Abstract
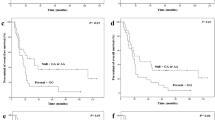
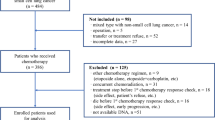
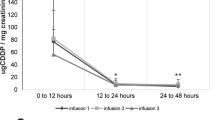
Chemotherapy based on platinum compounds is the standard treatment for NSCLC patients with EGFR wild type, and is also used as second line in mutated EGFR patients. Nevertheless, this therapy presents poor clinical outcomes. ERCC1, ERCC2, XRCC1, MDM2, MTHFR, MTR, and SLC19A1 gene polymorphisms may contribute to individual variation in response and survival to platinum-based chemotherapy. The aim of this study was to investigate the influence of these polymorphisms on response and survival of NSCLC patients treated with platinum-based chemotherapy. A retrospective–prospective cohorts study was conducted, including 141 NSCLC patients. Polymorphisms were analyzed by PCR real-time with Taqman® probes. Patients with ERCC1 rs3212986-GG (p = 0.0268; OR = 2.50; CI95% = 1.12–5.69) and XRCC1 rs25487-GG (p = 0.0161; OR = 2.99; CI95% = 1.26–7.62) genotype showed significantly better ORR. Cox survival analysis revealed that patients carrying the MDM2 rs1690924-GG genotype (p = 0.0345; HR = 1.99; CI95% = 1.05–3.80) presented higher risk of death. Furthermore, carriers of MTR rs1805087-A alleles (p = 0.0060; HR = 8.91; CI95% = 1.87–42.42) and SLC19A1 rs1051266-AA genotype (p = 0.0130; HR = 1.74; CI95% = 1.12–2.68) showed greater risk of progression. No influence of ERCC1 rs11615, ERCC2 rs13181, ERCC2 rs1799793, XRCC1 rs1799782, MDM2 rs1470383, MTHFR rs1801131, and MTHFR rs1801133 on platinum-based chemotherapy clinical outcomes was found. In conclusion, our results suggest that ERCC1 rs3212986, XRCC1 rs25487, MDM2 rs1690924, MTR rs1805087, and SLC19A1 rs1051266 gene polymorphisms may significantly act as predictive factors in NSCLC patients treated with platinum-based chemotherapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7–30.
Edge S, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Manual, 7th edn, Springer-Verlag New York, Inc.: New York, NY, USA, 2010.
Herbst RS HJ, Lippman SM. Lung cancer. N Engl J Med. 2008;359:1367–80.
Molina JR, Yang P, Cassivi SD, Schild SE, Adjei AA. Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc. 2008;83:584–94.
Ettinger DS, Wood DE, Akerley W, Bazhenova LA, Borghaei H, Camidge DR, et al. NCCN guidelines insights: non-small cell lung cancer, version 4.2016. J Natl Compr Cancer Netw. 2016;14:255–64.
Brule SY, Al-Baimani K, Jonker H, Zhang T, Nicholas G, Goss G, et al. Palliative systemic therapy for advanced non-small cell lung cancer: Investigating disparities between patients who are treated versus those who are not. Lung Cancer. 2016;97:15–21.
Zhong C, Liu H, Jiang L, Zhang W, Yao F. Chemotherapy plus best supportive care versus best supportive care in patients with non-small cell lung cancer: a meta-analysis of randomized controlled trials. PLoS ONE. 2013;8:e58466.
Blumenthal GM, Karuri SW, Zhang H, Zhang L, Khozin S, Kazandjian D, et al. Overall response rate, progression-free survival, and overall survival with targeted and standard therapies in advanced non-small-cell lung cancer: US Food and Drug Administration trial-level and patient-level analyses. J Clin Oncol. 2015;33:1008–14.
Cardenal F, Lopez-Cabrerizo MP, Anton A, Alberola V, Massuti B, Carrato A, et al. Randomized phase III study of gemcitabine-cisplatin versus etoposide-cisplatin in the treatment of locally advanced or metastatic non-small-cell lung cancer. J Clin Oncol. 1999;17:12–18.
Choi MK, Hong JY, Chang W, Kim M, Kim S, Jung HA, et al. Safety and efficacy of gemcitabine or pemetrexed in combination with a platinum in patients with non-small-cell lung cancer and prior interstitial lung disease. Cancer Chemother Pharmacol. 2014;73:1217–25.
Crino L, Weder W, van Meerbeeck J, Felip E. Early stage and locally advanced (non-metastatic) non-small-cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21(Suppl 5):103–115.
Fenchel K, Sellmann L, Dempke WC. Overall survival in non-small cell lung cancer-what is clinically meaningful? Transl Lung Cancer Res. 2016;5:115–9.
Gervais R, Robinet G, Clement-Duchene C, Denis F, El Kouri C, Martin P, et al. Pemetrexed and carboplatin, an active option in first-line treatment of elderly patients with advanced non-small cell lung cancer (NSCLC): a phase II trial. Lung Cancer. 2013;80:185–90.
Hasegawa Y, Miura D, Kitamura C, Suzuki T, Kobayashi K, Sato N. A randomized phase II trial of gemcitabine plus carboplatin: biweekly versus standard schedules in patients with advanced non-small cell lung cancer. Chemotherapy. 2013;59:346–53.
Ichiki M, Kawasaki M, Takayama K, Ninomiya K, Kuba M, Iwami F, et al. A multicenter phase II study of carboplatin and paclitaxel with a biweekly schedule in patients with advanced non-small-cell lung cancer: Kyushu thoracic oncology group trial. Cancer Chemother Pharmacol. 2006;58:368–73.
Karampeazis A, Vamvakas L, Kentepozidis N, Polyzos A, Chandrinos V, Rigas G, et al. Biweekly carboplatin plus gemcitabine as first-line treatment of elderly patients with advanced squamous non-small-cell lung cancer: a multicenter phase I-II trial by the Hellenic Oncology Research Group. Clin Lung Cancer. 2016;17:543–9.
Kim HJ, Kim TG, Lee HJ, Kim JH, Lim BH, Seo JW, et al. A phase II study of combination chemotherapy with docetaxel and carboplatin for elderly patients with advanced non-small cell lung cancer. Lung Cancer. 2010;68:248–52.
Maemondo M, Inoue A, Kobayashi K, Sugawara S, Oizumi S, Isobe H, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362:2380–8.
Schuette WH, Groschel A, Sebastian M, Andreas S, Muller T, Schneller F, et al. A randomized phase II study of pemetrexed in combination with cisplatin or carboplatin as first-line therapy for patients with locally advanced or metastatic non-small-cell lung cancer. Clin Lung Cancer. 2013;14:215–23.
Soejima K, Naoki K, Ishioka K, Nakamura M, Nakatani M, Kawada I, et al. A phase II study of biweekly paclitaxel and carboplatin in elderly patients with advanced non-small cell lung cancer. Cancer Chemother Pharmacol. 2015;75:513–9.
Takatani H, Nakamura Y, Nagashima S, Soda H, Kinoshita A, Fukuda M, et al. Phase I and II trials of vinorelbine with carboplatin for patients 75 years of age or older with previously untreated non-small-cell lung cancer. Clin Lung Cancer. 2012;13:347–51.
Belani CP, Einzig A, Bonomi P, Dobbs T, Capozzoli MJ, Earhart R, et al. Multicenter phase II trial of docetaxel and carboplatin in patients with stage IIIB and IV non-small-cell lung cancer. Ann Oncol. 2000;11:673–8.
Ozkaya S, Findik S, Atici AG, Dirica A. Cisplatin-based chemotherapy in elderly patients with advanced stage (IIIB and IV) non-small cell lung cancer patients. Neoplasma. 2011;58:348–51.
Ozkaya S, Findik S, Dirican A, Atici AG. Long-term survival rates of patients with stage IIIB and IV non-small cell lung cancer treated with cisplatin plus vinorelbine or gemcitabine. Exp Ther Med. 2012;4:1035–8.
Li T, Kung HJ, Mack PC, Gandara DR. Genotyping and genomic profiling of non-small-cell lung cancer: implications for current and future therapies. J Clin Oncol. 2013;31:1039–49.
Wei HB, Lu XS, Shang LH, Xu G, Hu J, Che DH, et al. Polymorphisms of ERCC1 C118T/C8092A and MDR1 C3435T predict outcome of platinum-based chemotherapies in advanced non-small cell lung cancer: a meta-analysis. Arch Med Res. 2011;42:412–20.
Wei SZ, Zhan P, Shi MQ, Shi Y, Qian Q, Yu LK, et al. Predictive value of ERCC1 and XPD polymorphism in patients with advanced non-small cell lung cancer receiving platinum-based chemotherapy: a systematic review and meta-analysis. Med Oncol. 2011;28:315–21.
Yang Y, Xian L. The association between the ERCC1/2 polymorphisms and the clinical outcomes of the platinum-based chemotherapy in non-small cell lung cancer (NSCLC): a systematic review and meta-analysis. Tumour Biol. 2014;35:2905–21.
Huang SJ, Wang YF, Jin ZY, Sun JY, Guo ZL. Role of ERCC1 variants in response to chemotherapy and clinical outcome of advanced non-small cell lung cancer. Tumour Biol. 2014;35:4023–9.
Li L, Wan C, Wen FQ. Polymorphisms in the XRCC1 gene are associated with treatment response to platinum chemotherapy in advanced non-small cell lung cancer patients based on meta-analysis. Genet Mol Res. 2014;13:3772–86.
Shen XY, Lu FZ, Wu Y, Zhao LT, Lin ZF. XRCC3 Thr241Met polymorphism and clinical outcomes of NSCLC patients receiving platinum-based chemotherapy: a systematic review and meta-analysis. PLoS ONE. 2013;8:e69553.
Shiraishi K, Kohno T, Tanai C, Goto Y, Kuchiba A, Yamamoto S, et al. Association of DNA repair gene polymorphisms with response to platinum-based doublet chemotherapy in patients with non-small-cell lung cancer. J Clin Oncol. 2010;28:4945–52.
Qian J, Liu H, Gu S, Wu Q, Zhao X, Wu W, et al. Genetic variants of the MDM2 gene are predictive of treatment-related toxicities and overall survival in patients with advanced NSCLC. Clin Lung Cancer. 2015;16:e37–53.
Zhu N, Gong Y, He J, Xia J, Chen X. Influence of methylenetetrahydrofolate reductase C677T polymorphism on the risk of lung cancer and the clinical response to platinum-based chemotherapy for advanced non-small cell lung cancer: an updated meta-analysis. Yonsei Med J. 2013;54:1384–93.
Cui LH, Zhang TT, Shin MH, Kim HN, Choi JS. Influence of polymorphisms in MTHFR 677 C→T, TYMS 3R→2R and MTR 2756 A→G on NSCLC risk and response to platinum-based chemotherapy in advanced NSCLC. Pharmacogenomics. 2011;12:797–808.
Matakidou A, El Galta R, Rudd MF, Webb EL, Bridle H, Eisen T, et al. Prognostic significance of folate metabolism polymorphisms for lung cancer. Br J Cancer. 2007;97:247–52.
Li WJ, Jiang H, Fang XJ, Ye HL, Liu MH, Liu YW, et al. Polymorphisms in thymidylate synthase and reduced folate carrier () genes predict survival outcome in advanced non-small cell lung cancer patients treated with pemetrexed-based chemotherapy. Oncol Lett. 2013;5:1165–70.
Tiseo M, Giovannetti E, Tibaldi C, Camerini A, Di Costanzo F, Barbieri F, et al. Pharmacogenetic study of patients with advanced non-small cell lung cancer (NSCLC) treated with second-line pemetrexed or pemetrexed-carboplatin. Lung Cancer. 2012;78:92–99.
Corrigan A, Walker JL, Wickramasinghe S, Hernandez MA, Newhouse SJ, Folarin AA, et al. Pharmacogenetics of pemetrexed combination therapy in lung cancer: pathway analysis reveals novel toxicity associations. Pharm J. 2014;14:411–7.
Smit EF, Burgers SA, Biesma B, Smit HJ, Eppinga P, Dingemans AM, et al. Randomized phase II and pharmacogenetic study of pemetrexed compared with pemetrexed plus carboplatin in pretreated patients with advanced non-small-cell lung cancer. J Clin Oncol. 2009;27:2038–45.
Adjei AA, Salavaggione OE, Mandrekar SJ, Dy GK, Ziegler KL, Endo C, et al. Correlation between polymorphisms of the reduced folate carrier gene (SLC19A1) and survival after pemetrexed-based therapy in non-small cell lung cancer: a North Central Cancer Treatment Group-based exploratory study. J Thorac Oncol. 2010;5:1346–53.
Perez-Ramirez C, Canadas-Garre M, Alnatsha A, Villar E, Delgado JR, Faus-Dader MJ, et al. Pharmacogenetic predictors of toxicity to platinum based chemotherapy in non-small cell lung cancer patients. Pharmacol Res. 2016;111:877–84.
Kartalou M, Essigmann JM. Recognition of cisplatin adducts by cellular proteins. Mutat Res. 2001;478:1–21.
Jordan P, Carmo-Fonseca M. Molecular mechanisms involved in cisplatin cytotoxicity. Cell Mol Life Sci. 2000;57:1229–35.
Sancar A. DNA repair in humans. Annu Rev Genet. 1995;29:69–105.
Garcia-Campelo R, Alonso-Curbera G, Anton Aparicio LM, Rosell R. Pharmacogenomics in lung cancer: an analysis of DNA repair gene expression in patients treated with platinum-based chemotherapy. Expert Opin Pharmacother. 2005;6:2015–26.
Jin S, Levine AJ. The p53 functional circuit. J Cell Sci. 2001;114(Pt 23):4139–40.
Michael D, Oren M. The p53-Mdm2 module and the ubiquitin system. Semin Cancer Biol. 2003;13:49–58.
Azzoli CG, Baker S, Temin S, Pao W, Aliff T, Brahmer J, et al. American Society of Clinical Oncology clinical practice guideline update on chemotherapy for stage IV non-small-cell lung cancer. J Clin Oncol. 2009;27:6251–66.
Benlloch S, Botero ML, Beltran-Alamillo J, Mayo C, Gimenez-Capitan A, de Aguirre I, et al. Clinical validation of a PCR assay for the detection of EGFR mutations in non-small-cell lung cancer: retrospective testing of specimens from the EURTAC trial. PLoS ONE. 2014;9:e89518.
Edge SE, Compton CC, Fritz AG, Green FL, Trotti A, editors. AJCC cancer staging manual. 7 ed. New York: Springer-Verlag; 2010. pp. XV–648.
Jimenez-Varo E, Canadas-Garre M, Henriques CI, Pinheiro AM, Gutierrez-Pimentel MJ, Calleja-Hernandez MA. Pharmacogenetics role in the safety of acenocoumarol therapy. Thromb Haemost. 2014;112:522–36.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MAR, Bender D, et al. PLINK: a toolset for whole-genome association and population-based linkage analysis. Am J Hum Genet. 2007;81:559–75.
Team RCR. A language and environment for statistical computing. [Internet]. Available from http://www.r-project.org/. Accessed Oct 2013.
Gao H, Ge RC, Liu HY, Wang Y, Yan S. Effect of ERCC1 polymorphism on the response to chemotherapy and clinical outcome of non-small cell lung cancer. Genet Mol Res. 2014;13:8997–9004.
Li F, Sun X, Sun N, Qin S, Cheng H, Feng J, et al. Association between polymorphisms of ERCC1 and XPD and clinical response to platinum-based chemotherapy in advanced non-small cell lung cancer. Am J Clin Oncol. 2010;33:489–94.
Panov KI, Panova TB, Gadal O, Nishiyama K, Saito T, Russell J, et al. RNA polymerase I-specific subunit CAST/hPAF49 has a role in the activation of transcription by upstream binding factor. Mol Cell Biol. 2006;26:5436–48.
Russell J, Zomerdijk JC. RNA-polymerase-I-directed rDNA transcription, life and works. Trends Biochem Sci. 2005;30:87–96.
Whitehouse CJ, Taylor RM, Thistlethwaite A, Zhang H, Karimi-Busheri F, Lasko DD, et al. XRCC1 stimulates human polynucleotide kinase activity at damaged DNA termini and accelerates DNA single-strand break repair. Cell. 2001;104:107–17.
Park JY, Lee SY, Jeon HS, Bae NC, Chae SC, Joo S, et al. Polymorphism of the DNA repair gene XRCC1 and risk of primary lung cancer. Cancer Epidemiol Biomark Prev. 2002;11:23–27.
Giachino DF, Ghio P, Regazzoni S, Mandrile G, Novello S, Selvaggi G, et al. Prospective assessment of XPD Lys751Gln and XRCC1 Arg399Gln single nucleotide polymorphisms in lung cancer. Clin Cancer Res. 2007;13:2876–81.
Joerger M, Burgers SA, Baas P, Smit EF, Haitjema TJ, Bard MP, et al. Germline polymorphisms in patients with advanced non-small cell lung cancer receiving first-line platinum-gemcitabine chemotherapy: a prospective clinical study. Cancer. 2012;118:2466–75.
Kalikaki A, Kanaki M, Vassalou H, Souglakos J, Voutsina A, Georgoulias V, et al. DNA repair gene polymorphisms predict favorable clinical outcome in advanced non-small-cell lung cancer. Clin Lung Cancer. 2009;10:118–23.
Kalikaki A, Voutsina A, Koutsopoulos A, Papadaki C, Sfakianaki M, Yachnakis E, et al. ERCC1 SNPs as potential predictive biomarkers in non-small cell lung cancer patients treated with platinum-based chemotherapy. Cancer Invest. 2015;33:107–13.
Sullivan I, Salazar J, Majem M, Pallares C, Del Rio E, Paez D, et al. Pharmacogenetics of the DNA repair pathways in advanced non-small cell lung cancer patients treated with platinum-based chemotherapy. Cancer Lett. 2014;353:160–6.
Tiseo M, Bordi P, Bortesi B, Boni L, Boni C, Baldini E, et al. ERCC1/BRCA1 expression and gene polymorphisms as prognostic and predictive factors in advanced NSCLC treated with or without cisplatin. Br J Cancer. 2013;108:1695–703.
Goode EL, Potter JD, Bigler J, Ulrich CM. Methionine synthase D919G polymorphism, folate metabolism, and colorectal adenoma risk. Cancer Epidemiol Biomark Prev. 2004;13:157–62.
Paz MF, Avila S, Fraga MF, Pollan M, Capella G, Peinado MA, et al. Germ-line variants in methyl-group metabolism genes and susceptibility to DNA methylation in normal tissues and human primary tumors. Cancer Res. 2002;62:4519–24.
Perez-Ramirez C, Canadas-Garre M, Alnatsha A, Villar E, Delgado JR, Faus-Dader MJ, et al. Pharmacogenetic predictors of toxicity to platinum based chemotherapy in non-small cell lung cancer patients. Pharmacol Res. 2016;111:877–84. Submitted
Li X, Shao M, Wang S, Zhao X, Chen H, Qian J, et al. Heterozygote advantage of methylenetetrahydrofolate reductase polymorphisms on clinical outcomes in advanced non-small cell lung cancer (NSCLC) patients treated with platinum-based chemotherapy. Tumour Biol. 2014;35:11159–70.
Okuda K, Sasaki H, Hikosaka Y, Kawano O, Yukiue H, Yano M, et al. Excision repair cross complementation group 1 polymorphisms predict overall survival after platinum-based chemotherapy for completely resected non-small-cell lung cancer. J Surg Res. 2011;168:206–12.
Takenaka T, Yano T, Kiyohara C, Miura N, Kouso H, Ohba T, et al. Effects of excision repair cross-complementation group 1 (ERCC1) single nucleotide polymorphisms on the prognosis of non-small cell lung cancer patients. Lung Cancer. 2010;67:101–7.
Zhao X, Zhang Z, Yuan Y, Yuan X. Polymorphisms in ERCC1 gene could predict clinical outcome of platinum-based chemotherapy for non-small cell lung cancer patients. Tumour Biol. 2014;35:8335–41.
Zhou W, Gurubhagavatula S, Liu G, Park S, Neuberg DS, Wain JC, et al. Excision repair cross-complementation group 1 polymorphism predicts overall survival in advanced non-small cell lung cancer patients treated with platinum-based chemotherapy. Clin Cancer Res. 2004;10:4939–43.
Wu W, Li H, Wang H, Zhao X, Gao Z, Qiao R, et al. Effect of polymorphisms in XPD on clinical outcomes of platinum-based chemotherapy for Chinese non-small cell lung cancer patients. PLoS ONE. 2012;7:e33200.
Su D, Ma S, Liu P, Jiang Z, Lv W, Zhang Y, et al. Genetic polymorphisms and treatment response in advanced non-small cell lung cancer. Lung Cancer. 2007;56:281–8.
Cheng J, Ha M, Wang Y, Sun J, Chen J, Wang Y, et al. A C118T polymorphism of ERCC1 and response to cisplatin chemotherapy in patients with late-stage non-small cell lung cancer. J Cancer Res Clin Oncol. 2012;138:231–8.
Dong J, Hu Z, Shu Y, Pan S, Chen W, Wang Y, et al. Potentially functional polymorphisms in DNA repair genes and non-small-cell lung cancer survival: a pathway-based analysis. Mol Carcinog. 2012;51:546–52.
Isla D, Sarries C, Rosell R, Alonso G, Domine M, Taron M, et al. Single nucleotide polymorphisms and outcome in docetaxel-cisplatin-treated advanced non-small-cell lung cancer. Ann Oncol. 2004;15:1194–203.
Park SY, Hong YC, Kim JH, Kwak SM, Cho JH, Lee HL, et al. Effect of ERCC1 polymorphisms and the modification by smoking on the survival of non-small cell lung cancer patients. Med Oncol. 2006;23:489–98.
Ryu JS, Hong YC, Han HS, Lee JE, Kim S, Park YM, et al. Association between polymorphisms of ERCC1 and XPD and survival in non-small-cell lung cancer patients treated with cisplatin combination chemotherapy. Lung Cancer. 2004;44:311–6.
Krawczyk P, Wojas-Krawczyk K, Mlak R, Kucharczyk T, Biernacka B, Milanowski J. Predictive value of ERCC1 single-nucleotide polymorphism in patients receiving platinum-based chemotherapy for locally-advanced and advanced non-small cell lung cancer--a pilot study. Folia Histochem Cytobiol. 2012;50:80–86.
Lv H, Han T, Shi X, Yao Y, Yao Y, Qiu W, et al. Genetic polymorphism of GSTP1 and ERCC1 correlated with response to platinum-based chemotherapy in non-small cell lung cancer. Med Oncol. 2014;31:86.
Du Y, Su T, Zhao L, Tan X, Chang W, Zhang H, et al. Associations of polymorphisms in DNA repair genes and MDR1 gene with chemotherapy response and survival of non-small cell lung cancer. PLoS ONE. 2014;9:e99843.
Shi ZH, Shi GY, Liu LG. Polymorphisms in ERCC1 and XPF gene and response to chemotherapy and overall survival of non-small cell lung cancer. Int J Clin Exp Pathol. 2015;8:3132–7.
Zhou C, Ren S, Zhou S, Zhang L, Su C, Zhang Z, et al. Predictive effects of ERCC1 and XRCC3 SNP on efficacy of platinum-based chemotherapy in advanced NSCLC patients. Jpn J Clin Oncol. 2010;40:954–60.
Ren S, Zhou S, Wu F, Zhang L, Li X, Zhang J, et al. Association between polymorphisms of DNA repair genes and survival of advanced NSCLC patients treated with platinum-based chemotherapy. Lung Cancer. 2012;75:102–9.
Wang J, Zhang Q, Zhang H, Wang Q, Yang X, Gu Y, et al. Association between polymorphisms of ERCC1 and response in patients with advanced non-small cell lung cancer receiving cisplatin-based chemotherapy. Chin J lung Cancer. 2010;13:337–41.
Huang D, Zhou Y. Nucleotide excision repair gene polymorphisms and prognosis of non-small cell lung cancer patients receiving platinum-based chemotherapy: a meta-analysis based on 44 studies. Biomed Rep. 2014;2:452–62.
Hong CY, Xu Q, Yue Z, Zhang Y, Yuan Y. Correlation of the sensitivity of NP chemotherapy in non-small lung cancer with DNA repair gene XRCC1 polymorphism. Chin J Cancer. 2009;28:1291–7.
Sun X, Li F, Sun N, Shukui Q, Baoan C, Jifeng F, et al. Polymorphisms in XRCC1 and XPG and response to platinum-based chemotherapy in advanced non-small cell lung cancer patients. Lung Cancer. 2009;65:230–6.
Wang ZH, Miao XP, Tan W, Zhang XR, Xu BH, Lin DX. Single nucleotide polymorphisms in XRCC1 and clinical response to platin-based chemotherapy in advanced non-small cell lung cancer. Chin J Cancer. 2004;23:865–8.
Xu C, Wang X, Zhang Y, Li L. Effect of the XRCC1 and XRCC3 genetic polymorphisms on the efficacy of platinum-based chemotherapy in patients with advanced non-small cell lung cancer. Chin J Lung Cancer. 2011;14:912–7.
Yuan P, Miao XP, Zhang XM, Wang ZH, Tan W, Sun Y, et al. XRCC1 and XPD genetic polymorphisms predict clinical responses to platinum-based chemotherapy in advanced non-small cell lung cancer. Zhonghua Zhong Liu Za Zhi. 2006;28:196–9.
Powrozek T, Mlak R, Krawczyk P, Homa I, Ciesielka M, Koziol P, et al. The relationship between polymorphisms of genes regulating DNA repair or cell division and the toxicity of platinum and vinorelbine chemotherapy in advanced NSCLC patients. Clin Transl Oncol. 2016;18:125–31.
Ke HG, Li J, Shen Y, You QS, Yan Y, Dong HX, et al. Prognostic significance of GSTP1, XRCC1 and XRCC3 polymorphisms in non-small cell lung cancer patients. Asian Pac J Cancer Prev. 2012;13:4413–6.
Zhang L, Ma W, Li Y, Wu J, Shi GY. Pharmacogenetics of DNA repair gene polymorphisms in non-small-cell lung carcinoma patients on platinum-based chemotherapy. Genet Mol Res. 2014;13:228–36.
Zhao W, Hu L, Xu J, Shen H, Hu Z, Ma H, et al. Polymorphisms in the base excision repair pathway modulate prognosis of platinum-based chemotherapy in advanced non-small cell lung cancer. Cancer Chemother Pharmacol. 2013;71:1287–95.
Han B, Guo Z, Ma Y, Kang S, Wang Y, Wei Q, et al. Association of GSTP1 and XRCC1 gene polymorphisms with clinical outcome of advanced non-small cell lung cancer patients with cisplatin-based chemotherapy. Int J Clin Exp Pathol. 2015;8:4113–9.
Liu JY, Liu QM, Li LR. Association of GSTP1 and XRCC1 gene polymorphisms with clinical outcomes of patients with advanced non-small cell lung cancer. Genet Mol Res. 2015;14:10331–7.
Liu D, Wu J, Shi GY, Zhou HF, Yu Y. Role of XRCC1 and ERCC5 polymorphisms on clinical outcomes in advanced non-small cell lung cancer. Genet Mol Res. 2014;13:3100–7.
Liao WY, Shih JY, Chang GC, Cheng YK, Yang JC, Chen YM, et al. Genetic polymorphism of XRCC1 Arg399Gln is associated with survival in non-small-cell lung cancer patients treated with gemcitabine/platinum. J Thorac Oncol. 2012;7:973–81.
Zhou M, Ding YJ, Feng Y, Zhang QR, Xiang Y, Wan HY. Association of xeroderma pigmentosum group D (Asp312Asn, Lys751Gln) and cytidine deaminase (Lys27Gln, Ala70Thr) polymorphisms with outcome in Chinese non-small cell lung cancer patients treated with cisplatin-gemcitabine. Genet Mol Res. 2014;13:3310–8.
Tan X, Xian L, Chen X, Shi L, Wang Y, Guo J, et al. Association between ERCC2 Lys751Gln polymorphism and lung cancer risk: a meta-analysis involving 23,370 subjects. Twin Res Human Genet. 2014;17:99–107.
Zhan P, Wang Q, Wei SZ, Wang J, Qian Q, Yu LK, et al. ERCC2/XPD Lys751Gln and Asp312Asn gene polymorphism and lung cancer risk: a meta-analysis involving 22 case-control studies. J Thorac Oncol. 2010;5:1337–45.
Wang Y, Yang H, Li H, Li L, Wang H, Liu C, et al. Association between X-ray repair cross complementing group 1 codon 399 and 194 polymorphisms and lung cancer risk: a meta-analysis. Cancer Lett. 2009;285:134–40.
Acknowledgements
The results of this investigation are part of the doctoral thesis presented by Cristina Pérez-Ramírez at the University of Granada.
Funding
This work was partly supported by a research grant for Cristina Pérez-Ramírez (FPU12/04722), from Ministerio de Educación, Cultura y Deporte.
Author contributions
CP-R revised the bibliography and wrote the protocol for this study and acted as the primary lead in the conception, design, and implementation of the project, data collection, molecular analysis, statistical analysis, and interpretation, as well as all aspects of the development and writing of the article and responses to internal and external reviewers. MC-G supervised the planning of the study protocol and contributed to the conception, design, and implementation of the project, statistical analysis, and interpretation as well as all aspects of the development and writing of the article and responses to internal and external reviewers. AA performed literature review, molecular analysis and interpretation, clinical data collection and interpretation, and collaborated in drafting the manuscript. EV performed molecular and pathological analysis and interpretation, clinical data collection and interpretation, and collaborated in drafting the manuscript. JVB participated in the clinical data collection and interpretation, and provided clinical guidance and feedback for this study and critical review of the manuscript. MJF-D and Miguel ÁC-H participated in article selection, study quality assessment, critical review of the manuscript, and contributed to revisions and responses to internal and external reviewers.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Pérez-Ramírez, C., Cañadas-Garre, M., Alnatsha, A. et al. Pharmacogenetics of platinum-based chemotherapy: impact of DNA repair and folate metabolism gene polymorphisms on prognosis of non-small cell lung cancer patients. Pharmacogenomics J 19, 164–177 (2019). https://doi.org/10.1038/s41397-018-0014-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41397-018-0014-8
This article is cited by
-
Genetic polymorphisms as potential pharmacogenetic biomarkers for platinum-based chemotherapy in non-small cell lung cancer
Molecular Biology Reports (2024)
-
X-ray cross-complementing family: the bridge linking DNA damage repair and cancer
Journal of Translational Medicine (2023)