Abstract
Study design
Cross-sectional survey.
Objectives
The objective of the study was to identify the treatments that people with traumatic spinal cord injury (SCI) used for their non-neuropathic pains (nonNeuPs) and how they subjectively rated the helpfulness of those treatments.
Setting
Six centers from the Spinal Cord Injury Model Systems.
Methods
Three hundred ninety one individuals who were at least 1-year post-traumatic SCI were enrolled. A telephone survey was conducted for pharmacologic and non-pharmacologic treatments utilized in the last 12 months for each participant’s three worst pains and the perceived helpfulness of each treatment for each pain.
Results
One hundred ninety (49%) participants reported at least one nonNeuP (Spinal Cord Injury Pain Instrument score < 2) in the previous 7 days. NSAIDs/aspirin, acetaminophen, opioids, and cannabinoids were the most commonly used and helpful pharmacologic treatments for overall nonNeuP locations (helpful in 77–89% of treated pains). Body position adjustment, passive exercise, massage, resistive exercise, and heat therapy were reported as the most commonly used non-pharmacological treatments for nonNeuPs. Heat therapy, aerobic exercise, massage, and body position adjustment were the most helpful non-pharmacological treatments for overall nonNeuP locations (helpful in 71–80% of treated pains). Perceived helpfulness of treatments varied by pain locations, which may be due to different mechanisms underlying pains in different locations.
Conclusions
Results of the study may help guide clinicians in selecting pain-specific treatments for nonNeuPs. The self-reported helpfulness of heat therapy, exercise, and massage suggests a possible direction for clinical trials investigating these treatments of nonNeuP while limiting the side effects accompanying pharmacologic treatments.
Similar content being viewed by others
Introduction
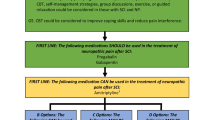
About 70% of individuals with spinal cord injury (SCI) have ongoing pain [1, 2]. Of those with ongoing pain after SCI, over half feel pain interferes with their activities of daily living including work [3]. Pain after SCI can be classified into two main pain types: neuropathic (NeuP) and non-neuropathic pain (nonNeuP). Different pain types have different pain generators and pathologies. Clinicians should identity the pain type first and then tailor a treatment to that specific pain. NonNeuP, especially the nociceptive pains (musculoskeletal pain and visceral pain) [4, 5], is common after SCI. Approximately 60% of individuals report ongoing musculoskeletal pain; no other pain type is more prevalent [6,7,8].
For many people, SCI-related chronic neuropathic pain is often refractory to treatment [9,10,11], while nonNeuPs may be more amenable to reduction via currently-available treatments. The general approach to treatments of nonNeuP for individuals with SCI is similar to that used for those without an SCI: either by treating the pain generating mechanisms directly or by amelioration of aggravating conditions, such as those related to poor position or posture and overuse [12,13,14,15]. The most common locations for ongoing musculoskeletal pains, as reported by approximately half of individuals with SCI, are the shoulder and back [16, 17].
Nevertheless, the observation that pains are prevalent at all times post injury [18] indicates that effective treatment options may be lacking, or are difficult to implement. There are few treatments for musculoskeletal pain, especially shoulder pain, that have been evaluated in those with SCI using high-quality randomized clinical trials [19, 20]. A few treatments have been evaluated using less rigorous methodologies such as matched cohort trials and controlled trials with small sample sizes, but the majority of evidence published on treatment effectiveness for nonNeuP in this population is in the form of case series or reports. Two randomized controlled trials indicated that a 12-week, home-based program of shoulder strengthening and stretching exercises plus optimal movement strategies, such as transfer and wheelchair skills, could be effective on reducing shoulder pain for individuals with SCI [21, 22]. A small randomized controlled trial showed that acupuncture reduced chronic shoulder pain, although the study also found that invasive sham acupuncture reduced shoulder pain [23]. Previous studies discussing the effects of pharmacological treatments on chronic pain for individuals with SCI [1, 20, 24] either focused on neuropathic pain or did not classify pain types and locations. Pharmacological treatments usually have short-term effects with other side effects [20]. For example, corticosteroid injection has a short-term pain-relief effect on shoulder pain but may weaken adjacent tendons [25]. NSAIDs and acetaminophen are often used on treating SCI-related pain [26, 27], but there are currently no published studies reporting their efficacy on treating SCI-related nonNeuPs. NSAIDs could affect bone metabolism and are often avoided during the first few months after spinal fusion surgery [28].
Given the paucity of evidence from studies supporting the effectiveness of treatments for nociceptive pains after SCI, another approach that can be useful in determining effective treatments, is to survey individuals with SCI to identify the treatments they report to be most helpful. Cardenas and Jensen and Widerström-Noga and Turk each conducted cross-sectional pain surveys in the early 2000’s [29, 30]. However, these surveys were administered when there was not an agreed-upon standard for pain classification after SCI. Thus, their results applied to pain in general, across heterogeneous pain types, making it difficult to differentiate treatment effects for different pain types (e.g., neuropathic, nociceptive, other) [29, 30]. Nevertheless, certain of their findings are notable. They both mentioned that opioids were reported by participants to be the most effective pharmacological treatments, and massage was the most effective non-pharmacological treatment [29, 30].
The purpose of this investigation was to learn what specific treatments, including pharmacological and non-pharmacological treatments, people with traumatic SCI used for nonNeuP. We investigated the treatments used for not only overall nonNeuP but for nonNeuP that has been identified as originating from specific anatomic locations, such as the shoulder and lower back. An additional purpose was to determine how individuals subjectively rated the helpfulness of these treatments for their pain. We hypothesized that certain non-pharmacological treatments targeted to specific locations of nonNeuP would be as helpful as pharmacological treatments, some of which (e.g., opioids) have negative side effects including addiction and tolerance [31,32,33,34,35,36]. This study used a survey method to address the limitations of previous studies by looking at distinct pain types (NeuP and nonNeuP) rather than pain after SCI in general, and also to expand the survey cohort to include a more geographically diverse group of individuals. Moreover the survey included the full range of potential pharmacologic and non-pharmacologic interventions thought to be comprehensive by experts in the field [37]. The results of this survey related to perceived helpfulness of different treatments could provide a reference for future research directions and clinical applications related to nonNeuP management for individuals with SCI.
Methods
This was a cross-sectional survey study of a subset of participants of the Spinal Cord Injury Model System (SCIMS) program [38]. Participants needed to be 18 years or older, at least 1-year post-traumatic SCI, and previously enrolled in one of the six participating SCIMS centers in the United States (for detailed inclusion/exclusion criteria for enrolling in SCIMS database, please refer to the review of SCIMS program [38]). Participants were recruited to participate in this pain survey study during their scheduled follow-up SCIMS interviews as part of the main SCIMS program between March 2017 and July 2019. If participants were willing to answer this pain survey, they were enrolled in this study, and the survey was completed by phone interview. At the beginning of the survey, participants were asked if they had any pain during the last 7 days. If yes, they would be further asked to report up to three worst pains they had during the last 7 days. The survey included the International Spinal Cord Injury Pain Basic Data Set (Version 2.0) [39], to document each worst pain location, intensity (0–10), and interference (for up to the three worst pains) during the past 7 days. The Spinal Cord Injury Pain Instrument (SCIPI) also was included in the survey and was used to differentiate pain types. In this study, we focused on participants’ nonNeuPs (SCIPI score <2) [5]. Participants’ nonNeuPs were categorized based on common pain locations, including the shoulder, elbow (elbow alone or elbow plus forearm), wrist, upper back, lower back, hip, and knee, as well as at less common areas including the throat, neck, hand/fingers, chest, abdomen, pelvis/genitalia, buttocks, anus, shin, calf, ankle, and foot/toes. Participants’ demographic and SCI characteristics, including age, time since injury, neurological level of injury, and ASIA Impairment Scale, were also collected.
The survey also included the “Treatments” section of the International Spinal Cord Injury Pain Extended Data Set (ISCIPEDS, Version 1.0) [37] to document treatments used over the last 12 months (Supplementary Table). The treatment section in the survey included specific pharmacologic and non-pharmacologic treatments as well as an “other” category permitting participants to describe additional treatments that they used but that were not listed in ISCIPEDS (Supplementary Table). First, participants would answer Yes/No to “Have you used this treatment for pain during the past 12 months?”. If yes, the perceived helpfulness of the treatment to each of their pains would be assessed by recording participants’ answers (Yes/No/Uncertain) to “Was the treatment helpful for your worst/second worst/third worst pain?” (three separate questions) respectively.
Statistical analysis
Pharmacological and non-pharmacological treatments participants used in the past 12 months for each nonNeuP were identified and used for the present analysis. Descriptive statistics, including mean, standard deviation (SD), and percentage, were used to characterize participants’ demographic information and the treatments they used for each of their nonNeuPs in the previous 12 months. Helpfulness of pharmacologic and non-pharmacologic treatments was ranked by the percentage of individuals who received that treatment during the past 12 months and answered “yes” to the question “Was the treatment helpful for your pain? Yes/No/Uncertain”. Because a wide variety of treatments were listed in the survey, and many of them were only used by a few of our participants (small sample size), we only reported the treatments endorsed by more than ten participants with nonNeuP. Because each participant had a different number of pains and used different types of treatments respectively or together to treat his/her pain(s) (mixed data set), which may violate assumptions of many statistical tests, descriptive statistics alone were determined to be the most appropriate for this study.
Results
Participant demographics
Of the total 391 participants enrolled in the study, 190 (49%) participants reported at least one nonNeuP during the previous 7 days. Approximately 76% of participants with nonNeuP were male, 49% had paraplegia, and 43% had complete SCI (Table 1).
Pain types
Participants reported a cumulative total of 652 differentiated pain problems. Among all the pain problems reported as present during the past 7 days, 298 of them were nonNeuPs (SCIPI <2) representing 46% of total pains characterized. The most commonly reported nonNeuP locations were shoulders, lower back, other, knee, upper back, and hip as detailed in Table 2. Additionally, 127 participants indicated that their worst pain was nonNeuP, with the most common worst pain locations identified as shoulder, lower back, and upper back repectively (Table 2).
The numbers shown in Table 2 were based on the number of nonNeuP problems. Because some participants had more than one shoulder or lower back nonNeuP, we also reported the number of participants here to provide a reference for future studies and for comparison with previous studies. Sixty-nine participants had at least one shoulder nonNeuP (18% of total participants and 36% of the participants with nonNeuP) during the previous 7 days. Forty-three participants had at least one lower back nonNeuP (11% of total participants and 23% of the participants with nonNeuP). Twenty-nine (7% of total), twenty-nine (7% of total), and twenty-five (6% of total) participants had at least one upper back, knee, and hip nonNeuPs respectively.
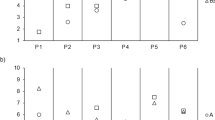
Pharmacologic treatments
Based on our study results, the most commonly used pharmacological treatments for nonNeuPs are, in descending order of prevalence, NSAIDs/Aspirin (n = 135, 71% of participants with nonNeuP), acetaminophen (n = 89, 47%), opioids (n = 84, 44%), antiepileptics (n = 82, 43%), and cannabinoids (n = 71, 37%). The pharmacological treatments reported to be most helpful for overall nonNeuPs are, in descending order of reported effectiveness, opioids (89% of opioid-treated nonNeuPs), acetaminophen (80%), NSAIDs/aspirin (79%), and cannabinoids (77%) (Table 3).
Further analyses of specific pain locations and their corresponding pharmacological treatments show that opioids, acetaminophen, and NSAIDs/aspirin were subjectively rated by participants as the most helpful pharmacologic treatments for shoulder, upper back, lower back, and knee pains (helpful in 79–100% of the pharmacologically treated pains, Table 3). NSAIDs/aspirin were helpful in 69% of NSAIDs/aspirin treated hip pains, but this perceived helpfulness rate was the lowest compared to the other common nonNeuP locations treated with NSAIDS/aspirin.
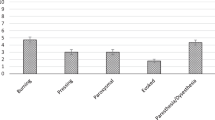
Non-pharmacological treatments
Body position adjustment (n = 148, 78% of participants with nonNeuP), passive exercise (n = 141, 74%), massage (n = 88, 46%), resistive exercise (n = 56, 29%), and heat therapy (n = 55, 29%) were the most commonly used non-pharmacological treatments for nonNeuPs. The non-pharmacological treatments reported to be most helpful for overall nonNeuP locations were heat therapy (80% of heat therapy-treated nonNeuPs), aerobic exercise (80%), massage (77%), and body position adjustment (71%), all of which were helpful for more than 70% of treated nonNeuPs (Table 3).
Heat therapy, massage, resistive exercise, passive exercise, and aerobic exercise were the most helpful non-pharmacological treatments for shoulder pain (helpful for 79% or more of non-pharmacologically treated pains, Table 3). The most helpful non-pharmacological treatment for upper back, lower back, and hip pains was body position adjustment (helpful for 79% or more of treated pains, see Table 3). As for knee pain, our results indicated that none of the non-pharmacological treatments were as helpful as the most helpful pharmacological treatments. Massage was the most helpful non-pharmacological treatment for knee pains (Table 3).
Comparisons between pharmacological and non-pharmacological treatments
Pharmacological treatments seem to have better effects on overall nonNeuPs (top three ranked helpfulness ranges from 79 to 89%, Table 3) compared to non-pharmacological treatments (77 to 80%). However, for treating shoulder nonNeuP, heat therapy and massage had comparable perceived helpfulness (91%) to acetaminophen (93%) and better helpfulness than opioids (86%) (Table 3). For treating hip nonNeuP, body position adjustment had better perceived helpfulness (82%) than NSAIDs (69%), which is the only helpful pharmacological treatment endorsed by more than ten participants for hip nonNeuP (Table 3).
Discussion
This study reports the perceived helpfulness of a wide range of individual treatments on specific nonNeuP locations, rather than on pain after SCI in general (i.e., combined NeuP and nonNeuP pain types and across anatomical regions). Opioids, acetaminophen, and NSAIDs/aspirin were reported as both the most commonly used and most helpful pharmacological treatments for all nonNeuPs regardless of location. Previous studies have shown that NSAIDs, acetaminophen, and opioids are the most common medications used in clinics to treat musculoskeletal pains [40, 41], but no studies have discussed their reported effectiveness. Our study results indicated that the use of NSAIDs, acetaminophen, and opioids may help treat nonNeuPs for individuals with SCI. For over 79% of the nonNeuPs, excluding those located at the hip, treatment using these three pharmacological agents was reported as helpful for their pain. However, opioids have significant side effects including physical dependence, respiratory depression, and addiction [42], which was not assessed in this study. For shoulder and lower back pains, the most common nonNeuP locations, acetaminophen was more helpful than opioids for pain relief based on participants’ report (Table 3), and acetaminophen has fewer and less significant side effects. NSAIDs was as helpful as opioids for upper back nonNeuPs as well (Table 3).
NSAIDs were the only pharmacological agent commonly used by participants to treat hip nonNeuPs. The perceived helpfulness of NSAIDs in the treatment of hip nonNeuPs was 69%, which was lower than the helpfulness of NSAIDs at other nonNeuP locations, including the shoulders, upper and lower back, and knees (Table 3, range from 79 to 100%). Interestingly, body position adjustment was commonly used by the participants with hip nonNeuP and was reported as helpful in 82% of those employing this method (Table 3). Body position adjustment may therefore be better for treating hip nonNeuP than commonly used pharmacological treatments which often have side effects. Few studies in the literature discuss hip nonNeuPs in individuals with SCI and, when mentioned, pains related to hip heterotopic ossification (HO) [43] and pressure injuries which often occur at the greater trochanters [44] are what is usually being referenced. In the present study, the percentages of individuals with complete SCI (43%) were higher than the aggregate percentage of individuals in the SCIMS database with complete SCI (32%) [45]. Complete SCI is one of the major risk factors for developing both HO and greater trochanteric pressure injury [46, 47]. Hip HO lacks a highly effective treatment [48, 49]. Mature HO of the hip joint(s) often leads to imbalance in sitting (posture), limited hip range of motion, and limitations in performance of seated functional activities [48, 50]. A few case reports indicate that seating and positioning adjustments can provide persons with HO improved seated stability, facilitating functional activities, as well as reducing pain [51, 52]. An ideal seating and sleeping position is also critical for the prevention of pressure injuries [44]. Studies have shown that appropriate cushioning, wheelchair measurements, and tilt and recline functions could effectively manage pressure to prevent pressure injuries [53, 54].
The survey by Cardenas and Jensen investigating treatments for pain in individuals with chronic SCI, indicated that strengthening exercises, physical therapy, heat, ROM exercise, and massage were the most commonly used non-pharmacological treatments, with massage reported as the most effective [29]. The survey by Widerström-Noga and Turk also indicated that massage, heat, and physical therapy were the most commonly used non-pharmacological treatments for general chronic pain after SCI [30]. Our study indicated that heat, aerobic exercise, massage, and body position adjustment were the most common and helpful non-pharmacological treatments for nonNeuPs. Even though the specific results of the present study and previous studies were slightly different, heat therapy and massage were shown to be more helpful than other non-pharmacological treatments in all the studies. Physical therapy, if encompassing the treatments rated most helpful here, including strengthening, aerobic, and ROM exercises, could also play an important role in an effective treatment program for nonNeuPs after SCI.
Compared to previous survey studies [29, 30], this present study had more participants (current 391 vs. previous 117 and 120) and categorized participants’ pains into NeuPs and nonNeuPs. Among the participants with nonNeuP, the gender distribution matches the data from SCIMS database (80% male and 20% female) [45], but the percentages of individuals with paraplegia (49%) and complete SCI (43%) were higher than the aggregate percentage of individuals in the SCIMS database with paraplegia (40%) and complete SCI (32%) [45]. The relatively high percentage of individuals with paraplegia in this study may be the reason that we had lower percentage of participants reporting ongoing nonNeuP (49%) compared to previous studies (60%) [6,7,8]. A previous study indicated that individuals with tetraplegia had almost twice the risk of experiencing upper extremity musculoskeletal pains when compared to those with paraplegia [55]. The study participants were enrolled from SCIMS participants, not from general population, which may influence the generalization of the study results.
One of the strengths of the present study is that we linked the nonNeuP to the location where the pain was perceived thereby better defining the general anatomic pain generators in a large cohort of individuals. We then linked these anatomic pain generators to specific treatments used for those pains. For shoulder nonNeuPs due to musculoskeletal injuries, including rotator cuff tears, tendinosis, and muscle strength imbalance [12,13,14], the literature has shown that strengthening, stretching, and aerobic exercises as well as wheelchair skills and transfer training can effectively improve shoulder pain [21, 22, 56, 57]. The present survey study further supports those study findings. Besides analgesic medication (NSAIDs, acetaminophen, and opioids), resistive, passive, and aerobic exercise were additionally rated as the most helpful treatments. Even though heat therapy and massage were rated as helpful treatments for shoulder nonNeuPs in this survey study, few studies with low-level evidence have previously supported their efficacy for treating shoulder pain [58,59,60,61]. More high-quality studies are needed to evaluate the effects of heat therapy and massage on shoulder nonNeuPs.
The most helpful non-pharmacological treatment for upper and lower back pains was found to be body position adjustment, which may reduce pain by correcting a participant’s posture in a wheelchair or bed. Poor posture and positioning in sitting or lying is a major contributor to upper and lower back pains in persons with SCI [15]. As for knee pain, our results indicated that none of the non-pharmacological treatments were as helpful as the pharmacological treatments of NSAIDs/aspirin and acetaminophen.
Study limitations
There are several limitations of this study. The assignment of broad pain types, NeuP versus nonNeuP, defined by the SCIPI screening tool, is not completely sensitive and specific [5]. Some pharmacological treatments, such as cannabinoids and opioids, may have legality issues for some individuals depending on where individuals reside. These participants may be reluctant to report use of these controversial pharmacological treatments. Some specific pain location treatment results were based upon small sample sizes. As most participants used more than one treatment for their different nonNeuPs, the data were mixed with statistically independent and paired data (some data from the same individuals but some from different individuals). As such, in this current study we used descriptive statistics to present the subjective survey results. Participants may not accurately recall all of the treatments they used during the previous 12 months. Also if a participant had been treated with a specific pharmacologic or non-pharmacologic treatment, prior to the year where they were surveyed and did not feel the treatment was helpful, this information would not be incorporated into the data, leading to inflation of the helpfulness for any particular treatment. Conversely, if they had been treated in the past with a specific treatment and that pain was no longer present at the time of interview, the treatment helpfulness of that particular intervention would not be captured. The study also did not document how long treatments were used and helpfulness lasted. Finally, as some individuals had more than one nonNeuP, and each pain was rated separately with regard to each intervention being helpful, the number of times a particular treatment was thought to be helpful may have been overcounted. Previous studies related to SCI pain screening, classification, and treatments all rated each participant’s pains separately [5, 30] and assumed that each participant could identify the differences of pains at each pain location.
Conclusion
The study results indicate that analgesic medications, such as NSAIDs, acetaminophen, and opioids, are perceived as helpful pharmacological treatments across nonNeuP locations. For treating shoulder pain specifically, heat therapy, massage, and strengthening programs seem to provide the most helpful non-pharmacological treatment effects. For treating upper and lower back and hip pain, body position adjustment also seems to be helpful, especially for hip pain. As for treating knee pain, pharmacological treatments, such as NSAIDs and acetaminophen, may be more helpful than non-pharmacological treatments. Acetaminophen and NSAIDs combined with some helpful non-pharmacologic treatments, such as heat, massage, exercise, and body position adjustment, could be recommended to potentially replace/reduce opioid use for pain relief. The results of the study from a consumer’s perspective provide guidance for future research in terms of developing clinical trials to obtain more empirical evidence for various nonNeuP treatments. For example, randomized controlled trials to see if some non-pharmacologic treatments with high self-reported helpfulness ratings could produce better or similar treatment effects for nonNeuPs than opioids for instance which have severe adverse side effects.
Data availability
The data generated and analyzed during the current study are available through the SCIMSs upon request.
References
Hadjipavlou G, Cortese AM, Ramaswamy B. Spinal cord injury and chronic pain. BJA Educ. 2016;16:264–8.
Dijkers M, Bryce T, Zanca J. Prevalence of chronic pain after traumatic spinal cord injury: a systematic review. J Rehabil Res Dev. 2009;46:13–29.
Cardenas DD, Bryce TN, Shem K, Richards JS, Elhefni H. Gender and minority differences in the pain experience of people with spinal cord injury. Arch Phys Med Rehabil. 2004;85:1774–81.
Dijkers MP, Bryce TN. Introducing the International Spinal Cord Injury Pain (ISCIP) Classification. Pain Manag. 2012;2:311–4.
Bryce TN, Richards JS, Bombardier CH, Dijkers MP, Fann JR, Brooks L, et al. Screening for neuropathic pain after spinal cord injury with the spinal cord injury pain instrument (SCIPI): a preliminary validation study. Spinal Cord. 2014;52:407–12.
Finnerup NB, Jensen MP, Norrbrink C, Trok K, Johannesen IL, Jensen TS, et al. A prospective study of pain and psychological functioning following traumatic spinal cord injury. Spinal Cord. 2016;54:816–21.
Finnerup NB, Norrbrink C, Trok K, Piehl F, Johannesen IL, Sorensen JC, et al. Phenotypes and predictors of pain following traumatic spinal cord injury: a prospective study. J Pain. 2014;15:40–8.
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003;103:249–57.
Felix ER. Chronic neuropathic pain in SCI: evaluation and treatment. Phys Med Rehabil Clin N Am. 2014;25:545–71. viii.
Warms CA, Turner JA, Marshall HM, Cardenas DD. Treatments for chronic pain associated with spinal cord injuries: many are tried, few are helpful. Clin J Pain. 2002;18:154–63.
Attal N, Cruccu G, Baron R, Haanpää M, Hansson P, Jensen TS, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17:1113–e88.
Kentar Y, Zastrow R, Bradley H, Brunner M, Pepke W, Bruckner T, et al. Prevalence of upper extremity pain in a population of people with paraplegia. Spinal Cord. 2018;56:695–703.
Patel RM, Gelber JD, Schickendantz MS. The weight-bearing shoulder. J Am Acad Orthop Surg. 2018;26:3–13.
Sirasaporn P, Saengsuwan J, Vichiansiri R. Ultrasonographic findings of shoulders in individuals with spinal cord injury. J Spinal Cord Med. 2019:1–7.
Turner JA, Cardenas DD, Warms CA, McClellan CB. Chronic pain associated with spinal cord injuries: a community survey. Arch Phys Med Rehabil. 2001;82:501–9.
Akbar M, Brunner M, Balean G, Grieser T, Bruckner T, Loew M, et al. A cross-sectional study of demographic and morphologic features of rotator cuff disease in paraplegic patients. J Shoulder Elb Surg. 2011;20:1108–13.
Michailidou C, Marston L, De Souza LH, Sutherland I. A systematic review of the prevalence of musculoskeletal pain, back and low back pain in people with spinal cord injury. Disabil Rehabil. 2014;36:705–15.
Modirian E, Pirouzi P, Soroush M, Karbalaei-Esmaeili S, Shojaei H, Zamani H. Chronic pain after spinal cord injury: results of a long-term study. Pain Med. 2010;11:1037–43.
Boldt I, Eriks-Hoogland I, Brinkhof MW, de Bie R, Joggi D, von Elm E. Non-pharmacological interventions for chronic pain in people with spinal cord injury. Cochrane Database Syst Rev. 2014;11:Cd009177.
Teasell RW, Mehta S, Aubut J-AL, Foulon B, Wolfe DL, Hsieh JTC, et al. A systematic review of pharmacologic treatments of pain after spinal cord injury. Arch Phys Med Rehabil. 2010;91:816–31.
Mulroy SJ, Thompson L, Kemp B, Hatchett PP, Newsam CJ, Lupold DG, et al. Strengthening and optimal movements for painful shoulders (STOMPS) in chronic spinal cord injury: a randomized controlled trial. Phys Ther. 2011;91:305–24.
Cardenas DD, Felix ER, Cowan R, Orell MF, Irwin R. Effects of home exercises on shoulder pain and pathology in chronic spinal cord injury: a randomized controlled trial. Am J Phys Med Rehabil. 2020;99:504–13.
Dyson-Hudson TA, Kadar P, LaFountaine M, Emmons R, Kirshblum SC, Tulsky D, et al. Acupuncture for chronic shoulder pain in persons with spinal cord injury: a small-scale clinical trial. Arch Phys Med Rehabil. 2007;88:1276–83.
Kupfer M, Formal CS. Non-opioid pharmacologic treatment of chronic spinal cord injury-related pain. J Spinal Cord Med. 2020:1–10.
Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet. 2010;376:1751–67.
Wiffen PJ, Knaggs R, Derry S, Cole P, Phillips T, Moore RA. Paracetamol (acetaminophen) with or without codeine or dihydrocodeine for neuropathic pain in adults. Cochrane Database Syst Rev. 2016;12:CD012227.
Moore RA, Chi CC, Wiffen PJ, Derry S, Rice ASC. Oral nonsteroidal anti‐inflammatory drugs for neuropathic pain. Cochrane Database Syst Rev. 2015;2015:CD010902.
Pountos I, Georgouli T, Calori GM, Giannoudis PV. Do nonsteroidal anti-inflammatory drugs affect bone healing? A critical analysis. ScientificWorldJournal. 2012;2012:606404.
Cardenas DD, Jensen MP. Treatments for chronic pain in persons with spinal cord injury: a survey study. J Spinal Cord Med. 2006;29:109–17.
Widerstrom-Noga EG, Turk DC. Types and effectiveness of treatments used by people with chronic pain associated with spinal cord injuries: influence of pain and psychosocial characteristics. Spinal Cord. 2003;41:600–9.
Adams EH, Breiner S, Cicero TJ, Geller A, Inciardi JA, Schnoll SH, et al. A comparison of the abuse liability of tramadol, NSAIDs, and hydrocodone in patients with chronic pain. J Pain Symptom Manag. 2006;31:465–76.
Angst MS, Clark JD. Opioid-induced hyperalgesia: a qualitative systematic review. Anesthesiology. 2006;104:570–87.
Bryce TN. Opioids should not be prescribed for chronic pain after spinal cord injury. Spinal Cord Ser Cases. 2018;4:66.
Chu LF, Clark DJ, Angst MS. Opioid tolerance and hyperalgesia in chronic pain patients after one month of oral morphine therapy: a preliminary prospective study. J Pain. 2006;7:43–8.
Dworkin RH, O’Connor AB, Backonja M, Farrar JT, Finnerup NB, Jensen TS, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007;132:237–51.
Martell BA, O’Connor PG, Kerns RD, Becker WC, Morales KH, Kosten TR, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146:116–27.
Widerstrom-Noga E, Biering-Sorensen F, Bryce TN, Cardenas DD, Finnerup NB, Jensen MP, et al. The International Spinal Cord Injury Pain Extended Data Set (Version 1.0). Spinal Cord. 2016;54:1036–46.
Chen Y, DeVivo MJ, Richards JS, SanAgustin TB. Spinal Cord Injury Model Systems: review of Program and National Database From 1970 to 2015. Arch Phys Med Rehabil. 2016;97:1797–804.
Widerstrom-Noga E, Biering-Sorensen F, Bryce TN, Cardenas DD, Finnerup NB, Jensen MP, et al. The International Spinal Cord Injury Pain Basic Data Set (version 2.0). Spinal Cord. 2014;52:282–6.
Arnér S, Meyerson BA. Lack of analgesic effect of opioids on neuropathic and idiopathic forms of pain. Pain. 1988;33:11–23.
Wall PD, Melzack R. Textbook of pain. Edinburgh: Churchill Livingstone; 1994.
Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, Sehgal N, et al. Opioid complications and side effects. Pain Physician. 2008;11:S105–20.
Alibrahim F, McIntyre A, Serrato J, Mehta S, Loh E, Teasell R. Heterotopic ossificaton following spinal cord injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Loh E, Sproule S, McIntyre A, Querée M, editors. Spinal cord injury rehabilitation evidence. Vancouver, BC: Spinal Cord Injury Research Evidence (SCIRE) Professional Project; 2016. Version 7.0:1–24.
Hsieh J, Benton B, Titus L, Gabison S, McIntyre A, Wolfe D, et al. Skin integrity and pressure injuries following spinal cord injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal cord injury rehabilitation evidence. Vancouver, BC: Spinal Cord Injury Research Evidence (SCIRE) Professional Project; 2020. Version 7.0:1–123.
National Spinal Cord Injury Statistical Center. Facts and figures at a glance 2019 SCI data sheet. University of Alabama at Brimingham National Spinal Cord Injury Statistical Center website; Birmingham, Alabama: University of Alabama at Birmingham; 2019.
TeslimOnigbinde A, Ogunsanya GI, Oniyangi SO. Pressure ulcer incidence among high-risk inpatients in Nigeria. Br J Nurs. 2012;21:S4–10.
Citak M, Suero EM, Backhaus M, Aach M, Godry H, Meindl R, et al. Risk factors for heterotopic ossification in patients with spinal cord injury: a case-control study of 264 patients. Spine. 2012;37:1953–7.
van Kuijk AA, Geurts AC, van Kuppevelt HJ. Neurogenic heterotopic ossification in spinal cord injury. Spinal Cord. 2002;40:313–26.
Ploumis A, Donovan JM, Olurinde MO, Clark DM, Wu JC, Sohn DJ, et al. Association between alendronate, serum alkaline phosphatase level, and heterotopic ossification in individuals with spinal cord injury. J Spinal Cord Med. 2015;38:193–8.
Rubayi S, Gabbay J, Kruger E, Ruhge K. The modified girdlestone procedure with muscle flap for management of pressure ulcers and heterotopic ossification of the hip region in spinal injury patients: a 15-year review with long-term follow-up. Ann Plast Surg. 2016;77:645–52.
Buckner R. Addressing impacts of heterotopic ossificans through seating and positioning for individuals with spinal cord injury: a case study. Physiother Res Rep. 2018;1:1–4.
Jamil F, Subbarao JV, Banaovac K, El Masry WS, Bergman SB. Management of immature heterotopic ossification (HO) of the hip. Spinal Cord. 2002;40:388–95.
Gefen A. Tissue changes in patients following spinal cord injury and implications for wheelchair cushions and tissue loading: a literature review. Ostomy Wound Manag. 2014;60:34–45.
Groah SL, Schladen M, Pineda CG, Hsieh CH. Prevention of pressure ulcers among people with spinal cord injury: a systematic review. PM R. 2015;7:613–36.
Barbetta DC, Lopes ACG, Chagas FNMR, Soares PT, Casaro FM, Poletto MF, et al. Predictors of musculoskeletal pain in the upper extremities of individuals with spinal cord injury. Spinal Cord. 2016;54:145–9.
Cratsenberg KA, Deitrick CE, Harrington TK, Kopecky NR, Matthews BD, Ott LM, et al. Effectiveness of exercise programs for management of shoulder pain in manual wheelchair users with spinal cord injury. J Neurol Phys Ther. 2015;39:197–203.
Tweedy SM, Beckman EM, Geraghty TJ, Theisen D, Perret C, Harvey LA, et al. Exercise and sports science Australia (ESSA) position statement on exercise and spinal cord injury. J Sci Med Sport. 2017;20:108–15.
Calis HT, Berberoglu N, Calis M. Are ultrasound, laser and exercise superior to each other in the treatment of subacromial impingement syndrome? A randomized clinical trial. Eur J Phys Rehabil Med. 2011;47:375–80.
Akyol Y, Ulus Y, Durmus D, Canturk F, Bilgici A, Kuru O, et al. Effectiveness of microwave diathermy on pain, functional capacity, muscle strength, quality of life, and depression in patients with subacromial impingement syndrome: a randomized placebo-controlled clinical study. Rheumatol Int. 2012;32:3007–16.
da Silva AC, De Noronha M, Liberatori-Junior RM, Aily JB, Gonçalves GH, Arrais-Lima C, et al. The effectiveness of ischemic compression technique on pain and function in individuals with shoulder pain: a systematic review. J Manipulative Physiol Ther. 2020;43:234–46.
Trofa DP, Obana KK, Herndon CL, Noticewala MS, Parisien RL, Popkin CA, et al. The evidence for common nonsurgical modalities in sports medicine, part 1: Kinesio tape, sports massage therapy, and acupuncture. J Am Acad Orthop Surg Glob Res Rev. 2020;4:e1900104.
Acknowledgements
The authors would like to acknowledge the data collectors in the SCIMSs centers.
Funding
The contents of this paper were developed under grants from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90SI5017, 90SI5023, 90SI5018, 90SI5015, 90SI5019, and 90DP0083). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this paper do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
Author information
Authors and Affiliations
Contributions
CYT was responsible for designing the work that led to the submission, acquiring and analyzing the data, interpreting results, and drafting and revising the paper. TNB was responsible for designing the work that led to the submission, interpreting results, and drafting part of the paper. ADD was responsible for designing the work that led to the submission, screening/recruiting eligible participants, and acquiring and analyzing the data. SM, BM, and SC were responsible for designing the work that led to the submission, interpreting results, and revising the paper. ERF was responsible for designing the work that led to the submission, analyzing the data, interpreting the results, and revising the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
Institutional Review Board approval (HSM# 11-01603) was obtained prior to conducting any study related procedures, and informed consent was obtained from each participant. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Tsai, CY., Bryce, T.N., Delgado, A.D. et al. Treatments that are perceived to be helpful for non-neuropathic pain after traumatic spinal cord injury: a multicenter cross-sectional survey. Spinal Cord 59, 520–528 (2021). https://doi.org/10.1038/s41393-021-00621-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00621-9