Abstract
Aromatic antiepileptic drugs (AEDs)-induced cutaneous adverse drug reactions (cADRs) add up to the limited use of the AEDs in the treatment and prevention of seizures. Human leukocyte antigen-B (HLA-B) alleles have been linked to AEDs-induced cADRs. We investigated the association between cADRs (including Stevens–Johnson syndrome; SJS/toxic epidermal necrolysis; TEN, drug reaction with eosinophilia and systemic symptoms; DRESS, and Maculopapular eruption; MPE) caused by AEDs (phenytoin, carbamazepine, lamotrigine, phenobarbital and oxcarbazepine) and HLA-B alleles in Thai population. Through the case-control study, 166 patients with AEDs-induced cADRs, 426 AEDs-tolerant patients (AEDs-tolerant controls), and 470 healthy subjects (Thai population) were collected. The HLA genotypes were detected using the polymerase chain reaction-sequence specific oligonucleotide probe (PCR-SSOP) method. We also performed a meta-analysis with these data and other populations. The carrier rate of HLA-B*15:02 was significantly different between AEDs-induced cADRs group and AEDs-tolerant group (Odds ratio; OR 4.28, 95% Confidence interval; CI 2.64–6.95, p < 0.001), AEDs-induced cADRs group and Thai population (OR 2.15, 95%CI 1.41–3.29, p < 0.001). In meta-analysis showed the strong association HLA-B*15:02 with AEDs-induced cADRs (OR 4.77, 95%CI 1.79–12.73, p < 0.001). Furthermore, HLA-B*15:02 was associated with SJS/TEN induced by AEDs (OR 10.28, 95%CI 6.50–16.28, p < 0.001) Phenytoin (OR 4.12, 95%CI 1.77–9.59, p = 0.001) and carbamazepine (OR 137.69, 95%CI 50.97–371.98, p < 0.001). This study demonstrated that genetic association for AEDs-induced cADRs was phenotype-specific. A strong association between HLA-B*15:02 and AEDs-induced SJS/TEN was demonstrated with an OR of 10.79 (95%CI 5.50–21.16, p < 0.001) when compared with AEDs-tolerant group. On the other hand, the carrier rates of HLA-B*08:01, HLA-B*13:01, and HLA-B*56:02 were significantly higher in the DRESS group compared with the AEDs-tolerant group (p = 0.029, 0.007, and 0.017, respectively). The HLA-B*15:02 allele may represent a risk factor for AEDs-induced cADRs.
Similar content being viewed by others
Introduction
Aromatic antiepileptic drugs (AEDs), such as phenytoin (PHT), carbamazepine (CBZ), lamotrigine (LTG), phenobarbital (PB), and oxcarbazepine (OXC), commonly prescribed to prevent or treat seizure, are frequently associated with cutaneous adverse drug reactions (cADRs) [1]. The overall incidence of cADRs induced by AEDs is ~10% [2]. cADRs can be classified into two types, immediate and delayed type. cADRs associated with AEDs are usually delayed type, and clinical manifestations include from mild maculopapular eruption (MPE) to severe and life-threatening severe cutaneous adverse reactions (SCARs); Stevens–Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and hypersensitivity syndrome (HSS)/drug-induced hypersensitivity syndrome (DIHS)/drug reaction with eosinophilia and systemic symptoms (DRESS) [3].
MPE, the mild delayed type cADRs, presents as a widespread, symmetrically distributed rash composed of pink-to-red macules and papules that may coalesce to form plaques. Redness of skin without blister, pruritus and low-grade fever may occur in MPE, but does not involve the internal organs [4]. SJS and TEN are severe life-threatening delayed type cADRs characterized by febrile illness in acute phases followed by the predominant involvement of skin and mucous membrane necrosis and systemic symptoms. The degree of skin detachment expressed in terms of the % body surface area affected classifies the SJS and TEN into 3 types: <10% body surface area is affected in SJS, 10–30% body surface area is affected in SJS-TEN overlap, and >30% body surface area is affected in TEN [5]. DRESS has a wide range of clinical characteristics, such as cutaneous eruption, fever, lymphadenopathy, hepatitis, and hematologic abnormalities with eosinophilia and atypical lymphocytes [6]. Severe cADRs has a crucial burden on healthcare system with the mortality rates reaching up to 40% [7]. Alleles of the human leukocyte antigen (HLA) genes have been associated with cADRs, and the screening of HLA alleles prior to the administration of AEDs can prevent the occurrence of cADRs.
The HLA-B genotype is a crucial immunological risk factor for cADRs. In 2004, Chung et al. reported a strong association between the HLA-B*15:02 allele and CBZ-induced SJS/TEN in Han Chinese [8]. In 2013, a systematic review and meta-analysis in Thai and Malaysian populations validated the association between the HLA-B*15:02 allele and CBZ-induced SJS/TEN [9]. In Thai population, the HLA-B*15:02 allele has a frequency of 8.16% which is higher when compared to other ethnicities: 4.87% in Asians, 2% in African-American, and rarely observed in East Asian populations (Japanese and Korean), Caucasian, and Hispanic/North Americans [10, 11]. The aim of this study was to extend the investigation of HLA-B susceptibility to AEDs-induced cADRs in Thai patients.
Materials and methods
Subjects and characteristics
We recruited cases between 2011 and 2017 with AEDs-induced cADRs. The enrolled cases of 166 patients with AEDs-induced cADRs included 71 with MPE, 49 with DRESS, and 46 with SJS/TEN. Patients tolerated to various AEDs (AEDs-tolerant controls; n = 426) for at least 6 months without evidence of cutaneous adverse effects were also recruited in this study. Healthy subjects (Thai population; n = 470) who did not take AEDs were included for analysis. All individuals enrolled were unrelated Thai population. This study was approved by the Ramathibodi Hospital Ethical Review Board for Human Research. Written informed consent was obtained from all the participants.
Diagnosis of AEDs-induced cADRs
All patients were diagnosed and confirmed based on the photographs, pathological slides, clinical morphology, and medical records by a dermatologist and allergist. MPE was diagnosed as a macular and papular rash without skin detachment or organ involvement. The RegiSCAR criteria were used to diagnose and classify SCARs [12]. DRESS was characterized by acute skin rash, fever above 38 °C, facial edema, enlarged lymph nodes, internal organ involvement (e.g., liver, kidney and lung), and hematological abnormalities, including lymphocytosis or lymphocytopenia, eosinophilia, and thrombocytopenia [12]. SJS was defined as skin detachment of <10% of the body surface area. TEN was defined as skin detachment >30%. The SJS-TEN overlap was defined as skin detachment of 10% to 30% [3]. In some cases, in vitro assay (such as ELISpot) was performed.
DNA extraction, HLA-A, HLA-B and CYP2C9*3 genotyping
Blood samples were collected into EDTA tubes. Genomic DNA was extracted by the MagNA Pure automated compact machine (Roche Diagnostics, USA). The purity and concentration of genomic DNA were detected using the Nanodrop ND-1000 ultraviolet spectrophotometer. DNA was stored at −20 °C before analysis.
HLA-A and HLA-B genotyping was performed using the polymerase chain reaction-sequence specific oligonucleotide probe (PCR-SSOP) method combined with Luminex™ Multiplex technology. Data analysis for the HLA-A and HLA-B assays was performed with software package HLA fusion 2.0.
TaqMan® SNP Genotyping Assays of CYP2C9*3 (1075A > C, rs1057910) were performed on the ViiA™ 7 real time-PCR System (Applied Biosystems, Foster City, California), according to the manufacturer’s instructions.
Statistical analysis
Statistical analyses were performed using SPSS version 16.0. Means and standard deviations (SD) were calculated for all continuous data. Comparison of continuous variables among clinical characteristics between cases and controls were analyzed using the t-test. Chi-square test or Fisher’s exact test was used for the comparison of HLA-A, HLA-B and CYP2C9 allele frequency in each group. Odds ratio (OR) and 95% confidence interval (CI) values were obtained. Bonferroni correction was applied to adjust for multiple comparisons (P < 0.0025) to indicate statistically significant association. For the meta-analysis, we used “metan” command of STATA program for pooling effect-size (StataCorp LLC. College Station, TX).
Results
Cases and controls study
Pharmacogenetic study was performed in 166 patients who had AEDs-induced cADRs, 426 AEDs-tolerant controls and 470 Thai population. Table 1 shows different types of cADRs and their causative AEDs including PHT (103; 62.04%), CBZ (38; 22.89%), LTG (15; 9.03%), PB (7; 4.21%) and OXC (3; 1.30%). Overall, 166 cases of AEDs-induced cADRs were 71 MPE, 46 SJS/TEN and 49 DRESS cases. Among 71 AEDs-induced MPE, we found 41(57.74%), 16(22.53%), 11(15.49%) and 3(4.22%) cases received PHT, CBZ, LTG and PB, respectively. In a group of SJS/TEN, 46 cases were related with PHT (22; 47.82%), CBZ (17; 36.95%), LTG (3; 6.52%), PB (1; 2.17%) and OXC (3; 6.52%). In a group of DRESS, the most common culprit drugs were PHT (40; 81.63%).
Of the AEDs tolerant controls, 105 (24.65%) patients received PHT, 271 (63.61%) patients received CBZ, and 50 (11.73%) patients received LTG. None of the AEDs tolerant controls received PB or OXC.
Association of HLA-B alleles with AEDs-induced cADRs
The association between HLA-B alleles and AEDs-induced cADRs was evaluated by comparing the AEDs-induced cADRs group (n = 166) with the AEDs-tolerant controls group (n = 426) and the Thai population (n = 470). The HLA-B genotypes of cADRs cases induced by AEDs are shown in Table 2. We found that 46 patients of 166 cADRs cases (27.7%) carried the HLA-B*15:02 allele, while only 35 (8.21%) of AEDs-tolerant group and 71 (15.1%) of the 470 Thai population carried this allele. HLA-B*15:02 allele was statistically significant in the AEDs-induced cADRs, with respect to the AEDs tolerant group (OR 4.282, 95%CI: 2.637–6.954; p < 0.001) and the Thai population (OR 2.154, 95%CI: 1.411–3.290; p < 0.001). Furthermore, 21 patients (12.6%) AEDs-induced cADRs group were positive for HLA-B*51:01, while only 29 (6.8%) of AEDs-tolerant controls group carried this allele (OR 2.292, 95%CI: 1.311–4.007; p = 0.003). However, the significant associations the HLA-B*51:01 alleles disappeared after correction for multiple testing (P < 0.0025). Remarkably, the HLA-B*13:01 allele was present in 4 (100%) patients with PB-induced SCARs.
Association of HLA-B*15:02 allele in each AEDs-drug with tolerant control
The HLA-B*15:02 allele of cADRs cases per drug is shown in Table 3. The HLA-B*15:02 frequency was statistically significant in the CBZ-induced cADRs (17 carriers of 38 cases, 44.73%) (OR 19.134, 95%CI: 7.943–46.091; p < 0.001) and in the LTG-induced cADRs (6 carriers of 15 cases, 40.00%) (OR 4.889, 95%CI: 1.281–18.664; p = 0.024) with respect to the AEDs-tolerant group. The frequency of HLA-B*15:02 allele was not significantly higher in the cases of PHT-induced cADRs compared with the tolerant controls (p = 0.671). One patient (14.28%) of PB- and two patients (66.67%) of OXC-induced cADRs group was a carrier of HLA-B*15:02 allele.
Association between HLA-B alleles and AEDs-induced MPE
We compared the HLA-B alleles frequency of 71 AEDs-induced MPE with 426 tolerant controls, and 470 healthy controls; the results are summarized in Table 4. The carrier rate of the HLA-B*15:02 allele was higher in the MPE group than in the controls. We found that 19 of the 71 MPE cases (26.8%) carried the HLA-B*15:02 allele, while only 8.2% of the AEDs-tolerant group (OR 4.301, 95%CI: 2.294–8.064; p < 0.001) and 15.1% of the healthy subjects carried the allele.
Association between HLA-B alleles and AEDs-induced SJS/TEN
We compared the HLA-B alleles frequency of 46 AEDs-induced SJS/TEN with 426 tolerant controls, and 470 healthy controls; the results are summarized in Table 5. The carrier rate of the HLA-B*15:02 allele was higher in the SJS/TEN group and reached a statistical significance compared to the tolerant controls (OR 10.790, 95%CI: 5.502–21.163; p < 0.001) and healthy subjects (OR 5.151, 95%CI: 2.740–9.684; p < 0.001). Moreover, HLA-B*15:21 allele showed significant association between AEDs-induced SJS/TEN and general Thai population (2/46 (4.3%) vs 2/470 (0.42%), OR 10.636, 95%CI: 1.462–77.359; p < 0.042), while the association between HLA-B*15:21 allele and AEDs-tolerant controls did not reach statistical significance (p = 0.214).
Association between HLA-B alleles and AEDs-induced DRESS
We compared the HLA-B alleles frequency of 49 AEDs-induced DRESS with 426 tolerant controls, and 470 healthy controls; the results are summarized in Table 6. The carrier rates of HLA-B*08:01, HLA-B*13:01, and HLA-B*56:02 were higher in the DRESS group than in the tolerant group. The carrier rates of these alleles between the two groups reached statistical significance (p = 0.029, 0.007, and 0.017, respectively). The carrier rate of HLA-B*08:01 allele was not found to be significantly higher in the DRESS cases as compared to the healthy subjects (p = 0.052). The carrier rates for HLA-B*13:01 and HLA-B*56:02 alleles were statistically higher in the DRESS group compared to the healthy population (p = 0.010 and 0.002, respectively). However, the significant associations these alleles disappeared after correction for Bonferroni correction (P < 0.0025).
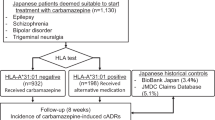
Association between HLA-A and CBZ-induced DRESS and MPE
To clarify the relationship between HLA-A*31:01 and CBZ-induced DRESS and MPE, the HLA-A was genotyped in this study. Then, we compared the frequency of HLA-A alleles between the 5 CBZ-induced DRESS or 16 CBZ-induced MPE patients and the 470 normal Thai subjects. The HLA-A*31:01 allele, which was previously reported to be associated with CBZ-induced DRESS and MPE, was not found in our study. Conversely, 3 of 5 (60.00%) CBZ-induced DRESS and 6 of 16 (37.5%) CBZ-induced MPE patients were HLA-A*33:03 carriers. However, there was no significant difference of HLA-A*33:03 between patients with CBZ-induced DRESS (p = 0.0605) and CBZ-induced MPE (p = 0.1253) and normal Thai subjects (99/470; 21.06%) in our study.
Association between CYP2C9*3 and PHT
To date there have been relatively few studies confirming the CYP2C9*3 risk association and PHT-induced SCARs. In this study we genotyped the CYP2C9*3 in 103 PHT-induced cADRs cases. The carrier rate of the CYP2C9*3 in this study was higher in the cADRs (12/103; 11.65%), which were 22.73% of SJS/TEN (5/22), 12.50% of DRESS (5/40) and 4.89% of MPE (2/41) group than in the tolerant control group (6/105; 5.71%). There was no difference in the frequency of subjects with the CYP2C9*3 between the cADRs and tolerant control group (OR 1.79; 95%CI 0.6116–5.2339, p = 0.2881). Nevertheless, there was also a trend toward an association between PHT-induced SJS/TEN and CYP2C9*3, compared to the tolerant control group (OR 3.88; 95%CI 0.9907–15.2146, p = 0.0516). Moreover, no significant differences in CYP2C9*3 frequency were found between the PHT-induced DRESS (OR 1.88; 95%CI 0.5024–7.0773, p = 0.3472) and PHT-induced MPE (OR 0.53; 95%CI 0.0617–4.5929, p = 0.5663), when compared with tolerant control group.
Meta-analysis: HLA-B*15:02 and AEDs-induced cADRs
The forest plots are shown in Fig. 1. Previous case-control studies on the association between HLA-B*15:02 and AEDs-induced cADRs were recruited in meta-analysis. We found that the association between the HLA-B*15:02 allele and AEDs-induced cADRs was statistically significant (OR 4.77, 95%CI 1.79–12.73, p < 0.001). After analyzed each AEDs separately, we found that the statistical significance of association between HLA-B*15:02 and CBZ-induced cADRs (OR 19.13, 95%CI7.94–46.09, p < 0.001), and HLA-B*15:02 and LTG-induced cADRs (OR 4.89, 95%CI 1.28–18.66, p = 0.020). But no statistical significance was found in PHT.
For SJS/TEN outcome, we found that individuals using AEDs and carrying HLA-B*15:02 allele increase of SJS/TEN by 17.74 folds compare with tolerance control group (OR 17.74, 95%CI 8.48–37.13, p < 0.001). We analyzed each AEDs separately and found the association of HLA-B*15:02 and PHT-induced SJS/TEN (OR 3.60, 95%CI 1.59–8.15, p = 0.001), and HLA-B*15:02 and CBZ-induced SJS/TEN (OR 141.89, 95%CI 48.14–419.19, p < 0.001).
We also found that the association between the HLA-B*15:02 allele and AEDs-induced MPE was statistically significant (OR 3.51, 95%CI 2.22–5.54, p < 0.001).
Discussion
AEDs are effective for controlling seizures. Several studies have reported about the CBZ-induced SJS/TEN in Asian ancestry, including Han Chinese, Indian, Thai, Vietnamese and Malaysian [8, 13,14,15,16,17]. The HLA-B*15:02 allele was reported to have been associated with PHT-induced SJS/TEN, LTG-induced SJS/TEN, OXC-induced SJS/TEN. Because of the sample size limitation, association of the HLA-B*15:02 allele with these AEDs-induced cADRs is unclear and needs to be further investigated. The US-FDA has recommended the testing for HLA-B*15:02 in patients of Asian and HLA-A*31:01 in patients of European, Korean and Japanese ancestry prior to CBZ treatment due to the risk of developing SCARs [18]. Physicians avoid using all types of AEDs when the patient is HLA-B*15:02 or HLA-A*31:01 positive. Thus, we aim to investigate the association between HLA-A, HLA-B alleles and CYP2C9*3 genotype and AEDs-induced cADRs. We also performed a meta-analysis with these data and other populations.
In this study, we recruited cases of AEDs-induced cADRs (n = 166) and performed HLA-B allele association to find a genetic marker to screen the patients before initiating the AEDs treatment. The carrier rate of the HLA-B*15:02 and HLA-B*51:01 alleles was significantly higher in the AEDs-induced cADRs cases than the tolerant control group. HLA-B*15:02 carriers were found in 44.73% (17/38) and 40.00% (6/15) cases of CBZ and LTG-treated patients. It bears noting that the HLA-B*15:02 allele frequency was higher (66.67%) in OXC-induced cADRs, although the patient samples were too small to draw any definitive conclusions. However, there is evidence in the literature of the involvement of the HLA-B*15:02 allele in the OXC-induced SJS/TEN in populations in the Taiwan and Thailand [20]. Moreover, our data also support the Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for HLA genotype and use of CBZ and OXC [21].
In the present study, we support the hypothesis that multiple HLA alleles might be involved in AEDs-induced cADRs. Interestingly, HLA-B*51:01 was also found significantly associated with AEDs-induced cADRs with OR 2.292, but when we separated the data in each drug category, we found that HLA-B*51:01 was significantly associated with PHT-induced STS/TEN and CBZ-induced DRESS compared to tolerant controls with OR of 6.19 and 7.94, respectively. SJS/TEN caused by PHT and PB was significantly associated with the HLA-B*51:01 allele in the Japanese population [22]. Moreover, the carrier rate of HLA-B*13:01 in the PB-induced SCARs was 100% (n = 4). This study first demonstrated the association between HLA-B*13:01 and PB-induced SCARs in Thai adults [23]. Further, we corroborated the findings of Li et al. where patients carrying the HLA-B*58:01 allele were associated with CBZ-induced MPE [24]. We identified significant associations between CBZ-induced MPE and the HLA-B*58:01 allele, compared with CBZ-tolerant: OR 5.15, 95%CI: 1.64–16.14; p = 0.011 and compared with healthy subjects: OR 3.29, 95%CI: 1.10–9.82; p = 0.041(Data not shown).
In addition, the HLA-B*15:02 allele has been reported to be specifically associated with CBZ-induced SJS/TEN in Asian populations, and no associations have been reported for drug-induced MPE and DRESS [2, 8, 16, 25, 26]. In this study, we found significant associations between HLA-B*15:02 and AEDs-induced MPE and SJS/TEN, however, this significance was not observed in DRESS cases [27]. Interestingly, previous studies reported no associations between the HLA- B*15:02 allele and the AEDs-induced MPE [14, 28, 29]. We believe that further studies need to be conducted to explore the molecular mechanism explaining the linkage between the HLA-B*15:02 allele and MPE. In the SJS/TEN group, we identified the HLA-B*15:21 allele associated with AEDs-induced SJS/TEN (compared with healthy population: OR 10.636, 95%CI: 1.462–77.359, p = 0.042). The HLA-B*15:21 allele belongs to the group of HLA-B75 serotype which consists of HLA-B*15:02, HLA-B*15:08, HLA-B*15:11, and HLA-B*15:21. As evident with the previous findings, the HLA-B*15:02 allele was the genetic risk factor for an AEDs-induced SJS/TEN in our study. Interestingly, the HLA-B*15:11 allele, another member of the HLA-B75 serotype, was found in SJS/TEN cases due to CBZ [25, 30,31,32,33,34]. These findings suggest that HLA-B75 serotype might have a role in AEDs-induced SJS/TEN, suggesting the need for screening of other alleles of the HLA-B75 serotype in case of HLA-B*15:02 negative screening. In DRESS group, although we found positive correlations between AEDs-induced DRESS and HLA-B*08:01, HLA-B*13:01, and HLA-B*56:02 alleles. If Bonferroni correction was performed for multiple comparisons, the significance of these alleles would be lost.
In the PHT group, we found similar frequency of the HLA-B*15:02 allele between the cases and the controls (19.40% vs 17.10%). This result suggests that the patient carrying HLA-B*15:02 allele is not at risk of PHT-induced cADRs, this finding contradicts that of Dean L., who recommended avoiding PHT as an alternative for CBZ in patients positive for HLA-B*15:02 [19]. In addition to PHT, we further genotyped the CYP2C9*3 variants in 92 cases of PHT-induced cADRs and found that only 9 patients showed CYP2C9 variation (4 SJS/TEN, 4 DRESS, and 1 MPE). No signification between CYP2C9*3 and PHT-induced cADRs. There was a trend that the carrier rates of CYP2C9*3 were higher in the PHT-induced SJS/TEN group than in the tolerant control group in this study. However, previous studies demonstrated that CYP2C9*3 and having Chinese ancestry were significant risk factors of PHT-induced SJS (adjusted OR = 5.40, p = 0.0097). [35,36,37,38].
HLA-A* 31:01 also showed to increase the risk of MPE and DRESS due to CBZ in European and Han-Chinese population [21]. Therefore, we analyzed the HLA-A in patients with CBZ-induced DRESS (n = 5) and CBZ-induced MPE (n = 16). Surprisingly, HLA-A*31:01 was not found in the patients with DRESS and MPE groups, suggesting that the HLA-A*31:01 allele could not be associated in the development of CBZ induced MPE and DRESS in Thai population. However, there was a trend that carriers rate of HLA-A*33:03 were higher in the MPE and DRESS groups than in the tolerant group. HLA-A*33:03 allele was detected in 60.00% of CBZ-induced DRESS (3/5) and 37.5% of CBZ-induced MPE (6/16). The HLA-A*31:01 is very low frequency (allele frequency=0.0085) but HLA-A*33:03 is the most common HLA-A alleles in Thai (allele frequency = 0.1117) [39]. In addition, a previous sequence analysis showed that HLA-A*31:01 and HLA-A*33:03 binding peptides have the same anchor residues at P2 and the C-terminus, the only difference being that HLA-A*33:03 binding peptides have two additional P2 anchor residues [40].
Finally, the meta-analysis was performed to clarify the relationship between HLA-B*15:02 and cADRs. There was a significant association between HLA-B*15:02 and AEDs-induced cADRs, and AEDs-induced SJS/TEN. while the association between HLA-B*15:02 and AEDs-induced DRESS did not reach statistical significance.
In conclusion, we found the association between HLA-B*15:02 and AEDs-induced cADRs. We also revealed an ambiguous association between the HLA-B*15:02 and the AEDs. Our results suggest that HLA-B*15:02 is not a risk allele for the cross-reactivity of AEDs-induced cADRs. We did not find any significant association between HLA-B*15:02 and PHT and PB-induced cADRs. If a patient has a positive HLA-B*15:02 genotype, a prescription for OXC needs to be carefully considered.
References
Perucca P, Gilliam FG. Adverse effects of antiepileptic drugs. Lancet Neurol. 2012;11:792–802.
Chung WH, Hung SI, Chen YT. Genetic predisposition of life-threatening antiepileptic-induced skin reactions. Expert Opin Drug Saf. 2010;9:15–21.
Roujeau J-C. Clinical heterogeneity of drug hypersensitivity. Toxicology. 2005;209:123–9.
Stern RS. Exanthematous drug eruptions. N Engl J Med. 2012;366:2492–501.
Harr T, French LE. Stevens–Johnson syndrome and toxic epidermal necrolysis. Chem Immunol Allergy. 2012;97:149–66.
Criado PR, Criado RF, Avancini JM, Santi CG. Drug reaction with eosinophilia and systemic symptoms (DRESS)/drug-induced hypersensitivity syndrome (DIHS): a review of current concepts. Bras Dermatol. 2012;87:435–49.
Kohanim S, Palioura S, Saeed HN, Akpek EK, Amescua G, Basu S, et al. Stevens–Johnson syndrome/toxic epidermal necrolysis—a comprehensive review and guide to therapy. I. Systemic disease. Ocul Surf. 2016;14:2–19.
Chung WH, Hung SI, Hong HS, Hsih MS, Yang LC, Ho HC, et al. Medical genetics: a marker for Stevens–Johnson syndrome. Nature. 2004;428:486.
Tangamornsuksan W, Chaiyakunapruk N, Somkrua R, Lohitnavy M, Tassaneeyakul W. Relationship between the HLA-B*1502 allele and carbamazepine-induced Stevens–Johnson syndrome and toxic epidermal necrolysis: a systematic review and meta-analysis. JAMA Dermatol. 2013;149:1025–32.
Puangpetch A, Koomdee N, Chamnanphol M, Jantararoungtong T, Santon S, Prommas S, et al. HLA-B allele and haplotype diversity among Thai patients identified by PCR-SSOP: evidence for high risk of drug-induced hypersensitivity. Front Genet. 2014;5:478.
Cao K, Hollenbach J, Shi X, Shi W, Chopek M, Fernandez-Vina MA. Analysis of the frequencies of HLA-A, B, and C alleles and haplotypes in the five major ethnic groups of the United States reveals high levels of diversity in these loci and contrasting distribution patterns in these populations. Hum Immunol. 2001;62:1009–30.
Kardaun SH, Sekula P, Valeyrie-Allanore L, Liss Y, Chu CY, Creamer D, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Br J Dermatol. 2013;169:1071–80.
Hung SI, Chung WH, Liu ZS, Chen CH, Hsih MS, Hui RC, et al. Common risk allele in aromatic antiepileptic-drug induced Stevens–Johnson syndrome and toxic epidermal necrolysis in Han Chinese. Pharmacogenomics. 2010;11:349–56.
Locharernkul C, Loplumlert J, Limotai C, Korkij W, Desudchit T, Tongkobpetch S, et al. Carbamazepine and phenytoin induced Stevens-Johnson syndrome is associated with HLA-B*1502 allele in Thai population. Epilepsia. 2008;49:2087–91.
Nguyen DV, Chu HC, Nguyen DV, Phan MH, Craig T, Baumgart K, et al. HLA-B*1502 and carbamazepine-induced severe cutaneous adverse drug reactions in Vietnamese. Asia Pac Allergy. 2015;5:68–77.
Chang CC, Ng CC, Too CL, Choon SE, Lee CK, Chung WH, et al. Association of HLA-B*15:13 and HLA-B*15:02 with phenytoin-induced severe cutaneous adverse reactions in a Malay population. Pharmacogenom J. 2017;17:170–3.
Mehta TY, Prajapati LM, Mittal B, Joshi CG, Sheth JJ, Patel DB, et al. Association of HLA-B*1502 allele and carbamazepine-induced Stevens–Johnson syndrome among Indians. Indian J Dermatol Venereol Leprol. 2009;75:579–82.
Ferrell PB, McLeod HL. Carbamazepine, HLA-B*1502 and risk of Stevens–Johnson syndrome and toxic epidermal necrolysis: US FDA recommendations. Pharmacogenomics. 2008;9:1543–6.
Dean L Phenytoin Therapy and HLA-B*15:02 and CYP2C9 Genotypes. 2016;
Chen CB, Hsiao YH, Wu T, Hsih MS, Tassaneeyakul W, Jorns TP, et al. Risk and association of HLA with oxcarbazepine-induced cutaneous adverse reactions in Asians. Neurology. 2017;88:78–86.
Phillips EJ, Sukasem C, Whirl-Carrillo M, Müller DJ, Dunnenberger HM, Chantratita W, et al. Clinical pharmacogenetics implementation consortium guideline for HLA genotype and use of carbamazepine and oxcarbazepine: 2017 update. Clin Pharm Ther. 2018;103:574–58.
Kaniwa N, Sugiyama E, Saito Y, Kurose K, Maekawa K, Hasegawa R, et al. Specific HLA types are associated with antiepileptic drug-induced Stevens–Johnson syndrome and toxic epidermal necrolysis in Japanese subjects. Pharmacogenomics. 2013;14:1821–31.
Manuyakorn W, Mahasirimongkol S, Likkasittipan P, Kamchaisatian W, Wattanapokayakit S, Inunchot W, et al. Association of HLA genotypes with phenobarbital hypersensitivity in children. Epilepsia 2016;57:1610–6.
Li LJ, Hu FY, Wu XT, An DM, Yan B, Zhou D. Predictive markers for carbamazepine and lamotrigine-induced maculopapular exanthema in Han Chinese. Epilepsy Res. 2013;106:296–300.
Sun D, Yu CH, Liu ZS, He XL, Hu JS, Wu GF, et al. Association of HLA-B*1502 and *1511 allele with antiepileptic drug-induced Stevens–Johnson syndrome in central China. J Huazhong Univ Sci Technol Med Sci. 2014;34:146–50.
Zhang Y, Wang J, Zhao LM, Peng W, Shen GQ, Xue L, et al. Strong association between HLA-B*1502 and carbamazepine-induced Stevens-Johnson syndrome and toxic epidermal necrolysis in mainland Han Chinese patients. Eur J Clin Pharm. 2011;67:885–7.
Sukasem C, Chaichan C, Nakkrut T, Satapornpong P, Jaruthamsophon K, Jantararoungtong T, et al. Association between HLA-B alleles and carbamazepine-induced maculopapular exanthema and severe cutaneous reactions in Thai patients. J Immunol Res. 2018;10:2780272.
Hung SI, Chung WH, Jee SH, Chen WC, Chang YT, Lee WR, et al. Genetic susceptibility to carbamazepine-induced cutaneous adverse drug reactions. Pharmacogenet Genom. 2006;16:297–306. 27
Man CB, Kwan P, Baum L, Yu E, Lau KM, Cheng AS, et al. Association between HLA-B*1502 allele and antiepileptic drug-induced cutaneous reactions in Han Chinese. Epilepsia. 2007;48:1015–8. 28
Kaniwa N, Saito Y, Aihara M, Matsunaga K, Tohkin M, Kurose K, et al. HLA-B*1511 is a risk factor for carbamazepine-induced Stevens–Johnson syndrome and toxic epidermal necrolysis in Japanese patients. Epilepsia. 2010;51:2461–5.
Kim SH, Lee KW, Song WJ, Kim SH, Jee YK, Lee SM, et al. Carbamazepine-induced severe cutaneous adverse reactions and HLA genotypes in Koreans. Epilepsy Res. 2011;97:190–7.
Jaruthamsophon K, Tipmanee V, Sangiemchoey A, Sukasem C, Limprasert P. HLA-B*15:21 and carbamazepine-induced Stevens–Johnson syndrome: pooled-data and in silico analysis. Sci Rep. 2017;7:45553.
Yuliwulandari R, Kristin E, Prayuni K, Sachrowardi Q, Suyatna FD, Menaldi SL, et al. Association of the HLA-B alleles with carbamazepine-induced Stevens-Johnson syndrome/toxic epidermal necrolysis in the Javanese and Sundanese population of Indonesia: the important role of the HLA-B75 serotype. Pharmacogenomics 2017;18:1643–8.
Capule F, Tragulpiankit P, Mahasirimongkol S, Jittikoon J, Wichukchinda N, Theresa Alentajan-Aleta L, et al. Association of carbamazepine-induced Stevens–Johnson syndrome/toxic epidermal necrolysis with the HLA-B75 serotype or HLA-B*15:21 allele in Filipino patients. Pharmacogenom J. 2020;20:533–41.
Yampayon K, Sukasem C, Limwongse C, Chinvarun Y, Tempark T, Rerkpattanapipat T, et al. Influence of genetic and non-genetic factors on phenytoin-induced severe cutaneous adverse drug reactions. Eur J Clin Pharm. 2017;73:855–65.
Tassaneeyakul W, Prabmeechai N, Sukasem C, Kongpan T, Konyoung P, Chumworathayi P, et al. Associations between HLA class I and cytochrome P450 2C9 genetic polymorphisms and phenytoin-related severe cutaneous adverse reactions in a Thai population. Pharmacogenet Genom. 2016;26:225–34.
Sukasem C, Sririttha S, Tempark T, Klaewsongkram J, Rerkpattanapipat T, Puangpetch A, et al. Genetic and clinical risk factors associated with phenytoin-induced cutaneous adverse drug reactions in Thai population. Pharmacoepidemiol Drug Saf. 2020;29:565–74.
Su SC, Chen CB, Chang WC, Wang CW, Fan WL, Lu LY, et al. HLA alleles and CYP2C9*3 as predictors of phenytoin hypersensitivity in East Asians. Clin Pharm Ther. 2019;105:476–85.
Satapornpong P, Jinda P, Jantararoungtong T, Koomdee N, Chaichan C, Pratoomwun J, et al. Genetic diversity of HLA class I and class II alleles in thai populations: contribution to genotype-guided therapeutics. Front Pharm. 2020;11:78.
Takiguchi M, Matsuda T, Tomiyama H, Miwa K. Analysis of three HLA-A*3303 binding peptide anchors using an HLA-A*3303 stabilization assay. Tissue Antigens 2000;55:296–302.
Acknowledgements
This study was supported by grants from the (1) Faculty of Medicine, Ramathibodi Hospital, Mahidol University (2) the Health System Research Institute under Genomics Thailand Strategic Fund, (3) The Skin and Allergy Research Unit, Chulalongkorn University, and (4) The International Research Network-The Thailand Research Fund (IRN60W003). The authors thank the study participants and staffs of Pharmacogenomic and Personalized Medicine of Ramathibodi Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with ethical standards
The studies involving human participants were reviewed and approved by the ethics committee of Ramathibodi Hospital.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sukasem, C., Sririttha, S., Chaichan, C. et al. Spectrum of cutaneous adverse reactions to aromatic antiepileptic drugs and human leukocyte antigen genotypes in Thai patients and meta-analysis. Pharmacogenomics J 21, 682–690 (2021). https://doi.org/10.1038/s41397-021-00247-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41397-021-00247-3
This article is cited by
-
Investigating the genetic makeup of the major histocompatibility complex (MHC) in the United Arab Emirates population through next-generation sequencing
Scientific Reports (2024)
-
Assessment of clinically actionable pharmacogenetic markers to stratify anti-seizure medications
The Pharmacogenomics Journal (2023)
-
Lamotrigine/phenobarbital
Reactions Weekly (2022)