Abstract
Background
Intradural cysts of the spine are arachnoid cysts, neuroenteric cysts, and ependymal cysts. The usual finding in case of a neurenteric cyst is a ventrally located non-contrast-enhancing lesion that is isointense on T1-weighted sequence and hyperintense on T2-weighted imaging. An arachnoid cyst is hypointense in T1-weighted image and hyperintense in T2-weighted image, mimicking cerebrospinal fluid(CSF), and the location is dorsal to the cord. But a neurenteric cyst can mimic an arachnoid cyst in appearance.
Case
A 48-yr old autorikshaw driver presented with weakness of fingers and lower limbs. All sensations were decreased below xiphisternum(T6). The gait was spastic. Magnetic Resonance Imaging(MRI) showed an extramedullary intradural cyst at C7-T1 level. It was hypointense on T1-weighted image and hyperintense on T2-weighted image. There was no enhancement with contrast. C7/T1 Laminectomy was done. On gentle retraction of the cord, a whitish cyst was seen. Some clear fluid was aspirated and cyst was excised en toto. Myelopathy improved over two weeks. Histopathological examination showed a cyst wall composed of fibrocollagenous tissue, and lined by pseudostratified epithelium containing many goblet cells and having focal ciliation. The findings were consistent with neurenteric cyst. Follow-up MRI after five years showed no recurrence.
Conclusion
To our knowledge, the peculiarities of the case are that the radiological features mimicked arachnoid cyst in having the intensity of CSF. But the ventral location was suggestive of a neurenteric cyst. Total excision could be done through the posterior approach after decompressing the cyst by aspiration.
Similar content being viewed by others
Introduction
A varety of cystic lesions of congenital, traumatic, inflammatory, or degenerative etiology can occur in the extradural, intradural, and intramedullary locations of the spinal canal [1]. The various cysts of the spinal canal are arachnoid cyst, meningeal cyst, perineural cyst, juxtafacet cyst, discal cyst, bronchogenic cyst, neurenteric cyst, dermoid cyst, epidermoid cyst, cystic schwannoma, hydatid cyst, abscess, and pseudocyst [1, 2]. The etiological factors of these are different, such as congenital, traumatic, inflammatory, degenerative, hydrostatic, osmotic,and secretory. The differential diagnoses of intradural cysts are arachnoid cysts, neuroenteric cysts, and ependymal cysts [3]. Progressive myelopathy is the usual clinical presentation of these lesions. The arachnoid derived lesions are the most common among the cysts [1]. A neurenteric cyst can mimic an arachnoid cyst in appearance.
Case report
A 48-yr old autorikshaw driver presented with weakness of fingers and lower limbs for few weeks. There was weakness of intrinsic muscles of hand. The lower limb muscles had power of grade 4. American Spinal Injury Association Impairment Scale (AIS) grade was D (incomplete). Knee and ankle jerks were very brisk bilaterally. All sensations were decreased below xiphisternum (T6). The gait was spastic.
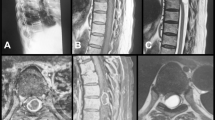
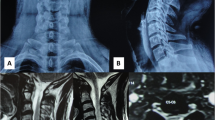
Magnetic Resonance Imaging(MRI) showed a well defined, extramedullary intradural mass lesion at C7-T1 level, causing severe compression of the spinal cord (Fig. 1). It was hypointense on T1-weighted image and hyperintense on T2-weighted image (Fig. 2). There was no enhancement with contrast (Fig. 3). The features were suggestive of arachnoid cyst or neurenteric cyst.
C7/T1 Laminectomy was done. The duramater was opened. On gentle retraction of the cord, a whitish cyst was seen, more on right side. Some clear fluid was aspirated to decompress and cyst wall was dissected and excised en toto (Fig. 4). The cord was seen relaxed after the removal of the cyst (Fig. 5). The postoperative period was uneventful except for small pseudomeningocele. Myelopathy improved over two weeks.
Histopathological examination showed a collapsed cystic mass. The sections showed a thin and translucent cyst wall composed of fibrocollagenous tissue, and lined by pseudostratified epithelium containing many goblet cells and having focal ciliation (Figs. 6 and 7). There was no keratinization, dermal appendages, inflammation or cytological atypia. The findings were consistent with neurenteric cyst.
Follow-up was done up to five years. He was asymptomatic except mild pain on lateral movement of neck. There was no difficulty in work. MRI was done and showed decompressed cord. There was no recurrence (Fig. 8).
Discussion
A search was done in Pubmed, Scopus, and Google Scholar for the neureneteric cysts of the spine. The search was for the etiology, clinical features, imaging, surgery, and the histopathological examination findings.
The main embryological factor is the persistence of the neurenteric canal leading to formation of cysts containing mucus-secreting epithelium reminiscent of the gastrointestinal tract [4, 5]. Holcomb and Matson coined the term neurenteric cyst (NEC) while describing the thoracic cyst of a four and a half year old boy [6].The cyst was attached to the anterior cord by a fibrous stalk through a defect in the third vertebral body. Microscopy showed fetal intestinal epithelium with layers of smooth muscle and was considered to be a cyst of neurenteric origin. The theory of formation of neurenteric cyst is based on midline abnormal entodermal-ectodermal adhesion resulting in interference with the rostral migration of mesoblasts and causing a split in the notochord [5, 7].
The World Health Organization (WHO) classification defines the neurenteric cyst as “a cyst lined by mucin secreting epithelium, resembling that of the gastrointestinal tract” [5]. Neurenteric cysts constitute about 0.7–1.3% of the spinal axis tumors and 90% of them occur in the intradural extramedullary compartment [4, 7]. The common locations are the ventral and the ventro-lateral aspect of the spinal cord [7, 8]. The most common level is cervical, followed by the thoracic and lumbosacral spine. Although the majority occur as solitary lesions, disseminated disease also has been reported [4, 9].
The usual age of presentation is in the second and third decades of life. There is a male predominance [4]. Progressive weakness is the usual symptom. But acute presentation is reported in children [10]. The clinical features seen are focal pain at the level of lesion, radicular pain along the dermatome, weakness, paresthesia and signs of myelopathy such as weakness, spasticity, and hyperreflexia [4, 7]. The symptoms and signs of myelopathy can be fluctuating. The reason behind the fluctuations in the spinal cord compression is the osmotic change in the cyst volume. The waxing and waning of symptoms can mimic demyelinating disease [4, 11]. The children may present with acute spinal cord compression, aseptic meningitis, pyogenic meningitis, pyrexia, or incontinence [4, 10]. A variety of congenital abnormalities can be seen in association with neurenteric cysts. They are spinal dysraphism, scoliosis, hemivertebrae, block vertebrae, butterfly vertebrae, bifid clivus, spina bifida, split cord malformation, spinal lipoma, meningocele, syringomyelia, and Kippel-Fiel syndrome [4, 5, 7, 10, 12].The cutaneous manifestations such as hairy patches, pedunculated growth, capillary hemangioma, and subcutaneous masses can be seen in children [7, 13]. Other systemic abnormalities such as duplication of the alimentary tract and fistulae, tracheoesophageal fistula, esophageal atresia, renal and limb dysgenesis, and Mullerian duct aplasia may also be seen in association with neureneteric cysts [5].
MRI and computed tomography (CT) with myelography are the imaging modalities. But the current preferred modality is MRI [4]. The usual MRI findings in favor of a neurenteric cyst are ventral location, isointensity on T1-weighted sequence, hyperintensity on T2-weighted image, and no enhancement with gadolinium [4, 5]. But hypointensity or hyperintensity in T1- weighted image also may be seen according to the density of the content [14, 15]. More atypical features are seen in intramedullary neurenteric cysts. A well defined peripherally enhancing intramedullary cystic lesion mimicking an abscess was reported [16]. Another intramedullary neurenteric cyst had a false mural nodule due to mucinous clots deposited at the bottom of the cyst [17]. Variation in location with dorsal relation to the cord is also reported [5, 13]. The only advantage of CT scan is that it can show the associated abnormalities of the vertebral canal [4]. A positive meniscus sign can be seen in CT myelography. Arachnoid cyst is the close differential diagnosis of a neurenteric cyst, among the intradural non-enhancing cysts [2]. But arachnoid cyst is hypointense in T1-weighted image and hyperintense in T2-weighted image, mimicking cerebrospinal fluid (CSF), and the usual location is dorsal to the cord.
The aim of treatment is total surgical excision [4, 5, 12]. The surgical options are total removal, subtotal resection, fenestration of cyst, and simple aspiration [7]. The posterior approach by laminectomy is the technique reported in most of the cases [4, 5, 12]. The advantage of the the posterior approach is that intraoperative complications are less [4]. But the disadvantage is that the ventral location and adherence to the cord may prevent total resection [7]. The chance of symptomatic recurrence is high with subtotal resection [4, 5, 7]. Intraoperative aspiration of the cyst content reduces the mass effect and can facilitate the resection [4, 7]. But a leakage of the content can induce chemical meningitis. Anterior approach by corpectomy can help in the complete excision of a ventral cyst [4, 5, 8, 18, 19]. But the chance of injury to the adjacent neurovascular structures and the need for instrumentation are the disadvantages of this approach. Although the lateral approach was used infrequently, it has the advantage of visualization of the boundary between the cyst and the cord [4, 20, 21]. The cyst could be dissected without retracting the cord, in the lateral approach.
A neurenteric cyst is lined by simple or pseudostratified columnar or cuboidal epithelium with or without cilia, mucous glands, and or goblet cells [4, 5, 7, 22]. The basal membrane is composed of type IV collagen. Other connective tissue elements also can be seen. Immunohistochemistry (IHC) of the epithelial cells show positivity for cytokeratin (CK), epithelial membrane antigen (EMA), and carcinoembryonic antigen (CEA). The histopathology of arachnoid cyst shows delicate connective tissue with a covering of meningothelial cells [23]. Epidermoid and dermoid cysts are white cystic lesions containing either keratin or sebaceous material. The lining epithelium is keratinizing squamous epithelium in both of these lesions.
To our knowledge, one of the peculiarities of the case is that the radiological features mimicked arachnoid cyst in having the intensity of CSF. But the ventral location was suggestive of a neurenteric cyst. Another importance is that total excision could be done through the posterior approach after decompressing the cyst by aspiration. MRI scan after 5 years showed no recurrence.
References
Sun, J. Classification, mechanism and surgical treatments for spinal canal cysts. Chin NeurosurgJl. 2, 7 (2016). https://doi.org/10.1186/s41016-016-0022-y.
Savardekar A, Singla N, Mohindra S, Ahuja CK, Gupta SK. Cystic spinal schwannomas: a short series of six cases. Can we predict them preoperatively? SurgNeurol Int. 2014;5:S349–53. https://doi.org/10.4103/2152-7806.139666.
Osenbach RK, Godersky JC, Traynelis VC, Schelper RD. Intraduralextramedullary cysts of the spinal canal: clinical presentation, radiographic diagnosis, and surgical management. Neurosurgery 1992;30:35–42.
Savage JJ, Casey JN, McNeill IT, Sherman JH. Neurenteric cysts of the spine. JCraniovertebr Junction Spine. 2010;1:58–63. https://doi.org/10.4103/0974-8237.65484.
Menezes AH, Traynelis VC. Spinal neurenteric cysts in the magnetic resonance imaging era. Neurosurgery. 2006;58:97–105. https://doi.org/10.1227/01.neu.0000192160.
Holcomb GW,Jr, Matson DD. Thoracic neurenteric cyst. Surgery. 1954;35:115–21.
Baek WK, Lachkar S, Iwanaga J, Oskouian RJ, Loukas M, Oakes WJ, et al. Comprehensive review of spinal neurenteric cysts with a focus on histopathological findings. Cureus. 2018;10:e3379 https://doi.org/10.7759/cureus.3379.
Kida K, Tani T, Kawazoe T, Hiroi M. A recurrent cervical neurenteric cyst treated anteriorly: safe, gross-total excision facilitated by prophylactic unilateral vertebral artery exposure, microdissection, and spinal cord monitoring-a case report and technical note. Case Rep Orthop. 2018;2018:7620182 https://doi.org/10.1155/2018/7620182.
Oyama H, Ikeda A, Inoue S, Nakamura S, Nishimura Y, Shibuya M. et al. Multiple neurenteric cysts in the posterior fossa and cervical spinal canal-case report. Neurol Med Chir (Tokyo). 2004;44:146–9.
de Oliveira RS, Cinalli G, Roujeau T, Sainte-Rose C, Pierre-Kahn A, Zerah M, et al. Neurenteric cysts in children: 16 consecutive cases and review of the literature. J Neurosurg. 2005;103:512–23. https://doi.org/10.3171/ped.2005.103.6.0512.
Vinters HV, Gilbert JJ. Neurenteric cysts of the spinal cord mimicking multiple sclerosis. Can J Neurol Sci. 1981;8:159–61. https://doi.org/10.1017/s0317167100043092. MayPMID: 7296425
Garg N, Sampath S, Yasha TC, Chandramouli BA, Devi BI, Kovoor JM, et al. Is total excision of spinal neurenteric cysts possible? Br J Neurosurg. 2008;22:241–51. https://doi.org/10.1080/02688690701818919.
Rauzzino MJ, Tubbs RS, Alexander E 3rd, Grabb PA, Oakes WJ. Spinalneurenteric cysts and their relation to more common aspects of occult spinal dysraphism. Neurosurg Focus. 2001;10:e2 https://doi.org/10.3171/foc.2001.10.1.3.
Miyagi K, Mukawa J, Mekaru S, Ishikawa Y, Kinjo T, Nakasone S. Enterogenous cyst in the cervical spinal canal. Case report JNeurosurg. 1988;68:292–6. https://doi.org/10.3171/jns.1988.68.2.0292.
Sasani M, Ozer AF, Oktenoglu BT, Peker K, Bozkus MH, Sarioglu AC, et al. Excision of an asymptomatic cervical intraduralneurenteric cyst through the anterior approach: a study of two cases and a review of the literature. Spine J. 2007;7:720–7. https://doi.org/10.1016/j.spinee.2006.12.010.
Muzumdar D, Bhatt Y, Sheth J. Intramedullary cervical neurenteric cyst mimicking an abscess. PediatrNeurosurg. 2008;44:55–61. https://doi.org/10.1159/000110664.
Paolini S, Ciappetta P, Domenicucci M, Guiducci A. Intramedullary neurenteric cyst with a false mural nodule: case report. Neurosurgery. 2003;52:243–5. https://doi.org/10.1097/00006123-200301000-00033.
Devkota UP, Lam JM, Ng H, Poon WS. An anterior intraduralneurenteric cyst of the cervical spine: complete excision through central corpectomy approach-case report. Neurosurgery. 1994;35:1150–3. https://doi.org/10.1227/00006123-199412000-00021.
Takase T, Ishikawa M, Nishi S, Aoki T, Wada E, Owaki H, et al. A recurrent intradural cervical neurenteric cyst operated on using an anterior approach: a case report. Surgical Neurol. 2003;59:34–9. https://doi.org/10.1016/s0090-3019(02)01001-7.
Abhishek A, Anushree A, Patir R, Sehgal AD. Extreme lateral approach in a case of acute-onset quadriplegia due to high cervical neurenteric cyst. PediatrNeurosurg. 2007;43:134–6. https://doi.org/10.1159/000098388.
Song JK, Burkey BB, Konrad PE. Lateral approach to a neurenteric cyst of the cervical spine: case presentation and review of surgical technique. Spine (Philos Pa 1976). 2003;28:E81–5. https://doi.org/10.1097/01.BRS.0000049225.46912.BA.
Chen CT, Lai HY, Jung SM, Lee CY, Wu CT, Lee ST. Neurenteric cyst or neuroendodermal cyst? immunohistochemical study and pathogenesis. World Neurosurg. 2016;96:85–90. https://doi.org/10.1016/j.wneu.2016.08.089.
Pant I, Chaturvedi S. Spectrum of histopathology in spinal lesions. Astrocyte. 2016;2:187–99.
Acknowledgements
We acknowledge Dr.Jayalakshmi Panicker Balakrishna for her pathology opinion in this work.
Author information
Authors and Affiliations
Contributions
The author treated the patient, searched the literature, and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Ethics approval
For retrospective analysis.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Unnithan, A.K.A. A case of neurenteric cyst of spine mimicking an arachnoid cyst. Spinal Cord Ser Cases 8, 31 (2022). https://doi.org/10.1038/s41394-022-00500-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-022-00500-2