Abstract
Introduction
Client-centered goal setting has multiple benefits in spinal rehabilitation. However, research has shown that many occupational therapists struggle to facilitate client-centered goal setting. South Africa presents unique challenges to client-centered goal setting, but no data is available on how it is applied.
Study design
A qualitative research design following an appreciative inquiry stance was used.
Objective
To explore how occupational therapists implement and envision the goal setting practices in spinal rehabilitation.
Setting
Rehabilitation facilities in Gauteng, South Africa.
Methods
A focus group consisting of five occupational therapists working within spinal rehabilitation was held. An appreciative inquiry stance was used to determine current successes and future ideas on how to implement goal setting in a spinal rehabilitation setting.
Results
Data was analysed thematically using Braun and Clark. Themes were developed under each phase of appreciative inquiry. Discovery phase: Participants felt that current effective goal setting is therapist-directed and that client insight facilitates effective goal setting. Dream phase: Participants agreed that client-centered goal setting is the ideal. In addition, effective collaboration within the team and adequate resources were identified during the dream phase as ideals to effective goal setting practices. Design and Destination phase: Participants generated ideas on how to improve on team collaboration during goal setting and how to ensure goal setting is client-centered for effective goal setting in spinal rehabilitation to take place.
Conclusions
The study emphasizes that for effective goal setting to occur, the process must remain client-centered. Essential to this process is collaboration between both the team and family members. Adequate resources and a low therapist-patient ratio supports effective goal setting.
Similar content being viewed by others
Introduction
Following a spinal cord injury (SCI), individuals receive multidisciplinary rehabilitation with the long term outcome of reintegration into the community [1,2,3]. The role of the occupational therapist (OT) is to enable the person with SCI to resume participation in their meaningful occupations such as work, activities of daily living and leisure [1, 4,5,6]. As a client centered healthcare profession, OTs respect that the person with SCI is the expert of their own lives and should determine which occupations are most meaningful to them [6, 7]. It is therefore essential that the individual is an active participant throughout the rehabilitation process, including the first step which is setting goals [6,7,8].
Wade defines goal setting as the formal procedure in which the rehabilitation team, client and family come together to discusses the most desirable outcomes of therapy [8]. The first step is to determine the most desirable outcome for the client. Achieving goals during rehabilitation is always more successful if the client considers the goals to be important [4, 8].
Including the individual with SCI in the goal setting process has proven to have many benefits including: increasing the client’s intrinsic motivation, decreasing anxiety and depression, improving insight and acceptance of the diagnosis and improving self-care and community integration [8,9,10].
Despite there being a variety of client-centered goal setting methods and strategies, many therapists indicate that involving their patients during goal setting is challenging [11,12,13]. Papadimitriou found that some therapists unintentionally exclude their clients from the process [4].
In South Africa, one of the difficulties that therapists face in client-centered goal setting is the rich diversity of cultures and languages [14, 15]. There is limited literature on how goals are set with individuals with SCI in South Africa and whether OT are client-centered in their approach [16, 17].
Research was therefore undertaken to establish the current goal setting practices of OT working in SCI rehabilitation and how they envision ideal goal setting practices.
Methods
Design
A qualitative research design with an appreciative inquiry (AI) stance was used [18,19,20]. Appreciative inquiry is a useful and innovative methodology in health care research. It is a creative approach which involves asking ‘unconditional positive questions’, as it assumes that every group of people or organization has untapped positive potential and that when this potential is focused on, it promotes change and provides a way forward [18, 19, 21]. During an AI process, the discussion progresses through four different phases, namely: the discovery, dream, design and destiny phases [22]. Ethical clearance was granted by the University of Pretoria’s Faculty of Health Research Committee (480/2018) and the National Research Health Data base (GP_201810_031).
Participant recruitment
Purposive sampling was used to recruit OT who had been working in either a private or public setting spinal rehabilitation unit in Gauteng (South Africa) for a minimum period of 6 months [23]. Five female therapists voluntarily consented to participate in the study. Their ages ranged from 21 to 30 years. Their years of experience in spinal rehabilitation ranged from 1 to 7 years. Two public and one private rehabilitation units were represented in the sample.
Data collection
The focus group was conducted by an experienced qualitative researcher with experience as an OT in physical rehabilitation to facilitate an in-depth discussion on current effective goal setting practices and to generate ideas for ideal goal setting practices in SCI rehabilitation within a South African context [24]. The researcher observed and took field notes during the focus group.
Data analysis
The data was transcribed verbatim and analysed thematically using the steps as described by Braun and Clarke [25]. The researcher familiarized herself with the data during transcription. Codes were developed and categorized into themes using a deductive process, considering the main concepts in literature as well as the phases of AI. An iterative process involving both the researcher and independent reviewer confirmed the themes. The decision process has been documented and is available as an audit trail. The data was described and triangulated with literature [25]. In order to ensure research rigor in this study, Guba’s Model of Trustworthiness as described by Krefting and Creswell’s strategies were implemented [26, 27]. Member-checking by the participants, and peer examination by both the supervisors and an independent coder contributed toward the credibility and therefore truth value of the study [26]. Consistency was established using dense descriptions of the data analysis which was subjected to a dependability audit by the independent coder and supervisors from the onset of the research [26].
Results
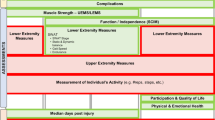
The study focused on current effective goal setting practices (the discovery phase), ideal goal setting practices (the dream phase), and lastly, generated ideas for best goal setting practices in the current context (the design and destiny phases). Seven themes emerged.
Discovery phase (current effective goal setting practices)
The objective of the discovery phase was to explore how OT in spinal rehabilitation currently set goals. Please see Table 1.1, which contains a summary of the themes in this phase.
THEME 1: client insight is a support to goal setting
The first theme that was developed during this phase was “Client insight is a support to goal setting.” The five participants identified that clients who have better insight into their diagnosis and situation are more likely to participate in the goal setting process. The participants added that clients normally have improved insight into their condition once they have been home for a weekend, which in turn facilitates the goal setting process.
-
“As [the client] understands more and starts to accept more they will also come with their suggestions or their requests or their goals”
-
“[This is] where they can go home and see what is problematic at home for them and when they come back they can say I struggled with getting into the bath or going shopping or whatever…”
THEME 2: current goal setting is therapist directed
Participants identified that current goal setting is therapist-directed. Five participants contributed toward this theme. Participants explained that they set goals for people with SCI based on own their clinical experience and clinical reasoning. During this therapist-directed process they will consider the following: the individual’s context, resources available at the client’s home and the expected outcomes of the person’s lesion according to the America Society of Spinal Cord Injury Impairment Scale. The participants added that they will only occasionally include other people in the goal setting process, including the family and other team members.
-
“So I end up setting goals from experience. And they’re not really client centered goals, [they are] necessary goals”
-
“After the assessment you see, are they working? Are they studying? What are they doing? And you try and incorporate that.”
-
“What’s important is the environment that they’re going back to. It really affects the type of transfers you’re going to do with them. What type of bath they use? Where is the space in that bathroom? The type of wheelchair that we issue all depends on the type of environment that they’re going back to. So that’s a big thing that guides the goals as well. That you’re not going to teach someone to go into a [large dish] if they don’t need to, so that’s a big thing for us. Especially our rural guys that don’t have toilets that flush, or where there isn’t water accessible.”
Dream phase (ideal goal setting practices)
The objective of the dream phase was to explore how OT in spinal rehabilitation envision ideal goal setting practices. The participants identified three important ideals in this phase: goal setting should be client-centered and that both adequate resources and effective collaboration support ideal goal setting. See Table 1.2 for an outline of the development of the themes in the phase.
THEME 3: goal setting should be client-centered
The five participants explained that ideally the client should always be involved during the goal setting process. Therapists should also attempt to improve client insight into their diagnosis and prognosis to ensure that the client is able to set realistic goals. The participants highlighted that goals should focus on community integration and not just on enabling the client to return home. To achieve this the participants explained that they would ideally like to see the environments that the clients were returning to.
-
“In the ideal world, it’s the patients’ needs and goals that are taken into account.”
-
“[The client] needs a person to facilitate that process of understanding of where you’re going to [in therapy].”
-
“[The patient’s] environment that is so far removed from us. We don’t always know how to assist them because how can you teach someone about something that you don’t even know what’s happening”.
THEME 4: adequate resources support ideal goal setting
Whilst envisioning about ideal goal setting practices, the five participants discussed resources that would support the goal setting process, including assistive devices and a smaller client-to-therapist ratio.
The participants explained that if they had a variety of assistive devices available, they would be able to show clients how they could more independently engage in tasks and be better able to facilitate realistic goals.
-
“You become so used to what you have that you tend to forget what actually is available out there… I have a patient, who is a quad, who wants to work on his computer again. But because we don’t have it, I tend to say ag, I don’t know how I’m going to help you it’s going to be very difficult. But then actually you just go onto google and there are such easy assistive devices that you can use. And I think having multiple assistive devices that you can experiment and explore with to help the patient to more easily realise and identify new goals.”
A smaller client-to-therapist ratio would be ideal and would give the therapists sufficient time to set appropriate and achievable goals with their clients.
-
“You’ll then have time to research, you have time to explore with your patient, you’ll have time to go on a home visit with your patient, so time would really make a difference.”
THEME 5: collaboration supports goal setting
The five participants from the focus group explained that in an ideal situation, the multidisciplinary team and the client’s family should be committed to work together during goal setting. The participants added that ideally, there should be regular meetings with the team to review goals.
-
“I do think that the [multidisciplinary team] approach is the dream”
Design and destination phase (steps to implement ideal goal setting)
The objective of the design and destination phase was to develop the steps required to implement ideal goal setting practices in the current context. See Table 1.3 for the development of the themes in this phase. The participants included steps to ensure client-centered practice and effective collaboration.
THEME 6: steps to ensure client-centered practice during goal setting
The five participants generated the following practical ideas of how to ensure goal setting remains client-centered: always address the client’s priorities first, advocate for client’s needs within the multidisciplinary team (MDT), empower the client with knowledge and set long term community goals. Doing home visits for clients who live in close proximity to the hospital was another suggestion.
-
“Ask the patient, and regularly ask them: what is important to you?”
-
“I realise that even in the MDT team people don’t really have information or knowledge on disability laws, maybe that’s a place for an OT where they can kind of advocate so long.”
-
“What are their goals as a community member?”
-
“But may be starting with patients in our catchment area, like within 20 to 30 min from the hospital and actually doing the home visit.”
THEME 7: steps to ensure collaboration during goal setting
The participants felt that to ensure collaboration, team communication should be improved. The participants added that it would be helpful to put structures in place to facilitate the team in setting goals together (Table 2).
-
“With everyone [in the MDT] sitting around the table and making time to fill [the goals] in.”
Discussion
The aim of the study was to explore how OT implement and envision goal setting practices in spinal rehabilitation. Goal setting is an important part of client-centered therapy and forms a critical part of rehabilitation [6, 8]. A goal is normally set for a future time frame involving an improvement or the maintenance of a client’s abilities. A goal should be the intentional result of a specific intervention, not a prediction of the future [8].
Goal setting allows the team to work toward the same goal, and ensures that all important aspects are addressed and saves time by allowing the rehabilitation team to monitor whether interventions have been beneficial to the client [8].
The participants explained that they rely on their clinical reasoning and their past experience when they are setting goals for clients. This is consistent with Holliday’s findings, which indicate that therapists formed the goals for intervention based on their own understanding of the client’s wishes and desires [11]. In addition, studies show that clients’ views and expectations are rarely explored [28, 29]. Clients who have adequate insight into their diagnosis are better able to participate in the goal setting process. Lack of insight can leave clients with a false expectation of recovery, which acts as a barrier during goal setting and could lead to a discrepancy in expectations between the client and the therapist [10, 30]. Barclay similarly found that individuals with SCI struggle to envision what independence may look like following a SCI, while the OT had clear ideas regarding what would be possible for the individual’s independence and knew how to achieve it [10]. Although therapist-led goals are practical and perhaps even easier, we need to acknowledge that this does not conform to the philosophy of client-centered practice, which permits the client to have a more active role in the therapy process [6, 7].
The participants described that, ideally, they would take a more client-centered approach to their goal setting. It has been found that goals set by the client are more effective [8]. A systematic review on goal setting in rehabilitation found that the most commonly suggested improvement that could be made to goal setting in rehabilitation was for an element of education to be included prior to the goal setting process [31]. This would improve the client’s insight and allow them to actively participate in the goal setting [31].
Efficient collaboration within the MDT was considered ideal. Literature suggests that collaboration with other members of the MDT is rare [32]. However, studies show that improved communication amongst a MDT have resulted in better-quality health care for the client and improves client outcomes in rehabilitation settings [32]. Sumsion and Nas et al. also suggest that the rehabilitation team should not only consist of the rehabilitation professionals, but should consist of a much broader team including the family [33, 34].
Collaborating with the client’s employer in order to plan for the return to work was emphasized, as well as the need for rehabilitation and goal setting to extend past discharge into the client’s home and community [35]. Research has found that in South Africa, people with SCIs were discharged from rehabilitation and sent back to their former environments without reaching functional independence or having their work addressed [16, 17]. The importance of continual rehabilitation post-discharge is supported by a study which found that patients who had successfully completed rehabilitation demonstrated gradual loss in their independence following discharge [36]. However, this changed after they received intervention post-discharge, even if it was via telehealth and not in person [36].
Ideal goal setting is made easier with adequate resources. Studies have shown that only a few of the nine provinces in South Africa have the resources to provide comprehensive care to the survivors of SCI’s, and that in the public sector, there is a high percentage of unmet rehabilitation needs [37]. It was found that in 71% of cases, the reason for not having met those rehabilitation needs was due to inadequate finances [37].
The participants highlighted that they would take steps to ensure better collaboration within the team, including better communication and establishing a goal setting structure. According to Nancarrow, communication strategies and structure are one of the key principles of good teamwork [38]. Finally, participants acknowledged that the client is an expert regarding their own lives, and their personal goals, opinions and interests should take priority during therapy [6, 7].
In conclusion, the study emphasized that for effective goal setting to occur, the process must remain client-centered and include effective collaboration within the team.
Data archiving
The data will be archived in the Occupational Therapy Department at the University of Pretoria until 1 December 2033.
References
Kelbine P. Adjustment to a spinal cord injury. Birmingham: National Institute of Disability and Rehabilitation Research; 2004.
Atkins MS. Spinal cord injury. In: Radomski MV, Trombly Latham CA, editors. Occupational therapy for physical dysfunction. sixth ed. Philadelphia: Wolters Kluwer; 2008. p. 1172–213.
Joseph C, Wikmar LN. Living with a long-term traumatic spinal cord injury in South Africa: Experiences related to readjustment and attained participation (self-perceived). Physiotherapy. 2015;101:e696–7.
Papadimitriou C, Carpenter C. Client-centered practice in spinal cord injury rehabilitation: a field guide. 2013. p. 3–42.
WFOT. Definitions of occupational therapy from member organizations. World Federation Occup Therapists 2013;2013:49.
Townsend E, Wilcock AA. Occupational justice and client-centred practice: a dialogue in progress. Can J Occup Ther. 2004;71:75–87.
Casteleijn D, Graham M. Incoporating a client-centered approach in the development of occupational therapy outcome domains for mental health care settings in South Africa. South African J Occup Therapy. 2012;42.
Wade D. Goal setting in rehabiliation: an overview of what, why and how. Clin Rehabil. 2009;23:291–5.
Elliott TR, Uswatte G, Lewis L, Palmatier A. Goal instability and adjustment to physical disability. J Counseling Psychol. 2000;47:251–65.
Barclay L. Exploring the factors that influence the goal setting process for occupational therapy intervention with an individual with spinal cord injury. Aust Occup Ther J. 2002;49:S. 3–13 (March 2001).
Holliday RC, Antoun M, Playford ED. A survey of goal-setting methods used in rehabilitation. Neurorehabilitation Neural Repair. 2005;19:227–31.
Restall G, Ripat J. Applicability and clinical utility of client-centered strategies frameword. Can J Occup Ther. 2008;75:228–300.
Parker DM. An exploration of client-centred practice in occupational therapy: Perspectives and impact: University of Birmingham; 2012.
Watson RM. Being before doing: the cultural identity (essence) of occupational therapy. Aust Occup Ther J. 2006;53:151–8.
Govender P, Mpanza DM, Carey T, Jiyane K, Andrews B, Mashele S. Exploring cultural competence amongst ot students. Occup Ther Int. 2017;2017:2179781.
Henn MJ. Evaluation of the rehabilitation program for persons with complete paraplegia at netcare rehabilitation hospital: University of Stellenbosch; 2009.
Hastings MB. Factors that influence functional ability in individuals with spinal cord injury: University of Witwatersrant; 2013:1–25;55.
Cooperrider DL, Whitney D. A positive revolution in change: appreciative inquiry. 1–36.
Carter B. “One expertise among many”” working appreciatively to make miracles instead of finding problems: Using appreciative inquiry as a way of reframing research. J Res Nurs. 2006;11:48–63.
Moore C [Internet] What is appreciative inquiry? A brief history & real life examples. 2019 [updated 27 April 2019; cited 2019 28 June]. https://positivepsychology.com/appreciative-inquiry/.
Trajkovski S, Schmied V, Vickers M, Jackson D. Using appreciative inquiry to transform health care. Contemp Nurse. 2013;45:95–100.
David C, Associates [Internet] What is appreciative inquiry. 2012 [cited 2018 7 May]. http://www.davidcooperrider.com/ai-process/.
Association SASC [Internet] Units with facilities for sci. 2017 [updated 7 June 2017; cited 2018 7 June]. Available from: www.sasca.org.za.
Liamputtong P. Focus group methodology: principles and practice. London: SAGE Publications Ltd; 2015.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3:77–101.
Krefting L. Rigor in qualitative research: The assessment of trustworthiness. the American journal of occupational therapy. 1991; 45.
Creswell JW, Poth CN. Qualitative inquiry and research design. Fouth ed: United States of America: Sage; 2018.
Adams K. Goal setting for occupational therapists and patients with spinal cord injuries. 2010.
Cameron L, Somerville L, Naismith C, Watterson D, Maric V, Lannin N. A qualitative investigation into the patient-centered goal-setting practices of allied health clinicians working in rehabilitation. Clin Rehabil. 2018;32:827–40.
Plant SE, Tyson SF, Kirk S, Parsons J. What are the barriers and facilitators to goal-setting during rehabilitation for stroke and other acquired brain injuries? A systematic review and meta-synthesis. Clin Rehabil. 2016;30:921–30.
Rose A, Rosewilliam S, Soundy A. Shared decision making within goal setting in rehabilitation settings: A systematic review. Patient Educ Counseling. 2017;100:65–75.
Falk-Kessler J. Professionalism, communication and teamwork. In: Cohn E, editor. Willard & spackmans occupational therapy. 2014. p. 452–66.
Sumsion T. Client-centred practice: the true impact. Can J Occup Ther. 1993;60:6–8.
Nas K, Yazmalar L, Sah V, Aydin A, Ones K. Rehabilitation of spinal cord injuries. World J Orthop. 2015;6:8–16.
Joseph C, Wahman K, Phillips J, Wikmar LN. Client perspectives on reclaiming participation after a traumatic spinal cord injury in South Africa. Phys Therapy. 2016;96.
Nishu Tyagi, Goel SA, Alexander M. Improving quality of life after spinal cord injury in india with telehealth. Spinal Cord Series. 2019:5:70–109.
Joseph C, Scriba E, Wilson V, Mothabeng J, Theron F. People with spinal cord injury in republic of South Africa. Am J Phys Med Rehabil. 2017;96:S109–11.
Nancarrow SA, Booth A, Ariss S, Smith T, Enderby P, Roots A. Ten principles of good interdisciplinary team work. Hum Resour Health. 2013;11:19.
Acknowledgements
We would like to thank everyone involved in the focus group and this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Snyman, A., de Bruyn, J. & Buys, T. Goal setting practices of occupational therapists in spinal cord injury rehabilitation in Gauteng, South Africa. Spinal Cord Ser Cases 7, 48 (2021). https://doi.org/10.1038/s41394-020-00352-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-020-00352-8