Abstract
Introduction
Atypical hangman’s fractures are coronally-oriented vertical fractures of the posterior body of C2. Though these are not uncommon injuries, there is a paucity of data investigating the management of these fractures, especially when they occur in association with subaxial fracture dislocations.
Case presentation
A 50-year-old male suffered a cervical extension injury when he dove into a shallow swimming pool while intoxicated. Initial examination demonstrated 2/5 strength in the right deltoid and biceps and 3/5 strength in the left deltoid and biceps with no motor or sensory function distal to the C5 level. Cervical CT scan revealed a C2 atypical hangman’s fracture and a C4 right-sided facet fracture with traumatic spondylolisthesis at C4/5. We performed C2–C5 anterior cervical discectomy and fusion followed by a C3–C5 posterior instrumented fusion. At the patient’s two year postoperative visit, the patient has had minimal improvement in neurologic function with 4/5 strength in bilateral deltoids and biceps and 2/5 strength in right wrist extension. Radiographs show a solid arthrodesis on flexion–extension radiographs.
Discussion
To our knowledge, this is the first case report discussing the operative management of an atypical hangman’s fracture with a concomitant subaxial fracture–dislocation. This case report adds to our current knowledge by demonstrating a novel anterior–posterior approach for treating these complicated injuries.
Similar content being viewed by others
Introduction
The hangman’s fracture is a classic cervical spine injury, which is universally recognizable as a bilateral fracture through the C2 pars and in higher degrees of injury, there is resultant anterior subluxation of the C2/3 segment [1]. Conversely, atypical hangman’s fractures are coronally-oriented vertical fractures of the posterior body of C2. Though these are not uncommon injuries, there is a paucity of data investigating the management of these fractures, especially in comparison to the more typical C2 fractures. At present, only six small case series have recognized atypical hangman’s fractures as a distinct entity [2,3,4,5,6,7], though other authors have acknowledged this fracture pattern as a subtype of miscellaneous axis body fractures [8, 9]. Upon closer scrutiny, only three of the aforementioned studies discuss operative management of atypical hangman’s fractures, each reporting on just one operative case [2, 7, 10]. No specific guidelines exist regarding the appropriate management of atypical hangman fractures; however, multiple authors have recommended that typical traumatic spondylolisthesis classification systems be utilized to guide decision-making [6, 7]. As such, the majority of atypical hangman’s fractures are managed nonoperatively. Indications for surgical intervention include new incomplete neurologic deficits or concomitant subaxial cervical injuries that confer mechanical instability. At present, there are no reports in the literature of atypical hangman’s fractures with an associated subaxial fracture–dislocation managed operatively. Many would consider this fracture pattern to be most amenable to a posterior approach with fusion from C1 to a level inferior to the subaxial fracture. Despite the instability of a hangman’s fracture being directed to the C2/3 segment, extension to the C1 level is necessary to compensate for the loss or compromise of the typical posterior fixation points at C2. In this case report, we describe a unique motion-preserving approach to an atypical hangman’s fracture with an associated unilateral vertebral artery injury (VAI) and C4 facet fracture–dislocation managed operatively with a C2–C5 fusion via a combined anterior–posterior approach.
Case presentation
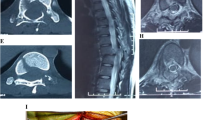
A 50-year-old male suffered a cervical extension injury when he dove into a shallow swimming pool while intoxicated. He was noted to be quadriplegic immediately following the injury. He was transported to an outside facility where he was evaluated. Cervical CT scan was performed and revealed a C2 atypical hangman’s fracture (Fig. 1), C3 right-sided uncinate process fracture, and C4 right-sided facet fracture (Fig. 2) with traumatic spondylolisthesis at C4/5 (Fig. 3) and anterior epidural hematoma extending from the craniocervical junction to the level of C4. He was immobilized in an extrication collar and transferred to a Level 1 Trauma center for further treatment of his spinal cord injury.
Following transport, initial examination demonstrated 2/5 strength in the right deltoid and biceps and 3/5 strength in the left deltoid and biceps with no motor or sensory function distal to the C5 level. Based upon these findings, he was classified as a C5 ASIA A spinal cord injury. Due to the mechanism of injury, a CT angiogram was obtained, which demonstrated a right-sided VAI at C3–C4 with attenuation cephalad to the level of the C2 transverse foramen and a left-dominant vertebral artery with a patent Circle of Willis (Fig. 4). An MRI of the cervical spine was obtained and demonstrated cord contusion from C3 to C6, epidural hematoma from C2 to C5, segmental three column osseoligamentous injuries centered at C2–C3 and C4–C5, and right-sided C4 facet fracture with traumatic anterolisthesis at C4–C5 (Figs. 5, 6). Given the unstable fracture–dislocation at C4–5, epidural hematoma with cord compression, and atypical hangman’s fracture, the decision was made to proceed with emergent surgical decompression and stabilization. Once the patient was positioned supine with Gardner-Wells tongs in place, traction was added sequentially to a total of 20 pounds, which reduced the spondylolisthesis at C4–C5. Given this patient’s concomitant C2 atypical hangman’s fracture and C4–C5 fracture–dislocation, we performed C2–C5 anterior cervical discectomy and fusion (ACDF) followed by a C3–C5 posterior instrumented fusion (Figs. 7, 8). The patient tolerated the procedure without intraoperative complications.
Postoperatively, the patient was transferred to the ICU in stable condition wearing a hard cervical collar. Immediately postoperatively, the patient was noted to have a slight improvement in his physical exam with 4/5 strength in the left deltoid and biceps and 3/5 strength in the right deltoid and biceps but no motor or sensory activity distal to the C5 level. The patient had an uneventful hospital course and was discharged to a spine rehabilitation hospital on postoperative day 11.
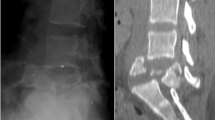
The patient’s postoperative course was complicated by dysphagia requiring temporary placement of a feeding tube, which was removed at 3 weeks postoperatively. At 8 weeks postoperatively, he was weaned out of his cervical collar. He also experienced delayed posterior wound healing, though this resolved completely without intervention by 10 weeks postoperatively. Following discharge from rehabilitation, the patient had a urinary tract infection in the setting of an indwelling urinary catheter required for neurogenic bladder which was treated with antibiotics. At the patient’s 2 year postoperative visit, the patient has had minimal improvement in neurologic function with 4/5 strength in bilateral deltoids and biceps and 2/5 strength in right wrist extension. Radiographs show a solid arthrodesis on flexion–extension radiographs at C2–5 and healing of the C2 fracture with evidence of adjacent segment degeneration at C5–6 (Figs. 9, 10).
Discussion
Atypical hangman’s fractures are coronally-oriented fractures of the posterior vertebral body of C2 that most frequently occur via a hyperextension mechanism. Due to their shared mechanism of injury, these fractures are commonly associated with VAI and other concomitant subaxial cervical spine injuries. Unlike typical hangman’s fractures, these atypical fractures have been theorized to result in higher rates of spinal cord injury because the fracture pattern does not result in disruption of the ring of C2, preventing spontaneous decompression of the spinal cord via anteroposterior widening of the canal [7].
The appropriate management of atypical hangman’s fractures has not been thoroughly investigated. Like typical hangman’s fractures, a few small case series have demonstrated that atypical hangman’s fractures are amenable to nonoperative treatment when following the same criteria for surgical intervention [3, 5, 11]. Only four studies have reported cases of atypical hangman’s fractures treated operatively, and none of the patients in these small case series had an associated subaxial fracture [2, 7, 10, 12]. In their series, Starr and Eismont reported good outcomes for six patients with atypical hangman’s fractures, five of which were treated with a halo, and one of which underwent posterior fusion from occiput to C3 [7]. Rainov et al. published a case report in which a patient with an atypical hangman’s fracture underwent C2–C3 ACDF with a hydroxyapatite inlay and anterior locking plate, followed by C2 bilateral dorsal transpedicular screw fixation [10]. The authors report that the patient did not experience any perioperative morbidity and achieved a stable bony fusion. Al-Mahfoudh et al. described a patient with an atypical hangman’s fracture that was treated operatively with C1–C3 posterior cervical fusion; however, the authors did not provide any information regarding the radiographic, clinical, or fusion outcomes [2]. More recently, Li et al. retrospectively reviewed a series of 46 patients with isolated atypical hangman’s fractures, 27 of whom underwent surgical treatment [12]. Of the 27 operative cases, 20 patients with standard pedicle and vertebral artery anatomy underwent a posterior approach with a C2–C3 lag-screw rod fixation technique, four patients with atypical vertebral artery anatomy or small C2 pedicles underwent a posterior approach with C1–C3 arthrodesis, one patient with a disc herniation underwent a one-level C2/3 ACDF, and two patients underwent a combined anterior and posterior approach. The authors reported that all operative and conservatively managed patients achieved solid bony fusion, an improvement in neck pain, and no evidence of neurologic deterioration. Each of the aforementioned studies discusses the operative management of isolated atypical hangman’s fractures; no case reports exist discussing the management of this fracture with a concomitant subaxial fracture–dislocation.
In addition to his atypical hangman’s fracture, our patient suffered a unilateral VAI. It has been estimated that 70–78% of VAI’s occur in the presence of cervical spine fracture [13,14,15], and conversely VAI may occur in up to 39% of cervical spine fractures [14, 16,17,18]. Though clinical symptoms of VAI may be present in some patients [19], a significant proportion of patients are initially asymptomatic [14, 20, 21]. In a study by Cothren et al. investigating a screening program for blunt cervical vascular injury (BCVI), 317 asymptomatic patients underwent screening angiography on the basis of cervical fracture pattern and 37% were discovered to have BCVI [20]. Current recommendations call for asymptomatic patients with risk factors for VAI to undergo screening to allow early treatment before the onset of neurological sequelae [22]. Digital subtraction angiography (DSA) has historically been considered the gold standard screening modality [13, 23], but the advent of higher resolution CT has led to sensitivity similar to DSA [13, 24, 25], and allows for concurrent imaging of other injuries, making CT angiography the modality of choice when screening for VAI. When a VAI is discovered, antithrombotic therapy should be initiated to reduce mortality and neurologic morbidity [17, 23, 26,27,28]. Level one studies have yet to elucidate a significant difference between the use of antiplatelets and anticoagulants [26, 28]. Endovascular and surgical treatments are reserved for high grade or progressing injuries. Our patient demonstrated complete occlusion of his right vertebral artery with distal reconstitution via muscular collaterals and a patent dominant left vertebral artery. His VAI was treated with heparin for 2 weeks followed by enoxaparin for an additional 6 weeks with no new neurologic sequelae.
Subaxial cervical spine injuries were traditionally classified according to Allen’s Classification, which is a comprehensive classification based on the mechanism of injury as assessed on plan radiographs [29]. However, many surgeons found this classification to be excessively exhaustive and to lack inter-observer variability [30]. In 2007, the Spine Trauma Study Group published the Subaxial Injury Classification, which classified injuries caudal to the level of the axis according to injury morphology, integrity of the posterior ligamentous complex (PLC), and severity of neurologic deficit [31]. More recently, the AOSpine Knowledge Forum published their classification of subaxial cervical spine injuries based on mechanism of injury with additional modifiers based on detailed review of advanced imaging [32]. Our patient suffered a C4 facet fracture with traumatic spondylolisthesis. Facet fracture–dislocation is caused by flexion and distraction forces, with or without an element of rotation. Allen and Ferguson categorized these injuries in the flexion-distraction phylogeny and assigned them varying levels of severity based on facet involvement and degree of spondylolisthesis [29]. As was performed in our patient, definitive management of facet dislocation begins with a closed reduction with skull traction, recognizing the risks of disk herniation. Typically, this reduction is performed in an awake patient so that neurologic monitoring can be performed; however, in our patient with a complete spinal cord injury and a pre-reduction MRI demonstrating no disk herniation posteriorly, a reduction under general anesthesia could be reasonably performed. Traditionally, posterior stabilization is then performed in order to restore the posterior tension band that is lost due to disruption of the PLC [33, 34]. In our patient, posterior alone cervical fusion would have required instrumentation from C1 to C5, leading to loss of motion at the important atlantoaxial junction. By performing C2–C5 ACDF followed by C2–C3 posterior instrumented fusion, we were able to obtain anterior column support, stabilize the C2 atypical hangman’s fracture, and stabilize the C4 facet fracture–dislocation while sparing rotational motion at the atlantoaxial junction. Lastly, it is important to understand that the “atypical hangman’s fracture” described herein is not synonymous with the Type IIA fracture in the Levine and Edwards classification, which is a flexion-distraction injury that disrupts the annulus and posterior longitudinal ligament rendering the C2/3 segment unstable to longitudinal stress. Type IIA hangman fractures are specifically contraindicated for cervical traction as this can induce cord stretch and injury. The use of traction in the setting of an atypical hangman’s fracture is not explicitly contraindicated, but should be performed in a stepwise fashion with serial lateral fluoroscopy to insure there is no longitudinal distraction.
Atypical hangman’s fractures are challenging to treat when combined with subaxial cervical spine surgeries. To our knowledge, this is the first case report discussing the operative management of an atypical hangman’s fracture with a concomitant subaxial fracture–dislocation. This case report adds to our current knowledge by demonstrating a novel anterior–posterior approach for treating these complicated injuries.
References
Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Jt Surg Am. 1985;67:217–26.
Al-Mahfoudh R, Beagrie C, Woolley E, Zakaria R, Radon M, Clark S, et al. Management of typical and atypical hangman’s fractures. Glob Spine J. 2016;6:248–56.
Bohay D, Gosselin RA, Contreras DM. The vertical axis fracture: a report on three cases. J Orthop Trauma. 1992;6:416–9.
Burke JT, Harris JH Jr. Acute injuries of the axis vertebra. Skelet Radiol. 1989;18:335–46.
German JW, Hart BL, Benzel EC. Nonoperative management of vertical C2 body fractures. Neurosurgery. 2005;56:516–21.
Samaha C, Lazennec JY, Laporte C, Saillant G. Hangman’s fracture: the relationship between asymmetry and instability. J Bone Jt Surg Br. 2000;82:1046–52.
Starr JK, Eismont FJ. Atypical hangman’s fractures. Spine. 1993;18:1954–7.
Benzel EC. Conservative treatment of neural arch fractures of the axis: computed tomography scan and X-ray study on consolidation time. World Neurosurg. 2011;75:229–30.
Effendi B, Roy D, Cornish B, Dussault RG, Laurin CA. Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Jt Surg Br. 1981;63-b:319–27.
Rainov NG, Heidecke V, Burkert W. Coronally oriented vertical fracture of the axis body: surgical treatment of a rare condition. Minim Invasive Neurosurg. 1998;41:93–6.
Iizuka H, Shimizu T, Hasegawa W, Takagishi K. Fractures of the posterior part of the body and unilateral spinous process of the axis: a case report. Spine. 2001;26:E528–30.
Li G, Zhong D, Wang Q. A novel classification for atypical Hangman fractures and its application: a retrospective observational study. Medicine. 2017;96:e7492.
Biffl WL, Egglin T, Benedetto B, Gibbs F, Cioffi WG. Sixteen-slice computed tomographic angiography is a reliable noninvasive screening test for clinically significant blunt cerebrovascular injuries. J Trauma. 2006;60:745–51.
Biffl WL, Moore EE, Elliott JP, Ray C, Offner PJ, Franciose RJ, et al. The devastating potential of blunt vertebral arterial injuries. Ann Surg. 2000;231:672–81.
Cothren CC, Moore EE, Biffl WL, Ciesla DJ, Ray CE Jr, Johnson JL, et al. Cervical spine fracture patterns predictive of blunt vertebral artery injury. J Trauma. 2003;55:811–3.
Franz RW, Willette PA, Wood MJ, Wright ML, Hartman JF. A systematic review and meta-analysis of diagnostic screening criteria for blunt cerebrovascular injuries. J Am Coll Surg. 2012;214:313–27.
Miller PR, Fabian TC, Croce MA, Cagiannos C, Williams JS, Vang M, et al. Prospective screening for blunt cerebrovascular injuries: analysis of diagnostic modalities and outcomes. Ann Surg. 2002;236:386–93.
Wang AC, Charters MA, Thawani JP, Than KD, Sullivan SE, Graziano GP. Evaluating the use and utility of noninvasive angiography in diagnosing traumatic blunt cerebrovascular injury. J Trauma Acute Care Surg. 2012;72:1601–10.
Desouza RM, Crocker MJ, Haliasos N, Rennie A, Saxena A. Blunt traumatic vertebral artery injury: a clinical review. Eur Spine J. 2011;20:1405–16.
Cothren CC, Moore EE, Ray CE Jr, Johnson JL, Moore JB, Burch JM. Cervical spine fracture patterns mandating screening to rule out blunt cerebrovascular injury. Surgery. 2007;141:76–82.
Jacobson LE, Ziemba-Davis M, Herrera AJ. The limitations of using risk factors to screen for blunt cerebrovascular injuries: the harder you look, the more you find. World J Emerg Surg. 2015;10:46.
Lohrer L, Vieth V, Nassenstein I, Hartensuer R, Niederstadt T, Raschke MJ, et al. Blunt cerebrovascular injuries in acute trauma care: a screening protocol. Eur Spine J. 2012;21:837–43.
Cothren CC, Moore EE, Ray CE Jr, Ciesla DJ, Johnson JL, Moore JB, et al. Screening for blunt cerebrovascular injuries is cost-effective. Am J Surg. 2005;190:845–9.
Eastman AL, Chason DP, Perez CL, McAnulty AL, Minei JP. Computed tomographic angiography for the diagnosis of blunt cervical vascular injury: is it ready for primetime? J Trauma. 2006;60:925–9.
Paulus EM, Fabian TC, Savage SA, Zarzaur BL, Botta V, Dutton W, et al. Blunt cerebrovascular injury screening with 64-channel multidetector computed tomography: more slices finally cut it. J Trauma Acute Care Surg. 2014;76:279–83.
Cothren CC, Biffl WL, Moore EE, Kashuk JL, Johnson JL. Treatment for blunt cerebrovascular injuries: equivalence of anticoagulation and antiplatelet agents. Arch Surg. 2009;144:685–90.
Cothren CC, Moore EE, Biffl WL, Ciesla DJ, Ray CE Jr, Johnson JL, et al. Anticoagulation is the gold standard therapy for blunt carotid injuries to reduce stroke rate. Arch Surg. 2004;139:540–5.
Stein DM, Boswell S, Sliker CW, Lui FY, Scalea TM. Blunt cerebrovascular injuries: does treatment always matter? J Trauma. 2009;66:132–43.
Allen BL Jr, Ferguson RL, Lehmann TR, O’Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine. 1982;7:1–27.
Carter JW, Mirza SK, Tencer AF, Ching RP. Canal geometry changes associated with axial compressive cervical spine fracture. Spine. 2000;25:46–54.
Vaccaro AR, Hulbert RJ, Patel AA, Fisher C, Dvorak M, Lehman RA Jr, et al. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine. 2007;32:2365–74.
Vaccaro AR, Koerner JD, Radcliff KE, Oner FC, Reinhold M, Schnake KJ, et al. AOSpine subaxial cervical spine injury classification system. Eur Spine J. 2016;25:2173–84.
Do Koh Y, Lim TH, Won You J, Eck J, An HS. A biomechanical comparison of modern anterior and posterior plate fixation of the cervical spine. Spine. 2001;26:15–21.
Duggal N, Chamberlain RH, Park SC, Sonntag VK, Dickman CA, Crawford NR. Unilateral cervical facet dislocation: biomechanics of fixation. Spine. 2005;30:E164–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pinter, Z.W., Lawson, B.K., Freedman, B.A. et al. Atypical hangman’s fracture with concomitant subaxial fracture–dislocation treated with circumferential fusion of C2–C5—a case report. Spinal Cord Ser Cases 6, 108 (2020). https://doi.org/10.1038/s41394-020-00365-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-020-00365-3