Abstract
Study design
Cross-sectional, observational study.
Objectives
To determine whether changes in essential care during the COVID-19 pandemic impacted satisfaction with activities, participation, and relationships among individuals with spinal cord injury (SCI).
Setting
Data were collected online between December 31, 2020 and February 14, 2021 among community dwelling adults with SCI (N = 123).
Methods
The primary outcome variables were satisfaction with the ability to complete activities of daily living (ADLs) (mobility, dressing, feeding, and toileting), as well as satisfaction with participation in household and recreational activities, and satisfaction with relationships among friends, family, and with the status of one’s relationship measured with the International Spinal Cord Injury Data Sets Activities and Participation Basic Data Set. Primary predictors were age, gender, time since injury, completeness of injury, injury level, access to mental health, access to medications, access to medical supplies, and access to personal care assistants (PCAs).
Results
Impact on access to mental health and impact on access to supplies were the most common factors affecting satisfaction with activities, participation, and relationships for individuals with SCI during the COVID-19 pandemic. Impact on access to PCAs/homecare was also found to impact certain outcomes including feeding and participation in household activities.
Conclusions
Future supply chain disruptions from pandemics or natural disasters could have wide-reaching effects for individuals with SCIs. Thus, further research and advocacy is needed to improve mental health care planning and supply chain access during subsequent natural disasters.
Similar content being viewed by others
Introduction
The COVID-19 pandemic has had wide-reaching health impacts, however indirect impacts of the pandemic on mental health have received less attention [1]. Studies in the general population have shown a decrease in psychological well-being during the pandemic [2,3,4]. In addition to the direct impact of the COVID-19 physical illness and its complications, research reveals a negative impact of home confinement and social isolation on mental and emotional health leading to higher rates of depression [5, 6].
Individuals with spinal cord injury (SCI) constitute a unique and particularly vulnerable population. Even pre-pandemic, these individuals faced increased challenges including barriers to community mobility and reduced access to healthcare services [7]. Furthermore, rates of depression are higher in the SCI population than in the general public [8]. Given that individuals with SCI are often directly impacted by gaps in the healthcare system due to their dependence on healthcare services to meet daily needs, it is unsurprising that the effects of a global pandemic may be amplified in this population [9, 10]. Due to stay-at-home and social distancing orders, access to personal care attendants (PCAs), medical supplies, mental health support, and other healthcare services were restricted for individuals with disabilities during the COVID-19 pandemic [11]. Furthermore, shortages in provisions led to rationing of medical supplies which may have disproportionately affected individuals with disabilities, such as SCI [10, 12].
Although the Federal Emergency Management Agency underscored the importance of the inclusion of individuals with disabilities in the planning and implementation of emergency programs, consistent guidelines have been lacking [13, 14]. A clearer understanding of the impact of medical rationing and changes in access to healthcare services during the pandemic would help to lay the foundation for further advocacy for individuals with SCI in times of crisis. The aim of this study was to determine whether perceived changes in essential care, such as access to mental health support, medications, medical supplies, PCAs, and the ability to maintain medical equipment during the COVID-19 pandemic impacted satisfaction with activities, participation, and relationships among adults living with SCI. We hypothesized that perceived changes in access to essential care would impact satisfaction with activities of daily living (ADLs), participation in household and recreational activities, and satisfaction with personal relationships.
Methods
This study reports cross-sectional findings from an observational, longitudinal study. REDCap was used to administer an online survey at five time-points (baseline, 3-, 6-, 9-, and 12-months). REDCap is a secure web application for building and managing online surveys and databases that can be used to support online data capture for research studies. The current study analyzed data from the 6-month time-point collected between December 31, 2020 and February 14, 2021. The Institution’s Review Board approved this study. All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Participants
Participants were recruited internationally through dissemination of recruitment materials to SCI stakeholder groups, including the Paralyzed Veterans of America, the North American Spinal Cord Injury Consortium, and the European Spinal Cord Injury Federation. Social media channels, such as Twitter and Facebook, were used to recruit participants. To be included in the study, participants had a diagnosis of SCI or disorder via self-report, were 18 years of age or older, and were fluent in English. A total of 218 participants were enrolled in the study (n = 187 with complete data); however, due to attrition at the 6-month time-point, data from 124 participants were used for analysis. In comparison to the participants at baseline, participants in the 6-month cohort were more likely to be younger, male, not employed full-time, and have an incomplete injury.
Variable definition
Outcomes
The primary outcome variable, satisfaction with activities and participation, was measured using the International Spinal Cord Injury Activities and Participation Basic Data Set [15]. The primary variables were satisfaction with the ability to complete ADLs (mobility, dressing, feeding, and toileting), as well as satisfaction with participation in household and recreational activities and with relationships among friends, family, and with the status of one’s relationship (i.e., no relationship; married/living together; romantic relationship, not living together). Participants rated satisfaction with each outcome variable as “not satisfied,” “somewhat satisfied,” or “very satisfied.” Higher scores on the Activities and Participation Basic Data Set reflect increased satisfaction.
Predictors
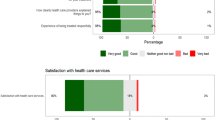
Our primary predictors were related to the perceived impact of COVID-19 on essential care; specifically, impact on access to mental health support, medications, medical supplies, PCAs/homecare services, and ability to maintain medical equipment. Participants rated the impact of the pandemic on a 4-point scale from “no impact” to “major impact.” Mental health support included access to a counselor, support groups, psychologist, or psychiatrist.
Demographic and injury characteristics were included as potential predictors of the outcomes and categorized at baseline by age (18–29, 30–49, 50–64, 65+), gender (male, female, transgender/other), level of injury (cervical, thoracic, lumbar, sacral), injury classification (tetraplegia, paraplegia), and injury completeness (complete, incomplete).
Statistical analysis
Multivariable linear regression was used to assess the effect of candidate predictor variables on the outcome variables of satisfaction with ADLs, participation, and relationships while controlling for demographic and injury characteristics. Satisfaction outcomes were treated as interval, as were impact of COVID-19 on access to essential care variables. COVID-19 impact on access to essential care was coded to indicate increasing impact such that the resulting beta-coefficient is associated with a one-level increase in impact on the access variable. Only observations where the participant responded with an impact rating (i.e., not “Prefer not to answer,” or “Don’t know,” if those choices were available) were included. For modeling purposes, injury characteristics (level, classification, and completeness) were coded to reflect increasing severity such that the resulting beta-coefficient is associated with an increase in severity. Because the outcome variables were coded to reflect increasing satisfaction, positive beta-coefficients indicate increasing satisfaction.
Each outcome variable was modeled with the primary predictor candidate variables and demographic and injury variables. Manual stepwise elimination with analyst judgment was used to determine the final model for each outcome. Observations with missing values for any modeled variable were dropped from the analysis. A p value of 0.05 or lower was considered significant; 95% confidence intervals are reported. All models were conducted using SAS v9.4 (Cary, North Carolina).
Results
Participant characteristics
A cohort of 123 participants responded to the 6-month survey and were included in the analysis. Demographic and injury characteristics are presented in Table 1. Most of the cohort was male (76.4%), white (88.7%), married or living with a partner (55.3%), living in a private residence (94.3%) and were 50 years of age or older at the time of the 6-month survey (78.9%). Participants were a mean of 20.5 years (SD = 14.3 years) from injury. Participants were nearly evenly split by injury classification, with 51.2% having tetraplegia and 48.8% having paraplegia. Most of the sample reported having incomplete (67.2%) injuries. Only one of the survey respondents was dependent on mechanical ventilation.
Predictors of the impact of the COVID-19 pandemic on ADLs
Mobility
In this multivariable linear regression (n = 93), increased impact on access to mental health support (p = 0.0318; −0.188, 95% CI [−0.359, −0.017]) was associated with decreased satisfaction in mobility (all model results are displayed in Table 2).
Dressing
In this multivariable linear regression, no model significantly explained satisfaction with dressing. Results are not presented.
Feeding
In this multivariable linear regression (n = 51), increased impact on access to PCA/homecare services (p = 0.0008; −0.402, 95% CI [−0.628, −0.177]) was associated with decreased satisfaction in feeding. The final model reflects only participants who reported needing in home assistance.
Toileting
In this multivariable linear regression (n = 93), injury classification as tetraplegia vs. paraplegia (p = 0.0054; −0.394, 95% CI [−0.669,−0.119]) and increased impact on ability to maintain medical equipment (p = 0.0102; −0.0224, 95% CI [−0.394,−0.055]) were associated with decreased satisfaction in toileting. An alternate model (results not shown) that included access to PCA/homecare services also found increased impact of COVID-19 on ability to maintain medical equipment to be significantly associated with decreased satisfaction with toileting. However, because impact to PCA/homecare services access itself was not significant and because the PCA/homecare item is asked only of those participants who indicated requiring such services, the more inclusive model was preferred.
Predictors of the impact of the COVID-19 pandemic on participation
Household activities
For this outcome, two multivariable linear regression models provided meaningful predictors of change in satisfaction: one model included all participants who responded to the satisfaction question (n = 83), whereas the second model only included people who required PCA/homecare services and responded to the satisfaction question (n = 37). In the first model, increased time since injury (p = 0.0120; 0.016, 95% CI [0.004, 0.028] and complete injury (vs. incomplete) (p = 0.0367; 0.377, 95% CI [0.024, 0.729]) were associated with increased satisfaction with participation in household activities. However, increased impact on access to medical supplies (p = 0.0154; −0.303, 95% CI [−0.547, −0.060]) was associated with decreased satisfaction with participation in household activities. In the second, limited model, increased time since injury (p = 0.0068; 0.024, 95% CI [0.007, 0.041]) was similarly associated with increased satisfaction with participation in household activities, and increased impact to access to medical supplies (p = 0.0323; −0.391, 95% CI [−0.747, −0.035]) was similarly associated with decreased satisfaction with participation in household activities (see Table 2). In addition, disruption to PCA/homecare services (vs. no disruption) (p = 0.0228; −0.563, 95% CI [−1.04, −0.084]) was significantly associated with decreased satisfaction with participation in household activities.
Recreational activities
In this multivariable linear regression (n = 90), increased impact on access to mental health support (p < 0.0001; −0.266, 95% CI [−0.395, −0.137]) was associated with decreased satisfaction with participation in recreational activities.
Predictors of the impact of the COVID-19 pandemic on satisfaction with relationships
Family relationships
In this multivariable linear regression (n = 92), increased impact on access to mental health support (p = 0.0011; −0.209, 95% CI [−0.331, −0.086]) and gender as female or transgender/other (p = 0.0050; −0.397, 95% CI [−0.670, −0.123]) were associated with decreased satisfaction with family relationships (all model results are displayed in Table 2).
Friend relationships
In this multivariable linear regression (n = 96), increased impact on access to mental health services (p = 0.0119; −0.165, 95% CI [−0.293, −0.037]) and increased impact on access to medical supplies (p = 0.0518; −0.178, 95% CI [−0.357, 0.001]) were both associated with decreased satisfaction with friend relationships.
Relationship status
In this multivariable linear regression, no model significantly explained satisfaction with one’s relationship status. Results are not presented.
Discussion
This study investigated whether changes in essential care during the COVID-19 pandemic impacted satisfaction with ADLs, participation in activities, and relationships among adults living with SCI. Consistent with our hypothesis, findings indicate that perceived impact of the pandemic on access to mental health support and medical supplies as well as ability to maintain medical equipment were related to satisfaction with certain activities, participation, and relationships.
Perceived impact of COVID-19 on access to mental health support was associated with decreased satisfaction with mobility, participation in recreational activities, and relationships with family and friends. Studies have shown that even low levels of depression can adversely affect interpersonal relationships and participation in activities in the general population; thus, it is unsurprising that individuals with SCI who are already at a greater risk of depression might report an impact to relationships and recreational activities given decreased access to mental health [16]. However, the authors are aware of few studies that have specifically looked at the impact of depression and access to mental health services during the pandemic in the SCI populations [1]. Further research is needed to examine these relationships.
The pandemic’s impact on access to medical supplies was associated with decreased satisfaction with participation in household activities. It was also nearly associated with decreased satisfaction with friend relationships (p = 0.0518) and would likely meet criteria for statistical significance with a larger sample. Importantly, this result is consistent with our other findings that the pandemic impacts on access to medical supplies is associated with changes in other measures of satisfaction with participation and activities. Further, the impact of COVID-19 on the ability to maintain medical equipment was related to decreased satisfaction with toileting. Among the participants who indicated an impact of the pandemic on medical supplies (n = 48), the most frequently reported supplies included gloves, bowel care supplies, wheelchairs, and wheelchair parts (Table 3). Given the disruption in access to bowel care supplies and gloves, it follows that individuals with SCI would have greater difficulty with toileting. Further, decreased satisfaction with bowel care due to access to supplies may have led to increased bowel incontinence, which may have impacted ability to leave the home. Disruption in access to wheelchairs and wheelchair parts may have led to multiple negative outcomes including skin breakdown, pain from improper positioning, and decreased mobility, all of which may have contributed to decreased ability to participate in household activities and to access the community to spend time with friends. Given these findings, supply chain disruptions may not only have a significant impact on physical health, but also on activities and participation for individuals with SCI.
The impact of COVID-19 on access to PCAs/homecare was related to decreased satisfaction with feeding and disruption to PCA/homecare services (vs. no disruption) was associated with decreased satisfaction with participation in household activities. Given that many individuals with SCI would require assistance with feeding multiple times per day as opposed to other ADLs, such as bathing or bowel care, disruption in access to PCAs may have placed a disproportionate burden on family related to feeding. Lack of access to PCAs also likely led to increased need for family to devote time to daily cares, possibly limiting their availability to encourage and assist with participation in household activities. Neither access to supplies nor access to medications emerged as a significant predictor of satisfaction with feeding; however, this is not entirely surprising given that medications and medical supplies are less relevant for feeding when compared to other activities, such as toileting. Given these findings, lack of access to PCAs may also have a significant impact on satisfaction with activities and participation for individuals with SCI.
Findings indicate that demographic and injury-related characteristics were also related to satisfaction with activities, participation, and relationships. Factors such as injury classification, gender, time since injury, and injury completeness contributed to the outcomes. Injury classification, for example, likely impacted toileting given that an individual with tetraplegia would be more dependent for toileting than an individual with paraplegia. Interestingly, non-male gender was associated with decreased satisfaction with family relationships. Studies of the effect of the pandemic on mental health in the general population have shown increased risk of low psychological well-being with female gender, but have not specifically looked at impact on family relationships [2, 3].
Contrary to our hypothesis, the impact of COVID-19 on essential care was not significantly related to satisfaction with dressing ability or one’s relationship status. Satisfaction with one’s relationship status, in this study, was in reference to whether people were satisfied with their current status, i.e., not in a relationship, married/living together, in a romantic relationship but not living together. Thus, satisfaction with relationship status may have been more directly impacted by factors such as increased time spent with family members during quarantine or loneliness as opposed to essential care.
Interestingly, although 24.8% of the cohort reported that the pandemic had an impact on their access to medications, this item did not emerge as a significant predictor of satisfaction outcome variables in any of the final models. It is unclear if this indicates a relative preservation of access to medications or that lack of access to medications simply did not have the largest impact on activities, participation, or relationships. It is possible that access variables constitute the mechanism by which certain injury characteristic/outcome relationships exist (e.g., injury classification [x], impact on medical supplies [m], satisfaction with toileting [y] or gender non-male [x], access to mental health support [m], satisfaction with family relationships [y]). Future studies might consider exploring mediation models to clarify these relationships.
Limitations
There are several study limitations that should be considered when interpreting these results. First, most participants in this cohort were white, male, and largely resided in the United States and in private residences. Additional sample selection bias may have been introduced via the method of recruiting participants through social media, online data collection, and disseminated materials through SCI stakeholder groups. There was also an attrition rate of 43% at 6 months when these data were collected, which may have led to a different sample population than the original group. Future studies should investigate a sample that is more generalizable to the broader SCI population. Furthermore, the cross-sectional nature of this study and lack of knowledge of prior satisfaction with the outcomes precludes causal inferences. For example, impact on access to mental health support may be associated with decreased relationship satisfaction, but those individuals may have also had decreased satisfaction with relationships prior to the pandemic. Future longitudinal studies are needed to elucidate the nature of these relationships. Finally, the impact of COVID-19 on essential care was measured by self-report questionnaires gathering information on perceived impact of the pandemic rather than by objective measures.
Conclusion
This study indicates that the pandemic’s impact on access to mental health services and medical supplies during the COVID-19 pandemic appeared to significantly impact satisfaction with activities and participation for individuals with SCI. Thus, future supply chain disruptions from pandemics or other disasters could have wide-reaching effects for individuals with SCIs. Advocacy and policy changes are needed to promote increased access to bulk provisions of medical supplies during times of crisis. Telehealth should also be used to connect persons with SCI with multi-disciplinary rehabilitation teams who can help them navigate care and supply needs. Given that the SCI community is already at increased risk of depression, virtual services should be made available for individuals with SCI to connect with rehabilitation psychologists as part of their interdisciplinary rehabilitation team. Advocacy is also needed to ensure that rehab psychology is not only physically accessible, but also financially accessible, for individuals with SCI. Further research investigating the indirect effects of the pandemic on mental health is needed to improve mental health care planning during subsequent natural disasters.
Data availability
Data are available from the corresponding author on request.
References
Mikolajczyk B, Draganich C, Philippus A, Goldstein R, Erin Andrews, Pilarski C, et al. Resilience and mental health in individuals with spinal cord injury during the COVID-19 pandemic. Spinal Cord. 2021. https://www.nature.com/articles/s41393-021-00708-3.
Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–42.
Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64.
Hossain MM, Sultana A, Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: a systematic umbrella review of the global evidence. Epidemiol Health. 2020;42:1–11.
Ammar A, Mueller P, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Psychological consequences of COVID-19 home confinement: the ECLB-COVID19 multicenter study. PLoS ONE. 2020;15. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7643949/.
Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66:317–20.
O’Connell CM, Eriks-Hoogland I, Middleton JW. Now, more than ever, our community is needed: spinal cord injury care during a global pandemic. Spinal Cord Ser Cases. 2020;6:18.
Williams R, Murray A. Prevalence of depression after spinal cord injury: a meta-analysis. Arch Phys Med Rehabil. 2015;96:133–40.
Lebrasseur A, Fortin-Bédard N, Lettre J, Bussières E-L, Best K, Boucher N, et al. Impact of COVID-19 on people with physical disabilities: a rapid review. Disabil Health J. 2021;14:1–9.
Lund EM, Forber-Pratt AJ, Wilson C, Mona LR. The COVID-19 pandemic, stress, and trauma in the disability community: a call to action. Rehabil Psychol. 2020;65:313.
Jesus T, Bhattacharjya S, Papadimitriou C, Bogdanova Y, Bentley J, Arango-Lasprilla J, et al. Lockdown-related disparities experienced by people with disabilities during the first wave of the COVID-19 pandemic: scoping review with thematic analysis. Int J Environ Res Public Health. 2021;18:6178.
Andrews EE, Ayers KB, Brown KS, Dunn DS, Pilarski CR. No body is expendable: medical rationing and disability justice during the COVID-19 pandemic. Am Psychol. 2021;76:451.
Fugate, C. Developing and maintaining emergency operations plans: comprehensive preparedness guide (CPG) 101. FEMA; United States: 2010.
Sabatello M, Burke TB, McDonald KE, Appelbaum PS. Disability, ethics, and health care in the COVID-19 pandemic. Am J Public Health. 2020;110:1523–7.
Post MW, Charlifue S, Biering-Sørensen F, Catz A, Dijkers MP, Horsewell J, et al. Development of the international spinal cord injury activities and participation basic data set. Spinal Cord. 2016;54:530–4.
Judd L, Paulus M, Wells K, Rapaport M. Socioeconomic burden of subsyndromal depressive symptoms and major depression in a sample of the general population. Am J Psychiatry. 1996;153:1411–7.
Acknowledgements
The authors would like to acknowledge the X for their contributions to this project.
Author information
Authors and Affiliations
Contributions
KRM, CD and AP were responsible for study design, oversight of data collection, extracting the data, interpreting results, and writing the manuscript. BM and LRM contributed to the introduction, results, and overall editing of the manuscript. KJE was responsible for the statistical analyses.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The institutional review board approved this study. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Draganich, C., Philippus, A., Eagye, K.J. et al. Changes in essential care in individuals with spinal cord injury during the COVID-19 pandemic. Spinal Cord 61, 76–82 (2023). https://doi.org/10.1038/s41393-022-00868-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00868-w