Abstract
Study design
Observational study.
Objectives
To evaluate the perceptions of patients requiring a tracheostomy tube and to identify possible different perceptions in critically ill patients with tracheostomy tubes who have acute (ASCI) or chronic spinal cord injuries (CSCI).
Setting
Medical and surgical intensive care units (ICU) and intermediate care unit of the BG University Hospital Bergmannsheil Bochum, Germany.
Methods
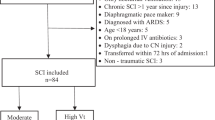
Patients who met the inclusion criteria completed a 25-item questionnaire on two consecutive days regarding their experiences and perceptions in breathing, coughing, pain, speaking, swallowing, and comfort of the tracheostomy tube.
Results
A total of 51 persons with ASCI (n = 31) and CSCI (n = 20) were included with a mean age of 53 years. Individuals with ASCI reported significantly more frequent pain and swallowing problems as compared to individuals with CSCI (p ≤ 0.014) at initial assessment. There were no differences between ASCI and CSCI reported with respect to speaking and overall comfort.
Conclusions
It is necessary to regularly assess the perceptions of critically ill patients with tracheostomy tubes with ASCI or CSCI in the daily ICU care routine. We were able to assess these perceptions in different categories. For the future, evaluating the perception of individuals with SCI and a tracheostomy should be implemented to their daily routine care.
Trial registration
DRKS00022073.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 1 print issues and online access
We are sorry, but there is no personal subscription option available for your country.
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data that was generated and analyzed during this study can be found within the published article. Additional data are available from the corresponding author on reasonable request.
References
Berlowitz DJ, Wadsworth B, Ross J. Respiratory problems and management in people with spinal cord injury. Breathe. 2016;12:328–40. https://doi.org/10.1183/20734735.012616.
Rogers WK, Todd M. Acute spinal cord injury. Best Pract Res Clin Anaesthesiol. 2016;30:27–39. https://doi.org/10.1016/j.bpa.2015.11.003.
Leelapattana P, Fleming JC, Gurr KR, Bailey SI, Parry N, Bailey CS. Predicting the need for tracheostomy in patients with cervical spinal cord injury. J Trauma Acute Care Surg. 2012;73:880–4. https://doi.org/10.1097/TA.0b013e318251fb34.
Branco BC, Plurad D, Green DJ, Inaba K, Lam L, Cestero R, et al. Incidence and clinical predictors for tracheostomy after cervical spinal cord injury: a National Trauma Databank review. J Trauma. 2011;70:111–5. https://doi.org/10.1097/TA.0b013e3181d9a559.
Kupfer M, Kucer BT, Kupfer H, Formal CS. Persons with chronic spinal cord injuries in the emergency department: a review of a unique population. J Emerg Med. 2018;55:206–12. https://doi.org/10.1016/j.jemermed.2018.04.029.
Ong B, Wilson JR, Henzel MK. Management of the patient with chronic spinal cord injury. Med Clin North Am. 2020;104:263–78. https://doi.org/10.1016/j.mcna.2019.10.006.
Berney S, Bragge P, Granger C, Opdam H, Denehy L. The acute respiratory management of cervical spinal cord injury in the first 6 weeks after injury: a systematic review. Spinal Cord. 2011;49:17–29. https://doi.org/10.1038/sc.2010.39.
Yugue I, Okada S, Ueta T, Maeda T, Mori E, Kawano O, et al. Analysis of the risk factors for tracheostomy in traumatic cervical spinal cord injury. Spine. 2012;37:E1633–8. https://doi.org/10.1097/BRS.0b013e31827417f1.
Childs BR, Moore TA, Como JJ, Vallier HA. American Spinal Injury Association Impairment Scale predicts the need for tracheostomy after cervical spinal cord injury. Spine. 2015;40:1407–13. https://doi.org/10.1097/BRS.0000000000001008.
Schonhofer B, Geiseler J, Dellweg D, Fuchs H, Moerer O, Weber-Carstens S, et al. Prolonged weaning: S2k guideline published by the German Respiratory Society. Respiration. 2020:1–102. https://doi.org/10.1159/000510085.
Newman H, Clunie G, Wallace S, Smith C, Martin D, Pattison N. What matters most to adults with a tracheostomy in ICU and the implications for clinical practice: a qualitative systematic review and metasynthesis. J Crit Care. 2022;72:154145 https://doi.org/10.1016/j.jcrc.2022.154145.
Sun GH, Chen SW, MacEachern MP, Wang J. Successful decannulation of patients with traumatic spinal cord injury: a scoping review. J Spinal Cord Med. 2022;45:498–509. https://doi.org/10.1080/10790268.2020.1832397.
Scantling D, Granche J, Williamson J, Gracely E, Thosani D, McCracken B. Development of clinical tracheostomy score to identify cervical spinal cord injury patients requiring prolonged ventilator support. J Trauma Acute Care Surg. 2019;87:195–9. https://doi.org/10.1097/TA.0000000000002286.
Raimondi N, Vial MR, Calleja J, Quintero A, Cortes A, Celis E, et al. Evidence-based guidelines for the use of tracheostomy in critically ill patients. J Crit Care. 2017;38:304–18. https://doi.org/10.1016/j.jcrc.2016.10.009.
McRae J, Smith C, Beeke S, Emmanuel A. Members of the Delphi expert panel g. Development of a swallowing risk screening tool and best practice recommendations for the management of oropharyngeal dysphagia following acute cervical spinal cord injury: an international multi-professional Delphi consensus. Disabil Rehabil. 2021:1–14. https://doi.org/10.1080/09638288.2021.2012607.
Hirota R, Terashima Y, Ohnishi H, Yamashita T, Yokogawa N, Sasagawa T, et al. Prognostic factors for respiratory dysfunction for cervical spinal cord injury and/or cervical fractures in elderly patients: a multicenter survey. Global Spine J. 2022:21925682221095470. https://doi.org/10.1177/21925682221095470.
Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18:805–35. https://doi.org/10.1097/EDE.0b013e3181577511.
Ely EW, Truman B, Shintani A, Thomason JW, Wheeler AP, Gordon S, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA. 2003;289:2983–91. https://doi.org/10.1001/jama.289.22.2983.
Gaudreau JD, Gagnon P, Harel F, Tremblay A, Roy MA. Fast, systematic, and continuous delirium assessment in hospitalized patients: the nursing delirium screening scale. J Pain Symptom Manage. 2005;29:368–75. https://doi.org/10.1016/j.jpainsymman.2004.07.009.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. https://doi.org/10.1016/0021-9681(87)90171-8.
Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D, et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord. 2007;45:190–205. https://doi.org/10.1038/sj.sc.3102007.
Burns AS, Marino RJ, Flanders AE, Flett H. Clinical diagnosis and prognosis following spinal cord injury. Handb Clin Neurol. 2012;109:47–62. https://doi.org/10.1016/B978-0-444-52137-8.00003-6.
Maynard FM Jr., Bracken MB, Creasey G, Ditunno JF Jr., Donovan WH, Ducker TB, et al. International standards for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Spinal Cord. 1997;35:266–74. https://doi.org/10.1038/sj.sc.3100432.
Ull C, Weckwerth C, Hamsen U, Jansen O, Spieckermann A, Schildhauer TA, et al. Development of the tracheostomy well-being score in critically ill patients. Eur J Trauma Emerg Surg. 2022. https://doi.org/10.1007/s00068-022-02120-9.
Ull C, Hamsen U, Weckwerth C, Schildhauer TA, Gaschler R, Jansen O, et al. The use of predefined scales and scores with eye-tracking devices for symptom identification in critically ill nonverbal patients. J Trauma Acute Care Surg. 2022;92:640–7. https://doi.org/10.1097/TA.0000000000003494.
Nakarada-Kordic I, Patterson N, Wrapson J, Reay SD. A systematic review of patient and caregiver experiences with a tracheostomy. Patient. 2018;11:175–91. https://doi.org/10.1007/s40271-017-0277-1.
Breckenridge SJ, Chlan L, Savik K. Impact of tracheostomy placement on anxiety in mechanically ventilated adult ICU patients. Heart Lung. 2014;43:392–8. https://doi.org/10.1016/j.hrtlng.2014.01.005.
van Diemen T, van Leeuwen C, van Nes I, Geertzen J, Post M. Body image in patients with spinal cord injury during inpatient rehabilitation. Arch Phys Med Rehabil. 2017;98:1126–31. https://doi.org/10.1016/j.apmr.2016.10.015.
Cuff L, Fann JR, Bombardier CH, Graves DE, Kalpakjian CZ. Depression, pain intensity, and interference in acute spinal cord injury. Top Spinal Cord Inj Rehabil. 2014;20:32–9. https://doi.org/10.1310/sci2001-32.
Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS. A longitudinal study of depression from 1 to 5 years after spinal cord injury. Arch Phys Med Rehabil. 2011;92:411–8. https://doi.org/10.1016/j.apmr.2010.10.036.
Craig A, Tran Y. Psychological aspects associated with spinal cord injury rehabilitation: new directions and best evidence. Nova Science Publishers, 2008. 286 p.
Acknowledgements
We thank Monica Monica Mary Heil for language editing the manuscript. This work was supported by the ”Junior Clinician Scientist Program” of the Ruhr-University Bochum, Germany [grant number K129-19]. The funding bodies did not influence the study’s design, the collection, analysis, and interpretation of data, nor in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Concept/design: CWe, CWa, RG, CU; Data analysis/interpretation: CWe, CWa, RG, CU; Writing of article: CWe, AS, CU; Critical revision of the article: CWe, CWa, UH, OC, AS, TAS, RG, MA, CU; Approval of article: CWe, CWa, UH, OC, AS, TAS, RG, MA, CU; Funding secured by: CU; Data collection: CU.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. It was approved by the local ethics committee (Ruhr-University Bochum, Germany, grant number of approval 18-6620-BR). Informed consent was obtained from each person. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Weckwerth, C., Waydhas, C., Hamsen, U. et al. Perceptions of critically ill individuals with acute and chronic spinal cord injury requiring a tracheostomy tube. Spinal Cord Ser Cases 10, 12 (2024). https://doi.org/10.1038/s41394-024-00624-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-024-00624-7