Abstract
Objective
To systematically review the literature on penetrating spinal cord injury (PSCI) and evaluate current management strategies, their impact on patient functional outcomes, and treatment complications.
Methods
PubMed, Scopus, and Cochrane were searched based on the Preferred Reporting Items for Systematic-Reviews and Meta-Analyses (PRISMA) guidelines to include studies on penetrating spinal cord injury (PSCI).
Results
We included 10 articles comprising 1754 cases of PSCI. Mean age was 19.2 years (range, 16–70), and most patients were male (89.9%). Missile spinal cord injury (MSCI) was the most common type, affecting 1623 patients (92.6%), while non-missile spinal cord injury (NMSCI) accounted for only 131 cases (7.4%). Gunshots were the most common cause of MSCI, representing 87.2%, while knife stabs were the most common cause of NMSCI, representing 72.5%. A total of 425 patients (28.0%) underwent surgical intervention, and 1094 (72.0%) underwent conservative management. The conservative group had a higher rate of complete spine cord injury compared with the surgical group (61.5% vs. 49.2; p < 0.001). Although surgery yielded a higher score improvement rate compared with the conservative management (41.5% vs. 20.5%, p < 0.001), neither treatment strategy displayed superiority in improving neurological outcomes for neither complete SCIs (OR:0.7, 95% CI, 0.3–1.64; I2 = 44%, p = 0.13) nor for incomplete SCIs (OR:1.15, 95% CI, 0.64–2,06; I2 = 40%, p = 0.12).
Conclusion
Surgical and conservative management strategies proved to be equally effective on PSCI, irrespective of injury severity. Therefore, tailored treatment strategies for each patient and careful surgical selection is advised.
Similar content being viewed by others
Introduction
Penetrating spinal cord injury (PSCI) involves a sharp object being forcefully driven through the spinal column, causing a focal injury along the tract of the object [1, 2]. While the estimated incidence of spinal cord injury (SCI) in the USA is 17,700 per year, SCI caused by PSCI roughly represents 5.5% and predominates disproportionately among males and the young population [1, 3]. Although blunt SCI accounts for most spinal injuries, PSCI is associated with higher morbidity and disability rates and thus is associated with substantial public health and economic burden [4, 5].
Studies investigating PSCI are scarce, reflecting their rarity [5, 6]. Current practices vary significantly worldwide, and several diagnostic and management protocols have been described [3, 7]. The management of PSCI focuses on acute and prompt patient care, mostly following the guidelines for blunt SCI management [8, 9]. The diagnostic workup primarily comprises imaging, such as MRI, to assess incomplete or progressive spinal injuries and to detect retained foreign bodies when needed [3]. In line with the general management paradigm for traumatic injuries, managing PSCI differs between cases and is tailored based on injury severity, type of retained object, neurological complications, and associated injuries–notably abdominal, thoracic, and pelvic viscera involvement [1, 3, 9, 10]. In some instances, surgical strategies are of substantial importance, ranging from wound debridement to spine decompressive laminectomy and spine stabilization procedures [1, 9]. Similarly, conservative therapeutic modalities, such as prophylactic antibiotics, steroids, and blood pressure-controlling agents, play a substantial and inspirable role [3].
Due to the limited data on the current standard of care, further investigations are needed to guide best management strategies. This study reviews the current literature on PSCI, focusing on clinical characteristics, treatment strategies, and functional outcomes.
Methods
Literature search
A systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [11]. PubMed, Scopus, and Cochrane were searched from database inception to September 2021. A medical subject headings (MeSH) term and keyword search of each database were conducted using the Boolean operators OR and AND. Terms used were as follows: “penetrating OR missile OR non-missile” AND “spine OR spinal” AND “trauma OR injury”.
Study selection
Pre-established inclusion and exclusion criteria were defined. Studies were included if they met the following criteria: (1) retrospective or prospective studies on patients with PSCI; (2) patients aged 16 years or older; (3) available data on clinical features, management, and treatment outcomes. Studies were excluded if they: (1) were meta-analyses, reviews, editorials, letters, or books; (2) reported pediatric (<16 years) cases; (3), contained <5 cases; (4) contained insufficient clinical data, namely lacking one of the following: patient demographics or management details and outcomes; (5) were not written in English.
Although important in rare diseases such as PSCI, grey literature was not sought due to its difficulty to be identified. It is important to keep this in context, as the absence of grey literature may contribute to a potential selection bias.
Two authors (C.S and O.B.A) independently assessed titles and abstracts of all extracted papers based on the inclusion and exclusion criteria. Full texts of studies that met inclusion criteria were then further evaluated independently by the same two authors, and disagreements were resolved via a third author (A.S.H.). References of the included articles were also screened for additional relevant articles.
Data extraction
Data from included studies were extracted by two authors (L.B. and O.B.A.) and confirmed independently by one author (A.S.H) to ensure accuracy. Extraction variables included: authors, year, study design, sample size, age and gender, injury type, injury mechanism, injury level, American Spinal Cord Injury Association (ASIA) Impairment Scale at presentation and discharge, management strategy, treatment complications, post-treatment functional outcomes. Missing data are either not reported by the author or reported indistinctively with other data that could not be differentiated.
Data synthesis
The primary outcomes of interest were clinical features, management, and functional outcomes of patients with PSCI. The level of evidence of each article was evaluated following the 2011 Oxford Centre for Evidence-Based Medicine guidelines. The risk of bias was independently assessed for each article by two authors (P.P. and O.B.A.) using the Joanna Briggs Institute checklists for case series [12, 13].
Statistical analysis
The software R version 4.1.1 (RStudio, Inc. URL: http://www.R-project.org/; R Foundation for Statistical Computing, Vienna, Austria) was used for all statistical analyses. R metaphor package version 2.0–0 was used to conduct the meta-analysis. Continuous variables are summarized as medians or means and ranges, while categorical variables are summarized as frequencies and percentages. A meta-analysis of pooled data was done according to the types of study obtained using a random-effect model. A statistically significant difference was considered for bilateral P < 0.05 and for ratios not crossing the value of 1, which represents the value of no effect. Data from all studies were combined to estimate the odds ratio with 95% confidence intervals (CIs) for treatment strategy. The Higgins I2 test was used to assess between-study heterogeneity.
Results
Study selection
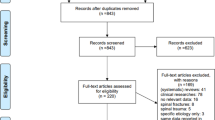
The initial literature search of PubMed, Scopus, and Cochrane databases yielded 2136 citations (Fig.1). After duplicate elimination, there were 1618 articles. A total of 1556 studies were excluded based on title and abstract. Sixty-two papers were sought for retrieval, but 4 articles were inaccessible. A total of 58 articles were evaluated for inclusion. Of the articles being assessed, 48 articles failed to meet our inclusion criteria and were subsequently excluded. Thus, a total of 10 articles categorized as levels IV were included based upon the pre-specified criteria [3, 14,15,16,17,18,19,20,21,22]. While one study included civilian and military injuries, 3 studies were conducted on civilian injuries only and 4 were conducted on military injuries only. However, one article did not specify the population or the injury setting (Table 1).
Risk of bias assessment resulted in a low risk of bias for all included studies (Supplementary Table 1). All articles had “good” quality, ranging 9–10, except for 2 papers that scored 8, due to unclear clinical picture and lacking demographic data [19, 21].
Demographics and clinical characteristics
Our results of 1754 patients with PSCI demonstrate a male predominance (88.9%) and a mean age of 19.2 years (range, 16 – 70) (Table 2). A total of 1623 (92.6%) had MSCI, and 131 (7.4%) had NMSCI. Gunshots were the most common cause of MSCI (N = 1416; 87.2%), followed by splinters (N = 161; 9.9%); however, the weapon for 46 (2.8%) cases were not specified. Knife stabs were the most common cause of NMSCI (N = 95; 72.5%), followed by screwdrivers (N = 4; 3.1%); however, the weapon for 32 (24.4%) cases was unspecified. The specific mechanism of injury was reported in 1653 cases. While the majority of injuries were reported as penetrating spinal cord injuries (N = 1576; 95.3%), a minority were referred as perforating spinal cord injuries (N = 77; 4.7%).
Among 635 patients with available data, a third (N = 218; 34.3%) had other associated injuries, mainly involving the abdomen (N = 77; 35.3%), chest (N = 76; 34.9%), and head and neck (N = 22; 10.1%). Among 264 patients with available data, 65 (24.6%) patients developed injury-related consequent complications, including, but not limited to, pressure ulcer (N = 20; 30.8%), neurogenic bladder (18; 27.7%), deep vein thrombosis/pulmonary embolism (N = 8; 12.3%), and pneumonia (N = 8; 12.3).
Survival data were available for 602 cases, showing that 41 (6.8%) patients had died at last follow-up. The cause of death varied and included pulmonary insufficiency (N = 12; 29.3%), renal failure (N = 6; 14.6%), and meningitis (N = 5; 12.1%), besides several other causes.
Management strategies: conservative vs. surgical
A total of 425 (28.0%) patients were treated surgically, while 1094 (72.0%) were managed conservatively (Table 3). Indications for surgery mainly included tissue contamination, spinal cord compression and instability, and exploration. On the other hand, medical treatment was mainly indicated for wound infection and hemodynamic instability. However, indications were generally reported without specifying the frequency of each indication. Missile injury was the most common injury type among the surgical (400, 94.1%) and conservative (1047, 95.7%) groups, with gunshot being the most common in both groups (69.6% Vs. 90.6%, respectively). A significantly higher rate of complete SCI (grade A in the ASIA score) was observed in the conservative group (602, 61.5%) compared with the surgical group (181, 49.1%) (P < 0.001). The thoracic spine was the most affected region among the surgical and conservative groups, yet at incomparable rates, with a higher rate among the conservative group (37.8 vs. 52.6; p < 0.001).
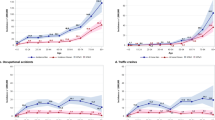
At admission, the rates of ASIA grades significantly differed among both groups (p < 0.001; Table 3; Fig. 2). The rates of ASIA grades for the surgical group were 49.2% for A, 23.9% for C, 13.3% for D, 12.8% for B, and 0.8% for E; while for the conservative group, they were 61.5% for A, 15.4% for C, 14.5% for B, 15.4% for D, and 0.7% for E. At discharge, the rate of ASIA grade A in the surgical group slightly decreased from 49.2% to 42.7% but remained the prevalent grade; while among the conservative group, the rate of ASIA grade A decreased greatly from 61.5% to 18.5%.
At last post-treatment follow-up, the surgical group had a significantly higher ASIA score improvement rate (41.5%) compared with the conservative group (20.5%), while the conservative group had a higher rate of patients who remained stable (79.1%) compared with the surgical group (56.1%) (p < 0.001).
By evaluating the efficacy of both treatment strategies (surgical vs. conservative), the meta-analysis (Fig. 3) showed that neither strategy displayed superior benefits in improving ASIA scores among complete SCIs (OR:0.7, 95% CI:0.3–1.64; I2 = 44%, p = 0.13) and incomplete SCIs (OR:1.15, 95% CI:0.64–2,06; I2 = 40%, p = 0.12).
Complication data for 284 cases of the surgical group were available (Fig. 2). Of which, 52 (18.3%) patients developed complications including CSF leaks/fistula 20 (38.5%), meningitis 18 (34.6%), and septic complications 6 (11.5%). Similarly, complication data were available for 278 cases among the conservative group. A total of 25 (8.9%) patients had complications, mainly including cerebrospinal fluid (CSF) leaks/fistula 7 (28%), meningitis 4 (16%), and pressure ulcer 3 (12%). However, most included articles did not clarify if these complications were trauma-related complications and consequences or treatment complications.
Discussion
PSCIs represent a group of devastating traumas typically characterized by forceful passage of a sharp object through the spinal column, resulting in neural injuries. Our results of 1754 patients showed that the rates of functional improvement are higher in patients managed with surgical treatments, but the meta-analysis failed to show significant superiority.
Demographics and clinical characteristics
In this review, most patients were young men with a mean age of 19.2 years. This differs from the general data on SCI, which mainly affects older patients (35.4 years). These results reflect the injury settings of PSCI, which mainly involve military combats and street fights. In contrast to blunt SCIs, PSCIs frequently result in concomitant injuries involving the abdominal and thoracic cavities, owing to their invading mechanisms involving multiple organs [5].
Among 635 cases with available data, we found that concomitant injuries were present in 218 (34.3%), highlighting the importance of timely prophylactic antimicrobial management. Several authors have discussed specific prophylactic antimicrobial treatment protocols, but controversies still exist. The majority recommend broad-spectrum antibiotics for patients who sustained missile and non-missile injury to the spine for at least 48 h, with a longer duration in patients with injuries to the intestine, especially the colon [6, 23,24,25].
The thoracic spine was the most commonly affected region in our cohort, contrary to the general data on all types of SCI reporting higher incidence rates of cervical spine injuries [1]. This difference likely derives from the fact that most SCI are of blunt origin, which preferentially involves the cervical spine.
Management strategies: conservative vs surgical
We found that rates of complete SCIs at patient admission time have decreased in both management groups, but more in the conservative group (from 61.5% to 18.5%) as compared with the surgical group (from 49.2% to 42.7%). Although this may suggest that conservative management may be more beneficial in patients with complete SCI, we presume that our findings may have been affected by patient selection bias, as surgical decompression would be pursued preferentially for severely injured patients, who are also less likely to improve.
Our pooled data showed that ASIA scores improved more in the surgical group (41.5%) compared with the conservative group (20.5%) (p < 0.001); however, the conservative group showed a higher stability rate (79.1%) than the surgical group (56.1%) (p < 0.001). These findings are comparable to another systematic review that examined all types of SCIs, inclusive of blunt and penetrating mechanisms [26]. The authors found that among complete SCIs, surgical management had a slightly less favorable ≥1 Grade improvement outcomes compared with the conservative group, showing an effect size of 18.4 (95% CI, 12.8–24.7) in the surgical group compared with an effect size of 20.6 (95% CI, 10.2–32.9) in the conservative group. This data highlights the importance of patient-tailored management planning, weighing expected benefits with potential complications, and pursuing surgical decompression strategies when appropriate.
We found a significant difference in ASIA grade improvement rates between the treatment strategies, but our meta-analysis failed to show any superior benefit of either modality in terms of score improvement. These results are consistent with another systematic review that examined treatment outcomes in patients affected by gunshot PSCIs limited to the lumbosacral spine, finding that surgical decompression was not associated with better neurological outcomes [25]. Although there has not been clear evidence to draw a meaningful conclusion, most authors agree that surgical intervention should be performed for only specific indications such as progressive neurological deficits, spine instability, persistent CSF leakage, and wound infection and exploration [14, 23, 27,28,29].
Among the surgical group, we observed more complications (18.3%) than in the conservative group (8.9%), consistent with the current understanding of the management strategies and their complication rates [27]. Despite our findings, insufficient data and major controversies still exist regarding the risk of complications, making it difficult to reach meaningful conclusions and correlations regarding complications following surgical and conservative management of PSCIs. In addition, most of our data did not explicitly indicate if the complications were injury-related or treatment-related. We assume that it almost impossible to eliminate the synergistic effect of the injury and attribute the complications to each specific management procedure irrespective of the patient’s overall condition prior to the management. Hence, more effort is needed to investigate the complication profile of patients with PSCIs, clearly describing the injury-related and procedure-related complications, along with patient functional status prior to their management.
Pathophysiology of PSCI
Spinal cord injury can be divided into primary and secondary (subsequent) injuries. Primary injury represents the initial mechanical damage to the microenvironment, including microvascular blood supply, leading to membrane ionic equilibrium and disruption to the neural and glial cell membranes [30]. A cascade of secondary injury then begins, causing permanent injury and dysfunction [31].
The secondary injury is divided based on chronicity into three groups: acute (within 48 h), subacute (2–14 days), intermediate (2–6 months), and chronic (more than six months) [32]. In each phase, different cellular mechanisms and molecular signals are involved. During the acute phase, the blood spinal cord barrier is disrupted, leading to an influx of cytokines and inflammatory cells [30]. Subsequently, apoptotic cell death is initiated, activating microglia to augment the inflammatory response and clear the cellular debris [33]. This process leads to edema formation, which marks the start of the subacute phase [34]. Progressing edema leads to a vicious cycle of further ischemic and cytotoxic injury [35]. Subsequently, intermediate and chronic phases are characterized by healing and scaring, including microvasculature growth, extracellular remodeling, and glial scar formation [30, 34, 36]. Then, ex vacuo cystic formation, which creates a barrier to cell migration and axonal repair, marks the end of the process [37, 38].
Of all phases, blunt SCI and PSCI differ in the initial phase of the primary injury. While both mechanisms start with blood supply blockage, the mechanical mechanisms of PSCI involve sharp, violent invasion, creating either direct vascular injury or neural injury [14, 39]. On the other hand, the blunt SCI involves a bony dislocation and firm compression of the microvasculature around the spinal cord [33, 34]. However, both modalities can lead to the initial ischemic injury, resulting in cellular wall injury, iconic disequilibrium, and secondary injury initiation.
Limitations
Our study has several limitations mainly due to the heterogeneous data available among our included studies, such as demographics, functional assessments, and complications. Some articles did not explicitly specify whether complications are injury-related or management-related, and most did not clearly report patient status prior to their treatment. Therefore, the synergistic effect of the injury on patient outcomes could not be eliminated. Moreover, many patients were lost at follow-up, limiting our meta-analysis and likely decreasing the statistical power of our conclusions.
Conclusion
PSCIs pose a severe burden, while ideal management strategies still require further evidence. Although neither strategy proved to be statistically superior, each strategy is meant for specific indications, and in most instances, they are inseparable elements of the management paradigm. Hence, patient-tailored management and careful selection of surgical cases is warranted.
Data availability
Data were generated using the included articles’ reported data. Data are available from the corresponding author on reasonable request.
References
Morrow KD, Podet AG, Spinelli CP, Lasseigne LM, Crutcher CL, Wilson JD, et al. A case series of penetrating spinal trauma: Comparisons to blunt trauma, surgical indications, and outcomes. Neurosurg Focus. 2019;46:E4. https://doi.org/10.3171/2018.12.FOCUS18577.
Pedram H, Reza ZM, Reza RM, Vaccaro AR, Vafa RM. Spinal fractures resulting from traumatic injuries. Chin J Traumatol. 2010;13:3–9. https://doi.org/10.3760/cma.j.issn.1008-1275.2010.01.001.
Seroto PM, Harrington BM, Lombard C, Vlok AJ. The role of tertiary neurosurgical intervention in non-missile penetrating injuries of the spine. Eur Spine J. 2021;30:1397–401.
Hurlbert RJ. Editorial. penetrating spinal trauma: snapshot of the American epidemic. Neurosurg Focus FOC. 2019;46:E5.
Blair JA, Possley DR, Petfield JL, Schoenfeld AJ, Lehman RA, Hsu JR, et al. Military penetrating spine injuries compared with blunt. Spine J. 2012;12:762–8.
Iqbal N, Sharif S, Hafiz M, Ullah Khan A. Gunshot spinal injury: factors determining treatment and outcome. World Neurosurg. 2018;114:e706–e712.
Roach MJ, Chen Y, Kelly ML. Comparing blunt and penetrating trauma in spinal cord injury: analysis of long-term functional and neurological outcomes. Top Spinal Cord Inj Rehabil. 2018;24:121–32.
Scientific, Educational Abstracts, and Case-of-the-Day Presented at the ASER 2014 Annual Scientific Meeting and Postgraduate Course September 10–13, Portland, Oregon. Emerg Radiol. 2014;21:431–71.
Klimo PJ, Ragel BT, Rosner M, Gluf W, McCafferty R. Can surgery improve neurological function in penetrating spinal injury? a review of the military and civilian literature and treatment recommendations for military neurosurgeons. Neurosurg Focus. 2010;28:E4.
Gheban BA, Rosca IA, Crisan M. The morphological and functional characteristics of the pineal gland. Med Pharm Rep. 2019;92:226–34.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372. https://doi.org/10.1136/bmj.n71.
Joanna Briggs Institute Case Series. Checklist for Case Series. Joanna Briggs Inst. Crit. Apprais. tools use JBI Syst. Rev. 2017; 1–6.
Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, et al. The Oxford 2011 Levels of Evidence. Oxford Centre Evidence-Based Medicine. 2011.
Abbas A, Aziz HF, Rizvi R, Rehaman L, Javeed F, Afzal A, et al. Gunshot acquired spinal cord injury in civilians. Turk Neurosurg. 2019;29:506–12.
Kelly ML, Roach MJ, Nemunaitis G, Chen Y. Surgical and Nonsurgical Treatment of Penetrating Spinal Cord Injury: Analysis of Long-term Neurological and Functional Outcomes. Top Spinal Cord Inj Rehabil. 2019;25:186–93.
Waters RL, Sie I, Adkins RH, Yakura JS. Motor recovery following spinal cord injury caused by stab wounds: A multicenter study. Paraplegia. 1995;33:98–101.
Benzel EC, Hadden TA, Coleman JE. Civilian gunshot wounds to the spinal cord and cauda equina. Neurosurgery. 1987;20:281–5.
Robertson DP, Simpson RK. Penetrating injuries restricted to the cauda equina: a retrospective review. Neurosurgery. 1992;31:265–70.
Aarabi B, Alibaii E, Taghipur M, Kamgarpur A. Comparative study of functional recovery for surgically explored and conservatively managed spinal cord missile injuries. Neurosurgery. 1996;39:1133–40.
Kahraman S, Gonul E, Kayali H, Sirin S, Duz B, Beduk A, et al. Retrospective analysis of spinal missile injuries. Neurosurg Rev. 2004;27:42–45.
Bhatoe HS, Singh P. Missile injuries of the spine. Neurol India. 2003;51:507–11.
Rathore FA, Ayub A, Farooq S, New PW. Suicide bombing as an unusual cause of spinal cord injury: a case series from Pakistan. Spinal Cord. 2011;49:851–4.
Crutcher CL II, Wilson JM, DiGiorgio AM, Fannin ES, Shields JA, Morrow KD, et al. Minimally invasive management of civilian gunshot wounds to the lumbar spine: A case series and technical report. Oper Neurosurg. 2020;19:219–25.
Heary RF, Vaccaro AR, Mesa JJ, Balderston RA. Thoracolumbar infections in penetrating injuries to the spine. Orthop Clin North Am. 1996;27:69–81.
Platt A, Dafrawy MH EL, Lee MJ, H Herman M, Ramos E, et al. Gunshot Wounds to the Lumbosacral Spine: Systematic Review and Meta-Analysis. Glob spine J. 2021;21925682211030870. https://pubmed.ncbi.nlm.nih.gov/34275384/
Khorasanizadeh M, Yousefifard M, Eskian M, Lu Y, Chalangari M, Harrop JS, et al. Neurological recovery following traumatic spinal cord injury: a systematic review and meta-analysis. J Neurosurg Spine 2019;30:683–99.
Bumpass DB, Buchowski JM, Park A, Gray BL, Agarwal R, Baty J, et al. An Update on Civilian Spinal Gunshot Wounds: Treatment, Neurological Recovery, and Complications. Spine. 2015;40:450–61.
Bono CM, Heary RF. Gunshot wounds to the spine. Spine J. 2004;4:230–40.
Lawless MH, Lytle EJ, McGlynn AF, Engler JA. Surgical management of penetrating spinal cord injury primarily due to shrapnel and its effect on neurological outcome: a literature review and meta-analysis. J Neurosurg Spine. 2018;28:63–71.
Ahuja CS, Wilson JR, Nori S, Kotter MRN, Druschel C, Curt A, et al. Traumatic spinal cord injury. Nat Rev Dis Prim. 2017;3:17018.
Schwartz G, Fehlings MG. Secondary injury mechanisms of spinal cord trauma: a novel therapeutic approach for the management of secondary pathophysiology with the sodium channel blocker riluzole. Prog Brain Res. 2002;137:177–90.
Badhiwala JH, Ahuja CS, Fehlings MG. Time is spine: a review of translational advances in spinal cord injury. J Neurosurg Spine. 2018;30:1–18.
Choo AM, Liu J, Lam CK, Dvorak M, Tetzlaff W, Oxland TR, et al. Contusion, dislocation, and distraction: primary hemorrhage and membrane permeability in distinct mechanisms of spinal cord injury. J Neurosurg Spine. 2007;6:255–66.
LaPlaca MC, Simon CM, Prado GR, Cullen DK. CNS injury biomechanics and experimental models. Prog Brain Res. 2007;161:13–26.
Li S, Mealing GA, Morley P, Stys PK. Novel injury mechanism in anoxia and trauma of spinal cord white matter: glutamate release via reverse Na+-dependent glutamate transport. J Neurosci. 1999;19:RC16.
Kwon BK, Tetzlaff W, Grauer JN, Beiner J, Vaccaro AR. Pathophysiology and pharmacologic treatment of acute spinal cord injury. Spine J. 2004;4:451–64.
Cafferty WBJ, Duffy P, Huebner E, Strittmatter SM. MAG and OMgp synergize with Nogo-A to restrict axonal growth and neurological recovery after spinal cord trauma. J Neurosci. 2010;30:6825–37.
Chen MS, Huber AB, van der Haar ME, Frank M, Schnell L, Spillmann AA, et al. Nogo-A is a myelin-associated neurite outgrowth inhibitor and an antigen for monoclonal antibody IN-1. Nature. 2000;403:434–9.
Stefanopoulos PK, Soupiou OT, Pazarakiotis VC, Filippakis K. Wound ballistics of firearm-related injuries—part 2: mechanisms of skeletal injury and characteristics of maxillofacial ballistic trauma. Int J Oral Maxillofac Surg. 2015;44:67–78.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The study idea was proposed by [Othman Bin Alamer, MBBS] and [Ali S. Haider, BS]. The literature search, articles screen, and data extraction were perfumed by [Caren Stuebe, MSc], [Paolo Palmisciano, MD], [Lokeshwar S. Bhenderu, BS], [Navraj S. Sagoo, MD], [Maryam Haider, MD], and [Ali S. Haider, BS]. Data analysis was performed by [Othman Bin Alamer, MBBS]. The manuscript was drafted by [Othman Bin Alamer, MBBS]. All authors critically revised and edited the first draft and commented on all versions of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bin-Alamer, O., Bhenderu, L.S., Stuebe, C. et al. Penetrating spinal cord injury: a systematic review and meta-analysis of clinical features and treatment outcomes. Spinal Cord 60, 845–853 (2022). https://doi.org/10.1038/s41393-022-00813-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00813-x