Abstract
Study design
Cross-sectional survey in Canada.
Objectives
To explore multimorbidity (the coexistence of two/more health conditions) in persons with non-traumatic spinal cord injury (NTSCI) and evaluate its impact on healthcare utilization (HCU) and health outcomes.
Setting
Community-dwelling persons.
Methods
Data from the Spinal Cord Injury Community Survey (SCICS) was used. A multimorbidity index (MMI) consisting of 30 secondary health conditions (SHCs), the 7-item HCU questionnaire, the Short Form-12 (SF-12), Life Satisfaction-11 first question, and single-item Quality of Life (QoL) measure were administered. Additionally, participants were grouped as “felt needed healthcare was received” (Group 1, n = 322) or “felt needed healthcare was not received” (Group 2, n = 89) using the HCU question. Associations among these variables were assessed using multivariable analysis.
Results
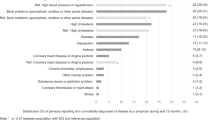
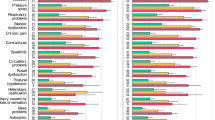
408 of 412 (99%) participants with NTSCI reported multimorbidity. Constipation, spasticity, and fatigue were the most prevalent self-reported SHCs. Group 1 had a higher MMI score compared to Group 2 (p < 0.001). A higher MMI score correlated with the feeling of not receiving needed care (OR 1.4, 95% CI 1.08–1.21), lower SF-12 (physical/mental component summary scores), being unsatisfied with life, and lower QoL (all p < 0.001). Additionally, Group 1 had more females (p < 0.001), non-Caucasians (p = 0.034), and lower personal annual income (p = 0.025).
Conclusions
Persons with NTSCI have multimorbidity, and the MMI score was associated with increased HCU and worse health outcomes. This work emphasizes the critical need for improved healthcare and monitoring. Future work determining specific thresholds for the MMI could be helpful for triage screening to identify persons at higher risk of poor outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data are not publicly available as participants did not provide informed consent to share them.
References
WHO. Multimorbidity: technical series on safer primary care. [Internet]. Geneva: World Health Organization. World Health Organization; 2016. p. Licence: CC BY-NC-SA 3.0 IGO. Available from: https://apps.who.int/iris/bitstream/handle/10665/252275/9789241511650-eng.pdf.
The Academy of Medical Sciences. Multimorbidity: a priority for global health research. 2018. https://acmedsci.ac.uk/file-download/82222577. Accessed 10 Jan 2022.
Johnston MC, Crilly M, Black C, Prescott GJ, Mercer SW. Defining and measuring multimorbidity: a systematic review of systematic reviews. Eur J Public Health. 2019;29:182–9.
Geda NR, Janzen B, Pahwa P. Chronic disease multimorbidity among the Canadian population: prevalence and associated lifestyle factors. Arch Public Health. 2021;79:60.
Ho ISS, Azcoaga-Lorenzo A, Akbari A, Black C, Davies J, Hodgins P, et al. Examining variation in the measurement of multimorbidity in research: a systematic review of 566 studies. Lancet Public Health. 2021;6:e587–97.
Kone AP, Mondor L, Maxwell C, Kabir US, Rosella LC, Wodchis WP. Rising burden of multimorbidity and related socio-demographic factors: a repeated cross-sectional study of Ontarians. Can J Public Health. 2021;112:737–47.
Richardson A, Samaranayaka A, Sullivan M, Derrett S. Secondary health conditions and disability among people with spinal cord injury: a prospective cohort study. J Spinal Cord Med. 2021;44:19–28.
Tallqvist S, Kauppila A-M, Vainionpää A, Koskinen E, Bergman P, Anttila H, et al. Prevalence of comorbidities and secondary health conditions among the finnish population with spinal cord injury. Spinal Cord. 2022;60:618–27.
Strøm V, Månum G, Arora M, Joseph C, Kyriakides A, Fort Mle, et al. Physical health conditions in persons with spinal cord injury across 21 countries worldwide. J Rehabilit Med. 2022;54:jrm00302.
Jensen MP, Truitt AR, Schomer KG, Yorkston KM, Baylor C, Molton IR. Frequency and age effects of secondary health conditions in individuals with spinal cord injury: a scoping review. Spinal Cord. 2013;51:882–92.
Cao Y, DiPiro N, Krause JS. Association of secondary health conditions with future chronic health conditions among persons with traumatic spinal cord injury. Top Spinal Cord Inj Rehabilit. 2020;26:283–9.
Piatt JA, Nagata S, Zahl M, Li J, Rosenbluth JP. Problematic secondary health conditions among adults with spinal cord injury and its impact on social participation and daily life. J Spinal Cord Med. 2016;39:693–8.
Peterson MD, Kamdar N, Whitney DG, Ng S, Chiodo A, Tate DG. Psychological morbidity and chronic disease among adults with nontraumatic spinal cord injuries: a cohort study of privately insured beneficiaries. Spine J. 2019;19:1680–6.
Noonan V, Fallah N, Park S, Dumont F, Leblond J, Cobb J, et al. Health care utilization in persons with traumatic spinal cord injury: the importance of multimorbidity and the impact on patient outcomes. Top Spinal Cord Inj Rehabilit. 2014;20:289–301.
Guilcher SJT, Munce SEP, Couris CM, Fung K, Craven BC, Verrier M, et al. Health care utilization in non-traumatic and traumatic spinal cord injury: a population-based study. Spinal Cord. 2010;48:45–50.
Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord. 2004;42:513–25.
Molinares DM, Gater DR, Daniel S, Pontee NL. Nontraumatic spinal cord injury: epidemiology, etiology and management. J Pers Med. 2022;12:1872.
New PW, Cripps RA, Bonne Lee B. Global maps of non-traumatic spinal cord injury epidemiology: towards a living data repository. Spinal Cord. 2014;52:97–109.
New PW, Guilcher SJT, Jaglal SB, Biering-Sørensen F, Noonan VK, Ho C. Trends, challenges, and opportunities regarding research in non-traumatic spinal cord dysfunction. Top Spinal Cord Inj Rehabilit. 2017;23:313–23.
Gedde MH, Lilleberg HS, Aßmus J, Gilhus NE, Rekand T. Traumatic vs non-traumatic spinal cord injury: a comparison of primary rehabilitation outcomes and complications during hospitalization. J Spinal Cord Med. 2019;42:695–701.
Adriaansen JJE, Ruijs LEM, Van Koppenhagen CF, Van Asbeck FWA, Snoek GJ, Van Kuppevelt D, et al. Secondary health conditions and quality of life in persons living with spinal cord injury for at least ten years. J Rehabilit Med. 2016;48:853–60.
New PW, Simmonds F, Stevermuer T. Comparison of patients managed in specialised spinal rehabilitation units with those managed in non-specialised rehabilitation units. Spinal Cord. 2011;49:909–16.
Noreau L, Noonan V, Cobb J, Leblond J, Dumont F. Spinal cord injury community survey: a national, comprehensive study to portray the lives of Canadians with spinal cord injury. Top Spinal Cord Inj Rehabilit. 2014;20:249–64.
Noonan VK, Kwon BK, Soril L, Fehlings MG, Hurlbert RJ, Townson A, et al. The Rick Hansen Spinal Cord Injury Registry (RHSCIR): a national patient-registry. Spinal Cord. 2012;50:22–7.
Noreau L, Noonan V, Cobb J, Leblond J, Dumont F. Spinal cord injury community survey: understanding the needs of Canadians with SCI. Top Spinal Cord Inj Rehabilit. 2014;20:265–76.
Noreau L, Cobb J, Bélanger LM, Dvorak MF, Leblond J, Noonan VK. Development and assessment of a community follow-up questionnaire for the rick hansen spinal cord injury registry. Arch Phys Med Rehabilit. 2013;94:1753–65.
Statistic Canada. Canadian Community Health Survey (CCHS) - Cycle 3.1. 2005. http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SurvId=1630&InstaId=22642&SDDS=3226.
Ware J, Kosinski M, Keller SD. How to score the SF-12 physical and mental health summary scales. 2nd ed. Boston, MA: The Health Institute, New England Medical Center; 1995.
Gill SC, Butterworth P, Rodgers B, Mackinnon A. Validity of the mental health component scale of the 12-item Short-Form Health Survey (MCS-12) as measure of common mental disorders in the general population. Psychiatry Res. 2007;152:63–71.
Fugl-meyer AR, Melin R, Fugl-meyer KS. Life satisfaction in 18- to 64-year-old Swedes: in relation to gender, age, partner and immigrant status. J Rehabilit Med. 2002;34:239–46.
Aubert CE, Schnipper JL, Roumet M, Marques-Vidal P, Stirnemann J, Auerbach AD, et al. Best definitions of multimorbidity to identify patients with high health care resource utilization. Mayo Clin Proc Innov Qual Outcomes. 2020;4:40–9.
Griffith LE, Gruneir A, Fisher K, Panjwani D, Gafni A, Patterson C, et al. Insights on multimorbidity and associated health service use and costs from three population-based studies of older adults in Ontario with diabetes, dementia and stroke. BMC Health Serv Res. 2019;19:313.
Ware JE, Kosinski M, Keller SD. A 12-Item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33.
Frølich A, Ghith N, Schiøtz M, Jacobsen R, Stockmarr A. Multimorbidity, healthcare utilization and socioeconomic status: a register-based study in Denmark. PLoS ONE. 2019;14:e0214183.
Krause JS, Murday D, Corley EH, DiPiro ND. Concentration of costs among high utilizers of health care services over the first 10 Years after spinal cord injury rehabilitation: a population-based study. Arch Phys Med Rehabilit. 2019;100:938–44.
Liddy C, Moroz I, Affleck E, Boulay E, Cook S, Crowe L, et al. How long are Canadians waiting to access specialty care? Retrospective study from a primary care perspective. Can Fam Physician. 2020;66:434–44.
Pentland W, Walker J, Minnes P, Tremblay M, Brouwer B, Gould M. Women with spinal cord injury and the impact of aging. Spinal Cord. 2002;40:374–87.
Rampersaud YR, Power JD, Perruccio AV, Paterson JM, Veillette C, Coyte PC, et al. Healthcare utilization and costs for spinal conditions in Ontario, Canada - opportunities for funding high-value care: a retrospective cohort study. Spine J. 2020;20:874–81.
Krause JS, Kemp B, Coker J. Depression after spinal cord injury: relation to gender, ethnicity, aging, and socioeconomic indicators. Arch Phys Med Rehabilit. 2000;81:1099–109.
Krause JS, Broderick LE, Saladin LK, Broyles J. Racial disparities in health outcomes after spinal cord injury: mediating effects of education and income. J Spinal Cord Med. 2006;29:17–25.
Kingsley C, Patel S. Patient-reported outcome measures and patient-reported experience measures. BJA Educ. 2017;17:137–44.
Acknowledgements
We express thanks to all participants who participated in the 2011–2012 SCI Community Survey (SCICS), and the Praxis Spinal Cord Institute (grant number: 2010-03), and the Ontario Neurotrauma Foundation (grant number: 2010-RHI-SURVEY-812) who supported the survey. We acknowledge Dr. Frédéric S. Dumont, Dr. Jean Leblond, and Dr. Luc Noreau from the Center for Interdisciplinary Research in Rehabilitation and Social Integration (CIRRIS) and Université Laval, Quebec City, Canada, as well as Mr. John Cobb from Vancouver General Hospital, Vancouver, British Columbia, Canada for their contributions to the development, design and implementation of the SCICS.
Funding
This study was supported by Praxis Spinal Cord Institute, Health Canada, and Western Economic Diversification Canada.
Author information
Authors and Affiliations
Contributions
All authors participated in the study design and provided feedback on the manuscript. HH, DW, SH, JP, NF, CC and VN analyzed the data, interpreted the results and HH wrote the manuscript. VN and NF were the principal investigators and directors of the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare that we are employees of the Praxis Spinal Cord Institute.
Ethics approval and consent to participate
Ethics was obtained from an independent ethics board (Institutional Research Board Services), the Research Ethics Board of Université Laval (project #2009-179), and from local research ethics boards to recruit participants from SCI centers across Canada. We further certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research and that informed consent was obtained from all subjects.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hong, H.A., Fallah, N., Wang, D. et al. Multimorbidity in persons with non-traumatic spinal cord injury and its impact on healthcare utilization and health outcomes. Spinal Cord 61, 483–491 (2023). https://doi.org/10.1038/s41393-023-00915-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-023-00915-0