Abstract
Study design
Retrospective cohort study Objectives: to describe the incidence and the associated risk factors of post-surgical complications and recurrence in individuals with spinal cord injury/disorder (SCI/D) presenting deep pressure injuries (PIs), treated with a specific surgical and rehabilitation treatment protocol.
Setting
Tertiary Rehabilitation Hospital for SCI/D in Italy. Methods: Retrospective analysis of the medical records of adult individuals with SCI/D, who developed a PI after the first discharge from a Spinal Unit, underwent flap surgery for PI between July 2011 and January 2018. The statistical unit of analysis was the surgical intervention. Logistic regression analysis with robust standard errors was performed to assess risk factors of post-surgical complications.
Results
434 surgical intervention records were included, for a total of 378 patients. The treated PIs were ischiatic in 56.2% of the cases, sacral in 32.5%, trochanteric in 15.7%, and 5.8% were in other sites. In 239 cases (55.1%) a histological diagnosis of osteomyelitis was confirmed. Minor complications occurred in 13.6% of interventions, while major complications were 3.9%. Sacral PI (OR = 2.55, 95%CI: 1.50–4.35) and muscular/musculocutaneous flap (OR = 2.12, 95%CI: 1.05–4.28) were significant factors associated with risk of post-surgical complications. After a mean follow-up of 21 months (range 12–36), six people (1.4%) had a recurrence. Patients with a recurrence had at least one comorbidity compared to 57% of people without recurrences (p = 0.036).
Conclusion
Our results demonstrate that complication and recurrence rates can be minimized when an established interdisciplinary and rehabilitation protocol is integrated in the clinical management.
Similar content being viewed by others
Background
People with spinal cord injury/disorder (SCI/D) are at high risk of pressure injury (PI) formation. A recent review by Cowan et al. reported a prevalence of 34% for persons with tetraplegia and 47% for persons with paraplegia [1]. In the chronic SCI/D stage, the reported PI prevalence varies between 15 and 30% and several risk factors can be identified: socio-demographic, neurological, medical, or behavioral [2]. PI is the second most frequent complication in people with SCI/D [3] and generates the highest cost among complications [4]. Moreover, Kriz et al. recently reported that PI is one of the most common causes of death after SCI/D [5]. Wu-Fienberg reported that interdisciplinary rounds in the SCI unit significantly improve the care of patients with PI [6]. PI classification according to the depth of the wound is established internationally by the American National Pressure Ulcer Advisory Panel (NPUAP) [7]. We consider grade III–IV and unstageable, according to NPUAP classification, deep PIs. Established treatment protocols for deep PIs involve a multidisciplinary team and include surgical debridement, bone biopsy, reconstructive surgery, antibiotics, bed rest, and behavioral training [8]. There is still much debate on the timing of the procedures: Sumanas reported a two-stage surgical treatment (debridement then reconstruction) in 74 ischial PIs [9], while Kreutzträger reports 63 PIs treated in one stage in the buttocks area [10]. Also the post-operative bed rest time is controversial: Sumanas advokates 2-week supine bed rest on an air-fluidized bed [9], while Kreutzträger describes that post-operative mobilization in a wheelchair was performed after a mean of 46 days [10]. On the other hand, it is widely accepted that the treatment should include rehabilitation interventions for the prevention of PI recurrence by improving adherence to appropriate behaviors, such as education to a proper sitting position, intensive transfer training, motivation, as well as environmental factors [11].
The aim of this study is to describe the incidence of post-surgical complications and recurrence in patients treated with a specific surgical and rehabilitation treatment protocol. In addition, the risk factors associated with complications and recurrence were investigated.
Materials and methods
Study design, participants and setting
This is a retrospective cohort study on a consecutive sample of individuals with the following inclusion criteria: adult with SCI/D, who developed a PI after the first discharge from a Spinal Unit, who underwent flap surgery for chronic PI between July 2011 and January 2018 at Montecatone Rehabilitation Institute and was treated according to the described protocol of surgery and rehabilitation. Exclusion criteria were: any associated cerebral lesion, PIs with an onset during the first admission to a Spinal Unit, PIs with acute infection, PIs that could be closed primarily after the debridement, PIs that had already been treated surgically during the observational period. Montecatone Rehabilitation Institute is a Tertiary Rehabilitation Hospital for SCI/D in Italy. It is the main Emilia-Romagna regional referral centre for intensive rehabilitation of people with spinal cord injury and one of the three regional referral centers for severe acquired brain injuries. Furthermore, it is renowned at national level. As a matter of fact, more than half of the patients come from outside Emilia-Romagna Region. The hospital also includes a Critical Care Unit, which allows a very early rehabilitation care, immediately after injury. Since 2010 Montecatone Rehabilitation Institute has been accredited by the Emilia-Romagna Regional Health Service for 150 beds for inpatient care and 8 beds for day hospital, dedicated to people SCI/D and/or severe acquired brain injuries.
The study was approved by the Institutional Ethical Committee AVEC with the reference number 1000-2020-OSS-AUSLIM on 19th November 2020.
Multidisciplinary treatment protocol
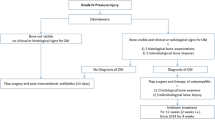
In 2011 at Montecatone Rehabilitation Institute a multidisciplinary treatment protocol for individuals with SCI/D presenting PI was developed. A multidisciplinary team of specialists such as wound care nurses, plastic surgeons, physiotherapists, and rehabilitation physicians are involved in the protocol of treatment, which takes place in different settings [Fig. 1]: telemedicine service, outpatient clinic, ward, operating room (OR) and rehabilitation center.
Our dedicated email inbox is the only way to access our services. This allows also persons from other regions and remote areas to consult us. Once a week, a plastic surgeon and a wound care nurse evaluate the emails and reply by email or by video-call to ask for more details, give instructions on dressings, or propose an appointment. For patients who live within our region, an appointment at the outpatient clinic is scheduled. The outpatient clinic is divided into a first-level clinic, managed by a specialized wound care nurse, and a second-level clinic, managed by a plastic surgeon, for persons presenting grade III–IV-unstageable PI with an indication for surgical treatment. Extra-regional patients are often directly admitted to the hospital to receive medical treatment of the PI. During admission, clinical and surgical consultations with general surgeons, urologist, orthopedic surgeon, or infectious disease specialists can be scheduled to plan eventual integrated additional therapies. The goals are to assess and improve nutritional status and general condition, improve local condition with advanced wound care and debridement if needed, and plan surgical treatment of complex wounds. Once surgery is scheduled, preoperative exams and anesthesiologic evaluations are performed in an outpatient setting and the patient is admitted at Montecatone Rehabilitation Institute the day before surgery. Pre-operative exams include chest x-ray, ecg, blood tests, etc (reported in Fig. 2). Based on protein levels nutritional implementation is started, if needed. The peri-operative treatment protocol is described in Fig. 2. The physiotherapist performs a computerized pressure mapping in sitting position to detect any asymmetries or incorrect posture [Fig. 3]. He or she also verifies the person’s pressure relief systems (cushion, wheelchair, mattress) and promptly activates any request for new assistive devices in case of inappropriateness. The person undergoes intestinal preparation at home before admission; on the day of surgery an anal plug is positioned to protect the surgical wound for 5 days, and an astringent diet is administered. We do not perform pre-operative magnetic resonance imaging to diagnose osteomyelitis, due to poor predictive value [12], we prefer treating every PI as if there was osteomyelitis. As a matter of fact, after coloring the PI with methylene blue, the surgical intervention always consists of a wide debridement of soft and bony tissues. Multiple deep biopsies of soft and bony tissues are sent for pathology and microbiology. In the same operation a reconstruction with a local or regional flap is performed. Fascio cutaneous flaps are usually the first choice, in order to leave muscular flaps in case of recurrence. In case of sacral PI, the flap is harvested unilaterally for the same reason. Only in case of trochanteric PI or recurrence of ischiatic PI muscular flap reconstruction is preferred (rectus femoris or lateral vastus flap for the trochanteric region and hamstring flap for the ischiatic region) in order to fill in the dead space and increase the thickness of the reconstruction. A suction drain is always placed. None of the persons receive any antimicrobial therapy during the 20 days before the operation due to poor sensitivity and specificity of preoperative superficial swab cultures [13, 14]. Patients receive piperacillin-tazobactam postoperatively until the results of the intra-operative specimen culture indicate adjustment of the therapy.
In the post-operative period bed rest for 3 consecutive weeks without weightbearing on the operated site is mandatory. Every 4 h, the person’s position is changed to prevent secondary injuries. When multiple injuries are treated in a single stage, a fluidized bed is used. Every 2 days, the surgical wound is dressed by a wound care nurse and twice a week by a plastic surgeon. After drain removal (generally 5–7 days after surgery), physiotherapy starts with passive and active mobilization of upper extremities, together with education on preventive strategies. Once a week, a multidisciplinary meeting is held to evaluate the person’s status and plan any additional therapies such as antimicrobial therapy, nutritional support, or blood transfusion. Antimicrobial therapy is adjusted by the infectious disease specialist based on the histological and microbiological findings on surgical specimens. In case of diagnosis of osteomyelitis (signs of hosteomyelitis at the histology plus at least one positive bone culture) the patient receives 6 weeks of appropriate antimicrobial therapy. Three weeks after surgery, the stitches are removed, and sitting is allowed for 1 h a day for 7 days. The person is trained to transfer properly from bed to wheelchair, and vice versa, without any skin friction. For tetraplegic individuals a lifter is used and a care giver is trained to transfer properly from bed to wheelchair, and vice versa, without any skin friction. The wound is checked every day after sitting to modulate sitting time and prevent immediate complications. Daily sitting time is increased by 1 h every week, and the person is discharged after rehabilitation to 3 h in a sitting position per day without wound complications. Prior to discharge, the physiotherapist performs again a computerized pressure mapping in sitting position to recommend changes on the sitting system [Fig. 4]. The person is discharged with clear instructions for preventive strategies (generally we advise a maximum of 6 h of daily sitting time in total for the first three post-operative months), the email address to contact the team for any doubt, and a follow-up appointment at 6 months.
At 6 and 12 months after surgery the person is seen by a plastic surgeon and a wound care nurse at the outpatient clinic for follow-up. This consultation includes clinical examination, a blood test with C-reactive protein, and ultrasound. Information on the person’s habits about preventive strategies (number of consecutive sitting hours, pressure relief maneuvers, hygienic status, technique to change position) is collected and the data are stored in a database. A telemedicine follow-up visit is offered to distant persons. Most of the patients also ask to be followed up every 6 months thereafter.
Data collection and outcome measures
Data were collected from the medical charts including: age, sex, comorbidities (obesity, diabetes, active smoking of more than 5 cigarettes a day, chronic kidney disease CKD, coronary heart disease CHD, obstructive sleep apnea syndrome OSAS), etiology of SCI/D, neurological level according to ASIA (American Spinal Injury Association) scale, number of treated PIs, localization of the PI (sacral, ischiatic, trochanteric, other site), histological diagnosis of osteomyelitis, type of flap reconstruction (fasciocutaneous, musculocutaneous), minor and major complications, length of stay in the rehabilitation hospital, recurrence. Obesity is defined as a calculated body mass index BMI > 20 kg/m2.
Diabetes is defined as reported anamnesis of glycemia >200 mg/dl in the presence of polyuria or polidypsia, or, in the absence of symptoms, a fasting blood glucose >200 mg/dl after oral glucose load. Diabetes is treated with a personalized therapy by inulin or other drugs, according to the indications of our internist.
CKD is defined as a reported anamnesis of chronically reduced eGFR in blood tests and chronically increased urine albumine to creatinine ratio in urine tests.
CHD is defined as a reported anamnesis of angina, chest pain, palpitation, unusual breathlessness triggered by physical activity or stressful situation, with previous cardiology evaluation that confirms the diagnosis.
OSAS is defined as a reported anamnesis of episodes of complete or partial obstruction of the upper airways during sleep, associated with daytime sleepiness and decreased cognitive function. Post-surgical complications were rated with the Clavien-Dindo grade [15], and considered minor when rated <3 and major when rated ≥3. Recurrence was recorded at the 6-month and 12 months follow-up visit. Often our surgical patients return to Montecatone Rehabilitation Hospital for periodical general health check ups, and during them they are checked also by the plastic surgeon. To reduce any possible loss to follow-up a telemedicine follow-up visit was offered to distant patients. In the analysis the primary outcomes were occurrence of post-surgical complications regardless of the degree of severity and recurrence.
Statistical analysis
The statistical unit of analysis is the surgical intervention. Indeed, during the study period a patient could have undergone more than one surgical treatment for PI. Robust standard errors were calculated to account for possible multiple interventions in the same individual, i.e., dependency among observations.
Incidence with 95% confidence interval (95% CI) was reported for minor complications, major complications, occurrence of any complication regardless of the degree of severity and recurrence.
Age was summarized as mean and standard deviation (SD) and compared between groups using the Student t test. Categorical variables were described using frequencies and percentages (%) and their association with the outcomes was investigated using Chi-squared test or Fisher’s exact test, as appropriate. Variables associated with the outcomes at p < 0.1 were included in a multiple logistic regression model with backward stepwise selection. Regression estimates were reported as Odds Ratios (OR) and 95% CI.
All analyses were performed using Stata statistical software version 15 (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC) and the significance level was set to p < 0.05.
Results
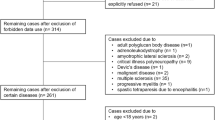
Between July 2011 and January 2018, 388 persons with SCI/D and PI were treated at Montecatone Rehabilitation Institute according to the described protocol of surgery and rehabilitation. When this study started in December 2020, 2 of them had died and 10 could not be traced. Therefore, 378 patients were included in the study, for a total of 434 surgical interventions and 521 treated PIs/. Fourty-four people underwent more than one surgical intervention during the study period and 71 patients underwent multiple (2 or 3) PI treatments in the same surgical intervention, among which 44 underwent multiple operations at different sites.
Sample mean age was 50.0 ± 13.5 years (range 15–80).Three hundred eighty-five treated PIs occurred in men (88.7%), and most of cases were of traumatic etiology (88.0%), uwhile the remaining were vascular (7.4%) or iatrogenic (4.6%). Tetraplegia and completeness of lesion (AIS A) were present in 26.7% and 85.7% of treated cases respectively. BMI was over 30 in 26.5% of cases, diabetes in 12%, and in 137 cases (31.6%) patients were active smokers). Characteristics of the study sample are reported in Table 1. lThe treated PIs were ischiatic in 56.2% of the cases (n = 244), sacral in 32.5% of the cases (n = 141), trochanteric in 15.7% of the cases (n = 68) and 5.8% were in other sites (n = 25). In 239 cases (55.1%) a histological diagnosis of osteomyelitis was confirmed. The average length of stay in the rehabilitation hospital was 55 days (range 42–150). In 59 cases (13.6%, 95%CI: 10.5%–17.2%) occurred a minor dehiscence (minor complications, grade 1–2 Clavien-Dindo). It was treated conservatively, which prolonged hospitalization but resulted in complete healingo,. Seventeen persons (3.9% of cases, 95%CI: 2.3%–6.2%) had a major complication that needed reintervention]: partial flap necrosis (n = 5), chronic seroma (n = 4) or fistula (n = 6). In two persons, the reintervention was for a hematoma on the first postoperative day, but both healed in the standard times. In two cases of trochanteric injuries treated with fasciocutaneous flaps, we found dehiscence and chronic seroma, successfully treated with a secondary reconstruction using a muscular flap. Overall the incidence of complications was 17.5% (95%CI: 14.0%–21.4%). In the group with complications there was a significantly higher frequency of cases with sacral PI and of injuries treated with muscular or musculocutaneous flaps, and a lower frequency of cases with ischiatic and other sites PIs, as compared to the group without complications (Table 1). In the multiple logistic regression analysis only sacral site and muscular/musculocutaneous flaps remained significant risk factors associated with post-surgical complications (Table 2). After a mean follow-up of 21 months (range 12–36), a recurrence occurred in 6 patients (1.4% of cases, 95%CI: 0.5%–3.0%). All these patients had at least one comorbidity as compared to 57.0% of people with no recurrence (p = 0.036). Specifically, 4 were active smokers and two of them had also CKD and CHD or obesity, one other patient was obese and another one had diabetes. Neither the level and cause of SCI, nor age and sex of the person were associated with the risk of recurrence or other complications.
Discussion
In our study on individuals with SCI/D presenting deep PI, treated with a specific surgical and rehabilitation treatment protocol, we report an overall incidence of post-surgical complications of 17.5% (95%CI: 14.0%–21.4%) and a recurrence rate of 1,4% (95%CI: 0.5%–3.0%), after a mean follow up of 21 months. To avoid any source of bias in the study, PIs that had already been treated surgically during the observational period were not included. Furthermore, only patients with chronic, non healing, deep wounds that needed a flap for reconstruction were included.
In the chronic stage PIs are a frequent complication related to socio-demographic, and behavioral factors [1]. PIs that appeared during the first admission in a Spinal Unit were not included because they have a different etiology, related more to the use of immobilizing devices for a prolonged period of time, intensive care unit admission, high injury severity score, mechanical ventilation and intracranial pressure monitoring, rather than to behavioral and social factors. Moreover in our practice we do not operate on PIS during the first admission to a Spinal Unit but prefer an accurate wound care, not to interfere with the rehabilitation program and training, that are a priority in this phase of the SCI/D.
Also PIs that could be closed primarily after the debridement were not included, as the risk of surgical complication is less conspicuous when flap surgery is not needed.
Few studies have been published on surgical treatment protocols for chronic PI in persons with SCI/D (Table 3). Moreover, few studies are prospective [16, 17] and include a very limited sample of patients (37–39 PIs), while most of the studies are retrospective [18,19,20,21,22,23].
Reporting an overview of pubblished studies on PI surgical outcomes in SCI/D patients in Table 3, we applied Clavien-Dindo classification of surgical complications referring to “minor complicarions” (grade 1–2) for those which prolonged hospitalization but resulted in complete healing without reintervention and to “major complications” (grade 3) for those that needed reintervention [15]. Anyway, reported outcomes are very heterogeneous, in particular minor complications not requiring reintervention, range from 6 to 37%. Reported major complications, requiring reintervention, range from 6 to 14%. In our sample, we found an incidence of 13.6% of minor complications and 3.9% of major complications, comparable with the data found in literature.
In our sample in the group with complications there was a significantly higher frequency of cases with sacral PI and of injuries treated with muscular or musculocutaneous flaps, and a lower frequency of cases with ischiatic and other sites PIs as compared to the group without complications (Table 1). In the multiple logistic regression analysis only sacral site and muscular/musculocutaneous flaps remained significant risk factors associated with post-surgical complications (Table 2).
Sacral PIs have not been reported as a risk factor for post-operative complications in the revised protocols, the area may allow a less extensive bony debridement, compared to ischiatic or trochanteric PIs and may be considered at higher risk of friction during bed mobilization, but further evidence should be collected to confirm our data.
Muscular flaps are known to have a higher risk of seroma [24], moreover, in individuals with SCI/D they may present dehiscence due to spasticity [25].
All our patients undergo intestinal preparation before admission, then follow an astringent diet and keep an anal plug to protect the surgical wound for 5 days. This useful protective bowel management allows wound consolidation without contamination, it is an easy trick that was not reported perviously.
According to our protocol, in case of diagnosis of osteomyelitis (signs of osteomyelitis at the histology plus at least one positive bone culture) the patient receives 6 weeks of appropriate antimicrobial therapy, that is comparable to what has recently been reported by Rigazzi et al. [26].
The most interesting finding in our study is the low recurrence rate at the surgical site, that was 1.4%. Reported recurrence rates range from 5 to 31%, with a mean recurrence rate of 19% [16,17,18,19,20,21,22,23]. We agree with Singh [27], who reports a recurrence rate of 5%, that the low recurrence might be due to active rehabilitation of these persons and involvement of the rehabilitation team in pre-operative care. Lindqvist [18] investigated factors influencing early complications, and found that a low serum albumin (<3.5 g/dl), and over- or underweight, were associated with an increased risk of complications and that 25% of the PIs were not healed at a 2-month follow-up. Our approach includes a nutritional status assessment and, if needed, correction before surgery, that is probably helpful, even if it was not matter of our analysis. In our records 2 of the 6 patients with recurrence were obese.
Surgery of PI in patients with SCI/D is not a low-risk venture. However, this surgery has an important impact on patients’ general health and quality of life [27] and, in an adequate setting with a comprehensive multidisciplinary treatment concept, complication and recurrence rates can be minimized.
The strengths of the treatment protocol are the established interprofessional and interdisciplinary team, prompt treatment of eventual complications as hematomas or dehiscence, thanks to a close follow up on the wound, protective bowel management, computerized pressure mapping in sitting position to detect and correct asymmetries, the check on the person’s pressure relief systems and the fact that the patients are constantly involved and engaged to learn and change their behaviors after this procedure. International accepted standards should be defined to increase the understanding of comprehensive treatment concepts.
The main limitation of our study and of most studies [18,19,20,21,22,23] is the retrospective nature of data collection, which does not allow to consider psychological or behavioral data, nor the presence of a care giver after surgery, which are factors that may be affecting the results; prospective studies should be conducted to collect more evidence.
Conclusion
A comprehensive treatment protocols for adult individuals with SCI/D in the chronic phase and deep PIs was presented. In this observational retrospective cohort study on a consecutive sample of individuals treated with the described multidisciplinary treatment protocol, we found a complete healing without complication nor recurrence at 12-month follow-up in 82% of cases. Our results demonstrate that complication and recurrence rates are low when an established interprofessional and interdisciplinary protocol is integrated in the clinical management.
Prospective studies should be conducted to collect more evidence.
Data availability
The data sets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cowan LJ, Ahn H, Flores M, Yarrow J, Barks LS, Garvan C, et al. Pressure Ulcer Prevalence by Level of Paralysis in Patients With Spinal Cord Injury in Long-term Care. Adv Ski Wound Care. 2019;32:122–30.
Gélis A, Dupeyron A, Legros P, Benaïm C, Pelissier J, Fattal C, et al. Pressure ulcer risk factors in persons with spinal cord injury Part 2: the chronic stage. Spinal Cord. 2009;47:651–61. https://doi.org/10.1038/sc.2009.32
DeVivo Michael FarrisV. Causes and Costs of Unplanned Hospitalizations Among Persons with Spinal Cord Injury. Top Spinal Cord Inj Rehabil. 2011;16:53–61.
White BAB, Dea N, Street JT, Cheng CL, Rivers CS, Attabib N, et al. The Economic Burden of Urinary Tract Infection and Pressure Ulceration in Acute Traumatic Spinal Cord Injury Admissions: Evidence for Comparative Economics and Decision Analytics from a Matched Case-Control Study. J Neurotrauma. 2017;34:2892–2900.
Kriz J, Sediva K, Maly M. Causes of death after spinal cord injury in the Czech Republic. Spinal Cord. 2021;59:814–20.
Wu-Fienberg Y, Henzel MK, Richmond MA, Becker DB. Impact of interdisciplinary rounds in the spinal cord injury unit on relational coordination for patients with pressure injury: A pilot study. J Spinal Cord Med. 2019;42:245–50.
Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M, et al. Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised Pressure Injury Staging System. J Wound Ostomy Cont Nurs. 2016;43:585–97. https://doi.org/10.1097/WON.0000000000000281
Kruger EA, Pires M, Ngann Y, Sterling M, Rubayi S. Comprehensive management of pressure ulcers in spinal cord injury: current concepts and future trends. J Spinal Cord Med. 2013;36:572–85. https://doi.org/10.1179/2045772313Y.0000000093
Jordan SW, De la Garza M, Lewis VL Jr. Two-stage treatment of ischial pressure ulcers in spinal cord injury patients: Technique and outcomes over 8 years. J Plast Reconstr Aesthet Surg. 2017;70:959–66. https://doi.org/10.1016/j.bjps.2017.01.004.
Kreutzträger M, Voss H, Scheel-Sailer A, Liebscher T. Outcome analyses of a multimodal treatment approach for deep pressure ulcers in spinal cord injuries: a retrospective cohort study. Spinal Cord. 2018;56:582–90. https://doi.org/10.1038/s41393-018-0065-3.
Mohamad Hashim N, Yusof ANM, Engkasan JP, Hasnan N. Factors affecting adherence to behaviours appropriate for the prevention of pressure injuries in people with spinal cord injury from Malaysia: a qualitative study. Spinal Cord. 2021;59:777–86.
Brunel A-S, Lamy B, Cyteval C, Perrochia H, Téot L, Masson R, et al. Diagnosing pelvic osteomyelitis beneath pressure ulcers in spinal cord injured patients: a prospective study. Clin Microbiol Infect. 2016;22:267.e1–267.e8.
Tedeschi S, Negosanti L, Sgarzani R, Trapani F, Pignanelli S, Battilana M, et al. Superficial swab versus deep-tissue biopsy for the microbiological diagnosis of local infection in advanced-stage pressure ulcers of spinal-cord-injured patients: a prospective study. Clin Microbiol Infect. 2017;23:943–7.
Summo V, Sgarzani R, Negosanti L, Fabbri E, Vietti Michelina V, Villani R, et al. Pressure Ulcers in Patients with Spinal Cord Injuries: Concordance Between Swab and Intraoperative Culture. Plast Reconstr Surg Glob Open. 2016;4:e651.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Singh R, Singh R, Rohilla RK, Magu NK, Goel R, Kaur K, et al. Improvisations in classic and modified techniques of flap surgery to improve the success rate for pressure ulcer healing in patients with spinal cord injury. Int Wound J. 2013;10:455–60.
Srivastava A, Gupta A, Taly AB, Murali T. Surgical management of pressure ulcers during inpatient neurologic rehabilitation: outcomes for patients with spinal cord disease. J Spinal Cord Med. 2009;32:125–31.
Lindqvist EK, Sommar P, Stenius M, Lagergren JF. Complications after pressure ulcer surgery - a study of 118 operations in spinal cord injured patients. J Plast Surg Hand Surg. 2020;54:145–50.
Morel J, Herlin C, Amara B, Mauri C, Rouays H, Verollet C, et al. Risk factors of pelvic pressure ulcer recurrence after primary skin flap surgery in people with spinal cord injury. Ann Phys Rehabil Med. 2019;62:77–83.
Paker N, Buğdaycı D, Gökşenoğlu G, Akbaş D, Korkut T. Recurrence rate after pressure ulcer reconstruction in patients with spinal cord injury in patients under control by a plastic surgery and physical medicine and rehabilitation team. Turk J Phys Med Rehabil. 2018;64:322–7.
Tadiparthi S, Hartley A, Alzweri L, Mecci M, Siddiqui H. Improving outcomes following reconstruction of pressure sores in spinal injury patients: a multidisciplinary approach. J Plast Reconstr Aesthet Surg. 2016;69:994–1002.
Ljung AC, Stenius MC, Bjelak S, Lagergren JF. Surgery for pressure ulcers in spinal cord-injured patients following a structured treatment programme: a 10-year follow-up. Int Wound J. 2017;14:355–9. https://doi.org/10.1111/iwj.12609
Biglari B, Büchler A, Reitzel T, Swing T, Gerner HJ, Ferbert T, et al. A retrospective study on flap complications after pressure ulcer surgery in spinal cord-injured patients. Spinal Cord. 2014;52:80–3.
Gruber S, Whitworth AB, Kemmler G, Papp C. New risk factors for donor site seroma formation after latissimus dorsi flap breast reconstruction:: 10-year period outcome analysis. J Plast Reconstr Aesthet Surg. 2011;64:69–74. https://doi.org/10.1016/j.bjps.2010.03.032.
King SJ, Bentz TW, Afifi ML, Reconstructive AM. surgery and patients with spinal cord injury: Perioperative considerations for the plastic surgeon. J Plast Surg Hand Surg. 2016;50:44–9. https://doi.org/10.3109/2000656X.2015.1071261.
Rigazzi J, Fähndrich C, Osinga R, Baumgartner S, Baumberger M, Krebs J, et al. Osteomyelitis and antibiotic treatment in patients with grade IV pressure injury and spinal cord lesion-a retrospective cohort study. Spinal Cord. 2022;60:540–7. https://doi.org/10.1038/s41393-022-00758-1.
Singh R, Singh R, Rohilla RK, Siwach R, Verma V, Kaur K, et al. Surgery for pressure ulcers improves general health and quality of life in patients with spinal cord injury. J Spinal Cord Med. 2010;33:396–400.
Acknowledgements
We aknowlegde for their contribution in the multidisciplinary treatment protocol developement and the constant team work Montecatone wound care team (Alba Boriello, Carlo Golinelli, Luca Spallone, Debora Donattini, Rita Capirossi), the physiotherapists Chiara Poletti and Barbara Oles and the phisicians Carlo Frondini, Cristina Orlandini, Gaetano Vetrone, Romano Linguerri, Emilio Emili, Francesco Costa, Mahmoud Ganem Sadam. Also thanks to Tiziana Giovannini and Cecilia Baroncini for their contribution.
Author information
Authors and Affiliations
Contributions
RS was responsible for writing the paper, EM revised the paper, LN prepared tables and figures, SL and MB collected the data, ST and FFT analyzed the data, KC reviewed the paper.
Corresponding author
Ethics declarations
Competing interests
All contributing authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest in the subject matter or materials discussed in this paper.
Ethics approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research, that was approved by the Institutional Ethical Committee AVEC with the reference number 1000-2020-OSS-AUSLIM on 19th November 2020.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sgarzani, R., Maietti, E., Tedeschi, S. et al. Multidisciplinary treatment protocol for ischiatic, sacral, trochanteric or other pressure injuries in people with spinal cord injury: a retrospective cohort study. Spinal Cord 61, 204–210 (2023). https://doi.org/10.1038/s41393-022-00869-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00869-9