Abstract
Introduction
Surgical site infections (SSI) following spinal surgery can result in serious complications. Although early detection and intensive care are essential to minimize possible sequelae, more than one surgical intervention is required to alleviate the infection in some cases.
Case presentation
A 66-year-old man with long-standing Parkinson’s disease (PD) developed SSIs after cervical laminoplasty. Despite surgical debridement and irrigation, his neurological status worsened severely and anterior infectious involvement at the C4-5 level was identified by magnetic resonance imaging. He underwent another urgent surgery for anterior debridement and iliac bone grafting. His laboratory results gradually normalized with antibiotic therapy, and his neurological status improved. One year after surgery, he was ambulatory with walker assistance. However, his right hand remained difficult to control with significant sensory loss and numbness.
Discussion
To our knowledge, this is the first case of SSI that extended rapidly to the anterior side despite immediate and intensive treatment in a patient with PD after laminoplasty. During SSI treatment, meticulous observation should be performed to check for exacerbations.
Similar content being viewed by others
Introduction
The development of a surgical site infection (SSI) following spinal surgery is a complex issue [1,2,3,4]. Once it occurs, patients face to extra burden, such as prolonged antibiotic administration, longer hospitalization, and additional surgery [4]. Longer treatment periods require additional costs to healthcare providers. Neurological deterioration and other possible sequelae are also important concerns [2]. To minimize these problems, postoperative observation should be performed to detect SSI immediately. Studies have suggested methods to detect early-stage SSI [5, 6]. However, choosing a surgical intervention such as debridement, based only on the clinical markers is difficult. Meticulous evaluation is required in uncertain cases. We report SSI case resulting in severe complications after cervical laminoplasty, even after early and intensive intervention.
Case presentation
A 66-year-old man presented with gradually worsening clumsiness of hands and difficulty in walking, which started 2 years previously. He had long-standing Parkinson’s disease (PD) with Hoen and Yahr stage 3. He had severe dyskinesia of the head and neck area, which was likely caused by the PD medication. His neurological findings were compatible with cervical myelopathy. He had a Japananese Orthopaedic Association score [7] (Table 1) of 7 (01-121-2) (full-scale: 33-222-3 = 17). Radiography showed moderate degenerative changes in the cervical spine (Fig. 1). Magnetic resonance imaging (MRI) revealed severe stenosis at the C4-5 level (Fig. 2a, b). We performed bilateral open-door laminoplasty at C3–C5. The operation lasted for 133 min, and the intraoperative blood loss was 50 ml. One day after surgery, he was able to grasp. The patient began rehabilitation, and his walking improved gradually.
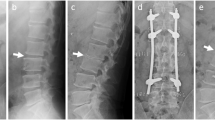
However, 10 days after surgery, partial dehiscence of the incision was noticed, and discharge developed at the surgical site. Retrospectively, he was afebrile, but his blood data worsened. His C-reactive protein (CRP) level increased from 0.23 to 9.54 mg/dL, and his white blood cell (WBC) count also increased from 3600 to 6800/μL. CT revealed fluid collection between the paraspinal musculature (Fig. 3). The patient underwent surgical debridement and irrigation. The intraoperative findings of purulent fluid confirmed deep SSI. Thus, intravenous antibiotic therapy was administered. The patient became delirium after the surgery and was closely observed. Two days after debridement, he recovered from delirium, and we noticed a lack of voluntary movement in the upper and lower extremities. However, he did not complain of pain or numbness. MRI based on the International Standards for Neurological Classification of Spinal Cord Injury was as follows; key muscles of upper extremities were grade 0 except finger flexors on both side as grade 1 and lower extremities had grade 0 in L2-L3 and L4-S1 lesion showed grade 1 on both sides. Sensory was disturbed below C5. Motor subscores were 2/50 in upper extremities and 6/50 in lower extremities. Sensory subscores were 64/112 in light touch and 62/112 in pinprick and ASIA impairment scale was C. We immediately performed MRI, which revealed an anterior inflammatory swelling and posterior fluid-like collection at the C4-5, suggesting discitis change and severe spinal cord compression (Fig. 4a, b). The patient underwent a second urgent surgery for anterior debridement and iliac bone grafting at C4-5 (Fig. 5). Cultures from the first debridement demonstrated Staphylococcus epidermidis. Antibiotics were changed from vancomycin to levofloxacin, which was administered for the next 6 days. This was then shifted to clindamycin because of temporary fever. Voluntary muscle contraction was observed the day after anterior surgery. Two weeks after anterior surgery, the motor strength improved such that he was able to hold his cellphone to talk. CRP level normalized after four weeks. His neurological function gradually improved with rehabilitation. One year after surgery, he was ambulatory with walker assistance. Key muscles recovered to grade 4 in C5 to C7 except C8 and T1 remained 3 and 1 respectively. All lower key muscles recovered to grade 4 on both sides.
Motor subscores were 32/50 in upper extremities and 40/50 in lower extremities. His sensory recovered to normal in C2 to C5, trunk area, and L1 to L2. Light touch and Pin prick test showed same disturbance with numbness on especially hand, finger region. Sensory subscores were 90/112 in light touch and 90/112 in pinprick. ASIA impairment scale was D. However, his right hand was still difficult to control with significant numbness.
Discussion
In this report, we presented a case of devastating condition after cervical laminoplasty who developed anterior involvement and neurological morbidity despite quick and intensive treatment for SSI. SSI following spinal surgery is a major concern in practice for spinal disorders [1,2,3,4]. In deep SSI cases, single surgical debridement was insufficient to address the infection [2, 8]. Increased medical costs are also an important issue in healthcare systems [9, 10]. Early detection of SSI is crucial to minimize concomitant problems, and adequate intervention is required to prevent serious sequelae. However, the diagnosis of SSI is sometimes difficult because the surgical site may not exhibit overt signs. Studies have reported several methods to detect early-stage SSIs. However, it remains challenging to choose a surgical intervention, such as debridement, based only on clinical markers [5, 6]. In the current case, the patient was unremarkable during the first week after surgery. He began rehabilitation the day after surgery, and he had no symptoms suggesting an SSI. His laboratory data 1 week later indicated a normal postoperative course. The CRP level decreased to 0.23 mg/dL from 2.1 mg/dL at 4 days after surgery, and the WBC count remained within the normal range. His lymphocyte count decreased to 1008/μL (28.4%) from 1246/μL (27.7%) 4 days after surgery. He remained afebrile after the surgery; thus, detecting SSI in this case was difficult. Upon noticing incision dehiscence and discharge, emergency debridement and irrigation were performed, and intravenous antibiotic was administered. Close observation did not show neurological changes due to postoperative delirium. His akinesia was likely caused by the sudden suspension of anti-PD medication because of urgent surgical debridement. However, prolonged quadriplegia led us to suspect that the SSI site was worsening. An anterior expansion of the infection from the posterior element can occur during SSI treatment [11, 12]. The infection may have expanded through the C4-5 peridiscal region on the base of the degenerated structure around the intervertebral disc, breakage of the posterior longitudinal ligament or annular ligament, and osteophyte formation at the C4-5. However, direct evidence of this mechanism was not obtained, and the CT taken before the first debridement showed no obvious change at the C4-5 level. Previously, subsequent spread of the infection to the adjacent disc space or epidural plexus was reported as a less common SSI complications after anterior disc surgery [13]. The rapid expansion of infection to the anterior element rarely occurs after surgical debridement in SSI. Deep SSI may not present with apparent signs of infection in the anterior and posterior approaches. A more meticulous observation should have been performed after the first debridement in the current case.
Conclusion
To our knowledge, this is the first case of SSI after laminoplasty in a patient with PD, which extended rapidly to the anterior side despite urgent surgical debridement and irrigation. Meticulous observation is essential even in cases without overt signs of infection during SSI treatment in the spinal region.
References
Pull ter Gunne A, Mohamed SA, Skolasky LR, Van Laarhoven CJ, Cohen DB. The presentation, incidence, etiology, and treatment of surgical site infections after spinal surgery. Spine. 2010;35:1323–8.
Abdul-Jabbar A, Berven SH, Hu SS, Chou D, Mummaneni PV, Takemoto S, et al. Surgical site infections in spine surgery. Spine 2013;38:E1425–E1431.
Barnes M, Liew S. The incidence of infection after posterior cervical spine surgery: a 10year review. Glob Spine J. 2012;2:3–6.
Sebastian A, Huddleston P, Kakar S, Habermann E, Wagie A, Nassr A. Risk factors for surgical site infection after posterior cervical spine surgery: an analysis of 5441 patients from the ACS NSQIP 2005-2012. Spine J. 2016;16:504–9.
Takahashi J, Shono Y, Hirabayashi H, Kamimura M, Nakagawa H, Ebara S, et al. Usefulness of white blood cell differential for early diagnosis of surgical site infection following spinal instrumentation surgery. Spine. 2006;31:1020–5.
Iwata E, Shigematsu H, Yamamoto Y, Tanaka Y, Okuda A, Morimoto Y, et al. Lymphocyte count at 4 days postoperatively A reliable screening marker for surgical site infection after posterior lumbar decompression surgery. Spine. 2018;43:E1096–E1101.
Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K. Interobserver and intraobserver reliability of the Japanese Orthopaedic Association Scoring System for evaluation of cervical compression myelopathy. Spine. 2001;26:1890–5.
Guo Q, Zhang M, Wang L, Lu X, Ni B. Deep surgical site infection after anterior decompression and fusion with plate fixation for cervical spondylotic radiculopathy or myelopathy. Clin Neurol Neurosurg. 2016;141:13–8.
Massie JB, Heller JG, Abitbol JJ, McPherson D, Garfin SR. Postoperative posterior spinal wound infections. Clin Orthop Relat Res. 1992;284:99–108.
Nasser R, Kosty JA, Shah S, Wang J, Cheng J. Risk factors and prevention of surgical site infections following spinal procedures. Glob Spine J. 2018;8:44S–48S.
Yamazaki T. Prevention and treatment of SSI in posterior spine surgery. Spine Spinal Cord. 2011;24:1069–74. Japanese
Hadipavlou A, Gaitanis IN, Papadopulos CA, Katonis PG, Kontakis GM. Serratia spondylodiscitis after elective lumbar spine surgery. Spine 2002;27:E507–E512.
Kulkarni AG, Hee HT. Adjcacent level discitis after anterior cervical deiscectomy and fusion (ACDF): a case report. Eur Spine J 2006;S5:S559–S563.
Author information
Authors and Affiliations
Contributions
MK: Main operator of this case and writing the manuscript; YK: first assistant of first and second surgery and outpatient follow-up; AY: assistant of third surgery; KO: reviewing English terms; NT: assistant of second surgery; TM: reference collection; YH: reviewing the draft; HS: outpatient follow-up and labo-data collection; SN: photograph preparation; and YT: supervising editor of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Koizumi, M., Kato, Y., Yoneda, A. et al. Severe complication subsequent to surgical site infection after cervical laminoplasty: a case report. Spinal Cord Ser Cases 8, 5 (2022). https://doi.org/10.1038/s41394-021-00472-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00472-9