE, Swen JJ, Gammal RS, Whirl-Carrillo M, Klein TE, et al. Comparison of the guidelines of the Clinical Pharmacogenetics Implementation Consortium and the Dutch Pharmacogenetics Working Group. Clin Pharm Ther. 2018;103:599–618.
The Pharmacogenomics Knowledge Base (PharmGKB). Clinical guideline annotations. Avaiable at: https://www.pharmgkb.org/. April, 2021.
Mikat-Stevens NA, Larson I, Tarini BA. Primary-care providers’ perceived barriers to integration of genetics services: a systematic review of the literature. Genet Med. 2015;17:169–76.
Slob EMA, Vijverberg SJH, Pijnenburg MW, Koppelman GH, van der Zee AHM. What do we need to transfer pharmacogenetics findings into the clinic? Pharmacogenomics. 2018;19:589–92.
Ventola CL. Pharmacogenomics in clinical practice: reality and expectations. P T. 2011;36:412–50.
Haga SB, Allen LaPointe NM, Moaddeb J. Challenges to integrating pharmacogenetic testing into medication therapy management. J Manag Care Spec Pharm. 2015;21:346–52.
Rigter T, Jansen ME, de Groot JM, Janssen SWJ, Rodenburg W, Cornel MC. Implementation of pharmacogenetics in primary care: A multi-stakeholder perspective. Front Genet. 2020;11:10.
Reynolds KK, Pierce DL, Weitendorf F, Linder MW. Avoidable drug-gene conflicts and polypharmacy interactions in patients participating in a personalized medicine program. Per Med. 2017;14:221–33.
Sugarman E, Cullors A, Centeno J, Taylor D. Contribution of pharmacogenetic testing to modeled medication change recommendations in a long-term care population with polypharmacy. Drugs Aging. 2016;33:929–36.
Papastergiou J, Tolios P, Li W, Li J. Innovative Canadian pharmacogenomic screening initiative in community pharmacy (ICANPIC) study. Int J Clin Pharm. 2017;39:331–2.
Finkelstein J, Friedman C, Hripcsak G, Cabrera M. Potential utility of precision medicine for older adults with polypharmacy: a case series study. Pharmgenomics Pers Med. 2016;9:31–45.
Keine D, Zelek M, Walker JQ, Sabbagh MN. Polypharmacy in an elderly population: enhancing medication management through the use of clinical decision support software platforms. Neurol Ther. 2019;8:79–94.
Lee YM, Danahey K, Knoebel RW, Ratain MJ, Meltzer DO, O’Donnell PH. Analysis of comprehensive pharmacogenomic profiling to impact in-hospital prescribing. Pharmacogenet Genomics. 2019;29:23–30.
van der Wouden CH, Bank PCD, Özokcu K, Swen JJ, Guchelaar HJ. Pharmacist-initiated pre-emptive pharmacogenetic panel testing with clinical decision support in primary care: record of PGx results and real-world impact. Genes. 2019;10:416.
Finkelstein J, Friedman C, Hripcsak G, Cabrera M. Pharmacogenetic polymorphism as an independent risk factor for frequent hospitalizations in older adults with polypharmacy: a pilot study. Pharmgenomics Pers Med. 2016;9:107–16.
Brixner D, Biltaji E, Bress A, Unni S, Ye X, Mamiya T, et al. The effect of pharmacogenetic profiling with a clinical decision support tool on healthcare resource utilization and estimated costs in the elderly exposed to polypharmacy. J Med Econ. 2016;19:213–28.
Kim K, Magness J, Nelson R, Baron V, Brixner DI. Clinical utility of pharmacogenetic testing and a clinical decision support tool to enhance the identification of drug therapy problems through medication therapy management in polypharmacy patients. J Manag Care Spec Pharm. 2018;24:1250–9.
Elliott LS, Henderson JC, Neradilek MB, Moyer NA, Ashcraft KC, Thirumaran RK. Clinical impact of pharmacogenetic profiling with a clinical decision support tool in polypharmacy home health patients: a prospective pilot randomized controlled trial. PLoS ONE. 2017;12:e0170905.
Saldivar JS, Taylor D, Sugarman EA, Cullors A, Garces JA, Oades K, et al. Initial assessment of the benefits of implementing pharmacogenetics into the medical management of patients in a long-term care facility. Pharmgenomics Pers Med. 2016;9:1–6.
Smith SM, Wallce E, Salisbury C, Sasseville M, Bayliss E, Fortin M. A core outcome set for multimorbidity research (COSmm). Ann Fam Med. 2018;16:132–8.
Rankin A, Cadogan CA, Ryan C, Clyne B, Smith SM, Hughes CM. Core outcome set for trials aimed at improving the appropriateness of polypharmacy in older people in primary care. J Am Geriatr Soc. 2018;66:1206–12.
Sterne JAC, Hernan M, Reeves BC, Savovic J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;355:i4919.
Stingl JC, Kaumanns KL, Claus K, Lehmann ML, Kastenmuller K, Bleckwenn M, et al. Individualized versus standardized risk assessment in patients at high risk for adverse drug reactions (IDrug) - study protocol for a pragmatic randomized controlled trial. BMC Fam Pr. 2016;17:1–8.
Delate T, Quinn A. Effectiveness of PGx testing. 2019. Available at: https://clinicaltrials.gov/ct2/show/NCT04120480. Accessed on: April 28, 2021.
Hersberger KE, Griese-Mammen N, Kos M, Horvat N, Messerli M, van Mil FJW. Pharmaceutical Care Network Europe - Position paper on the PCNE definition of medication review. PCNE Working Group. 2016. Available at: https://www.pcne.org/upload/files/149_Position_Paper_on_PCNE_Medication_Review_final.pdf. Accessed on: April 28, 2021.
van Mil FJW, Horvat N, Westerlund T. Pharmaceutical Care Network Europe - Classification for drug related problems. PCNE Working Group. 2017. Available at: https://www.pcne.org/upload/files/215_PCNE_classification_V8-01.pdf. Accessed on: April 28, 2021.
Altman RB. Pharmacogenomics: “Noninferiority” is sufficient for initial implementation. Clin Pharm Ther. 2011;89:348–50.
van der Wouden CH, Swen JJ, Samwald M, Mitropoulou C, Schwab M, Guchelaar HJ. A brighter future for the implementation of pharmacogenomic testing. Eur J Hum Genet. 2016;24:1658–60.
Pirmohamed M, Hughes DA. Pharmacogenetic tests: the need for a level playing field. Nat Rev Drug Disco. 2013;12:3–4.
Khoury MJ. Dealing with the evidence dilemma in genomics and personalized medicine. Clin Pharm Ther. 2010;87:635–8.
Ross S, Anand SS, Joseph P, Paré G. Promises and challenges of pharmacogenetics: an overview of study design, methodological and statistical issues. JRSM Cardiovascular Dis. 2012;1:cvd.2012.012001.
Huddart R, Sangkuhl K, Whirl-Carrillo M, Klein TE. Are randomized controlled trials necessary to establish the value of implementing pharmacogenomics in the clinic? Clin Pharm Ther. 2019;106:284–6.
Frueh FW. Back to the future: why randomized controlled trials cannot be the answer to pharmacogenomics and personalized medicine. Pharmacogenomics. 2009;10:1077–81.
Cavallari LH, Pratt VM. Building evidence for clinical use of pharmacogenomics and reimbursement for testing. Adv Mol Pathol. 2018;1:125–34.
Stingl J, Brockmoller J. Chapter 9 - Study designs in clinical pharmacogenetic and pharmacogenomic research. Pharmacogenomics. San Diego: Academic Press; 2013. p. 309–41.
American Society of Health-System Pharmacists (ASHP). ASHP statement on the pharmacist’s role in clinical pharmacogenomics. Am J Health-Syst Pharm. 2015;72:579–81.
Elewa H, Awaisu A. Pharmacogenomics in pharmacy practice: current perspectives. Integr Pharm Res Pract. 2019;8:97–104.
Crews KR, Cross SJ, McCormick JN, Baker DK, Molinelli AR, Mullins R, et al. Development and implementation of a pharmacist-managed clinical pharmacogenetics service. Am J Health Syst Pharm. 2011;68:143–50.
Haga SB, LaPointe NM, Cho A, Reed SD, Mills R, Moaddeb J, et al. Pilot study of pharmacist-assisted delivery of pharmacogenetic testing in a primary care setting. Pharmacogenomics. 2014;15:1677–86.
Alexander KM, Divine HS, Hanna CR, Gokun Y, Freeman PR. Implementation of personalized medicine services in community pharmacies: perceptions of independent community pharmacists. J Am Pharm Assoc. 2014;54:510–7.
de Denus S, Letarte N, Hurlimann T, Lambert JP, Lavoie A, Robb L, et al. An evaluation of pharmacists’ expectations towards pharmacogenomics. Pharmacogenomics. 2013;14:165–75.
McCullough KB, Formea CM, Berg KD, Burzynski JA, Cunningham JL, Ou NN, et al. Assessment of the pharmacogenomics educational needs of pharmacists. Am J Pharm Educ. 2011;75:51.
Kennedy MJ. Personalized medicines – are pharmacists ready for the challenge? Integr Pharm Res Pr. 2018;7:113–23.
Weitzel KW, Cavallari LH, Lesko LJ. Preemptive panel-based pharmacogenetic testing: the time is now. Pharm Res. 2017;34:1551–5.
Hicks JK, Stowe D, Willner MA, Wai M, Daly T, Gordon SM, et al. Implementation of clinical pharmacogenomics within a large health system: from electronic health record decision support to consultation services. Pharmacotherapy: J Hum Pharmacol Drug Ther. 2016;36:940–8.
Blagec K, Romagnoli KM, Boyce RD, Samwald M. Examining perceptions of the usefulness and usability of a mobile-based system for pharmacogenomics clinical decision support: a mixed methods study. PeerJ. 2016;4:e1671.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffman TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffman TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
Cochrane Effective Practice and Organisation of Care (EPOC). EPOC resources for review authors. What study designs should be included in an EPOC review and what should they be called? Available at: https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/what_study_designs_should_be_included_in_an_epoc_review.pdf. Accessed on: April, 2021.
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at: www.covidence.org. Accessed on: April, 2021.
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and shiny web app for visualizing risk-of-bias assessments. Research Synthesis Methods. 2020. Available at: https://www.riskofbias.info/welcome/robvis-visualization-tool. Accessed on: April 28, 2021.
Acknowledgements
We would like to thank Andrew Jones, Subject Librarian for the School of Pharmacy and Pharmaceutical Sciences, Trinity College Dublin, for assistance with the search strategy.
Author information
Authors and Affiliations
Contributions
JO’S led the execution of the report and was part of conception and data acquisition, analysis and interpretation. He drafted the article. CR and ML were part of conception and data acquisition, analysis and interpretation. CK contributed to data analysis. CR, ML and JG reviewed the article critically and substantively revised it. All the authors have agreed on the submission of the article to the Pharmacogenomics Journal. All the authors reviewed and agreed on all versions of the article before submission, and during revision, accepted the final version for publication, and any significant changes introduced at the proofing stage. All the authors agree to take responsibility and be accountable for the contents of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The legends of Figures 1, 2, 3 and 4 have been corrected.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
O’Shea, J., Ledwidge, M., Gallagher, J. et al. Pharmacogenetic interventions to improve outcomes in patients with multimorbidity or prescribed polypharmacy: a systematic review. Pharmacogenomics J 22, 89–99 (2022). https://doi.org/10.1038/s41397-021-00260-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41397-021-00260-6