Abstract
Study design
Pre-post intervention.
Objective
To explore the potential effect of exoskeletal-assisted walking (EAW) on seated balance for persons with chronic motor complete spinal cord injury (SCI).
Setting
A SCI research center.
Methods
Eight participants who were over 18 years of age with chronic SCI and used a wheelchair for mobility were enrolled. Seven able-bodied participants were used for normal seated balance comparative values. Participants with chronic SCI received supervised EAW training using a powered exoskeleton (ReWalkTM) for a median 30 sessions (range from 7 to 90 sessions). Before and after EAW training, seated balance testing outcomes were collected using computerized dynamic posturography, providing measurements of endpoint excursion (EPE), maximal excursion (MXE), and directional control (DCL). Modified functional reach test (MFRT) and the sub-scales of physical functioning and role limitations due to physical health from the Short Form (36) Health Survey (SF-36) were used to identify changes in functional activities.
Results
After EAW training, seated balance significantly improved in total-direction EPE and MXE (P < 0.01 and P < 0.017 respectively). The results of MFRT and sub-scales of physical functioning and role limitations due to physical health improved after EAW training but were not statistically significant.
Conclusions
EAW training may have the potential to improve seated balance for persons with chronic motor complete SCI. Due to the limitations of the study, such as small sample size and lack of a control group, further studies are needed to clarify the effect of improving seated balance through EAW training.
Similar content being viewed by others
Introduction
Paralysis from traumatic spinal cord injury (SCI) results in abrupt changes in lifestyle and mobility. Depending on the neurological level and completeness of SCI, those with more severe SCI may lose neuromuscular control of upper extremities, trunk, and/or lower extremities resulting in loss of the ability to sit, stand and walk, necessitating the use of a wheelchair for mobility. As such, persons with SCI need to perform almost all daily functional activities, such as dressing, transferring, and mobility in the sitting position. For individuals who do not have full control and activation of the entire trunk musculature, they need to re-learn how to control any spared innervated muscles to maintain sitting balance and avoid falling over. This involves compensatory patterns of muscle activation involving muscles not normally used for postural support [1,2,3]. As in standing, maintenance of safe and functional balance is essential while seated [1]. Without good static and dynamic sitting balance, wheelchair users have a high risk of a falling accident while manipulating their wheelchair and performing transfers [4]. Falls from wheelchairs during transfers can be associated with fracture and head injury, sometimes resulting in fatal injuries [5, 6]. In persons with SCI, poor sitting balance can limit independence for activities of daily living (ADLs) and further influence socialization and quality of life (QOL). Studies have shown that over time, people with chronic SCI have declining physical function and increased need for assistance in performing ADLs [7, 8].
Powered exoskeletal systems to assist with overground walking provide a mobility option and may have potential therapeutic value for persons with SCI. Mastering use of a powered exoskeleton for walking requires training of static and dynamic balance skills, particularly in controlling forward and lateral posture excursions while in an upright and dynamic position [9]. While walking in an exoskeleton, persons with SCI stand upright, control weight shifting, and walk with a walker or crutches. A few studies suggested that postural perturbations which occur during exoskeletal-assisted walking (EAW) in persons with SCI could result in better balance [10,11,12]. However, those study results were either from persons with SCI who had walking ability or a very small sample size. The effects of EAW on improving seated balance for individuals with motor complete SCI still needs to be further studied. The purpose of this study was to determine if seated balance could be improved in persons with motor complete SCI who received EAW training. In addition to previously reported positive benefits of EAW such as reducing spasticity and improving bowel function [13,14,15,16,17], the results of this study could provide an additional benefit for using EAW.
Methods
Participants
The study was approved by the James J. Peters VA Medical Center Institutional Review Board. Participants were recruited from a database of our previous study participants who provided written authorization to be contacted for future study considerations. All the participants provided informed consent before the testing protocol started. Persons who were over 18 years with chronic SCI (more than 1-year post injury) and used a wheelchair for indoor and outdoor mobility were recruited for screening. If the persons with SCI had existing pressure ulcers on the area contacting with the device, severe spasticity (Modified Ashworth Scale = 4), significant contractures, pregnancy, psychiatric or cognitive situations that may interfere with consent or training process, total hip bone mineral density (BMD) T-scores less than −3.5, knee BMD less than 0.6 gm/cm2, or concurrent medical diseases that would be exclusionary for standing, they were excluded from participating in this study. Able-body participants who were over 18 years with normal walking function without joint contractures were recruited for seated balance testing as a healthy comparative group to set directional references for the results of seated balance tests.
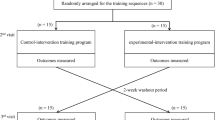
Study design
An initial pilot study with pre- and post-test design was conducted to determine efficacy for mobility skills using the ReWalkTM. Early on during this pilot study, it was observed by the trainers and reported by the participants that seated balance may be improved. As such, an amendment was added to use computerized seated posturography to measure seated balance changes after EAW training. Participants received supervised EAW training using a ReWalkTM. The ReWalkTM is a lower extremity powered exoskeleton which has a computerized control system with motors to power the hip and knee joints and through which coordinated joint motion is triggered by a user’s voluntary control of body movement [15]. Participants used their trunk and core musculature to perform weight shifting diagonally from side to side to trigger the device for exoskeleton walking.
EAW training included 3–4 sessions (4–6 h) per week. The training protocol by Asselin et al. was developed while conducting this study [9]. EAW training sessions included device donning and doffing, sit-to-stand and stand-to-sit, standing weight shifting balance skills, balancing with one crutch on each arm, coordinated crutch/walker timing, appropriate weight shifting during walking, and stopping [9]. In the device donning and doffing process, participants needed to learn how to transfer from their wheelchairs into the ReWalkTM device. Once participants sat in the device, they kept seated balance and placed their feet in the shoes and secured all the device leg and pelvic band straps. The trainer provided assistance as needed. While performing the sit-to-stand maneuver, participants learned to position the crutch tips posteriorly to their hips, lean forward, and use the crutches to push their body anteriorly so their feet would become loaded as the device stood them up. Once standing, balance exercises using the crutches to maintain static and dynamic balance would be the next stage of training. Participants needed to learn how to shift weight laterally to fully load one foot and unweight the other, which is an important skill while walking. While walking with the ReWalkTM, participants repeated diagonal (lateral and forward) weight shifting movement from side to side combined with controlling the crutches to keep balance. Last, participants practiced stopping which is performed by maintaining their balance point so that the swing leg would catch the ground causing the device to stop movement and return to standing. In the beginning of the walking training, the trainer provided any needed balance support to help participants walk with the ReWalkTM and corrected the amount, direction, and timing of weight shifting. Trainers progressively reduced the assistance as tolerated until unassisted EAW was achieved. As participants progressed, ReWalk system parameters were adjusted according to the specific walking progression for the EAW device in order to obtain improved walking speeds. Other mobility training was added to the walking training program when possible, including 90, 180, and 360 degree turns, navigating to rest on a wall, and walking outdoor and up and down a ramp. The training goals were to reach independent walking with the ReWalkTM and perform certain mobility skills.
Outcome measurement
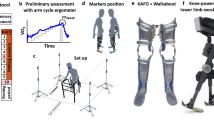
The training period was defined as the duration from the date of first EAW session to the date of the last EAW session. Seated balance was measured before and after EAW training by assessment of seated limits of stability (LOS) using computerized dynamic posturography (SMART EquiTest, Natus®) (Fig. 1) and modified functional reach test (MFRT) (Fig. 2) [18]. The SMART EquiTest system provides an objective measure of balance and postural stability in persons with a history of falls, vestibular disorders and other neurological and musculoskeletal conditions [19, 20]. Our previous study provided evidence that the seated dynamic posturography system could provide an accurate and sensitive evaluation tool to test seated balance for persons with paraplegia [21]. The LOS test quantifies the maximum distance a person can intentionally displace their center of pressure (COP). Participants sat on a cushioned block with back unsupported and arms crossed over the clavicles. While seated, participants were asked to move the avatar (which represented their COP) by leaning their upper body to targets on a computer screen and to maintain their stability on the targets for 1 s (Fig. 1). The targets on the screen were distributed in four cardinal directions (front, right, back, and left) and four diagonal directions (front right, back right, back left, front left). The LOS parameters of endpoint excursion (EPE), maximal excursion (MXE), and directional control (DCL) were used to quantify participants’ ability to intentionally displace their COP to the stability limits without losing balance. EPE is the distance of participants’ first movement toward the designated target, expressed as a percentage of maximum LOS distance. MXE is the maximum distance achieved during the trial of LOS testing, also expressed as a percentage of maximum LOS distance. DCL is a comparison of the amount of movement in the intended direction toward the target to the amount of extraneous movement away from the target. Increases of the three outcomes mean that participants could move further towards the target and with more postural control, indicating improvement of seated balance. For MFRT, the participant was positioned to sit on a mat table with a yardstick at the level of the acromion (Fig. 2). The participant’s feet were supported on the ground. The initial position was set with the participant’s single shoulder flexed to 90 degrees in the seated resting position. The ulnar styloid process was the anatomical landmark used to measure a reach. Then, the participant was asked to reach forward as far as possible without rotation of the trunk while a research team member guarded the participant on one side for safety concerns. The test-retest reliability of the MFRT is high, ranging from 0.85 to 0.94 [18]. Previous studies have also shown that MFRT has adequate correlation with other balance tests, such as Berg Balance Scale and Time Up and Go Test (validity) [22, 23]. In both the pre- and post-training evaluations, the LOS test and MFRT were repeated three times and averaged as each participant’s final results. The sub-scales of “Physical Functioning” and “Role Limitations due to Physical Health” from the Short Form (36 Health Survey (SF-36) [24] were also administered pre- and after-EAW training to see if participants had any physical functioning change after training.
Statistical analysis
For this pilot study, descriptive statistics were calculated and reported for the demographic data and each participant’s seated balance outcome measures. Due to the small sample size, skewed distributions with medians and ranges were reported. In order to prevent multiple comparisons which would lead to inflation of type I errors, the total-direction EPE, MXE, and DCL were used as the primary outcomes. The total-direction EPE, MXE, and DCL were defined as the average of the 8 directional EPE, MXE, and DCL respectively. Wilcoxon-signed ranks tests were used to compare differences in seated balance outcomes and physical health components of SF-36 between pre- and post-EAW (ReWalkTM) training. Spearman rank correlation (rho) was used to test if the seated balance changes (the changes of total-direction EPE, MXE, and DCL) were related to the EAW training period. Correlation rho values of 0.1, 0.3, and 0.5 were identified as small, medium, and large effect sizes, respectively [25]. The level of significance was set at 0.017 due to using Bonferroni correction for the comparisons of three major outcomes (P = 0.05/3). All statistical analyses were performed in SPSS 22.0 software.
Results
Participants
Eight persons with SCI participated in the study for EAW training and seated balance tests (Table 1). All 8 participants had chronic motor complete SCI. Seven able-bodied participants (6 males and 1 female) joined in the study for seated balance tests only as a healthy comparative group. Their median age was 32 years (range from 23 to 61 years).
Computerized dynamic posturography seated balance test results
The participants finished a median of 30 sessions of EAW training (range from 7 to 90 sessions) within a median 111 days (range from 87 to 210 days). Because a different number of training sessions were needed by different participants to achieve independent walking using the ReWalkTM and certain mobility skills, the number of finished EAW sessions varied among the participants. The majority of participants had improvement in their seated balance tests after EAW training (Fig. 3 and supplementary material), with significant increases in total-direction EPE and MXE (P = 0.008 and 0.016 respectively, Table 2). If the change in each direction is further explored, the participants demonstrated statistically non-significant improvements in EPE, MXE, and DCL in most of the eight directions (Fig. 4). Back EPE (median = 20%, range from −15 to 66%, P = 0.04), front and back-left MXE (median = 22%, range from −4 to 58%, P = 0.03; median = 9%, range from −11 to 23%, P = 0.06), and right DCL (median = 13%, range from −4 to 39%, P = 0.03) (Fig. 4) had the greatest amount of improvement. These increases were toward the values measured in the healthy comparative group (Fig. 4). The increases of EPE, MXE, and DCL indicate that participants can move their COP with larger excursion (EPE and MXE) and better directional control (DCL) after ReWalk training.
The Spearman correlation coefficients (rho) between total-direction EPE, MXE, and DCL changes and EAW training period were 0.04 (P = 0.93), 0.28 (P = 0.51), and 0.56 (P = 0.15) respectively. Although the correlation between change of each LOS parameter and EAW training period was not statistically significant, DCL change and EAW training period had a positive correlation with large effect size. Longer EAW training may have a trend to increase directional control of seated balance.
Results of MFRT and sub-scales of physical functioning and role limitations due to physical health from the SF-36
Five out of the eight participants finished the pre- and post-training MFRTs. Because the seated balance outcomes were added as an amendment to the existing pilot project, some participants didn’t finish pre- and post-MFRT. After EAW training, MFRT results in the five of eight participants showed a slight increase but did not reach significant differences compared to before training (P = 0.44, Table 2). All eight participants completed the subscales of physical functioning and role limitations due to physical health form SF-36. After EAW training, participants showed improvements in the subscales of physical functioning but not role limitations due to physical health on the SF-36 (P = 0.04 and P = 0.20 respectively, Table 2).
Discussion
The effects of ReWalk EAW training on improving seated balance for people with motor complete SCI are reported from this study. After ReWalk EAW training, participants demonstrated better control of trunk movement by moving their COP excursion further (increased EPE and MXE) with decreased COP deviation from the intended direction (increased DCL). A previous case report study [10] (N = 3) using a different research design and exoskeleton device, Ekso, showed similar results of improving seated balance after EAW training compared to treadmill-based robotic gait training. In another study, it was reported that after an 8-week EAW training (3 times per week) using the Ekso for individuals with SCI, the participants who had walking ability without using the Ekso had significant improvements on the results of Berg Balance Scale and Time Up and Go Test [11]. The study participants also had significant improvement on the score of “Use of Toilet” in the Spinal Cord Independence Measure, which implied the improvement of balance after the EAW training [12]. Using a different power exoskeleton device, ReWalk, and a different population, our current study provided further evidence to support the benefit of EAW training on improving seated balance.
During EAW training using ReWalkTM, users consistently needed to control their trunk to have an appropriate amount of weight shifting to trigger the power exoskeleton to take steps and manipulate two crutches for moving forward. Trunk movement with proper timing is also needed for the purpose of intentional stopping of walking. Other EAW skills, including turning, pivoting, and walking on uneven surfaces, all stimulate the existing innervated trunk muscles. A previous surface electromyography study had shown that overground EAW triggered by lateral weight shifting and trunk movement combined with manipulating a walker or crutches for moving forward could activate more trunk muscles, especially erector spinae, compared to Lokomat-assisted treadmill walking and have the potential for users to develop a new postural control strategy [26]. The trunk sagittal plane movement with more activation of erector spinae during overground EAW may lead to greater improvement on front-back direction of seated balance as shown in our current study (Fig. 4). All participants had chronic motor complete SCI and they improved seated balance after EAW training. This seated balance improvement suggests that existing trunk neurological signals appear to be strengthened.
This study was not originally intended to show that EAW could specifically train seated balance for persons with SCI. Rather, if EAW is being used as a therapeutic modality for mobility, recovery of walking, or as an activity-based exercise program, then improvement in seated balance may also be anticipated. Our participants showed significant improvement in seated balance after ReWalk EAW training. Although not statistically significant, participants showed a trend toward improvement in reaching ability and improved their perception of physical function in daily activities and work. Improvements in seated balance may translate to better seated safety and more independence for wheelchair users with SCI [27]. While ADL data was not collected in these studies, participants mentioned and commented on their ability to perform certain ADLs more easily such as putting on pants and reaching to open doors. A future study to determine if seated balance improvements from EAW are associated with ADL improvements would be indicated.
Even though EAW training appears to have some potential physiological, health-related and QOL benefits, such as reducing pain and spasticity and improving bowel function [13,14,15,16,17], plus improving seated balance as shown in this study, most persons with SCI will continue to use the wheelchair as the primary mode for mobility. Present day powered EAW devices are not technologically developed to the point of replacing the wheelchair because overground speed remains too slow for community ambulation of any distance. The fastest walking speeds in these EAW devices are about 1.0–1.5 mph (range from 0.45 to 0.67 m/s) [28,29,30]. The normal walking pace for a healthy, uninjured ambulatory adult is about 3.1 mph (1.39 m/s) [31,32,33,34]. A velocity of 1.0–1.5 mph is often too slow for covering distances in modern, fast-paced society, such as crossing a street. As such, wheelchairs are not likely to be replaced by exoskeletons any time soon. Therefore, with the current powered exoskeleton technology, persons with SCI may continue to use the wheelchair as the primary mode of mobility and seated balance will remain a critical component to successful and safe wheelchair use.
This study has several limitations. The small sample size may lower the study power and generalizability. The study mostly used biomechanical tests (tracking COP change) to determine the changes of seated balance, rather than directly measuring activities of daily living requiring seated balance function. MFRT and SF-36 may not be sensitive enough to reflect improvement of seated balance in functional activities [21, 35]. The study could not provide enough evidence to show that seated balance changes detected in the biomechanical tests may be able to translate to functional sitting performance. However, several studies have shown that COP measures could be more sensitive to detecting postural control changes [21, 36, 37]. Learning effects while performing LOS tests may slightly influence the results of pre- and post-training comparisons. The duration between baseline and post-training tests was about four months, which should have been enough time to wash out any learning effect for the LOS tests. The study was not designed to have a SCI control group who received standard of care of physical therapy as a comparison, as such we do not know if the seated balance improvement from EAW training is more effective than standard physical therapy care. The purpose of the study was to explore another benefit of EAW training, not to compare the effects between EAW and physical therapy. A future study with a larger sample size, different seated balance evaluation tools, including biomechanical analysis and functional outcomes, and a standard of care control group, is necessary to clarify the effect of improving seated balance through EAW training.
In conclusion, the study results indicated that EAW training may improve seated balance for participants with chronic motor complete SCI. The study provides another potential benefit of using EAW training which may be translated to use in clinics or for those who have EAW devices for personal use. This information could help clinicians design a more efficient EAW training program for people with SCI.
References
Boswell-Ruys CL, Sturnieks DL, Harvey LA, Sherrington C, Middleton JW, Lord SR. Validity and reliability of assessment tools for measuring unsupported sitting in people with a spinal cord injury. Arch Phys Med Rehabil. 2009;90:1571–7.
Seelen H, Potten Y, Drukker J, Reulen J, Pons C. Development of new muscle synergies in postural control in spinal cord injured subjects. J Electromyogr Kinesiol. 1998;8:23–34.
Seelen H, Vuurman E. Compensatory muscle activity for sitting posture during upper extremity task performance in paraplegic persons. Scand J Rehabil Med. 1990;23:89–96.
Fattal C, Mariano-Goulart D, Thomas E, Rouays-Mabit H, Verollet C, Maimoun L. Osteoporosis in persons with spinal cord injury: the need for a targeted therapeutic education. Arch Phys Med Rehabil. 2011;92:59–67.
Kirby RL, Ackroyd-Stolarz SA, Brown MG, Kirkland SA, MacLeod DA. Wheelchair-related accidents caused by tips and falls among noninstitutionalized users of manually propelled wheelchairs in Nova Scotia. Am J Phys Med Rehabil. 1994;73:319–30.
Calder CJ, Kirby RL. Fatal wheelchair-related accidents in the United States. Am J Phys Med Rehabil. 1990;69:184–90.
Gerhart KA, Bergstrom E, Charlifue SW, Menter RR, Whiteneck GG. Long-term spinal cord injury: functional changes over time. Arch Phys Med Rehabil. 1993;74:1030–4.
Thompson L. Functional changes in persons aging with spinal cord injury. Assistive Technol. 1999;11:123–9.
Asselin PK, Avedissian M, Knezevic S, Kornfeld S, Spungen AM. Training Persons with Spinal Cord Injury to Ambulate Using a Powered Exoskeleton. J Vis Exp. 2016:54071.
Chisholm AE, Alamro RA, Williams AMM, Lam T. Overground vs. treadmill-based robotic gait training to improve seated balance in people with motor-complete spinal cord injury: a case report. J Neuroeng Rehabil. 2017;14:27.
Bach Baunsgaard C, Vig Nissen U, Katrin Brust A, Frotzler A, Ribeill C, Kalke Y-B, et al. Gait training after spinal cord injury: safety, feasibility and gait function following 8 weeks of training with the exoskeletons from Ekso Bionics. Spinal Cord. 2018;56:106–16.
Baunsgaard CB, Nissen UV, Brust AK, Frotzler A, Ribeill C, Kalke YB, et al. Exoskeleton gait training after spinal cord injury: an exploratory study on secondary health conditions. J Rehabil Med. 2018;50:806–13.
Platz T, Gillner A, Borgwaldt N, Kroll S, Roschka S. Device-training for individuals with thoracic and lumbar spinal cord injury using a powered exoskeleton for technically assisted mobility: achievements and user satisfaction. BioMed Res Int. 2016;2016:8459018.
Mekki M, Delgado AD, Fry A, Putrino D, Huang V. Robotic Rehabilitation and Spinal Cord Injury: a Narrative Review. Neurotherapeutics. Neurotherapeutics. 2018;15:604–17.
Esquenazi A, Talaty M, Packel A, Saulino M. The ReWalk powered exoskeleton to restore ambulatory function to individuals with thoracic-level motor-complete spinal cord injury. Am J Phys Med Rehabil. 2012;91:911–21.
Stampacchia G, Rustici A, Bigazzi S, Gerini A, Tombini T, Mazzoleni S. Walking with a powered robotic exoskeleton: subjective experience, spasticity and pain in spinal cord injured persons. NeuroRehabilitation. 2016;39:277–83.
Kozlowski AJ, Bryce TN, Dijkers MP. Time and effort required by persons with spinal cord injury to learn to use a powered exoskeleton for assisted walking. Top Spinal Cord Inj Rehabil. 2015;21:110–21.
Lynch SM, Leahy P, Barker SP. Reliability of measurements obtained with a modified functional reach test in subjects with spinal cord injury. Phys Ther. 1998;78:128–33.
Furman JM. Role of posturography in the management of vestibular patients. Otolaryngol–Head Neck Surg. 1995;112:8–15.
Visser JE, Carpenter MG, van der Kooij H, Bloem BR. The clinical utility of posturography. Clin Neurophysiol. 2008;119:2424–36.
Harel NY, Asselin PK, Fineberg DB, Pisano TJ, Bauman WA, Spungen AM. Adaptation of computerized posturography to assess seated balance in persons with spinal cord injury. J Spinal Cord Med. 2013;36:127–33.
Bennie S, Bruner K, Dizon A, Fritz H, Goodman B, Peterson S. Measurements of balance: comparison of the timed “up and go” test and functional reach test with the berg balance scale. J Phys Ther Sci. 2003;15:93–7.
Katz-Leurer M, Fisher I, Neeb M, Schwartz I, Carmeli E. Reliability and validity of the modified functional reach test at the sub-acute stage post-stroke. Disabil Rehabil. 2009;31:243–8.
Forchheimer M, McAweeney M, Tate DG. Use of the SF-36 among persons with spinal cord injury. Am J Phys Med Rehabil. 2004;83:390–5.
Cohen J. A power primer. Psychol Bull. 1992;112:155–9.
Alamro RA, Chisholm AE, Williams AMM, Carpenter MG, Lam T. Overground walking with a robotic exoskeleton elicits trunk muscle activity in people with high-thoracic motor-complete spinal cord injury. J Neuroeng Rehabil. 2018;15:109.
Pandey V, Nigam V, Goyal TD, Chhabra H. Care of post-traumatic spinal cord injury patients in India: an analysis. Indian J Orthop. 2007;41:295–9.
Yang A, Asselin P, Knezevic S, Kornfeld S, Spungen AM. Assessment of in-hospital walking velocity and level of assistance in a powered exoskeleton in persons with spinal cord injury. Top Spinal Cord Inj Rehabil. 2015;21:100–9.
Kozlowski A, Bryce T, Dijkers M. Time and effort required by persons with spinal cord injury to learn to use a powered exoskeleton for assisted walking. topics in spinal cord injury. Rehabilitation. 2015;21:110–21.
Hartigan C, Kandilakis C, Dalley S, Clausen M, Wilson E, Morrison S, et al. Mobility outcomes following five training sessions with a powered exoskeleton. Top Spinal Cord Inj Rehabil. 2015;21:93–9.
Aspelin K. Establishing pedestrian walking speeds. Ontario, CA: Institute of Transportation Engineerings (ITE) District 6 Mid-Year Board Meeting; 2005.
Browning RC, Baker EA, Herron JA, Kram R. Effects of obesity and sex on the energetic cost and preferred speed of walking. J Appl Physiol. 2006;100:390–8.
Mohler BJ, Thompson WB, Creem-Regehr SH, Pick HL Jr, Warren WH Jr. Visual flow influences gait transition speed and preferred walking speed. Exp Brain Res. 2007;181:221–8.
Levine RV, Norenzayan A. The pace of life in 31 countries. J Cross Cultural Psychol. 1999;30:178–205.
Lin MR, Hwang HF, Chen CY, Chiu WT. Comparisons of the brief form of the World Health Organization Quality of Life and Short Form-36 for persons with spinal cord injuries. Am J Phys Med Rehabil. 2007;86:104–13.
Pajala S, Era P, Koskenvuo M, Kaprio J, Tormakangas T, Rantanen T. Force platform balance measures as predictors of indoor and outdoor falls in community-dwelling women aged 63-76 years. J Gerontol Ser A, Biol Sci Med Sci. 2008;63:171–8.
Tse CM, Chisholm AE, Lam T, Eng JJ, Team SR. A systematic review of the effectiveness of task-specific rehabilitation interventions for improving independent sitting and standing function in spinal cord injury. J Spinal Cord Med. 2018;41:254–66.
Acknowledgements
The study was made possible in part by the financial support provided by the VA RR&D National Center for the Medical Consequences of Spinal Cord Injury (VA RR&D #B9212C). This study is registered on clinicaltrials.gov (NCT01454570).
Author information
Authors and Affiliations
Contributions
All authors listed above have met all the following authorship criteria: 1. Conceived and/or designed the work that led to the submission, acquired data, and/or played an important role in interpreting the results. 2. Drafted or revised the manuscript. 3. Approved the final version. 4. Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Tsai, CY., Asselin, P.K., Hong, E. et al. Exoskeletal-assisted walking may improve seated balance in persons with chronic spinal cord injury: a pilot study. Spinal Cord Ser Cases 7, 20 (2021). https://doi.org/10.1038/s41394-021-00384-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00384-8